Abstract
Background:
The present study aimed to (i) evaluate previous observations that the association of blood pressure (BP) with outcomes varies by gait speed and (ii) evaluate the association of subsequent changes in BP and cardiovascular risk.
Methods:
Participants included 2,669 adults aged 70–79 years in the Health, Aging, and Body Composition (Health ABC) study. Gait speed was dichotomized at ≥1.0 m/s over a 20-m test at baseline. BP was measured at baseline, and changes in BP over 5 years were evaluated using (i) population-based trajectory models and (ii) intraindividual mean and slope.
Results:
Over a mean of 10 years, there were 1,366 deaths, 336 first myocardial infarctions, and 295 first strokes. There was a differential pattern of association between baseline systolic BP and diastolic BP and outcomes among brisk and moderate speed walkers. For example, the association between higher diastolic BP and mortality was in the protective direction for moderate speed walkers (hazard ratio = 0.75; 95% confidence interval: 0.63, 0.91) per 10 mmHg higher, whereas it was null in brisk walkers (hazard ratio = 1.05; 95% confidence interval: 0.98, 1.11), p value for interaction .01. The 5-year population-based trajectories did not add important information beyond baseline BP. Individual slopes in both systolic BP and diastolic BP did not appear to have important associations with the outcomes.
Conclusions:
In this study, we found that the overall level of BP was associated with myocardial infarction, stroke, and death, and this association differed by baseline gait speed, whereas changes in BP were not associated with these outcomes.
Key Words: Blood pressure, Epidemiology, Function, Gait speed, Hypertension.
Recent evidence has demonstrated that the associations of blood pressure (BP) with death and cardiovascular events may vary by functional status (1–5). In general, among well-functioning older adults, the association between high BP and worse clinical outcomes is strong and graded, similar to that observed in younger adults. In contrast, among persons with poor functional status, the association is either null or reversed, whereby higher BP is associated with better outcomes.
These prior investigations have examined the association of a one-time or “baseline” measure of BP and outcomes across strata of functional status. Although the one-time level of BP is strongly associated with outcomes, the single measure ignores the changes in BP over time. There is a developing body of literature on the associations of changes in BP and outcomes, although the findings have been mixed. Among young and middle-aged adults, increasing BP has been associated with coronary artery calcification (6), whereas in older adults, decreasing BP levels have been associated with increased mortality risk (7,8). No prior study has examined the impact of functional status on the associations of BP trajectories and outcomes.
The goal of the present investigation was 2-fold. First, we aimed to replicate prior studies that have demonstrated a differential association of baseline BP and outcomes, across levels of functional status. Second, we aimed to determine if subsequent changes in BP over 5 years were associated with cardiovascular risk. We conducted this investigation in a cohort of well-functioning black and white adults aged 70–79 years at baseline. We used gait speed as a measure of functional status, as it is an excellent integrative measure of health status and frailty, and may be a useful measure for risk stratification (9). We assessed BP at baseline, and then summarized subsequent changes in BP over 5 years by two methods: population-based trajectory models and intraindividual (within person) changes. This study will help elucidate whether or not subsequent changes in BP adds additional information beyond one-time BP levels, and whether these associations differ by gait speed in this population of older adults, free of disability at baseline.
Methods
Study Design and Participants
The Health, Aging, and Body Composition (Health ABC) study was a prospective study designed to assess health and function in initially well-functioning elderly adults. At baseline, the cohort included 3,075 persons aged 70–79 years; 42% self-reported as Black race and 52% were female. At each of the two study sites—Pittsburgh, Pennsylvania, and Memphis, Tennessee—participants were recruited from a list of Medicare beneficiaries between April 1997 and June 1998. Inclusion criteria were (i) reported ability to walk one-quarter mile, climb 10 steps, and perform basic activities of daily living without difficulty; (ii) the absence of life-threatening illness; and (iii) intention to remain in the current geographic area for at least 3 years. All participants gave informed written consent; the protocol was approved by the institutional review boards of the clinical sites and the Data Coordinating Center (University of California, San Francisco).
Outcomes
Outcomes of interest included incident myocardial infarction (MI) and stroke, and all-cause mortality. Follow-up for outcomes occurred every 6 months either by telephone or by annual visits to clinical centers, and participants were asked about hospitalizations and major outpatient procedures. Deaths were ascertained by review of local obituaries, by reports to the clinical centers by family members, or by means of the semiannual contacts. Diagnoses and cause of death were adjudicated based on interview, review of all hospital records, death certificates, and other support documents by a panel of clinicians.
