Abstract
Context
Medication drug exposures among young children continue to rise despite current poison prevention efforts. These exposures result in increased healthcare utilization and medical costs. New tactics are needed to reduce injuries related to pediatric drug exposures.
Objective
We aimed to identify cluster patterns in 1) calls for pediatric medication drug exposures and 2) a subset of calls that resulted in medical evaluation referrals. We identified and evaluated population characteristics associated with cluster patterns.
Methods
We analyzed 26,685 pharmaceutical drug exposures involving children less than 5 years of age based on calls reported to the Pittsburgh Poison Center from January 1, 2006 to December 31, 2010. We performed spatial statistics to assess for clustering. We used logistic regression was used to estimate population characteristics associated with clustering.
Results
Spatial analysis identified 22 exposure clusters and 5 referral clusters. 65% of 89 ZIP codes in the clusters of drug exposure with HCF referral were not identified in the exposure clusters. ZIP codes in the HCF referral clusters were characterized as rural, impoverished, and with high rates of unemployment and school dropouts.
Discussion
Our principal findings demonstrate pediatric drug exposures do exist in discrete geographic clusters and with distinct socioeconomic characteristics.
Conclusion
This study offers a starting point for subsequent investigations into the geographic and social context of pediatric medication drug exposures. This is an important step in revising pediatric poison prevention strategies.
Keywords: spatial analysis, GIS, injury prevention, socioeconomic
INTRODUCTION
Over the last century, American childhood deaths associated with accidental poisoning had been significantly reduced. Recent reports, however, indicate that not only are pediatric drug exposures on the rise, but the associated clinical outcomes are worsening in severity. These medication exposures ultimately result in increased healthcare utilization. 1–5 Poisoning is one of the top reasons for Emergency Department (ED) visits in the 1 to 5 year age group in the United States(US).6 Due to their exploratory nature, children in this age group are particularly vulnerable to unintentional self-exposures.7,8 New prevention strategies are required to reduce drug exposures and to decrease the associated healthcare burden.9,10 Identification of medication poisoning locations and understanding the communities at risk for injury is essential to revising prevention strategies. Geographic information systems (GIS) is a computerized platform designed to collect, manage, and analyze spatial and non-spatial data. 11.Public health campaigns have utilized GIS and spatial scan statistics to assess regional variation in substance abuse prevalence, alcohol related injury, as well as to plan and assess the impact of preventive interventions in childhood lead poisoning. 12–14
A critical gap exists in the literature regarding geographic trends and population characteristics of unintentional, drug exposures in children. In this study, we use poison center data, United States (US) Census information and spatial statistics to assess regional patterns of drug exposure in children < 5 years. The purpose of this study was to assess regional pharmaceutical poisoning rates, identify locations and populations at risk for injury, and determine geographic variations in the poisoning injury resulting in health services utilization. We hypothesized that drug exposures exist in clusters and are not randomly distributed over space. We performed a spatial analysis on all calls to the poison center regarding pediatric drug exposure and on the subset of calls that resulted in referrals for medical evaluation. We then compared population characteristics of ZIP codes with and without cluster patterns.
METHODS
Data Collection
The Pittsburgh Poison Center is the referral center for western Pennsylvania and covers 51 counties and a population of 5.9 million people. Data from phone calls are recorded in real time with a standardized electronic format and can serve as a surveillance system for pediatric drug exposure. We queried original data from the Pittsburgh Poison Center and searched for records meeting the following criteria: exposures in children < 5 years, call-types originating from non-healthcare facilities, and events occurring between January 1, 2006 and December 31st, 2010. Analysis of these records was limited to children with an unintentional exposure to a pharmaceutical agent. Unintentional exposures that resulted from a therapeutic error (i.e. caregivers giving a medication too frequently or in excess of recommended dosing) and adverse effects were excluded. We chose the 2006-2010 period as it corresponded to US Census collection of demographic data, in particular, the number of children by age group. We excluded records if the reported ZIP codes were located outside of Pennsylvania or if the US Census reported no children < 5 years. The primary outcome was the classification of a ZIP code in a cluster of drug exposure, (exposure cluster).
