Abstract
The incidence of the diverticulum of the small bowel varies from 0.2-1.3% in autopsy studies to 2.3% when assessed on enteroclysis. It occurs mostly in patients in the 6th decade of their life. Of all the small bowel diverticuli, jejunal diverticulum is the most common type. This rare entity is usually asymptomatic. However, they may cause chronic non-specific symptoms for a long period of time like dyspepsia, chronic postprandial pain, nausea, vomiting, borborgymi, alternating diarrhoea and constipation, weight loss, anaemia, steatorrhea or rarely lead to complications like haemorrhage, obstruction, perforation. Obstruction can be due to enterolith, adhesions, intussusception, and volvulus. The condition is difficult to diagnose because patients are generally presented with symptoms that mimic other diseases. It is important for clinicians to have awareness of this entity. Here, we present a case of multiple jejunal diverticuli with a history of repeated attacks of diverticulitis over past 20 years, which were misdiagnosed and now presented with intestinal obstruction due to volvulus of the involved segment along with mesentery around its axis. Resection of the diverticuli segment of jejunum was done with end-to-end jejuno-jejunal anastomosis. The patient is asymptomatic since 10 months of follow-up.
Keywords: Diverticulitis, Small intestinal diverticulosis, Intestinal obstruction, Intestinal volvulus, Laparotomy
What’s Known
Majority of jejunal diverticula are an incidental finding.
Bowel obstruction in jejunal diverticulosis occur due to distended diverticula, inflammatory masses associated with diverticulitis, stricture or adhesions from diverticulitis, intussusception at the site of the diverticulum, or rarely as volvulus.
What’s New
Our patient had previously suffered multiple episodes of abdominal pain with vomiting and diarrhea for the preceding 20 years, suggestive of misdiagnosed subclinical/clinical diverticulitis.
We underscore the need for a diagnostic consideration in cases of chronic abdominal pain, diarrhea, and discomfort in uncomplicated cases to prevent diagnostic delay.
Introduction
The incidence of the diverticulum of the small bowel varies from 0.2-1.3% in autopsy studies to 2.3% when assessed on enteroclysis.1 It may be congenital or acquired and its prevalence increases with the age, occurring mostly in the 6th decade.2 These diverticula occur most commonly in jejunum in around 80%, followed by 15% in the ileum and 5% in both.3,4 Small bowel motility disorders leading to raised intraluminal pressure are the established factors for their development. Most of the patients are asymptomatic, but about 10-30% of patients tend to develop severe complications like diverticulitis, stone formation, perforation, haemorrhage and intestinal obstruction.1,2 Surgery is the mainstay in most of the patients with gastrointestinal obstruction.5 Variable presentation of diverticuli leads to delayed diagnosis or misdiagnosis which results in associated morbidity and mortality.6 In our case, the patient was presented with severe pain in the periumbilical region with vomiting, constipation and with a history of similar episodes of pain since 20 years. Investigations were suggestive of volvulus leading to small bowel obstruction. Resection with end-to-end jejuno-jejunal anastomosis was done.
Case Presentation
A 62-year-old male patient presented to surgery emergency with the complaint of severe pain in the periumbilical region, non-radiating to back since two days with 5-6 episodes of vomiting associated with constipation since one day. The patient had a history of abdominal pain and vomiting episodes followed by diarrhoea dating back to 20 years. Another episode, one and four years later, used to occur after regular meals with increased pain intensity. The patient required 3 days hospitalization for the last episode. During the past year, the frequency of pain and vomiting increased to multiple episodes. The patient is a known alcoholic and drug addict. He was clinically examined and investigated thoroughly. His blood pressure was 110/78 mmHg, pulse 86 per minute. On abdominal examination, the abdomen was mildly distended with periumbilical tenderness with the absent of bowel sounds. Per rectal examination was normal. Routine blood investigations were done. His Hb was 13.8 gm/dl, total leukocyte count 18,600/cmm, blood urea 32 mg/dl, serum creatinine 1.2 mg/dl, blood sugar 108 gm%, PTI 83.33%, S. bilirubin 1.2 mg, SGOT 22, SGPT 32, and S. amylase 75 IU. USG abdomen revealed mild free fluid in the lower abdomen with thickened twisted mesentery along with thrombosed mesenteric vein s/o mesenteric ischaemia. A CECT abdomen revealed a homogeneous circumferential wall thickening of the small bowel loops with the luminal compromise of the bowel, visualized twisting of the mesenteric vessels, and small bowel (jejunum) around the mesentery with mesenteric vessels creating the whirl sign suggestive of volvulus (figures 1 and 2) with few enlarged mesenteric lymph nodes. Provisional diagnosis of the small bowel obstruction due to volvulus was made. After initial fluid resuscitation and antibiotics, the patient was taken up for exploratory laparotomy with informed consent. On opening the abdomen, about 200 ml of fluid was aspirated and the abdomen inspected. It revealed multiple diverticula along mesenteric border of the jejunum with two clockwise complete rotation of the small bowel segment containing diverticuli around its mesenteric axis causing volvulus. Proximal jejunal loops were dilated, edematous and congested with collapsed distal gut loops with the normal anatomical position of caecum and duodeno-jejunal junction. Volvulus segment of bowel was edematous and inflamed with patchy discolouration throughout.