Independent Variables
BP was measured annually and calculated as the average of two measurements by mercury sphygmomanometer, taken in the seated position after 5 minutes of quiet rest. Gait speed was measured as usual gait speed over a 20-m course. In the present study, “brisk walkers” were defined as participants with a usual gait speed ≥1.0 m/s; this cutpoint was chosen based on the strength of association with mortality in Health ABC study. “Moderate speed walkers” were defined as those participants with a usual gait speed of <1.0 m/s.
Other Variables
Other characteristics evaluated were as follows: age, sex, race, clinical site, educational level, fasting glucose, fasting high-density lipoprotein and low-density lipoprotein cholesterol, fasting triglycerides, smoking history, body mass index, diabetes, coronary heart disease (angina, MI, or revascularization), cerebrovascular disease (transient ischemic attack, stroke, or carotid endarterectomy), and heart failure. Coronary heart disease, cerebrovascular disease, and heart failure were assessed by self-report and medication use. Diabetes was assessed by self-report, medication use, or a positive diagnosis by fasting blood glucose level or oral glucose tolerance test. Medications were brought in by the participants and recorded.
Statistical Analysis
We compared the mean and proportion of baseline characteristics of the study participants across brisk and moderate speed gait speed. We also described baseline characteristics among those with and without gait speed test data.
We stratified the population, a priori, based on gait speed (≥1.0 and <1.0 m/s). We used Cox proportional hazards models to examine the unadjusted associations of baseline systolic BP (SBP) and diastolic BP (DBP) with mortality, MI, and stroke; hazard ratios are presented per 10 mmHg higher BP. We also tested for statistical interactions by including an interaction term between either SBP or DBP, and gait speed classified as a binary variable (brisk vs moderate speed). We then adjusted for covariates listed above in order to estimate the adjusted relationships; variables were classified as presented in Table 1. As an exploratory analysis, we also evaluated the association of BP with mortality, stratified by both gait speed and antihypertensive medication use; the number of MI and stroke events was not sufficient to examine further stratified analyses for these outcomes. We also present the event rates in persons with low and high BP; SBP was dichotomized as <140 and ≥140 mmHg and DBP was dichotomized as <80 and ≥80 mmHg because only 6% of the study population had DBP ≥90 mmHg.
Table 1.
Baseline Characteristics of Participants Stratified by Gait Speed
| Brisk Walkers (≥1.0 m/s) (N = 2,464) | Moderate Speed Walkers (<1.0 m/s) (N = 205) | |
|---|---|---|
| Mean ± SD or N (%) | ||
| Site | ||
| Memphis | 1,222 (49.6%) | 104 (50.7%) |
| Pittsburgh | 1,242 (50.4%) | 101 (49.3%) |
| Age (y) | 73.5±2.8 | 74.2±3.0 |
| Women | 1,203 (48.8%) | 161 (78.5%) |
| Black | 921 (37.4%) | 147 (71.7%) |
| Education | ||
| Less than high school | 533 (21.6%) | 82 (40%) |
| High school graduate | 821 (33.3%) | 70 (34.1%) |
| Postsecondary | 1,103 (44.8%) | 52 (25.4%) |
| Smoking status | ||
| Never | 1,080 (43.8%) | 106 (51.7%) |
| Current smoker | 236 (9.6%) | 30 (14.6%) |
| Former smoker | 1,145 (46.5%) | 68 (33.2%) |
| Body mass index (kg/m2) | ||
| <25 | 825 (33.5%) | 48 (23.4%) |
| 25–30 | 1,067 (43.3%) | 61 (29.8%) |
| >30 | 572 (23.2%) | 96 (46.8%) |
| Fasting glucose (mmol/L) | 5.74±1.77 | 5.86±2.26 |
| HDL cholesterol (mmol/L) | 1.38±0.43 | 1.51±0.52 |
| LDL cholesterol (mmol/L) | 3.15±0.87 | 3.20±1.00 |
| Triglycerides (mmol/L) | 1.57±0.91 | 1.39±0.74 |
| Diabetes | 343 (13.9%) | 43 (21.0%) |
| Coronary heart disease | 435 (18.0%) | 47 (23.7%) |
| Cerebrovascular disease | 172 (7.1%) | 26 (12.9%) |
| Heart failure | 57 (2.3%) | 10 (5.0%) |
| Antihypertensive medication use | 1,265 (51.3%) | 132 (64.4%) |
| SBP (mmHg) | 134.5±19.2 | 138.5±21.4 |
| DBP (mmHg) | 71.1±11.0 | 70.6±11.4 |
| SBP ≥ 140 mmHg | 849 (34.5%) | 90 (43.9%) |
| DBP ≥ 80 mmHg | 473 (19.2%) | 40 (19.5%) |
| 5-y intraindividual mean SBP (mmHg)* | 135.3±15.2 | 136.9±16.7 |
| 5-y intraindividual slope SBP (mmHg/y)* | 0.87±5.00 | 0.36±5.77 |
| 5-y intraindividual mean DBP (mmHg)* | 71.4±8.3 | 71.1±9.2 |
| 5-y intraindividual slope DBP (mmHg/y)* | 0.21±2.86 | 0.37±2.9 |
Notes: DBP = diastolic blood pressure; HDL = high-density lipoprotein; LDL = low-density lipoprotein; SBP = systolic blood pressure.
