Abstract
Background
Temperament and personality traits have been suggested as endophenotypes for bipolar disorder based on several lines of evidence, including heritability. Previous work suggested an anxious-reactive factor identified across temperament and personality inventories that produced significant group discrimination and could potentially be useful in genetic analyses. We have attempted to further characterize this factor structure in a sample of bipolar patients.
Methods
A sample of 1195 subjects with bipolar I disorder was evaluated, all with complete data available. Dimension reduction across two inventories identified 18 factors explaining 39% of the variance.
Results
The two largest factors reflected affective instability and general anxiety/worry, respectively. Subsequent analyses of the clinical features associated with bipolar disorder revealed specificity for the factors in a predictable pattern. Cluster analysis of the factors identified a subgroup defined by a strong lack of general anxiety and low affective instability represented by the first two factors. The remaining subjects could be distinguished into two clusters by the presence of either more positive characteristics, including persistence/drive, spirituality, expressivity, and humor, or more negative characteristics of depression and anxiety.
Limitations
These analyses involved bipolar I subjects only and must be extended to other bipolar spectrum diagnoses, unaffected relatives, and individuals at risk.
Conclusions
These results suggest that temperament and personality measures access latent traits associated with important clinical features of bipolar disorder. By translating clinical variables into quantitative traits, we may identify subgroups of bipolar patients with distinct clinical profiles, thereby facilitating both individual treatment strategies and genetic analyses.
Keywords: bipolar disorder, temperament, personality, factor, cluster
INTRODUCTION
Bipolar disorder (BD) is a severe mood disorder characterized by cycling between the emotional extremes of mania and major depression. Even the most severe form of BD, bipolar I, is common in the population, with a lifetime prevalence of approximately 1% (Goodwin and Jamison, 2007; Merikangas et al., 2011). Studies of BD face many challenges arising from the complex genetic architecture, as well as the inherent clinical heterogeneity. Current diagnostic systems primarily define BD using categorical clinical descriptors that inadequately capture the rich spectrum of bipolar symptomology, which is more consistent with a polygenic model and implies a continuous distribution of symptoms ranging from mild to severe. The historically high rate of misdiagnosis in BD highlights this need for alternative quantitative metrics that better capture the full range of bipolar symptomology (Altamura et al., 2015; Daigneault et al., 2015; Zimmerman et al., 2008).
As alternatives, temperament and other personality traits have been proposed as potential endophenotypes for BD (Savitz and Ramesar, 2006). Temperament refers to stable, innate aspects of one’s disposition that can be measured quantitatively and that show continuous variation in the population (Goldsmith et al., 1987; von Zerssen and Akiskal, 1998). It has been suggested that temperament represents the most common expression of the genes underlying BD and that extreme variation in temperament is associated with an increased risk for illness (Akiskal, 2002; Akiskal and Pinto, 2000; Akiskal and Akiskal, 2005; Kelsoe, 2003). According to this model, temperament and personality mediate between upstream biological mechanisms and downstream clinical diagnosis and may better model the underlying genetic architecture of BD. As quantitative traits, temperament and other personality measures may also provide more sensitive predictors of specific aspects of bipolar symptomatology.
Studies have shown that traits related to emotional instability, hostility, novelty seeking, and anxiety are elevated in bipolar spectrum disorders, even in euthymia (Bagby et al., 1997; Evans et al., 2005; Nowakowska et al., 2005; Osher et al., 1996; Savitz et al., 2008a, b). Other investigations have demonstrated the utility of temperament and personality traits for detecting genetic risk factors for BD (Alliey-Rodriguez et al., 2011; Greenwood et al., 2012; Greenwood et al., 2013a; Greenwood et al., 2013b; Savitz et al., 2008c), predicting risk for bipolar spectrum disorders (DeGeorge et al., 2014), and discriminating those with BD or other mood disorders from healthy controls (Akiskal et al., 1977; Cassano et al., 1992; Evans et al., 2005; Harley et al., 2011; Kesebir et al., 2005; Loftus et al., 2008; Mendlowicz et al., 2005; Young et al., 1995). For these investigations, the Temperament Evaluation of Memphis, Pisa, Paris, and San Diego Auto-questionnaire (TEMPS-A) has been used to evaluate lifelong, milder aspects of bipolar symptomatology according to five temperaments: hyperthymic, dysthymic, cyclothymic, irritable, and anxious (Akiskal et al., 2005a; Akiskal et al., 2005b). The Temperament and Character Inventory (TCI) has also been used to evaluate personality according to four temperament domains (novelty seeking, harm avoidance, reward dependence, and persistence) and three character domains (self-directedness, cooperativeness, and self-transcendence) (Cloninger et al., 1993). One study of BD patients, their family members, and healthy controls identified an anxious-reactive factor across these two inventories that produced significant group discrimination across mood states and genetic risk categories, suggesting potential utility for genetic analyses (Evans et al., 2005).
In the present study, we explore the utility of latent temperament and personality traits in defining clinical profiles within the context of BD. By combining items across domains from these instruments, we aim to identify quantitative traits that may serve as indices for key features of illness and help refine the clinical heterogeneity associated with BD.
METHODS
Subject Ascertainment
A sample of 1195 unrelated patients with bipolar I disorder were selected from the Bipolar Genome Study (BiGS). All were of European Ancestry and derived originally from those collected as part of Wave 5 by the National Institute of Mental Health Genetics Initiative for Bipolar Disorder at 11 sites across the US. All subjects were assessed using the Diagnostic Interview for Genetic Studies (DIGS), which was combined with family informant data and medical records to arrive at best-estimate diagnoses according to DSM-IV criteria (Nurnberger et al., 1994). Detailed demographic and clinical information was available for each subject from the DIGS interview, including overall functioning as measured by the Global Assessment of Functioning (GAF). Written informed consent was obtained for all subjects according to the local institutional review boards.
Phenotypes
The TEMPS-A and TCI-125 were administered at the time of the clinical interview, and only subjects with complete data across both instruments were selected for analysis. The TEMPS-A includes a total of 109 self-rated true/false questions (110 for women) measuring subclinical affective traits and has been shown to have very good reliability, internal consistency, and stability over time (Akiskal et al., 2005a; Akiskal et al., 1998; Kawamura et al., 2010; Perugi et al., 2012; Placidi et al., 1998a; Placidi et al., 1998b), as well as significant heritability in BD families (Greenwood et al., 2013a; Savitz et al., 2008c). The TCI-125 (125-question version) is a self-administered true/false questionnaire that evaluates personality according to a psychobiological model with demonstrated reliability, internal consistency, stability over time, and heritability in both BD families and the general population (Cloninger et al., 1993; Greenwood et al., 2013a; Heath et al., 1994; Keller et al., 2005; Savitz et al., 2008c). The Wender-Utah Rating Scale (WURS) was administered to evaluate childhood features of attention-deficit disorder in three factors related to oppositional/defiant behavior, inattention and resultant problems in school, and mood features of depression and anxiety (Ward et al., 1993). The Lifetime History of Aggression (LHA) scale was also administered to evaluate total aggression according to factors related to aggression, antisocial behavior, and self-directed aggression (Coccaro et al., 1997). The majority of subjects (77%) were euthymic at the time of assessment.