When a call regarding an exposure was placed to the poison center, a poison center specialist assessed the clinical signs, symptoms, and substance with a pre-determined practice guideline. If the exposure was deemed concerning, the specialist referred the child to a healthcare facility (HCF) for a medical evaluation. Occasionally, the poison center received a call when the child’s caregivers self-referred for a medical evaluation and were already en-route to a HCF. We grouped both of these referral types in the category of drug exposure with HCF referral (referral cluster).
Spatial Data Preparation
We used ArcGIS 10.2 Software (Esri Inc., Redlands, CA) to geocode (map) all calls according to the five digit ZIP codes reported to the Pittsburgh Poison Center by the caller at the time of the exposure. We created an incidence rate map for 1) all drug exposures and 2) the subset of drug exposures resulting in HCF referrals. The denominator for these incidence rates was the total population of children < 5 years in the respective ZIP code as reported by the US Census. We downloaded ZIP code shapefiles from ArcGIS Online and obtained demographic variables from 2006-2010 US Census summary files. We apportioned demographic variables to the ZIP code level. To characterize a ZIP code as urban or rural, we superimposed US Census urban shapefiles were superimposed on ZIP code centroids (centers). ZIP codes with centroids that fell within the urban area were designated as urban, while those that did not were characterized as a rural.
Spatial Analysis
We applied the spatial scan statistic in SatScan v9.3 (Kulldorff M. and Information Management Services, Inc, www.satscan.org) to identify nonrandom clusters. For this study, the null hypothesis assumed drug exposures were randomly distributed in geographic space and expected exposure counts were proportional to the population at risk. Using a Poisson-based model and adjusting for the underlying spatial inhomogeneity of the background population, the statistic placed a circular scanning window at each location and calculated the number of observed and expected observations both in and outside the window. The area with the maximum likelihood was designated the primary cluster; in other words, the most likely cluster and the least likely to have occurred by chance. A cluster with p-value <0.05 was considered to be statistically significant. 15,16 A circular scanning window was placed at different coordinates with maximum size set to contain 50%, 40%, 30%, 20%, 10% and 5% of the population at risk. The statistic performed 999 simulations and did not allow overlapping clusters.
Population Characteristics Analysis
We performed descriptive statistics to characterize the demographics of the sample region. We applied the chi-squared test to compare categorical variables and the Mann-Whitney U test to compare non-parametric continuous variables. We performed a backwards stepwise logistic regression in SPSS (Armonk, NY) to calculate odds ratios (ORs) for the association of population characteristics with clusters of drug exposure and clusters of drug exposure associated with HCF. The variables used in these models included education, poverty, unemployment, race, household size, income, women head of household, population density and the classification of a ZIP code as urban. The education variable is reported as the percentage of the population without a high school diploma and is a reflection of the high school dropout rate. Selection of these variables was based on plausible associations with drug exposure. Variables associated with the outcome in unadjusted bivariate analyses were selected by using a backward elimination logistic regression model. An iterative process was used to assess for multicollinearity. Education, poverty, unemployment, race, household size, income, women head of household, and population density were ranked in tertiles. Insignificant variables (p>0.2) were eliminated from the model. The Hosmer-Lemeshow test was used to assess model fit. University of Pittsburgh’s Institutional Review Board granted approval for this study.