*Over 5 years; 1,974 for brisk walkers and 134 for moderate speed walkers.
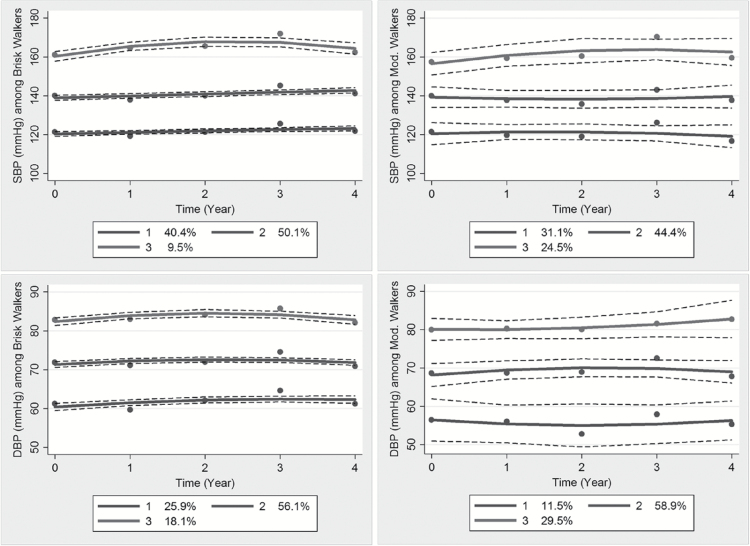
We were interested in understanding the relative importance of subsequent BP changes over 5 years with outcomes. We explored BP changes in two ways. First, we used a population-based trajectory model (10,11), which is an example of a finite mixture model, to identify distinctive clusters of trajectories of BP over 5 years in brisk and moderate speed walkers. In order to compare with the baseline BP analyses, we classified participants based on their baseline gait speed performance. A three-group model with quadratic trajectory was found to be the best model for both moderate speed and brisk walkers, based on the Bayesian information criterion. We plotted the estimated trajectories of BP for these three groups over 5 years. Next, we fit unadjusted Cox proportional hazards models of the outcomes using the trajectory group as the independent variable. The outcome in these models was the time-to-event from the fifth visit year; participants with an MI or stroke prior to the fifth visit were excluded from these analyses, respectively.
In a second approach, we calculated intraindividual mean and slope, based on ordinary least squares regression of the first 5 years of BP measurements. Participants were included in this analysis if they had at least three BP measures (n = 2,108) over these 5 years and had completed the fifth follow-up visit. The mean was calculated as the average of the measures, and the slope was calculated as the beta coefficient from a regression of BP on time (in years). These two parameters were then used as independent predictor variables in both unadjusted and adjusted Cox proportional hazards models of the three outcomes, assessed starting after the year 5 visit. Again, participants with an MI or stroke prior to the fifth visit were excluded from these analyses, respectively.
All analyses were conducted using Stata 13.1 (StataCorp, College Station, TX).
Results
Participants
Of the 2,669 participants with gait speed measured over the 20-m test, 2,464 (92%) had a gait speed of 1 m/s or faster (Table 1). Overall, brisk walkers were younger, less likely to be women and of black race, and had more years of education compared with moderate speed walkers (Table 1). Brisk walkers were more likely to be former smokers and had lower body mass index. Brisk walkers had lower high-density lipoprotein cholesterol, but higher triglycerides compared with moderate speed walkers. Chronic health conditions, including diabetes, coronary heart disease, cerebrovascular disease, and heart failure, and use of antihypertensives were less prevalent in brisk walkers compared with moderate speed walkers.
Compared with those with measured gait speed, the 406 with missing values were on average older and had higher chronic disease; characteristics are presented in Supplementary Table S1. The associations of SBP and DBP with the outcomes did not differ among those with and without measured gait speed (p > .1 for all interactions).