Statistical Analyses
Dimension reduction was performed on the combined 235 items from the TEMPS-A and TCI-125 via exploratory factor analysis. The Kaiser-Meyer-Olkin measure of sampling adequacy was 0.93 and the significance of Bartlett’s test of sphericity was <0.001. A variety of tests and criteria were used to best determine the number of relevant factors, including Kaiser’s criterion, the scree plot elbow rule, 50% variance explained cutoff, an a priori hypothesis of a ten factor structure (Evans et al., 2005), and parallel analysis. Ultimately, the 18-factor structure proposed by parallel analysis was chosen, as the factor solution exhibited minimal complex loadings, and each factor described a cohesive, distinct trait. Furthermore, parallel analysis has been shown to be more accurate in determining the optimal number of factors relative to both Kaiser’s criterion and the scree plot test (Franklin et al., 1995). Bivariate correlations were performed between all factor pairs and confirmed their independence with negligible correlations (r<0.001). The factors were then subjected to Varimax rotation and standardization. Cronbach’s alpha (α) was used to evaluate the internal consistency of the factors, which was generally quite high, with only four factors having an α<0.7.
To validate the factor structure, we explored relationship of each factor to clinical features of BD. Correlations of the factors with quantitative variables were evaluated using Pearson’s r, and independent samples t-tests were used to assess the relationship of the factors to categorical variables. Effect sizes were calculated using Cohen’s d for factors demonstrating significant differences. We hypothesized that each factor would produce a unique and specific pattern of association across clinical descriptors. A p value threshold of 0.003 was applied to represent a 5% probability of a false positive across the 18 independent factors.
Cluster analytic methods were applied to the 18 factors to identify subgroups of patients with more similar profiles. Subjects were first subjected to hierarchical clustering via Ward’s method according to their factor scores to determine a preliminary number of clusters. Results of these initial analyses suggested 2, 3, or 6 cluster structures. Further analysis with a two-step cluster procedure using the Bayesian information criterion confirmed a 3-cluster structure. K-means clustering was then performed with 3 subgroups (k=3) to generate a final cluster solution in the 18-variable space of the factors. Comparison of the k-means cluster solution with the 3-group hierarchical cluster solution suggested good agreement (p<0.001). To allow for visualization of the subgroups, multivariate discriminant analysis was performed to summarize the variation among factors that maximally separated the subgroups identified by k-means clustering. Analysis of variance was used to compare the factors across cluster groups. All analyses were carried out in SPSS v. 20. (IBM, Armonk, NY).
RESULTS
The 18 identified factors comprised 162 items and explained 39% of the variance in BD. A description of these factors is presented in Table 1. The largest factors encompassed traits related to affective instability (factor 1) and general anxiety/worry (factor 2) and explained 5% and 3.5% of the variance, respectively. Other factors related to compassion, social anxiety, dysthymia, insecurity, hostility, persistence/drive, spirituality, expressivity, risk-taking, humor, fatigue, impulsivity, physical anxiety, sentimentality, conformity, and extravagance. Table 2 provides representative items for each factor with complete item descriptions, factor loadings, and the instrument and domain of origin for each item provided in the Table S1.
Table 1.
Summary of the 18 extracted factors from a combined analysis of all TEMPS-A and TCI-125 items.
| Extracted Factor | Eigenvalue | % Total Variance | Cumulative % Variance | # Items | Cronbach’s Alpha* |
|---|---|---|---|---|---|
| 1 | 11.782 | 5.035 | 5.035 | 25 | 0.91 |
| 2 | 8.158 | 3.486 | 8.522 | 13 | 0.91 |
| 3 | 6.619 | 2.829 | 11.350 | 15 | 0.84 |
| 4 | 6.391 | 2.731 | 14.082 | 11 | 0.87 |
| 5 | 6.096 | 2.605 | 16.687 | 11 | 0.87 |
| 6 | 5.928 | 2.533 | 19.220 | 6 | 0.75 |
| 7 | 5.643 | 2.412 | 21.632 | 10 | 0.84 |
| 8 | 5.593 | 2.390 | 24.022 | 12 | 0.78 |
| 9 | 4.821 | 2.060 | 26.083 | 11 | 0.82 |
| 10 | 4.380 | 1.872 | 27.955 | 5 | 0.75 |
| 11 | 4.222 | 1.804 | 29.759 | 7 | 0.73 |
| 12 | 3.564 | 1.523 | 31.282 | 5 | 0.65 |
| 13 | 3.284 | 1.404 | 32.686 | 6 | 0.75 |
| 14 | 3.168 | 1.354 | 34.039 | 5 | 0.64 |
| 15 | 3.137 | 1.341 | 35.380 | 7 | 0.74 |
| 16 | 2.959 | 1.264 | 36.644 | 3 | 0.49 |
| 17 | 2.955 | 1.263 | 37.907 | 7 | 0.60 |
| 18 | 2.853 | 1.219 | 39.126 | 4 | 0.81 |
Cronbach’s alpha was calculated only for items with a factor loading >0.35.
Table 2.
Description of the Extracted Factors and Representative Items
| Factor | Description | Representative Items (factor loading) |
|---|---|---|
| 1 | Affective instability |
|
| 2 | Anxiety/worry |
|
| 3 | Compassion |
|
| 4 | Social anxiety |
|
| 5 | Dysthymia |
|
| 6 | Insecurity |
|
| 7 | Hostility |
|
| 8 | Persistence/drive |
|
| 9 | Spirituality |
|
| 10 | Expressivity |
|
| 11 | Risk-taking |
|
| 12 | Humor |
|
| 13 | Fatigue |
|
| 14 | Impulsivity |
|
| 15 | Physical anxiety |
|
| 16 | Sentimentality |
|
| 17 | Conformity |
|
| 18 | Extravagance |
|
Factor loadings are indicated in parentheses. Key: Items with the indication of *neg should be interpreted in the opposite context, as they are scored in reverse on the TCI-125. Similarly, items with negative factor loadings should be interpreted as the opposite. Items with both the indication of *neg and a negative factor loading should be interpreted as written, as these designations cancel each other.
Most factors combined similar items across domains from the TEMPS-A and TCI, and all demonstrated patterns of clinical specificity, as shown in Tables 3a and 3b. Factor 1 (affective instability) comprised items related to shifts in energy, mood, and mental activation, which represent the core features of BD. This factor revealed strong relationships with rapid cycling and comorbid OCD. Significant associations with other comorbid anxiety diagnoses and suicidal ideation were also observed, and this was the only factor to reveal a correlation with age at onset of BD. Interestingly, factor 1 was also correlated with total lifetime aggression and childhood ADHD features, likely a reflection of the instability in mood and energy. Factor 2 (anxiety/worry) revealed specificity for comorbid anxiety diagnoses and childhood ADHD features, particularly those related to mood, which reflects dysthymia and anxiety. Strong associations were also observed for factor 4 (social anxiety) with comorbid social phobia and factor 9 (spirituality) with psychosis.
Table 3a.
Relationships of the Extracted Factors to Clinical Features of BD and Illness Comorbidity
| Factor | Description | Effect Size (d)
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sex | Rapid Cycle | Irritable Mania | Psychosis | Suicidal Ideation | Panic | Agoraphobia | Social Phobia | OCD | Gambling | Alcohol | ||
| 1 | Affective instability | 0.76* | 0.39 | 0.47 | 0.48 | 0.37 | 0.52* | 0.31 | ||||
| 2 | Anxiety/worry | 0.23 | 0.23 | 0.40 | ||||||||
| 3 | Compassion | 0.40 | 0.64* | 0.39 | ||||||||
| 4 | Social anxiety | |||||||||||
| 5 | Dysthymia | 0.41 | 0.26 | |||||||||
| 6 | Insecurity | 0.27 | ||||||||||
| 7 | Hostility | 0.36* | 0.32 | 0.31 | 0.35 | |||||||
| 8 | Persistence/drive | |||||||||||
| 9 | Spirituality | 0.53* | ||||||||||
| 10 | Expressivity | −0.36 | ||||||||||
| 11 | Risk-taking | |||||||||||
| 12 | Humor | 0.21 | 0.21 | |||||||||
| 13 | Fatigue | −0.35 | ||||||||||
| 14 | Impulsivity | 0.37 | 0.35 | |||||||||
| 15 | Physical anxiety | −0.43 | −0.23 | 0.47 | ||||||||
| 16 | Sentimentality | −0.47 | −0.23 | 0.29 | ||||||||
| 17 | Conformity | −0.23 | 0.22 | 0.28 | ||||||||
| 18 | Extravagance | 0.23 | 0.21 | 0.43 | 0. 32 | |||||||
Effect sizes in bold text are significant at p<0.003, reflecting a correction for multiple tests across the 18 factors. All others are significant at p<0.05. Only those with at least a small effect size (>0.2) are listed.