RESULTS
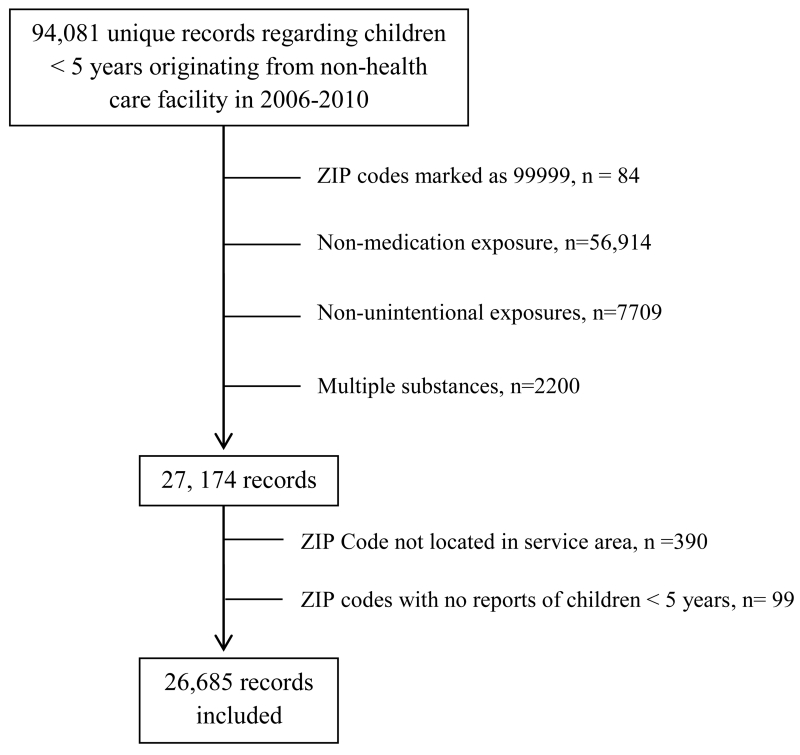
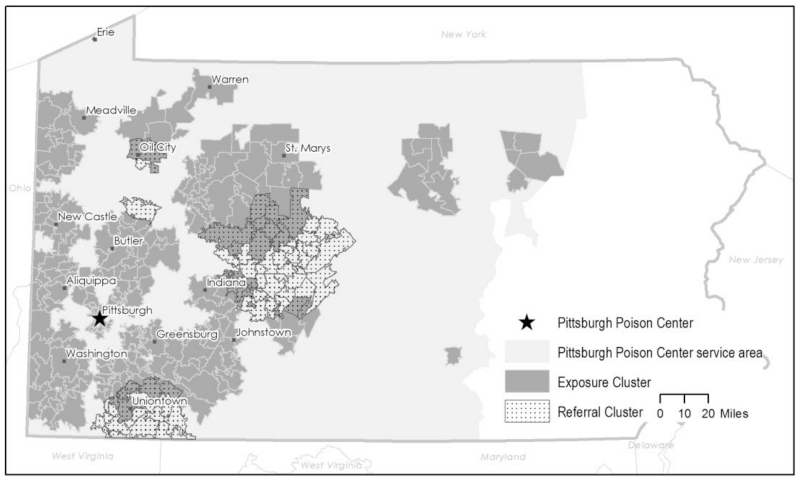
From January 1st, 2006 to December 31st, 2010, there were 94,081 unique records involving children < 5 years reported to the Pittsburgh Poison Center from a non-healthcare facility (Figure 1). There were 390 calls from outside the service area; 99 calls were located in 20 ZIP codes where no children < 5 years were reported by 2010 US Census. The final sample included 26,685 exposures with 877 drug exposures resulting in HCF referral (Table 1). The study area included 280,855 children < 5 years across 873 ZIP Codes. A scanning window set at 50% identified a large primary cluster occupying a large portion of southwest Pennsylvania. By restricting the window size to 5%, smaller clusters were identified with minimum risk of missing significant regional-level clusters. We identified 22 exposure clusters and 5 referral cluster (Figure 2). The primary cluster from each of these samples was identified in distinctly different geographic regions; the primary exposure cluster was located in Warren, PA (RR=1.7), while the primary HCF referral cluster was identified in Erie, PA (RR=37.5). While 9.5% of the 324 ZIP codes in the exposure cluster were also identified in a referral cluster (n = 31), 65% of 89 ZIP codes in referral clusters were not initially identified in the exposure clusters, demonstrating minimally overlapping geographic pattern (n =58).
Figure 1.
Flowchart of record selection process.
Table 1. Unintentional Drug Exposures for Children < 5 Years, Pittsburgh Poison Center, 2006-2010.
| Total Exposures | 26,685 |
| Ages | n, (%) |
| 0-6 months | 218 (0.8) |
| 7-12 months | 2253 (8.4) |
| 13-24 months | 17,536 (65.7) |
| 25 to <60 months | 6,678 (25.0) |
| Sex | |
| Female | 12,850 (48.2) |
| Male | 13,833 (51.8) |
| Unknown | 2 (<0.1) |
| Substance Number | |
| Single drug exposure | 25,757 (96.5) |
| Multiple drug exposure | 928 (3.5) |
| Case Management | |
| Managed on site (no medical evaluation necessary) | 25,788 (96.6) |
| Poison center specialist referred to health care facility | 772 (2.9) |
| Self-referred to health care facility | 105 (0.4) |
| Other/Unknown | 20 (0.1) |
Figure 2. Cluster Patterns of Pediatric Drug Exposures, Pittsburgh Poison Center, 2006-2010.
