Abstract
Background
The postpartum period represents a major transition in the lives of many women, a time when women are at increased risk for the emergence of psychopathology including depression and PTSD. The current study aimed to better understand the unique contributions of clinically significant postpartum depression, PTSD, and comorbid PTSD/depression on mother–infant bonding and observed maternal parenting behaviors (i.e., behavioral sensitivity, negative affect, positive affect) at 6 months postpartum.
Methods
Mothers (n=164; oversampled for history of childhood maltreatment given parent study's focus on perinatal mental health in women with trauma histories) and infants participated in 6-month home visit during which dyads engaged in interactional tasks varying in level of difficulties. Mothers also reported on their childhood abuse histories, current depression/PTSD symptoms, and bonding with the infant using standardized and validated instruments.
Results
Mothers with clinically significant depression had the most parenting impairment (self-report and observed). Mothers with clinically significant PTSD alone (due to interpersonal trauma that occurred predominately in childhood) showed similar interactive behaviors to those who were healthy controls or trauma-exposed but resilient (i.e., no postpartum psychopathology). Childhood maltreatment in the absence of postpartum psychopathology did not infer parenting risk.
Limitations
Findings are limited by (1) small cell sizes per clinical group, limiting power, (2) sample size and sample demographics prohibited examination of third variables that might also impact parenting (e.g., income, education), (3) self-report of symptoms rather than use of psychiatric interviews.
Conclusions
Findings show that in the context of child abuse history and/or current PTSD, clinically significant maternal depression was the most salient factor during infancy that was associated with parenting impairment at this level of analysis.
Keywords: Depression, Post-traumatic stress disorder, Postpartum period, Parenting
1. Introduction
The postpartum period represents a major transition in the lives of many women, a time of increased risk for the emergence of psycho-pathology (Ross and McLean, 2006; Studd and Nappi, 2012). Prevalence rates for postpartum depression or post traumatic stress disorder (PTSD) are relatively high, with estimates varying between 9% and 19% for depression (O'Hara and McCabe, 2013) and 3.6% and 15% for PTSD (Alcorn et al., 2010). Furthermore, comorbid depression and PTSD is common; findings from the National Comorbidity Survey show that 24.7% of depressed women also have PTSD, and 48.4% of women with PTSD also suffer depression.
These data are concerning because, relative to women with depression alone, women with comorbid PTSD exhibit more severe symptoms and are functionally more impaired (Cerulli et al., 2011; Kessler et al., 1995; Loveland Cook et al., 2004; Smith et al., 2006). During the postpartum period, mothers’ psychopathology and functional impairment may detrimentally impact parenting and child outcomes. Abundant literature has shown that postpartum depression is associated with intrusive or disengaged parenting, (Lovejoy et al., 2000; O'Hara and McCabe, 2013) and that affected children exhibit worse biopsychosocial outcomes (Davalos et al., 2012; Deave et al., 2008). Less is known about the impact of postpartum PTSD on parenting attitudes and behaviors. Given high rates of comorbidity, it is also unclear whether the potential impact of PTSD on parenting is unique, or whether it can be explained by co-occurring depression.
Prior work indicates that women with childhood maltreatment histories may be particularly vulnerable to developing clinically significant postpartum depression (Buist, 1998; Lev-Wiesel et al., 2009) and/or PTSD (Edwards et al., 2003; Koenen and Widom, 2009). Postpartum experiences (including childbirth itself; Grekin and O’Hara, 2014) may trigger recollection of past trauma and heighten symptoms (Onoye et al., 2013). Women with childhood maltreatment histories are also at increased risk for parenting problems. Indeed, the concept of “intergenerational transmission of risk” frames much of the literature on trauma and parenting, and in some studies, estimates for risk among mothers who were maltreated as children to parent their infant in an abusive or neglectful manner are as high as 70% (DiLillo, 2001; Egeland et al., 1988).
Moreover, maternal cumulative trauma is linked to decreased parenting satisfaction, reports of child neglect, increased use of physical punishment, higher child abuse potential, and a history of protective service involvement (Banyard et al., 2003). Indeed, several studies show that children of mothers with PTSD, alone or comorbid with depression, have worse outcomes including greater exposure to traumatic life events and psychological abuse (Chemtob et al., 2013) and more aggressive and emotionally reactive behavior problems (Chemtob et al., 2010a). Further, maternal PTSD effects on child emotion regulation already are evident in infancy (Bosquet Enlow et al., 2011). In fact, one study suggests that children of mothers with comorbid PTSD and depression display more clinically significant internalizing and externalizing behavior problems than children of mothers with depression alone (Chemtob et al., 2010a). Given these negative child developmental outcomes, the question arises whether maternal PTSD has unique parenting correlates that would explain this heightened risk.
The present study seeks to better understand the effects of postpartum depression and PTSD symptoms on parenting in the first six months postpartum. Three domains of parenting: were evaluated: maternal perceptions of mother–infant bonding impairment (to capture the subjective quality of mother–child relationship), and two measures of observed parenting: behavioral sensitivity (a parenting style marked by empathic and sensitive responding), and maternal positive and negative emotional displays. In prior research, all three parenting domains are associated with maternal depressive symptoms and child outcomes (Denham et al., 2000; Feldman, 2007; Lovejoy et al., 2000; Mäntymaa et al., 2015). However, less is known about the role of PTSD symptoms on these domains of parenting.
As such, we conducted a literature review of studies examining the unique contributions of postpartum depression and postpartum PTSD on these three domains of parenting during infancy, with mixed results. Some research shows differential outcomes associated with “simple PTSD” (i.e., PTSD due to one acute event, e.g., car accident or child birth) versus more complex PTSD (i.e., PTSD resulting from repeated and often chronic trauma exposure (Taylor et al., 2006). Therefore, further attention to the type of trauma experienced by postpartum women and its associations with psychopathology and parenting outcomes is needed.
Lang et al. (2010) examined the effects of postpartum PTSD on mothers’ self-reported parenting behaviors at one year postpartum in a non-clinical sample of mothers with varied trauma exposures. When controlling for co-morbid depression, postpartum PTSD symptoms were not a statistically significant predictors of parenting. Similarly, McDonald et al. (2011) examined the link between PTSD symptoms due to traumatic childbirth and self-reported parenting stress and mothers’ perception of their child at two years postpartum, controlling for co-morbid depression. Their results show that childbirth-related PTSD solely predicted parenting distress. In contrast, in a sample of depressed postpartum women in which 74% had a history of childhood maltreatment, Ammerman et al. (2012) failed to find significant associations between PTSD symptom severity and self-rated dysfunctional parenting, even after controlling for maternal depression..
In our own work studying the postpartum mother-infant relationship among mothers with childhood maltreatment histories, both postpartum depression and PTSD, but not maltreatment history alone, conveys risk for self-reported bonding problems (Muzik et al., 2012). This finding is based on data from the Maternal Anxiety in the Childbearing Years (MACY) study; a project evaluating the effects of mothers’ histories of childhood maltreatment on their postpartum psychosocial adaptation, parenting, mental health, and their young infants’ outcomes (NIMH K23 MH080147; PI: Muzik). Other published MACY data shows that, although childhood maltreatment history elevates risk for postpartum PTSD and depression, only postpartum depression (and not PTSD) is associated with less optimal observed parenting (Martinez-Torteya et al., 2014).
Similar results to the MACY findings are reported by Schechter et al. (2010) in a sample of low-income mothers with slightly older children (12–48 months). They report that, among women with trauma experiences, complex trauma is the norm and PTSD symptom levels vary across the sample (23% clinically significant PTSD, 41% sub threshold PTSD, 36% no PTSD). Schechter et al. also report a marginal correlation between observed atypical maternal behaviors during mother-child interaction and maternal PTSD (but not depression), but significant relations between maternal PTSD and the amount of time the child spent unsuccessfully trying to engage the mother in joint attention after a stressor (which the authors interpreted as maternal emotional unavailability). These investigators also report a significant correlation between maternal depression and PTSD and maternal self-reported parent-child dysfunctional interactions (measured via Parenting Stress Inventory). Of note, PTSD and depression symptoms are highly correlated in this sample (r=.80), and to our knowledge their analyses do not control for this comorbidity.