Indicates a medium effect size >0.5.
Note that for sex a negative effect indicates a higher factor score for females. Key: Rapid cycle = rapid cycling BD; Psychosis = the endorsement of hallucinations or delusions; Panic = panic disorder; OCD = obsessive-compulsive disorder; Gambling = pathological gambling; Alcohol = alcohol abuse or dependence.
Table 3b.
Correlations Between the Extracted Factors and Other Clinical Features
| Factor | Description | AAO | WURS | LHA | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| Oppositional Behavior | Inattention | Mood | Total | Aggression | Self-Aggression | Anti-social Behavior | Total | |||
| 1 | Affective instability | −0.25 | 0.33* | 0.28 | 0.38* | 0.40* | 0.27 | 0.27 | 0.31* | |
| 2 | Anxiety/worry | 0.23 | 0.20 | |||||||
| 3 | Compassion | −0.24 | −0.22 | −0.21 | −0.24 | |||||
| 4 | Social anxiety | |||||||||
| 5 | Dysthymia | 0.22 | ||||||||
| 6 | Insecurity | |||||||||
| 7 | Hostility | 0.35* | 0.29 | 0.46* | 0.20 | 0.43* | 0.50* | |||
| 8 | Persistence/drive | |||||||||
| 9 | Spirituality | |||||||||
| 10 | Expressivity | |||||||||
| 11 | Risk-taking | |||||||||
| 12 | Humor | |||||||||
| 13 | Fatigue | |||||||||
| 14 | Impulsivity | |||||||||
| 15 | Physical anxiety | |||||||||
| 16 | Sentimentality | |||||||||
| 17 | Conformity | |||||||||
| 18 | Extravagance | |||||||||
Correlations in bold text are significant at p<0.003, reflecting a correction for multiple tests across the 18 independent factors. Only comparisons with at least a small correlation (i.e., 0.2) are listed.
Indicates a medium correlation >0.3.
Key: AAO = age at onset of BD; WURS = Wender Utah Rating Scale measuring childhood ADHD symptoms; LHA = Lifetime History of Aggression.
Other factors produced more modest associations, yet this pattern of specificity was maintained. For example, factor 15 (physical anxiety) was associated with comorbid panic disorder and agoraphobia, factor 18 (extravagance) was associated with pathological gambling, and factor 5 (dysthymia) was associated with childhood mood features of dysthymia and anxiety. Factor 7 (hostility) was associated with irritable mania and revealed a pattern of correlations with lifetime aggression and oppositional/defiant behavior in childhood. Although modest, inverse correlations were observed between factor 3 (compassion) and lifetime aggression and oppositional/defiant behavior in childhood.
Significant gender differences were also observed for several factors, with females scoring moderately higher for traits related to expressivity, fatigue, physical anxiety, and sentimentality. To further evaluate potential gender effects, gender-stratified analyses of clinical features were performed for each factor. The observed patterns of results were consistent across genders and with the results observed in the larger combined analysis (see Tables S2a, S2b, S2c).
To assess the possible effect of current mood state on self-report and thus the resultant factor structure, we compared subjects who met criteria for current mania or depression symptoms with those that were euthymic at interview. Euthymic subjects comprised a majority (77%) of the sample and revealed significant differences for factor 1 (affective instability) only when compared with subjects who were depressed, which comprised 17% of the sample. No other group comparisons were significant, suggesting that state effects are relatively minor in this sample.
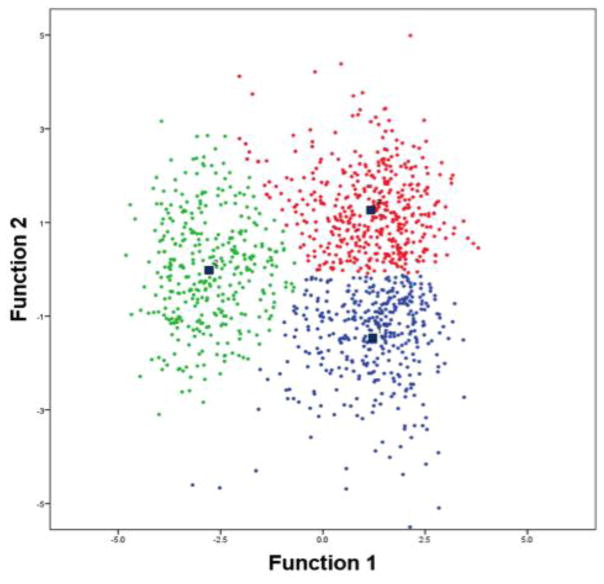
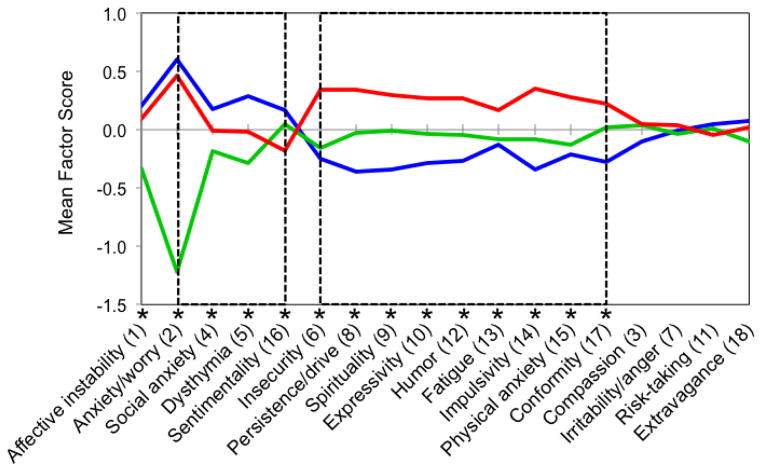
Cluster analysis of the factors suggested three distinct subgroups. Nearly all factors displayed significant group differences between the three clusters (p<0.001), with factors 2 (anxiety/worry) and 1 (affective instability) emerging as the primary and secondary drivers of the cluster solution, respectively. It is noteworthy that there was no apparent impact of gender on cluster structure, with an approximately equal distribution of males and females across the three clusters producing a non-significant group difference. To visualize these subgroups, multivariate discriminant analysis was used to reduce the 18-variable space of the factors to two discriminant functions that provided maximal group separation, as shown in Figure 1, with the first discriminant function reflecting the combination of anxiety, affective instability, and dysthymia and the second discriminant function reflecting persistence, impulsivity, spirituality, insecurity, expressivity, humor, conformity, and physical anxiety.
Figure 1.
Visualization of the three groups obtained through k-means clustering via discriminant function analysis. Cluster 1 is shown in blue, cluster 2 is shown in green, and cluster 3 is shown in red. The centroid of each group is indicated with a dark square. Discriminant function 1 represents a combination of four factors, with the largest contribution from factor 2 (anxiety/worry) and significant contributions from factors 1 (affective instability) and 5 (dysthymia). Function 2 represents a combination of the generally more “positive” factors, with significant contributions from factors 6 (insecurity), 8, (persistence), 9 (spirituality), 10 (expressivity), 12 (humor), 14 (impulsivity), 15 (physical anxiety), and 17 (conformity).