Spatial analysis demonstrates distinct exposure clusters and referral clusters. p<0.05 for all clusters.
ZIP codes within exposure clusters were urban and more densely populated compared to ZIP codes not in an exposure cluster (Table 2). These ZIP codes were also statistically different in terms of median household size, educational attainment, and women head of household; the results from the regression analysis are depicted in Table 3.
Table 2. Population Characteristics of ZIP Codes With and Without Geographic Clustering.
| Calls for Drug Exposure | Calls for Drug Exposure With Healthcare Facility Referral |
|||||
|---|---|---|---|---|---|---|
|
|
||||||
| Cluster | No Cluster |
p | Cluster | No Cluster |
p | |
| ZIP Codes, n | 324 | 549 | 89 | 784 | ||
| Household size | 2.36 | 2.45 | <.001 | 2.42 | 2.41 | 0.25 |
| Income | $33,846 | $34,653 | 0.28 | $29,545 | $35,002 | <.001 |
| No high school diploma, % | 12 | 13 | <.001 | 15 | 12 | <.001 |
| Non White, % | 2.2 | 2.0 | 0.42 | 1.6 | 2.1 | <.001 |
| Population per square mile | 200.6 | 79.8 | <.001 | 81.2 | 110.1 | 0.12 |
| Poverty, % | 10 | 10 | 0.19 | 13 | 10 | <.001 |
| Unemployed, % | 7 | 7 | 0.71 | 9 | 7 | <.001 |
| Urban*, % | 66.7 | 52.7 | <.001 | 43.8 | 59.4 | 0.005 |
| Women head of household, % | 14 | 13 | <.001 | 14 | 13 | 0.76 |
Table 3. Association Between Population Characteristics and Clusters.
| Population Characteristic | Exposure Cluster | Referral Cluster | ||
|---|---|---|---|---|
|
| ||||
| OR (95%CI) | P value | OR (95%CI) | P value | |
| Population density | 1.67 (1.34-2.01) | <.001 | ... | |
| No high school diploma | 0.78 (0.64-0.94) | 0.01 | ... | |
| Household size | 0.56 (0.46-0.68) | <.001 | 1.4 (1.01-1.96) | 0.04 |
| Non-White | 0.64 (0.52-0.79) | <.001 | 0.72 (0.53-0.99) | 0.04 |
| Unemployment | ... | 3.2 (2.2-4.7) | <.001 | |
| Income | ... | 0.34 (0.23-0.51) | <.001 | |
Notes. CI, confidence interval; OR, odds ratio. Both models included poverty, women head of household and urban classification as covariates. Ellipses indicate covariates not included in final model. Hosmer-Lemeshow goodness-of-fit p values were 0.58 and 0.03 respectively.
DISCUSSION
We hypothesized pediatric drug exposures exist in clusters and are not randomly distributed across western Pennsylvania. Our principal findings demonstrate pediatric drug exposures do, in fact, exist in distinct geographic patterns. Moreover, ZIP codes in referral clusters were geographically distinct from the exposure clusters and were characterized as largely rural, impoverished, and with high unemployment and school dropout rates.
These results have significant implications as they provide a starting point for further investigation into the relationship between location and the social environment of children with unintentional drug poisoning. While previous studies have applied spatial analysis to understand patterns in adult prescription drug use, we found a dearth of studies using spatial techniques to investigate geographic patterns of medication poisoning in children.17–20 Moreover, there is a critical gap in our understanding of the socioeconomic context of American childhood poisoning.21–24 This investigation’s demographic characterization offers some first insights to the socio-economic context of American childhood poisoning. The regression model indicates population density had a moderate effect on a ZIP code falling within an exposure cluster while education status appears to have a small effect. These findings are consistent with previous studies identifying population density as a positive predictor of poison center utilization, while less educated populations are associated with a decrease in poison center utilization. Poison center utilization is influenced by poison center awarenesss.30 In more densely populated and more educated communities, knowledge of poison center service may proliferate more easily, resulting in the increase of a population’s awareness of poison center services. This may translate into more calls regarding drug exposures.