In more recent work by Schechter's group evaluating a sample of mothers with a high prevalence of interpersonal trauma and their toddlers (12–48 months old) (Schechter et al., 2015a, 2015b), comorbid depression and PTSD symptoms also are observed (r=.57). They also report that maternal PTSD severity is positively linked to negative maternal attributions about their toddlers (uncontrolled for depression) as well as lower levels of observed sensitive parenting (even after controlling for depression).
Taken together, the few studies evaluating the impact of postpartum PTSD on parenting indicators with young children (in contrast to evaluating impact on child outcomes per se) have yielded inconsistent results, particularly regarding whether there is a significant postpartum PTSD effect on parenting after accounting for postpartum depression (Ammerman et al., 2012; Lang et al., 2010; Martinez-Torteya et al., 2014). Much of the extant literature also suffers from methodological problems that potentially limit interpretation, including (a) frequent reliance on self-reported parenting indices rather than observed behaviors (with the exception of work by Schechter's group); (b) a focus on symptoms rather than clinically significant symptom cut-offs are validated against clinical diagnoses, possibly obscuring effects due to clinical impairment; and (c) a failure to tease apart effects of depression alone, PTSD alone, and comorbid PTSD and depression.
The current study aims to address these limitations by examining how postpartum depression, postpartum PTSD, and comorbid PTSD/depression may impact observed maternal parenting behaviors during mother–infant interaction at 6 months postpartum. We hypothesize that clinically significant PTSD alone will confer less risk to parenting than clinically significant depression alone or comorbid PTSD and depression. This is based on the fact that there is currently more empirical support for the detrimental impact of depression on parenting than for PTSD. Results from extant PTSD research is mixed, particularly when the effects of comorbid depression are accounted for. Two specific hypotheses are evaluated:
-
(1)
Mothers with clinically significant postpartum depression (alone or with comorbid PTSD) will report more bonding problems than healthy mothers or mothers with PTSD alone.
-
(2)
Mothers with clinically significant postpartum depression (alone or with comorbid PTSD) will show less optimal parenting behaviors (lower behavioral sensitivity, higher negative/lower positive affect) during mother-infant interaction than healthy mothers or mothers with PTSD alone.
2. Methods
2.1. Participants
Analyses in the current study were based on data collected from a subset of 164 mother–infant dyads (51% male infants) that completed a home assessment at 6 months postpartum and had valid observational data. The present sample came from data collected in a larger ongoing longitudinal project, the MACY study (N=268; NIMH K23 MH080147; PI: Muzik). The parent MACY project is a longitudinal investigation of the impact of maternal childhood maltreatment on postpartum psychopathology and parenting. As such, recruitment efforts oversampled for women with childhood maltreatment histories. Participants were recruited either from a pregnancy survey administered at prenatal care clinics via direct invitation (n=155; for a comprehensive description, see Seng et al. (2009)) or through community advertisement via posted flyers in antenatal and primary care clinics, informal and state-funded (e.g., WIC, Maternal-Infant Health Programs) resource centers for pregnant and postpartum women, or baby clothing and toy stores (n=113; for a comprehensive description see Martinez-Torteya et al. (2014)). Flyers indicated that we were looking for mothers who experienced difficult childhood upbringing,” were now parenting an infant, and were willing to participate in a study on their adjustment to motherhood during the postpartum period. Inclusion criteria included: at least 18 years of age at intake, English-speaking, and pregnant or within 6 months postpartum. Exclusion criteria included: history of schizophrenia or bipolar disorder, substance abuse problems during the past 3 months, or baby born > 6 weeks prematurely.
The 164 mother–infant dyads who completed the 6 month home visit and provided data for this study did not differ significantly from the other dyads in the larger MACY study on key demographic characteristics (i.e., maternal age, race/ethnicity, education, partner status, income, and infant sex). Infant age at the 6-month home visit ranged from 5.19 to 8.61 months (M=6.58, SD=.66). The current sample (N=164) includes all mother-infant dyads who had data at the 6-month time point on study variables described below. Reasons for drop-out (i.e., being counted toward initial n=268 but not towards current study's n=164) included could not be contacted following initial 4 month postpartum phone call (56%), not interested (8%), ineligible for 6 month interview (7%), missing data on key study variables (27%), or moved away (2%).
At the time of the 6-month visit, mothers’ age ranged from 18 to 45 years (M=29.18, SD=5.66). Of the 164 women, 102 (62%) had a childhood history of maltreatment. Women were predominately Caucasian (60% Caucasian, 20% African American, 5% Asian, 4% Hispanic, 5% Multiracial/other), partnered (80% married/living with partner, 20% single), and completed college (31% completed bachelor's degree, 28% post graduate education, 27% completed some college, 14% high school degree or less). Median family income ranged from $50,000–$54,999 with families reporting less than $10,000 in annual income (10%) to ≥$100,000 (22%). The total number of children in the home (including target infant) ranged from 1 to 5, with most mothers (52%) having one child.
2.2. Procedure
All participants completed a phone screening interview for eligibility when infants were 4 months old and agreed to complete two home-assessments at 6 months postpartum. During the first home visit, mothers signed a written consent, completed interviews and the mother–infant interaction tasks, and were left with a packet of questionnaires to complete. The completed packet was retrieved at the second home visit (approximately 1–2 weeks later). Home visit examiners were trained bachelor's- or master's-level study team members masked to maternal history and study hypotheses.
2.3. Measures
2.3.1. Maternal trauma history and current psychopathology
The Childhood Trauma Questionnaire (CTQ; Bernstein and Fink, 1998) was completed via telephone interview at four months post-partum. Mothers self-rated their childhood maltreatment experiences on a 28-item, 5-point Likert scale. Test–retest reliabilities range from .79 to .86, and good validity has been reported (Bernstein and Fink, 1998), In the present study, a dichotomous score was given based on whether the mothers reported any history of maltreatment (yes or no). If women indicated significant maltreatment histories, follow-up interview questions were asked to inquire about what they identified as the primary traumatic experience, how many maltreatment experiences they recalled, and the different types of maltreatment experienced (see Table 1).
Table 1.
Trauma and symptom characteristics for total sample and by clinical sub-group.