The most prominent subgroup, cluster 2, was characterized by low anxiety and less affective instability. This cluster revealed a dramatically different temperament and personality profile compared with the other clusters (p<0.001), as shown in Figure 2. As might be expected, subjects in this cluster also displayed a later age at onset, higher overall functioning, and lower rates of rapid cycling, suicide attempt, lifetime aggression, and childhood ADHD features (p<0.001). This clinical profile suggests that cluster 2 may comprise subjects with a relatively stable course of BD.
Figure 2.
The three clusters derived from k-means clustering are shown according to group mean scores across all 18 factors. Cluster 1 is shown in blue, cluster 2 is shown in green, and cluster 3 is shown in red. Factors are arranged so as to emphasize the unique personality profiles observed for each cluster. Nearly all factors displayed significant differences between all three groups (p<0.003), as indicated by an asterisk (*).
In addition to the low anxiety group, two other distinct clusters (1 and 3) emerged that shared a profile of general anxiety and affective instability. However, as shown in Figure 2, these clusters could be distinguished by significant differences (p<0.001) for “negative” factors related to other measures of anxiety and dysthymia (cluster 1 higher) and more “positive” factors related to persistence, spirituality, expressivity, and humor (cluster 3 higher). The factor profiles of these groups are somewhat reflective of depression and mania, respectively. Interestingly, these clusters differed most significantly for factor 9 (spirituality), for which cluster 3 was higher. An evaluation of group differences across clinical features also revealed a significantly higher proportion of psychotic features in cluster 3.
To further examine the utility of quantitative traits in predicting clinical course, we compared the low anxiety subgroup obtained through factor and cluster analysis to a categorical grouping of subjects according to the presence or absence of anxiety disorder comorbidity (e.g., OCD, panic disorder, agoraphobia, or social phobia). An evaluation of group differences across other clinical features produced the same trend in the categorical grouping as observed in the cluster analysis: BD subjects without anxiety comorbidity appear to have a milder course of illness characterized by a later age at onset, higher overall functioning, and lower rates of rapid cycling and suicide attempt, lifetime aggression and childhood ADHD features (p<0.001). While both methods produced a subgroup with a milder course of illness, the quality and resolution of the low anxiety group obtained through clustering was superior. Although more than 30% of subjects within the cluster-defined low anxiety group were comorbid for at least one anxiety disorder, this group was much smaller (N=359) than the group defined by a complete lack of anxiety comorbidity (N=623) and reflected an even milder clinical profile when the same clinical characteristics as above were considered.
DISCUSSION
By combining items across two standard inventories of temperament and personality through dimension reduction, we have defined quantitative measures related to specific aspects of BD symptomatology. While the TEMPS-A and TCI-125 differ in their origins and intent, our results suggest that they are complementary and can be refined into smaller, independent factors, many of which incorporate items across domains and from both inventories. These results indicate that the combination of the TEMPS-A and TCI better captures the broad spectrum of temperament and personality than either alone and that extracted factors can be used to predict clinical features and course of illness in BD. As such, the factors effectively translate categorical clinical variables into continuous, quantitative variables that capture more variation in BD and are better suited to exploratory data analysis. These results thus demonstrate the utility of temperament and personality traits in quantitatively describing BD and suggest that BD exists at the extreme of continuously varying temperament and personality traits.
Although more factors were obtained than original domains from the TEMPS-A and TCI (18 vs. 12), the factors displayed increased specificity compared to the domains. Prior to dimension reduction, the domain scores of the TEMPS-A and TCI produced moderate to large correlations, indicating some degree of redundancy and similarity, as has been suggested by others (Maremmani et al., 2005) and detailed for this sample in Table S3. Following dimension reduction, however, the derived factors were completely uncorrelated (r<0.001), with each factor representing either an amalgam of items across TEMPS-A and TCI domains or a subset of items from a single domain. As a result, each factor cohesively described a single trait that was more specific in content than the domains of either questionnaire. For example, the dysthymia factor comprised questions from six different domains across the TEMPS-A and TCI, each reflecting a depressive, negative outlook on life. By contrast, the physical anxiety factor contained only the subset of items from the TEMPS-A anxious domain that describe physiological symptoms associated with panic and stress. Indeed, the fact that dimension reduction did not reproduce the original domains but rather more specific factors, many of which span domains, suggests the existence of distinct aspects of temperament and personality nestled within the broader domains of the TEMPS-A and TCI.
Another aspect of this specificity is reflected in the observed correlations with clinical features. For example, rapid cycling in BD is diagnosed when four or more episodes of mania or depression occur within a year. This pattern of frequent episodes typically predicts a more severe course of illness. Unsurprisingly, the affective instability factor, which reflects a pattern of mood and energy fluctuations, displayed the largest and most significant difference between subjects with and without rapid cycling (d=0.73, p<1×10−29). Such trends were observed for all clinical features considered in our study, and the more specific and proximate in content a factor was to a clinical feature, the stronger and more significant the observed association. Furthermore, the factors showed no differences by potential confounding variables, such as age and years of education. Although significant relationships with gender were observed for selected factors in a predictable pattern, gender-stratified analyses produced consistent patterns of associations with clinical features across the factors. Thus, the factors, as distinct aspects of personality, were sensitive to both the presence and magnitude of their associations with related clinical features and generally robust to outside perturbation.
The affective instability reflected in factor 1 seems to comprise the core features of illness, with high scores associated with key clinical features, including an earlier age at onset, ADHD symptoms in childhood, and increased aggression. An earlier age at onset of BD symptoms is associated with a more severe course of illness (Coryell et al., 2013; Oostervink et al., 2015; Suominen et al., 2007). Similarly, ADHD is highly comorbid with BD (Karaahmet et al., 2013; Perroud et al., 2014), and the presence of ADHD symptoms in childhood is associated with an earlier age of onset of BD (Jerrell et al., 2014; Wozniak et al., 1995) and a poor prognosis (Asherson et al., 2014). BD is also associated with heightened levels of aggression (Ballester et al., 2014). Higher scores for the affective instability factor thus replicate these clinical associations and predict a more severe course of illness.
These results are not entirely unprecedented. Previous investigations of temperament and personality domains in bipolar spectrum disorders have revealed associations with clinical course, relapse rate, suicide attempt, neurocognitive functioning, attachment, resilience, and response to antidepressants (Cassano et al., 1989; Harnic et al., 2014; Higier et al., 2014; Kesebir et al., 2015; Koukopoulos et al., 1983; Perugi et al., 2012; Rihmer et al., 2010; Sarisoy et al., 2012). Quantitative measurements of temperament and personality have also proved useful for gene identification in BD (Alliey-Rodriguez et al., 2011; Greenwood et al., 2013a; Greenwood et al., 2013b; Savitz et al., 2008c). Our study builds upon these previous findings by decomposing the broad domains of temperament and personality into distinct, well-defined factors that significantly capture clinical features of BD in a quantitative manner.
Cluster analysis of the factor scores suggested the existence of three distinct subgroups. The cluster structure was primarily driven by the anxiety/worry factor, which exhibited the largest inter-group and smallest intra-group differences. A low anxiety group emerged with a clinical profile that predicted a milder course of illness characterized by higher functioning, reduced comorbidity, less aggression, and fewer childhood ADHD symptoms. The other two groups revealed profiles generally reflective of depression (cluster 1) and hypomania (cluster 3). While these groups differed across multiple factors, one of the more prominent differences was observed for the factor related to spirituality, which reflects a subset of the TCI Self-Transcendence domain. Not only did cluster 3 produce significantly higher factor scores, a higher proportion of this group had comorbid psychotic features. This is consistent with previous findings that implicate high Self-Transcendence with increased psychotic symptoms in both BD and schizophrenia (Cortes et al., 2009; Guillem et al., 2002; Smith et al., 2008).