Figure 1.
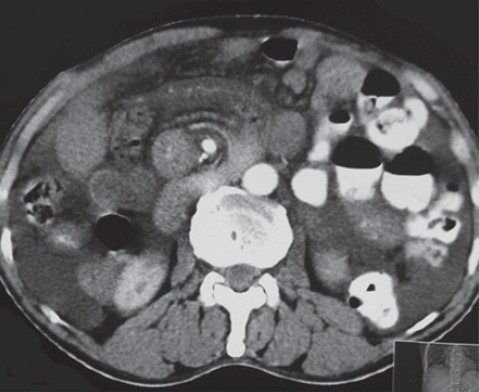
Transverse plane of CECT abdomen showing the classic whirlpool sign.
Figure 2.

Coronal section on CECT abdomen showing whirlpool sign.
After untwisting the volvulus segment, resection of about 1.5 feet of the affected part of the jejunum with diverticuli (figure 3) with end-to-end jejuno-jejunal anastomosis was done. After proper peritoneal toileting, the abdomen was closed in layers over a single drain placed in the pelvis. Appropriate antibiotics were started. Postoperative period was uneventful and the patient was discharged in satisfactory condition on the 12th postoperative day. The patient has remained asymptomatic on subsequent follow-ups since 10 months.
Figure 3.

Showing resected part of jejunum with multiple diverticula.
Discussion
Diverticuli is a false pulsion diverticuli, characterized by herniation of mucosa and submucosa through the muscular layer in places of minor resistance to the intraluminal pressure typically at the mesenteric side where blood vessels penetrate the intestinal wall.2-4,7 Diverticula occur more commonly in jejunum and in the terminal ileum, probably due to the larger size of the vasa recta.3,6
Diverticuli are usually multiple, in contrast to the congenital Meckel’s diverticulum.1 They tend to be larger and more in number in the proximal jejunum but smaller and fewer distally.1,6 Isolated jejunal diverticulosis coexists with diverticuli of the oesophagus (2%), of the duodenum (26%) and of the colon (35%).3
The etiology of diverticulosis is believed to develop as a result of abnormalities in peristalsis, intestinal dyskinesis probably due to motor dysfunction of the smooth muscle or myenteric plexus in the small bowel leading to high segmental intraluminal pressures and penetration of mucosa and submucosa through weak mesenteric sites.1-3
It is commonly seen with visceral neuropathies, visceral myopathy and connective tissue disorders like Ehlers-Danlos syndrome, progressive systemic sclerosis, and SLE.5 Intestinal diverticulae incidence increases with age and about 80% occurs in the 7th decade of life with slight male predominance.6
Majority of jejunal diverticuli are an incidental finding4,5 with most having chronic clinical manifestations which may be misdiagnosed as dyspepsia and irritable bowel syndrome. Patient presents with chronic postprandial pain, nausea, vomiting, borborgymi, alternating diarrhoea and constipation, weight loss, anaemia, steatorrhea, tenderness and fever, when symptomatic.5 A triad has been described by Edwards in such patients as “Flatulent dyspepsia: Epigastric pain, abdominal discomfort, flatulence one or two hours after meals”.3 Characteristically, the intermittent, variable periodicity and severity of symptoms extends over many years.6
Complications, namely inflammation, obstruction (dynamic/adynamic), perforation, hemorrhage, and malabsorption occur in 10-30% of cases,3,7 which may be managed conservatively. However, complications requiring surgical intervention occur in 8-30% of patients.2,3 Mechanical intestinal obstruction can be due to enteroliths, intussusception, adhesive band formation as a result of previous diverticulitis, and volvulus.7 In volvulus, the diverticulum acts as a pivot, commonly around the adhesive band2 or the fluid filled involved heavier segment might be responsible for initiating the volvulus.5,8 In literature, cases of bowel obstruction indiverticulosis due to distended diverticula, inflammatory mass associated with diverticulitis, stricture or adhesions from recent or past diverticulitis, and intussusception at the site of the diverticulum have been reported.9 Lobo et al. reported that dynamic intestinal obstruction is the most frequent complication of jejunal diverticulosis, which needs surgical intervention.10
Majority of jejuna diverticulosis, being asymptomatic or with mild symptoms, suspicion is difficult and the diagnosis is often missed or delayed. Thus, one should be aware of its varied presentation. It can be diagnosed radiographically on barium enema, which shows the corkscrew appearance.5,8 The enteroclysis and enteroscopy are the best diagnostic imaging, however, in emergency situations like in the present case due to time constraints its utility is limited.2 When complications arise, computed tomography is the best investigation. The “whirl sign” on abdominal CT shows spiral shape of the mesenteric vessels, accompanying the intestinal loops and their feeding vessels. On angiogram,‘barber pole sign’ may be seen due to spiralling of superior mesenteric artery.8