International literature has investigated the relationship of socioeconomic disparity and childhood poisoning.25,26 In the United Kingdom, children from lower socioeconomic status were at greater risk of death associated with poisoning when compared to children from more affluent status. Lower socioeconomic status may be a surrogate marker of suboptimal child supervision which might result in neglect and increased child injury.27–29 Our findings suggest a similar relationship may exist in impoverished, rural American communities with high unemployment and school dropout rates.
This study offers a novel strategy in closing this gap in the poison prevention literature. Understanding where clusters exist at a local level offers target areas for revised prevention strategies. For example, within these high risk areas, poison injury resources may be dispensed at the point-of-sale of prescription medications. Professional associations might create promotional campaigns to educate pharmacists in directing customers to keep medications in original child-resistant containers; pediatricians can be prompted to discuss poison prevention tactics with families of young children living in identified cluster areas. Neighborhood and community social networks in high risk areas can be encouraged to organize “Take Back Medications” campaigns to safely and properly dispose of prescription medications. Drug exposure and drug poisoning cluster identification can also be useful to health departments by providing a means to measure the impact and performance of any poison intervention programs.
An important concept to consider is that the data sampled are from phone calls placed to the poison center; these calls may not necessarily reflect true exposure incidence, but rather a population’s utilization of poison center services. Decreased poison center utilization has been associated with increased healthcare utilization. Moreover, poison center underutilization in rural areas is believed to be associated with increased hospitalization.31,32 Our findings support a similar pattern; if exposure clusters serve as a proxy for poison center utilization, then there exists a distinct pattern of referral clusters in rural communities, outside of these areas of high poison center use. Poison Center specialists do not consider proximity to a health care facility in the decision to refer a child for a medical evaluation. Specialists gather information based on pre-determined criteria and refer when clinical concern is high. In order to gain insight on this geographic disparity, future research will investigate potential differences in the type of medications that urban and rural children are exposed to.
While identifying locations of high rates for exposure allows important characterization of population attributes associated with increased poison center awareness, the locations with low rates are also of interest. Studies have indicated increased poison center utilization is associated with reductions in ED visits and hospital admissions as poison center specialists may facilitate safe medical management of low-risk poison exposures at home.32,33 Therefore, raising poison center awareness in the ZIP codes in low rate cluster locations may lead to reductions in healthcare costs associated with unnecessary medical evaluations. Past efforts to raise poison center awareness such as mass media mailings, however, have been challenging and expensive.34–36 A cost-effective strategy may be to use spatial analysis to perform a community-based assessment to identify communities within low utilization clusters.
Limitations
These results offer evidence of geographic patterns in calls placed to a single regional poison center. While it is unknown whether these findings are generalizable across populations, this technique may be easily applied to other regional centers. It is also important to note the geographic scale in this analysis. Due to privacy concerns, poison centers do not record street addresses. Inferences should be interpreted with caution as ZIP codes contain inherent socioeconomic heterogeneity, suggesting an ecologic bias. Nonetheless, this information remains relevant as it provides insight to the location and environmental risk factors surrounding pediatric drug exposures. Moreover, injury prevention strategies are often aimed at aggregate areas of at-risk individuals, such as ZIP codes. The impact of these interventions is often measured in geopolitical units (e.g. rate reductions per ZIP code). Therefore, in this case, the ecological bias becomes less concerning.
Another caveat to consider is the poison center data does not capture all drug exposures. This reporting bias may be the product of limitations in access (e.g., no telephone), lack of awareness of the poison center, poisoning severity (emergency calls are placed to 911 rather than the poison center) and language barriers. In this study, we aimed to characterize the population at the origin of exposure; thus, reports from healthcare facilities were excluded from this analysis since the ZIP code associated with these calls do not necessarily reflect the location of the exposure. Therefore, our data may underestimate the true occurrence of drug exposures and the associated healthcare utilization.
For time period of this study, approximately 2.6% calls PPC accepted were from outside the PPC service area. These calls were largely cellphones from all over the country. These calls were random and not necessarily areas adjacent to the service area. 1.5% of calls were misrouted to another poison center. While a limitation, these numbers are small and are unlikely to significantly impact our results.