| Clinical group | Childhood maltreatment | Primary maltreatment typea | Number of maltreatment experiencesa | Number of maltreatment typesc | Depression and PTSD symptoms |
|---|---|---|---|---|---|
| Total sample n=164 | Yes: 62% (n=102) No: 30% (n=50) Missing: 8% (n=12) |
Sexual: 26% (n=27) Physical: 22% (n=22) Neglect: 4% (n=4) Emotional: 28% (n=29) Missing: 20% (n=21) |
Range: 1–40 Mean: 7.92 SD: 6.88 Mode: 4 Median: 6.00 |
Range: 1–4 Mean: 2.73 SD: 1.01 Mode: 2 Median: 3 |
Depression M=63.12 Depression SD=22.43 PTSD M=4.18 PTSD SD=4.36 |
| Healthy n=108 | Yes: 51% (n=55) No: 39% (n=42) Missing: 10% (n=11) |
Sexual: 22% (n=12) Physical: 21% (n=12) Neglect: 4% (n=2) Emotional: 26% (n=14) Missing: 27% (n=15) |
Range: 1–26 Mean: 6.65 SD: 5.42 Mode: 2 Median: 5.50 |
Range: 1–4 Mean: 2.48 SD: .96 Mode: 2 Median: 2 |
Depression M=52.01 Depression SD=12.69 PTSD M=1.92 PTSD SD=2.19 |
| Depressed n=14 | Yes: 64% (n=9) No: 29% (n=4) Missing: 7% (n=1) |
Sexual: 40% (n=4) Physical: 30% (n=3) Neglect: 0% (n=0) Emotional: 20% (n=2) Missing: 10% (n=1) |
Range: 2–14 Mean: 7.38 SD: 4.21 Modeb: 4, 11 Median: 6.50 |
Range: 1–4 Mean: 3.00 SD: 1.07 Mode: 3 Median: 3 |
Depression M=93.43 Depression SD=14.00 PTSD M=3.79 PTSD SD=2.89 |
| PTSD n=22 | Yes: 86% (n=19) No: 14*% (n=3) Missing: 0% (n=0) *=2 due to traumatic childbirth, 1 due to interpersonal violence in adulthood |
Sexual: 28% (n=5) Physical: 11% (n=2) Neglect: 0% (n=0) Emotional:43% (n=8) Missing: 18% (n=4) |
Range: 2–15 Mean: 6.33 SD: 3.27 Modeb: 4, 5, 8 Median: 5.00 |
Range: 1–4 Mean: 2.80 SD: 1.08 Mode: 4 Median: 3 |
Depression M=64.63 Depression SD=11.67 PTSD M=10.11 PTSD SD=2.31 |
| Comorbid n=20 | Yes: 95% (n=19) No: 5% (n=1) Missing: 0% (n=0) |
Sexual: 30% (n=6) Physical: 25% (n=5) Neglect: 10% (n=2) Emotional: 25% (n=5) Missing: 10% (n=21) |
Range: 2–40 Mean: 12.88 SD: 10.87 Modeb: 2, 4, 7, 12,24 Median: 9.50 |
Range: 1–4 Mean: 3.19 SD: .91 Mode: 4 Median: 3 |
Depression M=100.45 Depression SD=14.81 PTSD M=11.05 PTSD SD=2.89 |
Note: PTSD=posttraumatic stress disorder, M=mean, SD=standard deviation.
Numbers reflect % of women out of women who experienced childhood maltreatment (n=102).
Multiple modes exist.
Number of maltreatment types=how many categories (i.e., sexual, physical neglect, emotional) experienced with possible range 1–4.
Mothers reported on the level of their current depressive symptoms at the 6-month home visit using the Postpartum Depression Screening Scale (PPDS) (Beck and Gable, 2002). The PPDS includes 35 items rated using a 5-point Likert scale. Scores are summed to yield a total symptom score. The total symptom count was evaluated in the present study (α=.95). A score of 80 or higher denotes a likely clinical diagnosis (Beck and Gable, 2000). Twenty-two percent of women in the current sample had clinically significant depression at 6 months postpartum.
Mothers also reported on current PTSD symptoms at the 6-month home visit (National Women's Study PTSD Module; NWS-PTSD) (Resnick et al., 1993). This 26-item instrument is a modified version of the Diagnostic Interview Schedule (DIS) adapted for use in large epidemiological studies, which provides both continuous symptom scores and indicates clinically significant PTSD status based on a standard cut-off. External validity is good, as shown by adequate agreement (κ=.77) with a clinician-administered structured interview (SCID) (Resnick et al., 1993). In the current study, 26% of women displayed clinically significant PTSD symptoms at 6 months postpartum.
2.3.2. Theoretical group membership based on trauma history and symptom presentation
Based on their clinical cut-off scores, mothers were categorized into five different clinical groups: (A) Healthy Controls (n=53) with no trauma history and no current clinically significant PTSD or depression symptoms; (B) Resilient (n=55) with history of childhood maltreatment but no current clinically significant PTSD or depression symptoms; (C) Depressed (n=14; 4/10 had child abuse history) with clinically significant depression only; (D) PTSD (n=22; 19 had a child abuse history, 3 had trauma in adulthood only) with clinically significant PTSD only; and (E) Comorbid (n=20; 20 had child abuse history) and clinically significant depression and PTSD.
To promote parsimony, the Healthy Control and Resilient groups were combined (Healthy group; n=108). The women in these groups had no current psychopathology and did not differ significantly on measures of impaired bonding or parenting behaviors, as was the case in prior work in this project (Muzik et al., 2012).
There were no significant differences between the four groups on demographic variables [i.e., maternal age, child age, household income, maternal education, marital status, number of children in home; Wilks’ λ=.78, F(15, 221)=1.33, p=.19, ; child gender (X2 (3)=.67, p=.88), ethnicity Fisher's Exact Test (2-sided) p=.66].
2.3.3. Self-reported parenting
The Postpartum Bonding Questionnaire (PBQ) (Brockington et al., 2001), assessed mother's feelings or attitudes towards her relationship with her infant (e.g., “I feel close to my baby,” “my baby irritates me”) using a 6-point Likert scale. The original instrument has 25-items with 2 questions tapping into risk of infant abuse; however, based on previously reported poor psychometric properties (Brockington et al., 2006) and the potential to upset mothers, we omitted those two questions. Prior work indicates good reliability and validity for the remaining 23 items of the PBQ (Brockington et al., 2001, 2006). For this study, the Total Score was used to assess Impaired Bonding (α=.80) with higher scores reflecting greater impairment.
2.3.4. Observed parenting
Multiple dimensions of maternal parenting behavior were scored from videotapes of mother-infant interaction within the same day across two tasks: a 10-minute Free-play task (split into five minute segments for coding) and two 3-minute teaching tasks. A standard set of age-appropriate toys was provided and mothers were invited to play with their infant as they normally would. Following the play session, dyads participated in two consecutive teaching tasks (i.e., putting blocks into a bucket, stacking cups) designed to be beyond the infants’ developmental capacities. The teaching tasks were included to provide an assessment of parenting under challenging circumstances.
The video segments in each context were scored for three dimension of maternal interactive behavior (Behavioral Sensitivity, Positive Affect, and Negative Affect) using 5-point Likert ratings from the MACY Infant-Parent Coding System (MIPCS; Earls et al., 2009). This procedure resulted in 4 ratings for each code: Free-play 1 (first 5 min of free-play), Free-play 2 (second 5 min of free-play), Teaching Task 1 (first teaching task), and Teaching Task 2 (second teaching task). Scoring was carried out by trained coders masked to maternal trauma history, maternal psychopathology status, and the study's hypotheses. To evaluate inter-coder reliability, coders independently rescored 40 randomly selected videotapes, Intraclass correlations (ICC) were generally well above .80, denoting very good inter-coder agreement: Behavioral Sensitivity (ICC Free-play=.85; ICC Teaching tasks=.86); Negative Affect (ICC Free-play=.93; ICC Teaching tasks=.90); and Positive Affect, ICC Free-play=.93; ICC Teaching tasks=.85).
2.3.5. Analytic plan
We first used frequencies, Fisher's Exact tests, and univariate and multivariate Analysis of Variance (ANOVAs) to better understand the trauma characteristics of the sample and symptom levels of the clinical groups. We then used univariate and multivariate ANOVAs to examine mean levels differences in parenting outcomes by clinical group. Lastly, we used repeated measures ANOVAs (RMANOVAs) to investigate the effect of level of challenge on maternal parenting across the four interactive tasks, given that tasks became more challenging as time progressed. In the RMANOVAs, clinical group (4) was the between-subjects variable and Time (4; Free-play 1, Free-play 2, Teaching Task 1, Teaching Task 2) was the within-subjects variable. When relevant, we include Cohen's d as a measure of effect size of mean differences and followed Cohen's (1992) criteria: .10 (small effect), .30 (medium effect), and .50 (large effect).
3. Results
3.1. Preliminary descriptive analyses
Given the importance of understanding trauma characteristics (e.g., single trauma versus complex trauma), we examined the trauma characteristics of the overall sample, as well as by each group (see Table 1). In the present sample, 62% of mothers (n=102) had a significant history of childhood maltreatment, 29% had no history of childhood maltreatment, and 7% had missing data. Clinical interviewing was used to follow up about trauma experiences for the women who indicated maltreatment histories. Regarding number of maltreatment experiences (i.e., number of times a woman recalled experiencing some form of abuse), the sample ranged from 1 abuse experience to 40 experiences (mean=7.92, mode=4). Regarding primary trauma type (the trauma that women identified as most impactful), 36% reported sexual abuse, 34% reported psychological abuse, 24% reported physical abuse, and 6% reported physical neglect. The majority of women (86.5%) experienced > 1 maltreatment type (i.e., physical, sexual, psychological, and/or neglect).