Most of acute complications of jejunoileal diverticulum need surgical intervention. As in our patient, conclusive diagnosis was made by diagnostic laparotomy, resulting in appropriate surgical treatment such as intestinal resection with end-to-end anastomosis. A simple diverticulectomy, as advised earlier, is no longer recommended as it causes increased incidence of postoperative leakage, sepsis, and death.6
The purpose of presenting this case is that the patient in our case had previous multiple episodes of abdominal pain with vomiting and diarrhoea after food intake for past 20 years. These were suggestive of subclinical and clinical diverticulitis and misdiagnosed for such a long period of time. Thus, it stresses the need for a diagnostic consideration in cases of chronic abdominal pain, diarrhoea, and discomfort in uncomplicated cases to prevent diagnostic delay and the associated mortality.
Conclusion
Although this phenomenon is rare, we should keep in mind that intestinal diverticulosis may induce intestinal obstructions of different kinds. Thus, repeat physical examinations and X-ray films are needed and enteroclysis studies or CT scan is helpful in diagnosis. Timely intervention prevents associated mortality.
Acknowledgement
We are thankful to Dr. Prem Singla, Dr. Neeraj Pawar, Dr. Chandrashekhar, Dr. Kamlesh Singh for their help and support in preparing this case report.
Conflict of Interest: None declared.
References
- 1.Lin CH, Hsieh HF, Yu CY, Yu JC, Chan DC, Chen TW, et al. Diverticulosis of the jejunum with intestinal obstruction: A case report. World J Gastroenterol. 2005;11:5416–7. doi: 10.3748/wjg.v11.i34.5416. [ PMC Free Article] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nejmeddine A, Bassem A, Mohamed H, Hazem BA, Ramez B, Issam BM. Complicated jejunal diverticulosis: A case report with literature review. N Am J Med Sci. 2009;1:196–9. [ PMC Free Article] [PMC free article] [PubMed] [Google Scholar]
- 3.Falidas E, Vlachos K, Mathioulakis S, Archontovasilis F, Villias C. Multiple giant diverticula of the jejunum causing intestinal obstruction: report of a case and review of the literature. World J Emerg Surg. 2011;6:8. doi: 10.1186/1749-7922-6-8. [ PMC Free Article] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Aydin I, Pergel A, Yucel AF, Sahin DA. A rare cause of acute abdomen: jejunal diverticulosis with perforation. J Clin Imaging Sci. 2013;3:31. doi: 10.4103/2156-7514.115763. [ PMC Free Article] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hu JL, Chen WZ. Midgut volvulus due to jejunal diverticula: a case report. World J Gastroenterol. 2012;18:5826–9. doi: 10.3748/wjg.v18.i40.5826. [ PMC Free Article] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Singh O, Gupta SS, Shukla S, Mathur RK, Shukla S. Jejunal diverticulae: reports of two cases with review of literature. Indian J Surg. 2009;71:238–44. doi: 10.1007/s12262-009-0077-5. [ PMC Free Article] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tiwari A, Gupta V, Hazrah P, Lal R. A rare case of multiple jejunal diverticulosis presenting as intestinal obstruction. Clin Pract. 2013;3:e21. doi: 10.4081/cp.2013.e21. [ PMC Free Article] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sekar GP, Subha TV, Selvaraj B, Usman MM. Small bowel volvulus due to multiple jejuna diverticulae – a rare case report. International Journal of Recent Trends in Science And Technology. 2014;11:207–9. [Google Scholar]
- 9.Hayee B, Khan HN, Al-Mishlab T, McPartlin JF. A case of enterolith small bowel obstruction and jejunal diverticulosis. World J Gastroenterol. 2003;9:883–4. doi: 10.3748/wjg.v9.i4.883. [ PMC Free Article] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lobo DN, Braithwaite BD, Fairbrother BJ. Enterolith ileus complicating jejunal diverticulosis. J Clin Gastroenterol. 1999;29:192–3. doi: 10.1097/00004836-199909000-00019. [DOI] [PubMed] [Google Scholar]