In terms of cluster identification, there exist several techniques and no single technique is identified as the gold standard. The SatScan technique is popular as it is freely available and is relatively easy to use. It is limited in that it may not detect “holes”, or areas that may not be clusters, within the clusters. It is also dependent on the user’s designation of window size. By designating a smaller window size, users may be too restrictive and miss potential clusters. While our data demonstrate certain variables increase the odds for potential clustering, the analysis does not imply causality.
CONCLUSIONS
We conclude that drug exposure and drug exposure with HCF referral exist in distinct geographical clusters. ZIP codes identified within these clusters have specific population characteristics. This study offers a starting point for subsequent investigations into the geographical and social patterns of pediatric drug exposures and associated healthcare utilization.
Acknowledgments
Funding Source: The project was supported by the University of Pittsburgh Clinical and Translational Science Institute (CTSI) through the National Institutes of Health through Grant Number UL1TR000005.
Footnotes
Financial Disclosures: The authors have no financial relationships to disclose relevant to this article.
Conflicts of Interests: The authors have no conflicts of interests to disclose relevant to this article.
Contributor’s Statement Page:
Margaret Nguyen, MD: conceptualized and designed the study, performed data collection, data processing, geospatial analysis and interpretation, drafted the initial manuscript, made revisions to the manuscript and approved the final manuscript as submitted.
Anthony Pizon, MD: Dr. Pizon contributed to the data collection, participated in data analysis and interpretation and made critical revisions to the manuscript.
Charles Branas, PhD: Dr. Branas contributed to the design of the spatial analysis, participated in data analysis and interpretation, made critical revisions to the manuscript, and approved the final manuscript as submitted.
Anthony Fabio, PhD: Dr. Fabio contributed to the design of the study, participated in data analysis and interpretation, made critical revisions to the manuscript, and approved the final manuscript as submitted.
DECLARATION OF INTEREST
The authors report no declarations of interest.
References
- 1.Bond GR, Woodward RW, Ho M. The Growing Impact of Pediatric Pharmaceutical Poisoning. J Pediatr. 2012 Feb;160(2):265–70. e1. doi: 10.1016/j.jpeds.2011.07.042. [DOI] [PubMed] [Google Scholar]
- 2.Setlik J, Ho M, Bond GR. Emergency department use after pediatric pharmaceutical ingestion: comparison of two national databases. Clin Toxicol Phila Pa. 2010 Jan;48(1):64–7. doi: 10.3109/15563650903397234. [DOI] [PubMed] [Google Scholar]
- 3.Schillie SF, Shehab N, Thomas KE, Budnitz DS. Medication Overdoses Leading to Emergency Department Visits Among Children. Am J Prev Med. 2009 Sep;37(3):181–7. doi: 10.1016/j.amepre.2009.05.018. [DOI] [PubMed] [Google Scholar]
- 4.Lovegrove MC, Mathew J, Hampp C, Governale L, Wysowski DK, Budnitz DS. Emergency Hospitalizations for Unsupervised Prescription Medication Ingestions by Young Children. Pediatrics. 2014 Oct 1;134(4):e1009–16. doi: 10.1542/peds.2014-0840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Spiller HA, Beuhler MC, Ryan ML, Borys DJ, Aleguas A, Bosse GM. Evaluation of changes in poisoning in young children: 2000 to 2010. Pediatr Emerg Care. 2013 May;29(5):635–40. doi: 10.1097/PEC.0b013e31828e9d00. [DOI] [PubMed] [Google Scholar]