Trauma characteristics from childhood maltreatment by clinical group are presented in Table 1. There were significant differences across clinical groups in number of maltreatment experiences [F(3, 76) =4.03, p=.010, ]. Specifically, women in the comorbid group reported more experiences than women in Healthy (d=.73) and PTSD (d=.82) groups. There were no differences by group in the primary maltreatment type experienced, or whether or not the perpetrator of maltreatment was a parent [Fisher's Exact Test (2-sided) p=.81, p=.91, respectively].
As hypothesized, there were significant differences in depression and PTSD symptom levels across clinical groups [Wilks’ λ=.13, F(6, 312)=90.64, p < .001, ]. Specifically, women in the PTSD and comorbid groups reported higher PTSD symptom levels than women in the Healthy (d=3.64, 3.56 respectively) and Depression (d=2.42, 2.51 respectively) groups. However, there was no significant difference in PTSD symptoms between women in the PTSD and Comorbid groups (p=.76).
Regarding depression symptoms, women in the Depressed group reported higher depression symptoms than women in the Healthy and PTSD groups (d=15.88, 8.90, respectively), women in the PTSD group reported higher depression symptoms than women in the Healthy group (d=5.52), and women in the Comorbid group reported higher symptoms than women in the Healthy and PTSD groups (d=21.69, 12.18, respectively). There was no significant difference in depression symptoms between women in the Depressed and Comorbid groups (p=.54).
3.2. Mean differences in parental bonding by clinical group
Univariate ANOVA results indicated there was a significant main effect of clinical group on bonding impairment (see Table 2). Post hoc tests indicated that women in the Depressed and the Comorbid groups reported more bonding impairment than women in the Healthy group.
Table 2.
Means, standard deviations, ranges, and sidak post hoc analyses for study variables.
| Maternal variable | Maternal clinical sub-groups |
ANOVA F test | Post hoc comparisons | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| A. Healthy |
B. Depressed |
C. PTSD |
D. Comorbid |
|||||||
|
n=108 |
n=14 |
n=22 |
n=20 |
|||||||
| M (SD) | Range | M (SD) | Range | M (SD) | Range | M (SD) | Range | Significant Group Differences (Cohen's d) | ||
| Impaired Bonding | 8.02 (6.71) | 0–46 | 13.07 (8.13) | 2–33 | 11.23 (6.19) | 0–23 | 12.40 (5.73) | 4–26 | F(3, 159)=4.85, p=.003, | A<B (−3.77, p=.04) A<D (−3.81, p=.04) |
| Behavioral Sensitivity-FP | 3.65 (.84) | 1.5–5.0 | 3.06 (1.07) | 1.1–5.0 | 3.85 (.77) | 1.6–5.0 | 3.5 (.96) | 1.5–4.9 | F(3, 157)=2.61, p=.05, | B<C (−.85) |
| Behavioral Sensitivity-TT | 3.32 (.96) | 1.0–5.0 | 2.77 (.99) | 1.5–4.8 | 3.40 (.75) | 2.3–5.0 | 3.26 (1.10) | 1.3–4.8 | NS | NS |
| Positive Affect-FP | 2.57 (.55) | 1.5–5.0 | 2.12 (.58) | 1.3–3.5 | 2.71 (.51) | 1.6–3.9 | 2.33 (.41) | 1.5–3.0 | F(3, 157)=4.85, p=.003, | B<A (−.80), C (−1.05) |
| Positive Affect-TT | 2.51 (.58) | 1.3–4.5 | 2.11 (.45) | 1.5–2.8 | 2.69 (.50) | 1.5–3.5 | 2.51 (.46) | 1.8–3.5 | F(3, 152)=3.40, p=.02, | B<A (−.77), C (−1.22) |
| Negative Affect-FP | 1.13 (.35) | 1.0–2.9 | 1.41 (.75) | 1.0–3.8 | 1.06 (.14) | 1.0–1.5 | 1.11 (.31) | 1.0–2.3 | F(3, 157)=2.86, p=.04, | B > A (.48), C (.65), D (.52) |
| Negative Affect-TT | 1.09 (.30) | 1.0–3.0 | 1.54 (.69) | 1.0–2.5 | 1.03 (.16) | 1.0–1.8 | 1.11 (.35) | 1.0–2.5 | F(3, 152)=7.68, p<.001, | B >A (.85), C (1.02), D (.79) |
Note: impaired bonding=Self-reported from Postpartum Bonding Questionnaire, FP=free play, TT=teaching task, PTSD=posttraumatic stress disorder.
3.3. Mean differences in parenting behavior by clinical group
Utilizing MANOVA, we calculated mean differences in observed parenting behaviors by clinical group. To simplify results and cut back on the number of analyses conducted, an average score was computed for each code per task (i.e., average for Free-play, average for Teaching Task). Separate analyses were conducted for the Free-play and teaching tasks. Omnibus test results are reported in text. Subsequent ANOVA and post hoc tests are reported in Table 2.
Free-play
A significant main effect of clinical group was found [Wilks’ λ=.88, F(9, 377.38)=2.36, p=.01, ]. Specifically, women in the Depressed group exhibited less Behavioral Sensitivity than women in the PTSD group. Women in the Depressed group also showed less Positive Affect than women in the Healthy and PTSD groups; and more Negative Affect than women in the Healthy and PTSD groups.
Teaching Task
A significant clinical group main effect was also observed for maternal behavior during the teaching tasks [Wilks’ λ=.85, F(9, 365.21)=2.82, p=.003, ]. Specifically, women in the Depressed group showed less Positive Affect than women in the Healthy and PTSD groups, and more Negative Affect than women in the Healthy, PTSD, and Comorbid groups.
3.4. Observed parenting behavior across tasks by clinical group
A total of 3 RMANOVAs were conducted, given that there were 3 behavioral observation codes of interest (Behavioral Sensitivity, Positive Affect, Negative Affect). All statistical test results of the RMANOVAs are presented in Table 3.
Table 3.
RMANOVA results and follow-up analyses for observational codes.
| Variable | Mauchly's testa (ε) | Multivariate effect | Follow-up ANOVAb |
|---|---|---|---|
| Behavioral Sensitivity Time Time×Clinical Group |
χ2(5)=34.48, p< .001* (ε=.90) |
F(2.59, 372.53) = 11.15, p<.001, * F(7.76, 372.53) =.26, p=.98, |
NA |
| Positive Affect Time Time×Clinical Group |
χ2(5)=62.71, p< .001* (ε=.80) |
F(2.32, 333.80)=1.96, p=.14, F(6.95, 333.80)= 1.17, p=.32, |
NA |
| Negative Affect Time Time×Clinical Group |
χ2(5)=108.41, p < .001* (ε=.77) |
F(2.22, 315.69)=5.25, p=.004, * F(6.67, 315.69)=2.52, p=.017, * |
F(3, 144) =4.45 p=.005, |
Mauchly's test was used to assess for violations of sphericity assumptions; and when violated Greenhouse-Geisser estimates (given ε < .75) were used to test for significant main effects of context or interaction effects between time and clinical group.
Univariate ANOVA was used to examine significant interaction term (Time×Clinical Group).
p< .05.
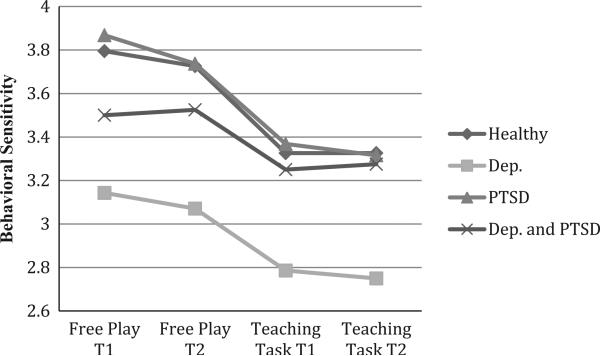
For Behavioral Sensitivity, there was a significant main effect of time on observed behavioral sensitivity. Examination of the means and the plot revealed that, regardless of clinical group, all mothers tended to decrease in behavioral sensitivity across time (i.e., as challenged increased across tasks), see Fig. 1. There was no significant interaction between time and clinical group.