Baseline SBP and DBP and Outcomes
Over a mean of 10 years, there were 1,366 deaths, 336 first MIs, and 295 first strokes (Table 2). The absolute event rates of mortality and stroke were highest among those with moderate walking speed, regardless of SBP (Table 2). In proportional hazards models, higher SBP at baseline was associated with mortality, MI, and stroke in brisk walkers, although the association with MI no longer reached statistical significance after adjustment for covariates (Table 2). In contrast, among moderate speed walkers, higher SBP was not significantly associated with any of the outcomes. The different patterns of association across gait speed were more evident for DBP. Among moderate speed walkers, the event rates among persons with DBP ≥80 mmHg were lower compared with those in persons with DBP <80 mmHg and were similar to the event rates in brisk walkers. The association between higher DBP and mortality differed significantly by gait speed and was in the protective direction for moderate speed walkers (hazard ratio = 0.75 [95% confidence interval: 0.63, 0.91] per 10 mmHg higher). There were also differences for the outcome of stroke; among brisk walkers, a 10 mmHg higher DBP was associated with a hazard ratio for stroke of 1.26 (95% confidence interval: 1.11, 1.42). In contrast, higher DBP was not associated with stroke among moderate speed walkers. The differential pattern of the association of DBP and mortality among moderate speed and brisk walkers persisted when we additionally stratified by antihypertensive medication use (Supplementary Table S2).
Table 2.
Association of Baseline SBP and DBP With Mortality, MI, and Stroke Stratified by Gait Speed
| Brisk Walkers (≥1.0 m/s) (n = 2,464) | Moderate Speed Walkers (<1.0 m/s) (n = 205) | p Value for Interaction | ||
|---|---|---|---|---|
| SBP | ||||
| Mortality (n = 1,366) | ||||
| Rate per 1,000 person-years | ≥140 mmHg | 43.7 | 59.1 | |
| <140 mmHg | 36.2 | 60.3 | ||
| HR (95% CI) | Unadjusted | 1.05 (1.02, 1.08)** | 0.97 (0.90, 1.06) | .11 |
| Per 10 mmHg higher | Adjusted† | 1.04 (1.00, 1.07)* | 0.96 (0.87, 1.06) | .13 |
| MI (n = 336) | ||||
| Rate per 1,000 person-years | ≥140 mmHg | 14 | 10.6 | |
| <140 mmHg | 10.6 | 14.3 | ||
| HR (95% CI) | Unadjusted | 1.08 (1.02, 1.15)** | 1.01 (0.84, 1.21) | .54 |
| Per 10 mmHg higher | Adjusted† | 1.06 (0.99, 1.03) | 0.96 (0.77, 1.20) | .46 |
| Stroke (n = 295) | ||||
| Rate per 1,000 person-years | ≥140 mmHg | 12.8 | 20.5 | |
| <140 mmHg | 9.6 | 16.3 | ||
| HR (95% CI) | Unadjusted | 1.11 (1.05, 1.18)** | 1.07 (0.91, 1.25) | .65 |
| Per 10 mmHg higher | Adjusted† | 1.10 (1.03, 1.17)** | 1.06 (0.88, 1.29) | .55 |
| DBP | ||||
| Mortality (n = 1,366) | ||||
| Rate per 1,000 person-years | ≥80 mmHg | 39.7 | 45.5 | |
| <80 mmHg | 37.1 | 65.1 | ||
| HR (95% CI) | Unadjusted | 1.02 (0.96, 1.08) | 0.84 (0.72, 0.97)* | .01 |
| Per 10 mmHg higher | Adjusted† | 1.05 (0.98, 1.11) | 0.75 (0.63, 0.91)** | .01 |
| MI (n = 336) | ||||
| Rate per 1,000 person-years | ≥80 mmHg | 12.5 | 12.4 | |
| <80 mmHg | 11 | 13.5 | ||
| HR (95% CI) | Unadjusted | 1.05 (0.94, 1.16) | 0.98 (0.70, 1.37) | .67 |
| Per 10 mmHg higher | Adjusted† | 1.00 (0.89, 1.12) | 0.88 (0.57, 1.36) | .99 |
| Stroke (n = 295) | ||||
| Rate per 1,000 person-years | ≥80 mmHg | 12.7 | 10.1 | |
| <80 mmHg | 9.5 | 20.1 | ||
| HR (95% CI) | Unadjusted | 1.19 (1.06, 1.33)** | 0.87 (0.65, 1.16) | .04 |
| Per 10 mmHg higher | Adjusted† | 1.26 (1.11, 1.42)*** | 0.93 (0.64, 1.35) | .09 |
Notes: CI = confidence interval; DBP = diastolic blood pressure; HDL = high-density lipoprotein; HR = hazard ratio; LDL = low-density lipoprotein; MI = myocardial infarction; SBP = systolic blood pressure.
*p < .05, **p < .01, ***p < .001.
†Adjusted for age, gender, race, education, smoking status, body mass index, fasting glucose, HDL, LDL, triglycerides, coronary heart disease (not for MI model), cerebrovascular disease (not for stroke model), heart failure, and antihypertensive medications.