- 6.National Center for Injury Prevention and Control. Centers for Disease Control and Prevention (producer) National Estimates of the 10 Leading Causes of Nonfatal Injuries Treated in Hospital Emergency Departments, United States – 2011. Centers for Disease Control and Prevention. Web-based Injury Statistics Query and Reporting System (WISQARS); [Online]. [Internet]. 2011 [cited 2013 Jan 15]. Available from: www.cdc.gov/ncipc/wisqars. [Google Scholar]
- 7.Franklin RL, Rodgers GB. Unintentional Child Poisonings Treated in United States Hospital Emergency Departments: National Estimates of Incident Cases, Population-Based Poisoning Rates, and Product Involvement. Pediatrics. 2008 Dec 1;122(6):1244–51. doi: 10.1542/peds.2007-3551. [DOI] [PubMed] [Google Scholar]
- 8.Schoenewald S, Ross S, Bloom L, Lin L, Patel M, Shah M, Lynch J, Kuffner E. New Insights into Root Causes of Accidental Unsupervised Ingestions (AUIs) of Over-the-Counter (OTC) Medications. Clin Toxicol. 2009 Sep;47:702–65. doi: 10.3109/15563650.2013.855314. 2009 47 702–765. [DOI] [PubMed] [Google Scholar]
- 9.Budnitz DS, Lovegrove MC. The Last Mile: Taking the Final Steps in Preventing Pediatric Pharmaceutical Poisonings. J Pediatr. 2012 Feb;160(2):190–2. doi: 10.1016/j.jpeds.2011.09.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Budnitz DS, Salis S. Preventing Medication Overdoses in Young Children: An Opportunity for Harm Elimination. Pediatrics. 2011 Jun 1;127(6):e1597–9. doi: 10.1542/peds.2011-0926. [DOI] [PubMed] [Google Scholar]
- 11.Bell N, Schuurman N. GIS and Injury Prevention and Control: History, Challenges, and Opportunities. Int J Environ Res Public Health. 2010 Mar;7(3):1002–17. doi: 10.3390/ijerph7031002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sudakin D, Power LE. Regional and temporal variation in methamphetamine-related incidents: applications of spatial and temporal scan statistics. Clin Toxicol. 2009 Mar;47(3):243–7. doi: 10.1080/15563650802516160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gruenewald PJ, Freisthler B, Remer L, LaScala EA, Treno A. Ecological models of alcohol outlets and violent assaults: crime potentials and geospatial analysis. Addiction. 2006;101(5):666–77. doi: 10.1111/j.1360-0443.2006.01405.x. [DOI] [PubMed] [Google Scholar]
- 14.The Childhood Lead Poisoning Prevention Program Geographic Information System Workgroup Using GIS to Assess and Direct Childhood Lead Poisoning Prevention. Guidance for State and Local Childhood Lead Poisoning Prevention Programs [Internet] 2004 [cited 2013 Feb 3]. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1497528/pdf/12766217.pdf.
- 15.Kulldorff M. Communications in Statistics: Theory and Methods. A spatial scan statistic. [Google Scholar]
- 16.Kulldorff M, Huang L, Pickle L, Duczmal L. An elliptic spatial scan statistic. Stat Med. 2006 Nov 30;25(22):3929–43. doi: 10.1002/sim.2490. [DOI] [PubMed] [Google Scholar]
- 17.Dasgupta N, Davis J, Jonsson Funk M, Dart R. Using Poison Center Exposure Calls to Predict Methadone Poisoning Deaths. PLoS ONE [Internet] 2012 Jul 19;7(7) doi: 10.1371/journal.pone.0041181. cited 2014 Mar 5. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3400615/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Brownstein JS, Green TC, Cassidy TA, Butler SF. Geographic Informations Systems and Pharmacoepidemiology: Using spatial cluster detection to monitor local patterns of prescription opioid abuse. Pharmacoepidemiol Drug Saf. 2010 Jun;19(6):627–37. doi: 10.1002/pds.1939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Green TC, Grau LE, Carver HW, Kinzly M, Heimer R. Epidemiologic trends and geographic patterns of fatal opioid intoxications in Connecticut, USA: 1997 - 2007. Drug Alcohol Depend. 2011 Jun 1;115(3):221–8. doi: 10.1016/j.drugalcdep.2010.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nkhoma ET, Ed Hsu C, Hunt VI, Harris AM. Detecting spatiotemporal clusters of accidental poisoning mortality among Texas counties, U.S., 1980 - 2001. Int J Health Geogr. 2004 Oct 27;3:25. doi: 10.1186/1476-072X-3-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Uziel Y, Adler A, Aharonowitz G, Franco S, Fainmesser P, Wolach B. Unintentional childhood poisoning in the Sharon area in Israel: a prospective 5-year study. Pediatr Emerg Care. 2005 Apr;21(4):248–51. [PubMed] [Google Scholar]