Fig. 1.
Maternal behavioral sensitivity across time by clinical group. Note: Healthy=healthy controls and resilient; Dep=mothers with clinically significant Depression; PTSD=mothers with clinically significant post traumatic stress disorder; Dep and PTSD=mothers with comorbid clinically significant depression and PTSD.
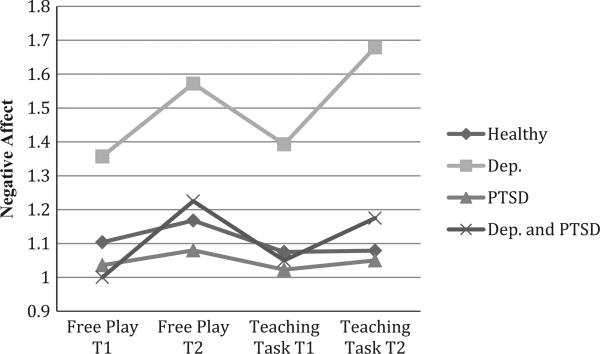
For Positive Affect, there was no significant main effect for time, nor was there a significant interaction between context and clinical group. In contrast, for Negative Affect, there was a significant effect of time that was qualified by a significant interaction effect of time by clinical group on observed Negative Affect. Post hoc analyses using a Sidak correction revealed that mothers in the Depressed group were more likely than the mothers in the other groups to display negative affect across time (p < .001).
To further explore the Time×Clinical Group interaction effect, a univariate ANOVA was conducted to examine whether there were group differences on the amount of change in negative affect across tasks. Based on visual inspection of Fig. 2, change scores were computed (Time 2–Time 1) to examine change from the first time point (Free-play 1) to the last time point (Teaching Task 2). There was a significant effect of clinical group on change in Negative Affect from Free-play 1 to Teaching Task 2 (Table 3). Post hoc analyses using a Sidak correction revealed that mothers in the Depressed group increased their negative affect across time more than mothers in the Healthy or PTSD groups (d=4.79, 3.45, respectively). Mothers in the Depressed group and Comorbid group were no longer significantly different when the specific contrast was examined.
Fig. 2.
Maternal negative affect across time by clinical group. Note: Healthy=healthy controls and resilient; Dep=mothers with clinically significant depression; PTSD=mothers with clinically significant post traumatic stress disorder; Dep and PTSD=mothers with comorbid clinically significant depression and PTSD.
4. Discussion
The goal of this study was to investigate whether mothers who had clinically significant depression, PTSD, or comorbid depression and PTSD differed on self-rated and observed parenting indicators, and whether these three groups differed significantly from mothers without current psychopathology. Overall, we found that mothers with depression had the least optimal parenting outcomes, whether indexed with self-rated or observed parenting measures. More specifically, depressed mothers, regardless of PTSD comorbidity, reported more bonding impairment than healthy or resilient mothers. During observed free-play interactions with their infants, depressed mothers were behaviorally less sensitive than mothers with PTSD alone, affectively less positive than healthy/resilient mothers, and affectively more negative than mothers in all other groups. The teaching task results paralleled the free-play results.
To evaluate the level of interactive challenge on parenting in the three maternal psychopathology groups, we examined the temporal pattern of observed maternal behaviors across tasks and time. All mothers independent of psychopathology decreased in behavioral sensitivity with their infants across tasks and time; however, only the mothers with depression significantly increased in negative affect.
Our findings are intriguing as they indicate that there may be unique effects of PTSD and depression on parenting during infancy. Our consideration of distinct clinical categories and comorbidity allows us to better understand the relation between distinct and comorbid diagnoses and postpartum parenting rather than merely controlling for comorbid symptoms. Given that infancy is a critical period for relationship-based learning optimized by sensitive and positive parenting, our study also has clinical significance because it sheds further light on our understanding of the impact of maternal psychopathology on perceived and observed parenting with young infants.
Although results from the present study on maternal depression are consistent with previous reports on the detrimental effects of post-partum depression on parenting quality and infant outcomes for reviews see (Cooper and Murray, 1998; Lovejoy et al., 2000; Weinberg and Tronick, 1998), they also provide contrasting results. Specifically, our results show that the detrimental effect of depression on parenting holds only for mothers with postpartum depression, and not for mothers with comorbid depression and PTSD. This was a surprising result, because comorbid depression and anxiety is usually regarded as reflecting greater illness severity and likely to be predictive of worse maternal and child outcomes (Field et al., 2010; Pollack, 2005). For instance, prior work shows that comorbid depression and PTSD negatively impact child outcomes in preschoolers (Chemtob et al., 2010, 2013), and that maternal PTSD has unique (independent of depression) detrimental effects on infant emotion regulation (Bosquet Enlow et al., 2011).
Although the reason for these contrasting results is not fully understood, methodological differences among studies may play an important role. For instance, in the present study, our study utilized a different sample, procedures, and measures than those utilized in prior studies reporting a detrimental impact of maternal PTSD. For instance, our study evaluates parenting at younger child ages than prior research (e.g., Schechter et al. (2014) evaluated preschool-aged children). Our study also focuses on maternal behavior rather than child behavior (e.g., Chemtob et al., 2010b; Enlow et al., 2011), and utilizes both observational measures of parenting as well as parent self-report measures (e.g., Ammerman et al. (2012) relied solely on self-report).
It is interesting that mothers in the current study with comorbid depression and PTSD self-reported highest bonding problems with their infants. This suggests impairment in these women's subjective experience of motherhood. However, during observed mother-infant interactions, mothers with comorbid PTSD and depression were actually interacting quite sensitively and with low negativity with their infants, which may indicate the presence of subjective cognitive distortion in this group. The notion that PTSD may bias mothers’ self-perceptions of their parenting and of their child, is consistent with others’ work documenting that maternal PTSD is associated with higher self-report of dysfunctional mother-child interactions (Schechter et al., 2010), and negative, distorted maternal attributions about the self, own attachment figures and the baby (Schechter et al., 2015a, 2015b). With regard to maternal postpartum PTSD, we found that mothers with clinically significant PTSD alone showed similar interactive behaviors to those in the healthy control group and women who were trauma-exposed but who showed no psychopathology at this level of analysis.
Thus, our findings show that, in the context of childhood abuse history and/or current PTSD, maternal depression is the most salient risk factor associated with parenting impairment during infancy. Our results are in line with previous reports, showing that PTSD effects disappear when maternal depression is accounted for (Lang et al., 2010). One explanation may be that PTSD symptoms fluctuate, even within an individual, based on context and being triggered by trauma reminders, whereas depression involves more global and persistent impairment, which possibly impacts parenting behaviors more chronically. Another explanation may be that our behavioral tasks (free-play and teaching) were relatively safe and non-threatening. In sub analyses not presented in this paper, the level of the infants’ negative affect during free-play and teaching tasks was relatively low and did not differentiate across groups. Thus, maternal PTSD symptoms may not have been activated during the mother-infant interaction contexts included in this study and thus may not have interfered with “good enough” parenting.
In the current study, women with depression were also very likely to have a childhood maltreatment history given that this sample was over-representing childhood maltreatment survivors. One might speculate that depressed women may have experienced more frequent traumatization than mothers in other groupings, which, in turn, may have heightened their risk for mood symptoms that interfere with parenting. However, our results do not support this explanation as there were no significant group differences in number of maltreatment experiences or whether the perpetrator was a parent or not, between the maternal depression only versus comorbid depression/PTSD groups. Moreover, mothers’ depression symptom levels did not differ between depression only and comorbid depression/PTSD groups, indicating that in regards to depression severity both groups were equally impacted.