Our findings are also consistent with previous studies that have noted the high comorbidity of anxiety disorders in BD (Bauer et al., 2005; Otto et al., 2006; Pavlova et al., 2015). In the context of BD, anxiety is associated with a more severe course of illness (Boylan et al., 2004), including an earlier age at onset (Bauer et al., 2005) and increased suicide ideation and attempt (Dilsaver et al., 2006; Schaffer et al., 2015; Young et al., 1993). Anxiety is also associated with childhood ADHD symptoms (Jerrell et al., 2014; Wozniak et al., 1995) and an increased risk for developing BD (Perich et al., 2015). Furthermore, anxiety has also been observed to mediate between perfectionist, goal-oriented cognitive styles and increased depressive and manic symptoms in BD subjects (Corry et al., 2013). The results presented here further suggest that a quantitatively defined anxious temperament is superior to anxiety disorder comorbidity in predicting course of illness severity. Taken together, these findings suggest that an anxious temperament acts as an activation factor in BD, where increased levels of anxiety allow for greater expression of the BD phenotype.
A previous combined factor analysis of the TEMPS-A and TCI produced a primary anxious/reactive factor in a sample of BD probands, unaffected relatives, relatives with major depressive disorder (MDD), and healthy controls (Evans et al., 2005). This factor appeared promising as a predictor of risk, based on its ability to significantly discriminate between healthy control subjects and unaffected relatives, who are at a higher risk for BD due to shared genetic factors (Craddock and Jones, 1999; McGuffin et al., 2003). This factor combines items from first two factors identified here (affective instability and anxiety/worry) in a sample solely comprised of subjects with bipolar I disorder. Our findings replicate and extend these findings into more cohesive and specific traits within the context of BD that demonstrate a clear relationship with clinical features.
Our data further suggest that clustering by factors provides increased resolution and specificity compared with groupings based on clinical variables. The low anxiety group identified via clustering of factor scores was much smaller than the group of patients lacking anxiety comorbidity and displayed an even milder clinical profile. Furthermore, grouping by anxiety disorder comorbidity required a priori knowledge that anxiety is important in defining the course of illness in BD, as well as the assumption of two groups defined by this comorbidity. By contrast, clustering according to quantitative measurements of personality and temperament allowed for a data-driven approach that identified two other distinct subgroups of potential relevance to BD, in addition to a low anxiety subgroup. The quantitative nature of the factors also allowed for an assessment of inter-group differences and intra-group cohesion among clusters, ultimately indicating which factors were most important. Thus, while both methods confirmed the existence of a low anxiety group with a milder course of illness, the quantitative method was data-driven, required fewer assumptions, and captured more information. This suggests that quantitative measurements of personality and temperament may be superior to clinically defined categorical groupings in detecting distinct subgroups in BD.
There are several limitations to this study that should be considered. One possible limitation is the sole use of subjects with bipolar I disorder because TEMPS-A and TCI data was not available for control subjects. However, this has enabled us to examine temperament and personality traits within the context of BD and their relationships to important clinical features. While the TEMPS-A and TCI are designed to measure lifelong characteristics and demonstrate good stability over time, it is possible that the self-assessment might be influenced by a subject’s mood state at the time of testing. Yet, euthymic subjects comprised the majority of the sample, and an evaluation of current mood state suggested a minimal impact on the factor structure. Finally, it must be noted that cluster analysis is an open-ended approximation process, with many possible, equally valid ways of clustering a sample. Furthermore, the k-means clustering method used is sensitive to the order of subjects; however, the low-anxiety group remained stable across multiple iterations. The cluster solution also demonstrated good concordance with a 3-cluster structure arrived at through hierarchical clustering, lending confidence to the results.
It should be noted that these results represent exploratory analyses that make no assertions as to the causal relationships between personality, temperament, mood, and the clinical features of BD. Indeed, it is outside of the scope of this study to definitively establish such relationships. Regardless of causality, our results demonstrate that measures of temperament and personality access latent traits in BD that are significantly and specifically associated with important clinical features of illness, effectively translating clinical variables into a quantitative traits. The anxiety factor identified here was a better predictor of illness severity than anxiety disorder comorbidity, and the affective instability factor captured key elements of BD that may also predict illness severity. While these results demonstrate the utility and promise of temperament and personality traits as quantitative descriptors of BD, replication and extension to other BD spectrum diagnoses and individuals at risk is needed.
Supplementary Material
HIGHLIGHTS.
A factor analysis was performed across the TEMPS-A and TCI in bipolar patients.
The two largest factors reflected affective instability and anxiety.
All factors revealed specific associations with clinical features.
Cluster analysis identified three groups of patients with specific profiles.
Temperament and personality measures may predict clinical course.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Akiskal HS. The bipolar spectrum--the shaping of a new paradigm in psychiatry. Curr Psychiatry Rep. 2002;4:1–3. doi: 10.1007/s11920-002-0001-1. [DOI] [PubMed] [Google Scholar]
- Akiskal HS, Akiskal KK, Haykal RF, Manning JS, Connor PD. TEMPS-A: progress towards validation of a self-rated clinical version of the Temperament Evaluation of the Memphis, Pisa, Paris, and San Diego Autoquestionnaire. J Affect Disord. 2005a;85:3–16. doi: 10.1016/j.jad.2004.12.001. [DOI] [PubMed] [Google Scholar]
- Akiskal HS, Djenderedjian AM, Rosenthal RH, Khani MK. Cyclothymic disorder: validating criteria for inclusion in the bipolar affective group. Am J Psychiatry. 1977;134:1227–1233. doi: 10.1176/ajp.134.11.1227. [DOI] [PubMed] [Google Scholar]