There was no evidence for effect modification of SBP or DBP by gait speed measured at the fifth visit (p > .1 for all interactions), although the missing gait speed measures appeared informative at this visit. The estimates of effect of higher SBP and DBP were consistently further in the protective direction for those not completing the gait test compared with those who completed the test (Supplementary Table S3).
Trajectories of SBP and DBP Over 5 Years and Outcomes
After the first 5 years of follow-up, there were 880 deaths, 211 first MIs, and 202 first strokes. The population-based trajectory groups of SBP and DBP among moderate speed and brisk walkers appeared to be primarily distinguished by baseline level of BP; the differences in change in BP over 5 years appeared small across the groups (Figure 1). The associations between the population trajectory groups and outcomes paralleled what we observed for the baseline level of BP and outcomes (Table 3). Among brisk walkers, the group with the persistently high trajectory of SBP had an increased risk of mortality, MI, and stroke; whereas a high trajectory of SBP was directionally and significantly associated with only MI in moderate speed walkers, and the estimate was imprecise. Among brisk walkers, the group with the persistently high trajectory of DBP had an increased risk for death and stroke; whereas among the moderate speed walkers, the group with the high trajectory of DBP had lower risks for these same outcomes.
Figure 1.
Trajectories of SBP (top) and DBP (bottom) over 5 years from population-based trajectory models, in brisk (left) and moderate speed (right) walkers based on quadratic model. DBP = diastolic blood pressure; SBP = systolic blood pressure.
Table 3.
Unadjusted and Adjusted Association of Population-based Trajectories of BP Over 5 Years With Mortality, MI, and Stroke Stratified by Baseline Gait Speed
| Brisk Walkers (≥1.0 m/s) | Moderate Speeder Walkers (<1.0 m/s) | ||||||
|---|---|---|---|---|---|---|---|
| HR (95% CI) | |||||||
| Group 1 | Group 2 | Group 3 | Group 1 | Group 2 | Group 3 | ||
| SBP | (n = 978) | (n = 1,262) | (n = 213) | (n = 60) | (n = 95) | (n = 50) | |
| Mortality (n = 880) | Unadjusted | Reference | 1.22 (1.05, 1.42)* | 1.68 (1.34, 2.12)*** | Reference | 0.79 (0.49, 1.29) | 0.80 (0.49, 1.29) |
| Adjusted† | Reference | 1.23 (1.05, 1.45)* | 1.60 (1.25, 2.05)*** | Reference | 0.57 (0.32, 1.01) | 0.77 (0.38, 1.54) | |
| MI (n = 211) | Unadjusted | Reference | 1.15 (0.85, 1.57) | 2.34 (1.54, 3.57)*** | Reference | 1.67 (0.34, 8.26) | 3.48 (0.70, 17.3) |
| Adjusted† | Reference | 1.18 (0.85, 1.64) | 1.96 (1.24, 3.11)** | Reference | ‡ | ‡ | |
| Stroke (n = 202) | Unadjusted | Reference | 1.38 (1.00, 1.90)* | 2.83 (1.85, 4.34)*** | Reference | 0.93 (0.33, 2.62) | 0.82 (0.23, 2.90) |
| Adjusted† | Reference | 1.31 (0.93, 1.84) | 2.44 (1.52, 3.90)*** | Reference | 0.97 (0.27, 3.49) | 0.64 (0.11, 3.61) | |
| DBP | (n = 595) | (n = 1,455) | (n = 414) | (n = 19) | (n = 132) | (n = 54) | |
| Mortality (n = 880) | Unadjusted | Reference | 0.87 (0.73, 1.02) | 1.24 (1.01, 1.52)* | Reference | 0.72 (0.38, 1.33) | 0.33 (0.15, 0.71)** |
| Adjusted† | Reference | 0.99 (0.83, 1.15) | 1.46 (1.16, 1.84)* | Reference | 0.80 (0.39, 1.63) | 0.33 (0.14, 0.78)* | |
| MI (n = 211) | Unadjusted | Reference | 1.00 (0.71, 1.40) | 1.07 (0.69, 1.67) | Reference | 0.61 (0.13, 2.83) | 0.37 (0.06, 2.24) |
| Adjusted† | Reference | 1.05 (0.73, 1.49) | 1.13 (0.71, 1.80) | Reference | ‡ | ‡ | |
| Stroke (n = 202) | Unadjusted | Reference | 1.32 (0.90, 1.93) | 1.87 (1.20, 2.93)** | Reference | 0.30 (0.10, 0.88)* | 0.22 (0.06, 0.82)* |
| Adjusted† | Reference | 1.35 (0.90, 2.00) | 2.01 (1.24, 3.27)** | Reference | 0.39 (0.09, 1.65) | 0.27 (0.05, 1.35) | |
Notes: BP = blood pressure; CI = confidence interval; DBP = diastolic blood pressure; HDL = high-density lipoprotein; LDL = low-density lipoprotein; MI = myocardial infarction; SBP = systolic blood pressure.