There may be third unmeasured variables that may be affecting our results (e.g., mothers’ childhood attachment status). Similarly, the developmental period at which we studied parenting (infancy) may have influenced our results. Prior studies with older children report that maternal PTSD exerts a detrimental influence parenting (e.g., Schechter et al., 2010, 2015a, 2015b). It may be that older children exhibit particular child behaviors that are more likely to be “triggers” that affect parenting (e.g., child temper tantrums, separation anxiety) than during early infancy. Future research would benefit from examining the link between PTSD symptoms and parenting behaviors long-itudinally to account for potential developmental differences.
Our study is not free of limitations. First, we have relatively small cell sizes per clinical group, limiting power. However, even with our small sample, we found clear differentiation in parenting quality between clinical groups. Future work would benefit from a replication with a larger data set, particularly to confirm the possibly protective effects of comorbid PTSD with depression to parenting sensitivity and affect. Second, many other factors may impact parenting risk (e.g., low income, poor education, partnered status) which were not evaluated in the present study due to power restrictions and the fact that our clinical groups did not differ on those variables. Although our sample included women from a range of socioeconomic and educational backgrounds, the majority were Caucasian, partnered, and college-educated. Further research with larger, more diverse samples of postpartum women and infants is needed. Third, diagnoses were not assessed using psychiatric interviews, but derived based on cut-offs on self-report measures. Women's responses on such measures may have been influenced by the symptoms themselves (e.g., experiential avoidance associated with PTSD). However, these self-report questionnaires are well validated against diagnostic interviews, increasing our confidence that our clinical categories match up with clinical diagnoses. Fourth, we also acknowledge that our use of the word “Resilient” makes an interpretive assumption that we did not directly examine in the present study. Future research would benefit from better understanding what characteristics (e.g., type of trauma, individual traits) and factors (e.g., environmental support, receipt of therapy) differentiated women who were trauma exposed and did/did not have current psychopathology.
Finally, the nature of our sample and tasks must be considered when making sense of our results. For example, we acknowledge the range of trauma experiences in our sample and are unable to draw conclusions about any one particular type of trauma. We can con-fidently say that the majority of our mothers had multiple traumas (mean=7.9, mode=4), and that primary trauma type and perpetrator (caregiver versus other person) did not differ by clinical group. However, we are unable to evaluate whether results differ for mothers who had a single trauma versus complex trauma; this is an important focus for future research.
Our results have clinical implications. First, our data suggest that a mother's childhood trauma history alone may not determine poor parenting in the absence of co-occurring mental illness allowing clinicians to offer a message of hope and resilience to their clients with trauma histories. Our results highlight that a maternal history of child abuse may not necessarily be associated with her own abusive parenting behaviors. This result is consistent with prior work that shows that while parents who were maltreated as children themselves are at higher risk of abusing their own children (Chemtob et al., 2013; Ertem et al., 2000; Loseke et al., 2005, 81, 82), not all do, and in fact, that the majority of abusing parents were not themselves abused (Hunter et al., 1978; Widom and Wilson, 2015). The literature review by Ertem's group (2000) suggests that approximately only 30% of caregivers with a childhood abuse history go on to abuse their own children, while Oliver (1993) suggests that 33% will go on to engage in neglectful or abusive parenting themselves, while 33% of victims do not, and the remaining 34% of victims will remain vulnerable to the effects of caregiver stress. Thus, clinicians should be aware that mothers with trauma histories may be prone to have faulty cognitions and mental representations about their bonding or parenting, and that such faulty cognitions can be reduced through quality interventions that target such distorted parenting attributions in these trauma-exposed mothers (Muzik et al., 2015; Schechter et al., 2015a, 2015b). While our sample is a convenience sample over-representing a group of mothers with interpersonal maltreatment histories who self-referred in response to a flyer asking about childhood “upbringing difficulties”, we believe that this cohort is representative of the large group of maltreatment survivor women in the community given the high rates of interpersonal violence experienced by women in the US, and thus, the findings generalizable to a larger community. Interpersonal violence exposure, during childhood or adulthood, is quite prevalent with rates exceeding 25% of US females (Agrawal et al., 2014; Gazmararian et al., 1996; NCANDS, 2013).
Finally, our results highlight the primacy of maternal postpartum depression as a critical maternal characteristic impinging on parenting sensitivity. This fact confirms and highlights the clinical necessity to screen for and treat postpartum depression to assure the establishment of healthy mother–child relationships, and to allow for a positive child developmental trajectory.
References
- Agrawal A, Ickovics J, Lewis JB, Magriples U, Kershaw TS. Postpartum intimate partner violence and health risks among young mothers in the United States: a prospective study. Matern. Child Health J. 2014;18(8):1985–1992. doi: 10.1007/s10995-014-1444-9. http://dx.doi.org/10.1007/s10995-014-1444-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alcorn KL, O'Donovan A, Patrick JC, Creedy D, Devilly GJ. A prospective longitudinal study of the prevalence of post-traumatic stress disorder resulting from childbirth events. Psychol. Med. 2010;40(11):1849–1859. doi: 10.1017/S0033291709992224. http://dx.doi.org/10.1017/S0033291709992224. [DOI] [PubMed] [Google Scholar]
- Ammerman RT, Putnam FW, Chard KM, Stevens J, Van Ginkel JB. PTSD in depressed mothers in home visitation. Psychol. Trauma: Theory, Res., Pract. Policy. 2012;4(2) doi: 10.1037/a0023062. http://dx.doi.org/10.1037/a0023062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Banyard VL, Williams LM, Siegel JA. The impact of complex trauma and depression on parenting: an exploration of mediating risk and protective factors. Child Maltreat. 2003;8(4):334–349. doi: 10.1177/1077559503257106. [DOI] [PubMed] [Google Scholar]
- Beck CT, Gable RK. Postpartum Depression Screening Scale: development and psychometric testing. Nurs. Res. 2000;49(5):272–282. doi: 10.1097/00006199-200009000-00006. [DOI] [PubMed] [Google Scholar]
- Beck CT, Gable RK. Postpartum Depression Screening Scale Manual. Western Psychological Services; Los Angeles: 2002. [Google Scholar]
- Bernstein DP, Fink L. Childhood Trauma Questionnaire: A Retrospective Self-Report Manual. The Psychological Corporation; San Antonio: 1998. [Google Scholar]