- Akiskal HS, Mendlowicz MV, Jean-Louis G, Rapaport MH, Kelsoe JR, Gillin JC, Smith TL. TEMPS-A: validation of a short version of a self-rated instrument designed to measure variations in temperament. J Affect Disord. 2005b;85:45–52. doi: 10.1016/j.jad.2003.10.012. [DOI] [PubMed] [Google Scholar]
- Akiskal HS, Pinto O. Soft bipolar spectrum: footnotes to Kraepelin on the interface of hypomania, temperament and depression. In: Marneros A, Angst J, editors. Bipolar Disorders: 100 Years after Manic-depressive Insanity. Kluwer Academic; Dordrecht: 2000. pp. 37–62. [Google Scholar]
- Akiskal HS, Placidi GF, Maremmani I, Signoretta S, Liguori A, Gervasi R, Mallya G, Puzantian VR. TEMPS-I: delineating the most discriminant traits of the cyclothymic, depressive, hyperthymic and irritable temperaments in a nonpatient population. J Affect Disord. 1998;51:7–19. doi: 10.1016/s0165-0327(98)00152-9. [DOI] [PubMed] [Google Scholar]
- Akiskal KK, Akiskal HS. The theoretical underpinnings of affective temperaments: implications for evolutionary foundations of bipolar disorder and human nature. J Affect Disord. 2005;85:231–239. doi: 10.1016/j.jad.2004.08.002. [DOI] [PubMed] [Google Scholar]
- Alliey-Rodriguez N, Zhang D, Badner JA, Lahey BB, Zhang X, Dinwiddie S, Romanos B, Plenys N, Liu C, Gershon ES. Genome-wide association study of personality traits in bipolar patients. Psychiatr Genet. 2011;21:190–194. doi: 10.1097/YPG.0b013e3283457a31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Altamura AC, Buoli M, Caldiroli A, Caron L, Cumerlato Melter C, Dobrea C, Cigliobianco M, Zanelli Quarantini F. Misdiagnosis, duration of untreated illness (DUI) and outcome in bipolar patients with psychotic symptoms: A naturalistic study. J Affect Disord. 2015;182:70–75. doi: 10.1016/j.jad.2015.04.024. [DOI] [PubMed] [Google Scholar]
- Asherson P, Young AH, Eich-Hochli D, Moran P, Porsdal V, Deberdt W. Differential diagnosis, comorbidity, and treatment of attention-deficit/hyperactivity disorder in relation to bipolar disorder or borderline personality disorder in adults. Curr Med Res Opin. 2014;30:1657–1672. doi: 10.1185/03007995.2014.915800. [DOI] [PubMed] [Google Scholar]
- Bagby RM, Bindseil KD, Schuller DR, Rector NA, Young LT, Cooke RG, Seeman MV, McCay EA, Joffe RT. Relationship between the five-factor model of personality and unipolar, bipolar and schizophrenic patients. Psychiatry Res. 1997;70:83–94. doi: 10.1016/s0165-1781(97)03096-5. [DOI] [PubMed] [Google Scholar]
- Ballester J, Goldstein B, Goldstein TR, Yu H, Axelson D, Monk K, Hickey MB, Diler RS, Sakolsky DJ, Sparks G, Iyengar S, Kupfer DJ, Brent DA, Birmaher B. Prospective longitudinal course of aggression among adults with bipolar disorder. Bipolar Disord. 2014;16:262–269. doi: 10.1111/bdi.12168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauer MS, Altshuler L, Evans DR, Beresford T, Williford WO, Hauger R, Team VACS. Prevalence and distinct correlates of anxiety, substance, and combined comorbidity in a multi-site public sector sample with bipolar disorder. J Affect Disord. 2005;85:301–315. doi: 10.1016/j.jad.2004.11.009. [DOI] [PubMed] [Google Scholar]
- Boylan KR, Bieling PJ, Marriott M, Begin H, Young LT, MacQueen GM. Impact of comorbid anxiety disorders on outcome in a cohort of patients with bipolar disorder. J Clin Psychiatry. 2004;65:1106–1113. doi: 10.4088/jcp.v65n0813. [DOI] [PubMed] [Google Scholar]
- Cassano GB, Akiskal HS, Musetti L, Perugi G, Soriani A, Mignani V. Psychopathology, temperament, and past course in primary major depressions. 2. Toward a redefinition of bipolarity with a new semistructured interview for depression. Psychopathology. 1989;22:278–288. doi: 10.1159/000284608. [DOI] [PubMed] [Google Scholar]
- Cassano GB, Akiskal HS, Savino M, Musetti L, Perugi G. Proposed subtypes of bipolar II and related disorders: with hypomanic episodes (or cyclothymia) and with hyperthymic temperament. J Affect Disord. 1992;26:127–140. doi: 10.1016/0165-0327(92)90044-7. [DOI] [PubMed] [Google Scholar]
- Cloninger CR, Svrakic DM, Przybeck TR. A psychobiological model of temperament and character. Arch Gen Psychiatry. 1993;50:975–990. doi: 10.1001/archpsyc.1993.01820240059008. [DOI] [PubMed] [Google Scholar]
- Coccaro EF, Berman ME, Kavoussi RJ. Assessment of life history of aggression: development and psychometric characteristics. Psychiatry Res. 1997;73:147–157. doi: 10.1016/s0165-1781(97)00119-4. [DOI] [PubMed] [Google Scholar]
- Corry J, Green M, Roberts G, Frankland A, Wright A, Lau P, Loo C, Breakspear M, Mitchell PB. Anxiety, stress and perfectionism in bipolar disorder. J Affect Disord. 2013;151:1016–1024. doi: 10.1016/j.jad.2013.08.029. [DOI] [PubMed] [Google Scholar]
- Cortes MJ, Valero J, Gutierrez-Zotes JA, Hernandez A, Moreno L, Jariod M, Martorell L, Vilella E, Labad A. Psychopathology and personality traits in psychotic patients and their first-degree relatives. Eur Psychiatry. 2009;24:476–482. doi: 10.1016/j.eurpsy.2009.06.002. [DOI] [PubMed] [Google Scholar]
- Coryell W, Fiedorowicz J, Leon AC, Endicott J, Keller MB. Age of onset and the prospectively observed course of illness in bipolar disorder. J Affect Disord. 2013;146:34–38. doi: 10.1016/j.jad.2012.08.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Craddock N, Jones I. Genetics of bipolar disorder. J Med Genet. 1999;36:585–594. doi: 10.1136/jmg.36.8.585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daigneault A, Duclos C, Saury S, Paquet J, Dumont D, Beaulieu S. Diagnosis of bipolar disorder in primary and secondary care: what have we learned over a 10-year period? J Affect Disord. 2015;174:225–232. doi: 10.1016/j.jad.2014.10.057. [DOI] [PubMed] [Google Scholar]
- DeGeorge DP, Walsh MA, Barrantes-Vidal N, Kwapil TR. A three-year longitudinal study of affective temperaments and risk for psychopathology. J Affect Disord. 2014;164:94–100. doi: 10.1016/j.jad.2014.04.006. [DOI] [PubMed] [Google Scholar]
- Dilsaver SC, Akiskal HS, Akiskal KK, Benazzi F. Dose-response relationship between number of comorbid anxiety disorders in adolescent bipolar/unipolar disorders, and psychosis, suicidality, substance abuse and familiality. J Affect Disord. 2006;96:249–258. doi: 10.1016/j.jad.2006.07.008. [DOI] [PubMed] [Google Scholar]
- Evans L, Akiskal HS, Keck PE, Jr, McElroy SL, Sadovnick AD, Remick RA, Kelsoe JR. Familiality of temperament in bipolar disorder: support for a genetic spectrum. J Affect Disord. 2005;85:153–168. doi: 10.1016/j.jad.2003.10.015. [DOI] [PubMed] [Google Scholar]
- Franklin SB, Gibson DJ, Robertson PA, Pohlmann JT, Fralish JS. Parallel analysis - a method for determining significant principal components. J Veg Sci. 1995;6:99–106. [Google Scholar]