*p < .05, **p < .01, ***p < .001.
†Adjusted for age, gender, race, education, smoking status, body mass index, fasting glucose, HDL, LDL, triglycerides, coronary heart disease (not for MI model), cerebrovascular disease (not for stroke model), heart failure, and antihypertensive medications.
‡Insufficient cell size.
Intraindividual slope of BP over 5 years did not add important information beyond the mean (Table 4). Among brisk walkers at baseline, higher mean SBP over 5 years (per SD) was associated with increased risk of mortality, MI, and stroke, and slope was not associated with any of these outcomes. Among brisk walkers, higher mean DBP was associated with a greater risk of death and stroke, and a steeper increase in DBP was associated with increased risk of MI. In contrast, among moderate speed walkers, higher mean DBP was associated with a decreased risk of death and stroke.
Table 4.
Person-specific Mean and Slope of SBP and DBP Over 5 Years and Mortality, MI, and Stroke Stratified by Baseline Gait Speed
| Brisk Walkers (≥1.0 m/s) (n = 1,974) | Moderate Speed Walkers (<1.0 m/s) (n = 134) | ||
|---|---|---|---|
| Hazard Ratio (95% Confidence Interval) | |||
| Per 10 mmHg for Mean and per 1 mmHg/Y for Slope | |||
| SBP | |||
| Mortality (n = 727) | |||
| Intraindividual mean§ | Unadjusted | 1.11 (1.06, 1.17)*** | 0.95 (0.82, 1.10) |
| Adjusted† | 1.10 (1.05, 1.17)*** | 0.89 (0.73, 1.07) | |
| Intraindividual slope | Unadjusted | 1.00 (0.98, 1.01) | 0.97 (0.93, 1.02) |
| Adjusted† | 1.00 (0.98, 1.02) | 0.97 (0.92, 1.03) | |
| MI (n = 194) | |||
| Intraindividual mean | Unadjusted | 1.21 (1.10, 1.33)*** | 1.26 (0.94, 1.70) |
| Adjusted† | 1.17 (1.06, 1.30)** | ‡ | |
| Intraindividual slope | Unadjusted | 1.00 (0.97, 1.03) | 0.97 (0.89, 1.06) |
| Adjusted† | 1.02 (0.99, 1.05) | ‡ | |
| Stroke (n = 191) | |||
| Intraindividual mean | Unadjusted | 1.24 (1.13, 1.37)*** | 1.05 (0.79, 1.40) |
| Adjusted† | 1.21 (1.09, 1.34)*** | 1.00 (0.67, 1.49) | |
| Intraindividual slope | Unadjusted | 1.01 (0.98, 1.04) | 0.96 (0.88, 1.04) |
| Adjusted† | 1.00 (0.97, 1.03) | 0.95 (0.84, 1.06) | |
| DBP | |||
| Mortality (n = 727) | |||
| Intraindividual mean§ | Unadjusted | 1.05 (0.96, 1.15) | 0.65 (0.51, 0.83)*** |
| Adjusted† | 1.14 (1.03, 1.26)* | 0.52 (0.37, 0.72)*** | |
| Intraindividual slope | Unadjusted | 1.00 (0.97, 1.03) | 0.97 (0.89, 1.06) |
| Adjusted† | 1.00 (0.97, 1.03) | 0.94 (0.84, 1.04) | |
| MI (n = 194) | |||
| Intraindividual mean | Unadjusted | 1.06 (0.89, 1.27) | 0.84 (0.46, 1.52) |
| Adjusted† | 1.10 (0.91, 1.33) | ‡ | |
| Intraindividual slope | Unadjusted | 1.00 (0.95, 1.05) | 0.87 (0.71, 1.06) |
| Adjusted† | 1.06 (1.00, 1.12)* | ‡ | |
| Stroke (n = 191) | |||
| Intraindividual mean§ | Unadjusted | 1.22 (1.02, 1.47)* | 0.57 (0.35, 0.94)* |
| Adjusted† | 1.26 (1.03, 1.54)* | 0.35 (0.15, 0.78)** | |
| Intraindividual slope | Unadjusted | 0.98 (0.93, 1.04) | 0.94 (0.79, 1.13) |
| Adjusted† | 0.97 (0.92, 1.03) | 0.73 (0.56, 0.94)* | |
Notes: DBP = diastolic blood pressure; HDL = high-density lipoprotein; LDL = low-density lipoprotein; MI = myocardial infarction; SBP = systolic blood pressure.