- Buist A. Childhood abuse, postpartum depression and parenting difficulties: A literature review of associations. Aust. N. Z. J. Psychiatry. 1998;32(3):370–378. doi: 10.3109/00048679809065529. http://dx.doi.org/10.3109/00048679809065529. [DOI] [PubMed] [Google Scholar]
- Bosquet Enlow M, Kitts RL, Blood E, Bizarro A, Hofmeister M, Wright RJ. Maternal posttraumatic stress symptoms and infant emotional reactivity and emotion regulation. Infant Behav. Dev. 2011;34(4):487–503. doi: 10.1016/j.infbeh.2011.07.007. http://dx.doi.org/10.1016/j.infbeh.2011.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brockington IF, Fraser C, Wilson D. The Postpartum Bonding Questionnaire: a validation. Arch. Women's Ment. Health. 2006;9(5):233–242. doi: 10.1007/s00737-006-0132-1. http://dx.doi.org/10.1007/s00737-006-0132-1. [DOI] [PubMed] [Google Scholar]
- Brockington IF, Oates J, George S, Turner D, Vostanis P, Sullivan M, Murdoch C. A Screening Questionnaire for mother-infant bonding disorders. Arch. Women's Ment. Health. 2001;3(4):133–140. http://dx.doi.org/10.1007/s007370170010. [Google Scholar]
- Cerulli C, Talbot NL, Tang W, Chaudron LH. Co-occurring intimate partner violence and mental health diagnoses in perinatal women. J. Women's Health. 2011;20(12):1797–1803. doi: 10.1089/jwh.2010.2201. http://dx.doi.org/10.1089/jwh.2010.2201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chemtob CM, Gudiño OG, Laraque D. Maternal posttraumatic stress disorder and depression in pediatric primary care: association with child maltreatment and frequency of child exposure to traumatic events. JAMA Pediatrics. 2013;167(11):1011–1018. doi: 10.1001/jamapediatrics.2013.2218. http://dx.doi.org/10.1001/jamapediatrics.2013.2218. [DOI] [PubMed] [Google Scholar]
- Chemtob CM, Nomura Y, Rajendran K, Yehuda R, Schwartz D, Abramovitz R. Impact of maternal posttraumatic stress disorder and depression following exposure to the September 11 attacks on preschool children's behavior. Child Dev. 2010a;81(4):1129–1141. doi: 10.1111/j.1467-8624.2010.01458.x. http://dx.doi.org/10.1111/j.1467-8624.2010.01458.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chemtob CM, Nomura Y, Rajendran K, Yehuda R, Schwartz D, Abramovitz R. Impact of maternal posttraumatic stress disorder and depression following exposure to the September 11 attacks on preschool children's behavior. Child Dev. 2010b;81(4):1129–1141. doi: 10.1111/j.1467-8624.2010.01458.x. http://dx.doi.org/10.1111/j.1467-8624.2010.01458.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J. A power primer. Psychol. Bull. 1992;112(1):155–159. doi: 10.1037//0033-2909.112.1.155. http://dx.doi.org/10.1037/0033-2909.112.1.155. [DOI] [PubMed] [Google Scholar]
- Cooper PJ, Murray L. Postnatal depression. BMJ (Clin. Res. Ed.) 1998;316(7148):1884–1886. doi: 10.1136/bmj.316.7148.1884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davalos DB, Yadon CA, Tregellas HC. Untreated prenatal maternal depression and the potential risks to offspring: a review. Arch. Women's Ment. Health. 2012;15(1):1–14. doi: 10.1007/s00737-011-0251-1. http://dx.doi.org/10.1007/s00737-011-0251-1. [DOI] [PubMed] [Google Scholar]
- Deave T, Heron J, Evans J, Emond A. The impact of maternal depression in pregnancy on early child development. BJOG: Int. J. Obstet. Gynaecol. 2008;115(8):1043–1051. doi: 10.1111/j.1471-0528.2008.01752.x. http://dx.doi.org/10.1111/j.1471-0528.2008.01752.x. [DOI] [PubMed] [Google Scholar]
- Denham SA, Workman E, Cole PM, Weissbrod C, Kendziora KT, Zahn-Waxler C. Prediction of externalizing behavior problems from early to middle childhood: the role of parental socialization and emotion expression. Dev. Psychopathol. 2000;12(1):23–45. doi: 10.1017/s0954579400001024. http://dx.doi.org/10.1017/S0954579400001024. [DOI] [PubMed] [Google Scholar]
- DiLillo D. Interpersonal functioning among women reporting a history of childhood sexual abuse: empirical findings and methodological issues. Clin. Psychol. Rev. 2001;21(4):553–576. doi: 10.1016/s0272-7358(99)00072-0. [DOI] [PubMed] [Google Scholar]
- Earls L, Muzik M, Beeghly M. Maternal and Infant Behavior Coding Manual. 2009 [Google Scholar]
- Edwards VJ, Holden GW, Felitti VJ, Anda RF. Relationship between multiple forms of childhood maltreatment and adult mental health in community respondents: Results from the Adverse Childhood Experiences study. Am. J. Psychiatry. 2003;160(8):1453–1460. doi: 10.1176/appi.ajp.160.8.1453. http://dx.doi.org/10.1176/appi.ajp.160.8.1453. [DOI] [PubMed] [Google Scholar]
- Egeland B, Jacobvitz D, Sroufe LA. Breaking the cycle of abuse. Child Dev. 1988;59(4):1080–1088. doi: 10.1111/j.1467-8624.1988.tb03260.x. [DOI] [PubMed] [Google Scholar]
- Enlow MB, Kitts RL, Blood E, Bizarro A, Hofmeister M, Wright RJ. Maternal posttraumatic stress symptoms and infant emotional reactivity and emotion regulation. Infant Behav. Dev. 2011;34(4):487–503. doi: 10.1016/j.infbeh.2011.07.007. http://dx.doi.org/10.1016/j.infbeh.2011.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ertem IO, Leventhal JM, Dobbs S. Intergenerational continuity of child physical abuse: how good is the evidence? Lancet (Lond., Engl.) 2000;356(9232):814–819. doi: 10.1016/S0140-6736(00)02656-8. http://dx.doi.org/10.1016/S0140-6736(00)02656-8. [DOI] [PubMed] [Google Scholar]
- Feldman R. Parent-infant synchrony: biological foundations and developmental outcomes. Curr. Directions Psychol. Sci. 2007;16(6):340–345. http://dx.doi.org/10.1111/j.1467-8721.2007.00532.x. [Google Scholar]
- Field T, Diego M, Hernandez-Reif M, Figueiredo B, Deeds O, Ascencio A, Kuhn C. Comorbid depression and anxiety effects on pregnancy and neonatal outcome. Infant Behav. Dev. 2010;33(1):23–29. doi: 10.1016/j.infbeh.2009.10.004. http://dx.doi.org/10.1016/j.infbeh.2009.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gazmararian JA, Lazorick S, Spitz AM, Ballard TJ, Saltzman LE, Marks JS. Prevalence of violence against pregnant women. J. Am. Med. Assoc. 1996;275(24):1915–1920. [PubMed] [Google Scholar]
- Grekin R, O'Hara MW. Prevalence and risk factors of postpartum posttraumatic stress disorder: a meta-analysis. Clin. Psychol. Rev. 2014;34(5):389–401. doi: 10.1016/j.cpr.2014.05.003. http://dx.doi.org/10.1016/j.cpr.2014.05.003. [DOI] [PubMed] [Google Scholar]
- Hunter RS, Kilstrom N, Kraybill EN, Loda F. Antecedents of child abuse and neglect in premature infants: a prospective study in a newborn intensive care unit. Pediatrics. 1978;61(4):629–635. [PubMed] [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Arch. Gen. Psychiatry. 1995;52(12):1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- Koenen KC, Widom CS. A prospective study of sex differences in the lifetime risk of posttraumatic stress disorder among abused and neglected children grown up. J. Traum. Stress. 2009;22(6):566–574. doi: 10.1002/jts.20478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lang AJ, Gartstein MA, Rodgers CS, Lebeck MM. The impact of maternal childhood abuse on parenting and infant temperament. J. Child Adolesc. Psychiatric Nurs.: Off. Publ. Assoc. Child Adolesc. Psychiatric Nurs. 2010;23(2):100–110. doi: 10.1111/j.1744-6171.2010.00229.x. http://dx.doi.org/10.1111/j.1744-6171.2010.00229.x. [DOI] [PubMed] [Google Scholar]
- Lev-Wiesel R, Daphna-Tekoah S, Hallak M. Childhood sexual abuse as a predictor of birth-related posttraumatic stress and postpartum posttraumatic stress. Child Abuse Negl. 2009;33(12):877–887. doi: 10.1016/j.chiabu.2009.05.004. http://dx.doi.org/10.1016/j.chiabu.2009.05.004. [DOI] [PubMed] [Google Scholar]