- Goldsmith HH, Buss AH, Plomin R, Rothbart MK, Thomas A, Chess S, Hinde RA, McCall RB. Roundtable: what is temperament? Four approaches. Child Dev. 1987;58:505–529. [PubMed] [Google Scholar]
- Goodwin FK, Jamison KR. Manic-depressive illness: Bipolar disorders and recurrent depression. Oxford University Press; New York: 2007. [Google Scholar]
- Greenwood TA, Akiskal HS, Akiskal KK, Study BG, Kelsoe JR. Genome-wide association study of temperament in bipolar disorder reveals significant associations with three novel Loci. Biol Psychiatry. 2012;72:303–310. doi: 10.1016/j.biopsych.2012.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenwood TA, Badner JA, Byerley W, Keck PE, McElroy SL, Remick RA, Sadovnick AD, Akiskal HS, Kelsoe JR. Heritability and genome-wide SNP linkage analysis of temperament in bipolar disorder. J Affect Disord. 2013a;150:1031–1040. doi: 10.1016/j.jad.2013.05.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenwood TA, Badner JA, Byerley W, Keck PE, McElroy SL, Remick RA, Sadovnick AD, Kelsoe JR. Heritability and genome-wide SNP linkage analysis of personality in bipolar disorder. J Affect Disord. 2013b;151:748–755. doi: 10.1016/j.jad.2013.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guillem F, Bicu M, Semkovska M, Debruille JB. The dimensional symptom structure of schizophrenia and its association with temperament and character. Schizophr Res. 2002;56:137–147. doi: 10.1016/s0920-9964(01)00257-2. [DOI] [PubMed] [Google Scholar]
- Harley JA, Wells JE, Frampton CM, Joyce PR. Bipolar Disorder and the TCI: Higher Self-Transcendence in Bipolar Disorder Compared to Major Depression. Depress Res Treat. 2011;2011:529638. doi: 10.1155/2011/529638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harnic D, Pompili M, Innamorati M, Erbuto D, Lamis DA, Bria P, Girardi P, Janiri L. Affective temperament and attachment in adulthood in patients with Bipolar Disorder and Cyclothymia. Compr Psychiatry. 2014;55:999–1006. doi: 10.1016/j.comppsych.2013.12.006. [DOI] [PubMed] [Google Scholar]
- Heath AC, Cloninger CR, Martin NG. Testing a model for the genetic structure of personality: a comparison of the personality systems of Cloninger and Eysenck. J Pers Soc Psychol. 1994;66:762–775. doi: 10.1037//0022-3514.66.4.762. [DOI] [PubMed] [Google Scholar]
- Higier RG, Jimenez AM, Hultman CM, Borg J, Roman C, Kizling I, Larsson H, Cannon TD. Enhanced neurocognitive functioning and positive temperament in twins discordant for bipolar disorder. Am J Psychiatry. 2014;171:1191–1198. doi: 10.1176/appi.ajp.2014.13121683. [DOI] [PubMed] [Google Scholar]
- Jerrell JM, McIntyre RS, Park YM. Correlates of incident bipolar disorder in children and adolescents diagnosed with attention-deficit/hyperactivity disorder. J Clin Psychiatry. 2014;75:e1278–1283. doi: 10.4088/JCP.14m09046. [DOI] [PubMed] [Google Scholar]
- Karaahmet E, Konuk N, Dalkilic A, Saracli O, Atasoy N, Kurcer MA, Atik L. The comorbidity of adult attention-deficit/hyperactivity disorder in bipolar disorder patients. Compr Psychiatry. 2013;54:549–555. doi: 10.1016/j.comppsych.2012.11.005. [DOI] [PubMed] [Google Scholar]
- Kawamura Y, Akiyama T, Shimada T, Minato T, Umekage T, Noda Y, Ukawa K, Hashidume C, Sakai Y, Otowa T, Sasaki T, Akiskal HS. Six-year stability of affective temperaments as measured by TEMPS-A. Psychopathology. 2010;43:240–247. doi: 10.1159/000313522. [DOI] [PubMed] [Google Scholar]
- Keller MC, Coventry WL, Heath AC, Martin NG. Widespread evidence for non-additive genetic variation in Cloninger’s and Eysenck’s personality dimensions using a twin plus sibling design. Behav Genet. 2005;35:707–721. doi: 10.1007/s10519-005-6041-7. [DOI] [PubMed] [Google Scholar]
- Kelsoe JR. Arguments for the genetic basis of the bipolar spectrum. J Affect Disord. 2003;73:183–197. doi: 10.1016/s0165-0327(02)00323-3. [DOI] [PubMed] [Google Scholar]
- Kesebir S, Unubol B, Tatlidil Yaylaci E, Gundogar D, Unubol H. Impact of childhood trauma and affective temperament on resilience in bipolar disorder. International journal of bipolar disorders. 2015;3:3. doi: 10.1186/s40345-015-0023-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kesebir S, Vahip S, Akdeniz F, Yuncu Z, Alkan M, Akiskal H. Affective temperaments as measured by TEMPS-A in patients with bipolar I disorder and their first-degree relatives: a controlled study. J Affect Disord. 2005;85:127–133. doi: 10.1016/j.jad.2003.10.013. [DOI] [PubMed] [Google Scholar]
- Koukopoulos A, Caliari B, Tundo A, Minnai G, Floris G, Reginaldi D, Tondo L. Rapid cyclers, temperament, and antidepressants. Compr Psychiatry. 1983;24:249–258. doi: 10.1016/0010-440x(83)90076-7. [DOI] [PubMed] [Google Scholar]
- Loftus ST, Garno JL, Jaeger J, Malhotra AK. Temperament and character dimensions in bipolar I disorder: a comparison to healthy controls. J Psychiatr Res. 2008;42:1131–1136. doi: 10.1016/j.jpsychires.2007.11.005. [DOI] [PubMed] [Google Scholar]
- Maremmani I, Akiskal HS, Signoretta S, Liguori A, Perugi G, Cloninger R. The relationship of Kraepelian affective temperaments (as measured by TEMPS-I) to the tridimensional personality questionnaire (TPQ) J Affect Disord. 2005;85:17–27. doi: 10.1016/S0165-0327(03)00099-5. [DOI] [PubMed] [Google Scholar]
- McGuffin P, Rijsdijk F, Andrew M, Sham P, Katz R, Cardno A. The heritability of bipolar affective disorder and the genetic relationship to unipolar depression. Arch Gen Psychiatry. 2003;60:497–502. doi: 10.1001/archpsyc.60.5.497. [DOI] [PubMed] [Google Scholar]
- Mendlowicz MV, Jean-Louis G, Kelsoe JR, Akiskal HS. A comparison of recovered bipolar patients, healthy relatives of bipolar probands, and normal controls using the short TEMPS-A. J Affect Disord. 2005;85:147–151. doi: 10.1016/j.jad.2004.01.012. [DOI] [PubMed] [Google Scholar]
- Merikangas KR, Jin R, He JP, Kessler RC, Lee S, Sampson NA, Viana MC, Andrade LH, Hu C, Karam EG, Ladea M, Medina-Mora ME, Ono Y, Posada-Villa J, Sagar R, Wells JE, Zarkov Z. Prevalence and correlates of bipolar spectrum disorder in the world mental health survey initiative. Arch Gen Psychiatry. 2011;68:241–251. doi: 10.1001/archgenpsychiatry.2011.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nowakowska C, Strong CM, Santosa CM, Wang PW, Ketter TA. Temperamental commonalities and differences in euthymic mood disorder patients, creative controls, and healthy controls. J Affect Disord. 2005;85:207–215. doi: 10.1016/j.jad.2003.11.012. [DOI] [PubMed] [Google Scholar]
- Nurnberger JI, Jr, Blehar MC, Kaufmann CA, York-Cooler C, Simpson SG, Harkavy-Friedman J, Severe JB, Malaspina D, Reich T. Diagnostic interview for genetic studies. Rationale, unique features, and training. NIMH Genetics Initiative. Arch Gen Psychiatry. 1994;51:849–859. doi: 10.1001/archpsyc.1994.03950110009002. discussion 863–844. [DOI] [PubMed] [Google Scholar]