*p < .05, **p < .01, ***p < .001.
†Adjusted for age, gender, race, education, smoking status, body mass index, fasting glucose, HDL, LDL, triglycerides, coronary heart disease (not for MI model), cerebrovascular disease (not for stroke model), heart failure, and antihypertensive medications.
‡Insufficient cell size.
§Statistically significant interaction.
Discussion
This study contributes to the growing body of evidence that demonstrates the heterogeneity of older adults with regard to the association of BP and outcomes. Consistent with prior research, we observed differential patterns of associations between level of BP and outcomes by gait speed among older adults (1,2). Among brisk walkers, higher BP was associated with an increased risk of death, MI, and stroke, whereas among moderate speed walkers, the associations were null or even reversed. The patterns of associations were similar when BP was measured as a single baseline measure or as an average over 5 years. We did not observe clear trajectories of change in BP for the population overall, and intraindividual 5-year changes in BP were not associated with risk of events. Taken together, these findings suggest that although the level of BP is differentially associated with outcomes among brisk and moderate speed walkers, 5-year changes in BP as assessed by the methods employed do not appear to be important determinants of cardiovascular risk in this cohort of older adults free of disability at baseline.
The present study confirms prior investigations that have found that the association of higher BP and mortality was in the harmful direction among better functioning older adults, and attenuated or inverted among poorer functioning older adults (1–5). To our knowledge, this is the first study to evaluate differences between the association of BP trajectories and outcomes, across a measure of functional status. Recent attention has focused on the importance of the trajectory of BP and outcomes. In young and middle-aged adults, Allen et al. (6) identified five distinct trajectories of BP, and both higher and increasing BP trajectories were associated with increased coronary calcification. There have been conflicting findings regarding the importance of the trajectory of BP in older adults. In the Established Populations for Epidemiologic Studies of the Elderly, Satish et al. (7) found among older adults that a decrease of 20 mmHg SBP or 10 mmHg DBP over 3 years was associated with an increased risk of mortality, cardiovascular mortality, and cardiovascular events. Additionally, in the Leiden 85-plus Study, a cohort study of 271 Swedish men and women aged 85 years at baseline, investigators found that falling and low SBP <150 mmHg were associated with increased risk of mortality (8). In an urban primary care system cohort, both increasing and decreasing BP were associated with mortality (12). Some of the discrepancy in findings may be due to the different methods used to measure change. Group-based methods average changes across populations and do not capture within-person change. Therefore, we used a second approach to estimate within-person change over time; based on this approach, we observed wide variability in the within-person change over five visits, as evidenced by the high SD of SBP and DBP slope. In the present study, neither the group-based nor intraindividual change estimates were associated with cardiovascular events.
We found that the level of BP, measured at a single time-point or averaged over 5 years, was independently associated with cardiovascular events and mortality, and these associations differed by functional status. The associations were more robust when we used the time-averaged measures, presumably because of the reduced variability of time-averaged measures and because this approach may better capture the cumulative burden of high BP over time. The mechanisms mediating these divergent associations merit further investigation. Low BP may be a marker of subclinical vascular disease in poor functioning older adults. Additionally, recent literature has reported an association of low BP and an increased risk of falls and fracture in poorer functioning older adults, which could result in a cascade of events that lead to morbidity and mortality (13,14). Finally, some have suggested that low DBP may also result in inadequate perfusion of the central organs, especially the heart, which is perfused during diastole (5,15).
This study also has some limitations that should be considered when interpreting the results. Primarily, there were a small number of moderate speed walkers <1 m/s in the Health ABC study. We chose this threshold because it was most strongly associated with mortality, and is therefore a strong discriminator of health status; however, there is limited ability to look at the lower functioning group in this cohort. Notably, the level of gait speed did not modify the effect of BP at the fifth visit, although the associations of BP and outcomes varied among those with and without gait speed data at this visit. These findings support the hypothesis that functional status is an effect modifier of BP, although highlight the uncertainty over which test or threshold may best capture this modification. Future studies or systematic reviews that examine multiple measures across multiple cohorts may better answer this question. Additionally, although we examined trajectories of BP over time, we were unable to examine trajectories prior to enrollment in the Health ABC study. The reasons why brisk and moderate speed walkers had low or high levels of BP may be complex and due to a lifetime of exposures and lifestyle. In addition, we did not observe large changes in BP in the study population likely partially due to the pharmacologic control of BP over the follow-up period; over half of the study population was on medication for BP. Finally, we did not examine whether these associations varied by other factors that may affect the optimal level of BP including diabetes and chronic kidney disease.