- 22.Flanagan RJ, Rooney C, Griffiths C. Fatal poisoning in childhood, England & Wales 1968–2000. Forensic Sci Int. 2005 Mar;148(2-3):121–9. doi: 10.1016/j.forsciint.2004.04.083. [DOI] [PubMed] [Google Scholar]
- 23.Roberts I. Cause specific social class mortality differentials for child injury and poisoning in England and Wales. J Epidemiol Community Health. 1997 Jun 1;51(3):334–5. doi: 10.1136/jech.51.3.334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bailey JE, Campagna E, Dart RC, RADARS System Poison Center Investigators The underrecognized toll of prescription opioid abuse on young children. Ann Emerg Med. 2009 Apr;53(4):419–24. doi: 10.1016/j.annemergmed.2008.07.015. [DOI] [PubMed] [Google Scholar]
- 25.Alwash R, McCarthy M. Accidents in the home among children under 5: ethnic differences or social disadvantage? BMJ. 1988 May 21;296(6634):1450–3. doi: 10.1136/bmj.296.6634.1450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sibert R. Stress in families of children who have ingested poisons. Br Med J. 1975 Jul 12;3(5975):87–9. doi: 10.1136/bmj.3.5975.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zielinski DS. Child maltreatment and adult socioeconomic well-being. Child Abuse Negl. 2009 Oct;33(10):666–78. doi: 10.1016/j.chiabu.2009.09.001. [DOI] [PubMed] [Google Scholar]
- 28.Gillham B, Tanner G, Cheyne B, Freeman I, Rooney M, Lambie A. Unemployment rates, single parent density, and indices of child poverty: Their relationship to different categories of child abuse and neglect. Child Abuse Negl. 1998 Feb;22(2):79–90. doi: 10.1016/s0145-2134(97)00134-8. [DOI] [PubMed] [Google Scholar]
- 29.Hapgood R, Kendrick D, Marsh P. How well do socio-demographic characteristics explain variation in childhood safety practices? J Public Health. 2000 Sep 1;22(3):307–11. doi: 10.1093/pubmed/22.3.307. [DOI] [PubMed] [Google Scholar]
- 30.Litovitz T, Benson BE, Youniss J, Metz E. Determinants of U.S. poison center utilization. Clin Toxicol Phila Pa. 2010 Jun;48(5):449–57. doi: 10.3109/15563651003757947. [DOI] [PubMed] [Google Scholar]
- 31.LoVecchio F, Curry SC, Waszolek K, Klemens J, Hovseth K, Glogan D. Poison control centers decrease emergency healthcare utilization costs. J Med Toxicol. 2008 Dec;4(4):221–4. doi: 10.1007/BF03161204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zaloshnja E, Miller T, Jones P, Litovitz T, Coben J, Steiner C, et al. The Potential Impact of Poison Control Centers on Rural Hospitalization Rates for Poisoning. Pediatrics. 2006 Nov 1;118(5):2094–100. doi: 10.1542/peds.2006-1585. [DOI] [PubMed] [Google Scholar]
- 33.Zaloshnja E, Miller T, Jones P, Litovitz T, Coben J, Steiner C, et al. The impact of poison control centers on poisoning-related visits to EDs—United States, 2003. Am J Emerg Med. 2008 Mar;26(3):310–5. doi: 10.1016/j.ajem.2007.10.014. [DOI] [PubMed] [Google Scholar]
- 34.Krenzelok EP, Mrvos R. Is mass-mailing an effective form of passive poison center awareness enhancement? Vet Hum Toxicol. 2004 Jun;46(3):155–6. [PubMed] [Google Scholar]
- 35.Everson G, Rondeau ES, Kendrick M, Garza I. Ineffectiveness of a mass mailing campaign to improve poison center awareness in a rural population. Vet Hum Toxicol. 1993 Apr;35(2):165–7. [PubMed] [Google Scholar]
- 36.Yudizky M, Grisemer P, Shepherd G, Ray M, Garrison J. Can textbook covers be used to increase poison center utilization? Vet Hum Toxicol. 2004 Oct;46(5):285–6. [PubMed] [Google Scholar]