- Loseke DR, Gelles RJ, Cavanaugh MM. Current Controversies on Family Violence 2nd ed. SAGE Publications, Inc.; Thousand Oaks,CA.: 2005. [Google Scholar]
- Lovejoy MC, Graczyk PA, O'Hare E, Neuman G. Maternal depression and parenting behavior: a meta-analytic review. Clin. Psychol. Rev. 2000;20(5):561–592. doi: 10.1016/s0272-7358(98)00100-7. [DOI] [PubMed] [Google Scholar]
- Loveland Cook CA, Flick LH, Homan SM, Campbell C, McSweeney M, Gallagher ME. Posttraumatic stress disorder in pregnancy: prevalence, risk factors, and treatment. Obstet. Gynecol. 2004;103(4):710–717. doi: 10.1097/01.AOG.0000119222.40241.fb. http://dx.doi.org/10.1097/01.AOG.0000119222.40241.fb. [DOI] [PubMed] [Google Scholar]
- Mäntymaa M, Puura K, Luoma I, Latva R, Salmelin RK, Tamminen T. Shared pleasure in early mother–infant interaction: predicting lower levels of emotional and behavioral problems in the child and protecting against the influence of parental psychopathology. Infant Ment. Health J. 2015;36(2):223–237. doi: 10.1002/imhj.21505. http://dx.doi.org/10.1002/imhj.21505. [DOI] [PubMed] [Google Scholar]
- Martinez-Torteya C, Dayton CJ, Beeghly M, Seng JS, McGinnis E, Broderick A, Muzik M. Maternal parenting predicts infant biobehavioral regulation among women with a history of childhood maltreatment. Dev. Psychopathol. 2014;26(2):379–392. doi: 10.1017/S0954579414000017. http://dx.doi.org/10.1017/S0954579414000017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDonald S, Slade P, Spiby H, Iles J. Post-traumatic stress symptoms, parenting stress and mother–child relationships following childbirth and at 2 years postpartum. J. Psychosom. Obstet. Gynecol. 2011;32(3):141–146. doi: 10.3109/0167482X.2011.596962. http://dx.doi.org/10.3109/0167482X.2011.596962. [DOI] [PubMed] [Google Scholar]
- Muzik M, Bocknek EL, Broderick A, Richardson P, Rosenblum KL, Thelen K, Seng JS. Mother–infant bonding impairment across the first 6 months postpartum: the primacy of psychopathology in women with childhood abuse and neglect histories. Arch. Women's Ment. Health. 2012;16(1):29–38. doi: 10.1007/s00737-012-0312-0. http://dx.doi.org/10.1007/s00737-012-0312-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muzik M, Rosenblum KL, Alfafara EA, Schuster MM, Miller NM, Waddell RM, Kohler ES. Mom power: preliminary outcomes of a group intervention to improve mental health and parenting among high-risk mothers. Arch. Women's Mental Health. 2015;18(3):507–521. doi: 10.1007/s00737-014-0490-z. http://dx.doi.org/10.1007/s00737-014-0490-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Child Abuse and Neglect Data System (NCANDS) Report, 2013. 〈〈 http://www.acf.hhs.gov/sites/default/files/cb/cm2013.pdf〉 (downloaded 22.03.16).
- O'Hara MW, McCabe JE. Postpartum depression: current status and future directions. Annu. Rev. Clin. Psychol. 2013;9(1):379–407. doi: 10.1146/annurev-clinpsy-050212-185612. http://dx.doi.org/10.1146/annurev-clinpsy-050212-185612. [DOI] [PubMed] [Google Scholar]
- Oliver JE. Intergenerational transmission of child abuse: rates, research, and clinical implications. Am. J. Psychiatry. 1993;150(9):1315–1324. doi: 10.1176/ajp.150.9.1315. http://dx.doi.org/10.1176/ajp.150.9.1315. [DOI] [PubMed] [Google Scholar]
- Onoye JM, Shafer LA, Goebert DA, Morland LA, Matsu CR, Hamagami F. Changes in PTSD symptomatology and mental health during pregnancy and postpartum. Arch. Women's Ment. Health. 2013;16(6):453–463. doi: 10.1007/s00737-013-0365-8. http://dx.doi.org/10.1007/s00737-013-0365-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pollack MH. Comorbid anxiety and depression. J. Clin. Psychiatry. 2005;66(Suppl. 8):S22–S29. [PubMed] [Google Scholar]
- Resnick HS, Kilpatrick DG, Dansky BS, Saunders BE, Best CL. Prevalence of civilian trauma and posttraumatic stress disorder in a representative national sample of women. J. Consult. Clin. Psychol. 1993;61(6):984–991. doi: 10.1037//0022-006x.61.6.984. [DOI] [PubMed] [Google Scholar]
- Ross LE, McLean LM. Anxiety disorders during pregnancy and the postpartum period: a systematic review. J. Clin. Psychiatry. 2006;67(8):1285–1298. doi: 10.4088/jcp.v67n0818. [DOI] [PubMed] [Google Scholar]
- Schechter DS, Moser DA, Reliford A, McCaw JE, Coates SW, Turner JB, Willheim E. Negative and distorted attributions towards child, self, and primary attachment figure among posttraumatically stressed mothers: what changes with Clinician Assisted Videofeedback Exposure Sessions (CAVES). Child Psychiatry Hum. Dev. 2014;46(1):10–20. doi: 10.1007/s10578-014-0447-5. http://dx.doi.org/10.1007/s10578-014-0447-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schechter DS, Moser DA, Reliford A, McCaw JE, Coates SW, Turner JB, Willheim E. Negative and distorted attributions towards child, self, and primary attachment figure among posttraumatically stressed mothers: what changes with Clinician Assisted Videofeedback Exposure Sessions (CAVES). Child Psychiatry Hum. Dev. 2015a;46(1):10–20. doi: 10.1007/s10578-014-0447-5. http://dx.doi.org/10.1007/s10578-014-0447-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schechter DS, Suardi F, Manini A, Cordero MI, Rossignol AS, Merminod G, Serpa SR. How do maternal PTSD and alexithymia interact to impact maternal behavior? Child Psychiatry Hum. Dev. 2015b;46(3):406–417. doi: 10.1007/s10578-014-0480-4. http://dx.doi.org/10.1007/s10578-014-0480-4. [DOI] [PubMed] [Google Scholar]
- Schechter DS, Willheim E, Hinojosa C, Scholfield-Kleinman K, Turner JB, McCaw J, Myers MM. Subjective and objective measures of parent-child relationship dysfunction, child separation distress, and joint attention. Psychiatry. 2010;73(2):130–144. doi: 10.1521/psyc.2010.73.2.130. http://dx.doi.org/10.1521/psyc.2010.73.2.130. [DOI] [PubMed] [Google Scholar]
- Seng JS, Low LK, Sperlich M, Ronis DL, Liberzon I. Prevalence, trauma history, and risk for posttraumatic stress disorder among nulliparous women in maternity care. Obstet. Gynecol. 2009;114(4):839–847. doi: 10.1097/AOG.0b013e3181b8f8a2. http://dx.doi.org/10.1097/AOG.0b013e3181b8f8a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith MV, Poschman K, Cavaleri MA, Howell HB, Yonkers KA. Symptoms of posttraumatic stress disorder in a community sample of low-income pregnant women. Am. J. Psychiatry. 2006;163(5):881–884. doi: 10.1176/ajp.2006.163.5.881. http://dx.doi.org/10.1176/ajp.2006.163.5.881. [DOI] [PubMed] [Google Scholar]
- Studd J, Nappi RE. Reproductive depression. Gynecol. Endocrinol.: Off. J. Int. Soc. Gynecol. Endocrino. 2012;28(Suppl. 1):S42–S45. doi: 10.3109/09513590.2012.651932. http://dx.doi.org/10.3109/09513590.2012.651932. [DOI] [PubMed] [Google Scholar]
- Taylor S, Asmundson GJG, Carleton RN. Simple versus complex PTSD: a cluster analytic investigation. J. Anxiety Disord. 2006;20(4):459–472. doi: 10.1016/j.janxdis.2005.04.003. http://dx.doi.org/10.1016/j.janxdis.2005.04.003. [DOI] [PubMed] [Google Scholar]
- Weinberg MK, Tronick EZ. Emotional characteristics of infants associated with maternal depression and anxiety. Pediatrics. 1998;102(5 Suppl. E):S1298–S1304. [PubMed] [Google Scholar]
- Widom CS, Wilson HW. Intergenerational transmission of violence. In: Lindert J, Levav I, Lindert J, Levav I, editors. Violence and Mental Health: Its Manifold Faces. Springer Science+Business Media; New York, NY, US: 2015. pp. 27–45. [Google Scholar]