In summary, we confirm prior investigations that have demonstrated a differential association between level of BP and outcomes among brisk and moderate speed walkers. This is the first study to examine subsequent changes in BP, and we did not observe clear population-based patterns of change across 5 years of follow-up among brisk and moderate speed walkers. Additionally, we did not find that the intraindividual slope of BP over 5 years contributed importantly to cardiovascular risk in this well-functioning cohort of older adults. Future research should account for heterogeneity in functional status when evaluating the impact of BP in older adults.
Supplementary Material
Please visit the article online at http://gerontologist.oxfordjournals.org/ to view supplementary material.
Funding
The Health ABC study was supported by National Institute on Aging (NIA) Contracts N01-AG-6-2101; N01-AG-6-2103; N01-AG-6-2106; NIA grant R01-AG028050; and NINR grant R01-NR012459, and in part by the Intramural Research Program of the NIH, NIA. Additional support for this research was provided by NIA (K01AG039387, R01AG46206).
Supplementary Material
References
- 1. Odden MC, Covinsky KE, Neuhaus JM, Mayeda ER, Peralta CA, Haan MN. The association of blood pressure and mortality differs by self-reported walking speed in older Latinos. J Gerontol A Biol Sci Med Sci. 2012;67:977–983. doi:10.1093/gerona/glr245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Odden MC, Peralta CA, Haan MN, Covinsky KE. Rethinking the association of high blood pressure with mortality in elderly adults: the impact of frailty. Arch Intern Med. 2012;172:1162–1168. doi:10.1001/archinternmed.2012.2555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Sabayan B, van Vliet P, de Ruijter W, Gussekloo J, de Craen AJ, Westendorp RG. High blood pressure, physical and cognitive function, and risk of stroke in the oldest old: the Leiden 85-plus Study. Stroke. 2013;44:15–20. doi:10.1161/STROKEAHA.112.663062 [DOI] [PubMed] [Google Scholar]
- 4. Sabayan B, Oleksik AM, Maier AB, et al. High blood pressure and resilience to physical and cognitive decline in the oldest old: the Leiden 85-plus Study. J Am Geriatr Soc. 2012;60:2014–2019. doi:10.1111/j.1532-5415.2012.04203.x [DOI] [PubMed] [Google Scholar]
- 5. Peralta CA, Katz R, Newman AB, Psaty BM, Odden MC. Systolic and diastolic blood pressure, incident cardiovascular events, and death in elderly persons: the role of functional limitation in the Cardiovascular Health Study. Hypertension. 2014;64:472–480. doi:10.1161/HYPERTENSIONAHA.114.03831 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Allen NB, Siddique J, Wilkins JT, et al. Blood pressure trajectories in early adulthood and subclinical atherosclerosis in middle age. JAMA. 2014;311:490–497. doi:10.1001/jama.2013.285122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Satish S, Zhang DD, Goodwin JS. Clinical significance of falling blood pressure among older adults. J Clin Epidemiol. 2001;54:961–967. [DOI] [PubMed] [Google Scholar]
- 8. Poortvliet RK, de Ruijter W, de Craen AJ, et al. Blood pressure trends and mortality: the Leiden 85-plus Study. J Hypertens. 2013;31:63–70. doi:10.1097/HJH.0b013e32835aa351 [DOI] [PubMed] [Google Scholar]
- 9. Studenski S, Perera S, Patel K, et al. Gait speed and survival in older adults. JAMA. 2011;305:50–58. doi:10.1001/jama.2010.1923 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Nagin DS. Analyzing developmental trajectories: a semiparametric, group-based approach. Psychol Method. 1999;4:139. [DOI] [PubMed] [Google Scholar]
- 11. Nagin D. Group-based Modeling of Development. Boston, MA: Harvard University Press; 2005. [Google Scholar]
- 12. Gao S, Hendrie HC, Wang C, et al. Redefined blood pressure variability measure and its association with mortality in elderly primary care patients. Hypertension. 2014;64:45–52. doi:10.1161/HYPERTENSIONAHA.114.03576 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Butt DA, Mamdani M, Austin PC, Tu K, Gomes T, Glazier RH. The risk of hip fracture after initiating antihypertensive drugs in the elderly. Arch Intern Med. 2012;172:1739–1744. doi:10.1001/2013.jamainternmed.469 [DOI] [PubMed] [Google Scholar]
- 14. Tinetti ME, Han L, Lee DS, et al. Antihypertensive medications and serious fall injuries in a nationally representative sample of older adults. JAMA Intern Med. 2014;174:588–595. doi:10.1001/jamainternmed.2013.14764 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Muller M, Smulders YM, de Leeuw PW, Stehouwer CD. Treatment of hypertension in the oldest old: a critical role for frailty? Hypertension. 2014;63:433–441. doi:10.1161/HYPERTENSIONAHA.113.00911 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.