- Oostervink F, Nolen WA, Kok RM, Board EA. Two years’ outcome of acute mania in bipolar disorder: different effects of age and age of onset. Int J Geriatr Psychiatry. 2015;30:201–209. doi: 10.1002/gps.4128. [DOI] [PubMed] [Google Scholar]
- Osher Y, Cloninger CR, Belmaker RH. TPQ in euthymic manic-depressive patients. J Psychiatr Res. 1996;30:353–357. doi: 10.1016/0022-3956(96)00023-4. [DOI] [PubMed] [Google Scholar]
- Otto MW, Simon NM, Wisniewski SR, Miklowitz DJ, Kogan JN, Reilly-Harrington NA, Frank E, Nierenberg AA, Marangell LB, Sagduyu K, Weiss RD, Miyahara S, Thas ME, Sachs GS, Pollack MH Investigators SB. Prospective 12-month course of bipolar disorder in out-patients with and without comorbid anxiety disorders. Br J Psychiatry. 2006;189:20–25. doi: 10.1192/bjp.bp.104.007773. [DOI] [PubMed] [Google Scholar]
- Pavlova B, Perlis RH, Alda M, Uher R. Lifetime prevalence of anxiety disorders in people with bipolar disorder: a systematic review and meta-analysis. Lancet Psychiatry. 2015;2:710–717. doi: 10.1016/S2215-0366(15)00112-1. [DOI] [PubMed] [Google Scholar]
- Perich T, Lau P, Hadzi-Pavlovic D, Roberts G, Frankland A, Wright A, Green M, Breakspear M, Corry J, Radlinska B, McCormack C, Joslyn C, Levy F, Lenroot R, Nurnberger JI, Jnr, Mitchell PB. What clinical features precede the onset of bipolar disorder? J Psychiatr Res. 2015;62:71–77. doi: 10.1016/j.jpsychires.2015.01.017. [DOI] [PubMed] [Google Scholar]
- Perroud N, Cordera P, Zimmermann J, Michalopoulos G, Bancila V, Prada P, Dayer A, Aubry JM. Comorbidity between attention deficit hyperactivity disorder (ADHD) and bipolar disorder in a specialized mood disorders outpatient clinic. J Affect Disord. 2014;168:161–166. doi: 10.1016/j.jad.2014.06.053. [DOI] [PubMed] [Google Scholar]
- Perugi G, Toni C, Maremmani I, Tusini G, Ramacciotti S, Madia A, Fornaro M, Akiskal HS. The influence of affective temperaments and psychopathological traits on the definition of bipolar disorder subtypes: a study on bipolar I Italian national sample. J Affect Disord. 2012;136:e41–49. doi: 10.1016/j.jad.2009.12.027. [DOI] [PubMed] [Google Scholar]
- Placidi GF, Maremmani I, Signoretta S, Liguori A, Akiskal HS. A prospective study of stability and change over 2 years of affective temperaments in 14–18 year-old Italian high school students. J Affect Disord. 1998a;51:199–208. doi: 10.1016/s0165-0327(98)00182-7. [DOI] [PubMed] [Google Scholar]
- Placidi GF, Signoretta S, Liguori A, Gervasi R, Maremmani I, Akiskal HS. The semi-structured affective temperament interview (TEMPS-I). Reliability and psychometric properties in 1010 14–26-year old students. J Affect Disord. 1998b;47:1–10. doi: 10.1016/s0165-0327(97)00122-5. [DOI] [PubMed] [Google Scholar]
- Rihmer Z, Akiskal KK, Rihmer A, Akiskal HS. Current research on affective temperaments. Curr Opin Psychiatry. 2010;23:12–18. doi: 10.1097/YCO.0b013e32833299d4. [DOI] [PubMed] [Google Scholar]
- Sarisoy G, Kacar OF, Pazvantoglu O, Ozturk A, Korkmaz IZ, Kocamanoglu B, Boke O, Sahin AR. Temperament and character traits in patients with bipolar disorder and associations with attempted suicide. Compr Psychiatry. 2012;53:1096–1102. doi: 10.1016/j.comppsych.2012.05.002. [DOI] [PubMed] [Google Scholar]
- Savitz J, van der Merwe L, Ramesar R. Dysthymic and anxiety-related personality traits in bipolar spectrum illness. J Affect Disord. 2008a;109:305–311. doi: 10.1016/j.jad.2007.12.006. [DOI] [PubMed] [Google Scholar]
- Savitz J, van der Merwe L, Ramesar R. Hypomanic, cyclothymic and hostile personality traits in bipolar spectrum illness: a family-based study. J Psychiatr Res. 2008b;42:920–929. doi: 10.1016/j.jpsychires.2007.10.011. [DOI] [PubMed] [Google Scholar]
- Savitz J, van der Merwe L, Ramesar R. Personality endophenotypes for bipolar affective disorder: a family-based genetic association analysis. Genes Brain Behav. 2008c;7:869–876. doi: 10.1111/j.1601-183X.2008.00426.x. [DOI] [PubMed] [Google Scholar]
- Savitz JB, Ramesar RS. Personality: is it a viable endophenotype for genetic studies of bipolar affective disorder? Bipolar Disord. 2006;8:322–337. doi: 10.1111/j.1399-5618.2006.00309.x. [DOI] [PubMed] [Google Scholar]
- Schaffer A, Isometsa ET, Azorin JM, Cassidy F, Goldstein T, Rihmer Z, Sinyor M, Tondo L, Moreno DH, Turecki G, Reis C, Kessing LV, Ha K, Weizman A, Beautrais A, Chou YH, Diazgranados N, Levitt AJ, Zarate CA, Jr, Yatham L. A review of factors associated with greater likelihood of suicide attempts and suicide deaths in bipolar disorder: Part II of a report of the International Society for Bipolar Disorders Task Force on Suicide in Bipolar Disorder. Aust N Z J Psychiatry. 2015;49:1006–1020. doi: 10.1177/0004867415594428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith MJ, Cloninger CR, Harms MP, Csernansky JG. Temperament and character as schizophrenia-related endophenotypes in non-psychotic siblings. Schizophr Res. 2008;104:198–205. doi: 10.1016/j.schres.2008.06.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suominen K, Mantere O, Valtonen H, Arvilommi P, Leppamaki S, Paunio T, Isometsa E. Early age at onset of bipolar disorder is associated with more severe clinical features but delayed treatment seeking. Bipolar Disord. 2007;9:698–705. doi: 10.1111/j.1399-5618.2007.00388.x. [DOI] [PubMed] [Google Scholar]
- von Zerssen D, Akiskal HS. Personality factors in affective disorders: historical developments and current issues with special reference to the concepts of temperament and character. J Affect Disord. 1998;51:1–5. doi: 10.1016/s0165-0327(98)00151-7. [DOI] [PubMed] [Google Scholar]
- Ward MF, Wender PH, Reimherr FW. The Wender Utah Rating Scale: an aid in the retrospective diagnosis of childhood attention deficit hyperactivity disorder. Am J Psychiatry. 1993;150:885–890. doi: 10.1176/ajp.150.6.885. [DOI] [PubMed] [Google Scholar]
- Wozniak J, Biederman J, Kiely K, Ablon JS, Faraone SV, Mundy E, Mennin D. Mania-like symptoms suggestive of childhood-onset bipolar disorder in clinically referred children. J Am Acad Child Adolesc Psychiatry. 1995;34:867–876. doi: 10.1097/00004583-199507000-00010. [DOI] [PubMed] [Google Scholar]
- Young LT, Bagby RM, Cooke RG, Parker JD, Levitt AJ, Joffe RT. A comparison of Tridimensional Personality Questionnaire dimensions in bipolar disorder and unipolar depression. Psychiatry Res. 1995;58:139–143. doi: 10.1016/0165-1781(95)02684-o. [DOI] [PubMed] [Google Scholar]
- Young LT, Cooke RG, Robb JC, Levitt AJ, Joffe RT. Anxious and non-anxious bipolar disorder. J Affect Disord. 1993;29:49–52. doi: 10.1016/0165-0327(93)90118-4. [DOI] [PubMed] [Google Scholar]
- Zimmerman M, Ruggero CJ, Chelminski I, Young D. Is bipolar disorder overdiagnosed? J Clin Psychiatry. 2008;69:935–940. doi: 10.4088/jcp.v69n0608. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.