Abstract
Objective:
To identify the different subtypes of acute ischemic stroke, and estimate the frequency of various risk factors among these patients.
Methods:
In this retrospective, cross-sectional study, we reviewed the medical records of patients admitted with the diagnosis of acute ischemic stroke at King Fahd Hospital of the University, Al-Khobar, Saudi Arabia from March 2008 till December 2015. The demographic characteristics, subtypes of stroke, risk factors (hypertension, diabetes mellitus, hyperlipidemia, coronary artery disease, atrial fibrillation, valvular heart disease) and other relevant data were documented on pre-defined data sheets.
Results:
The records of 343 patients were included in the study; 64.4% were male and 35.6% were female. The mean age was 59.3+13.6 (mean+SD) years for males, and 66.8+14.9 years for females. Small vessel occlusion was the most common etiologic subtype of ischemic stroke (32.1%), followed by cardio embolic (21.9%), and large artery atherosclerosis (14.6%). The middle cerebral artery was the most commonly affected territory. Hypertension was found in 78.1%, diabetes mellitus in 62.7%, hyperlipidemia in 54.8%, and ischemic heart disease in 24.2% of patients.
Conclusion:
Small vessel occlusion was the most common etiology in our cohort. The onset of stroke at a relatively younger age group in the male population is of great concern and needs to be verified by further epidemiological studies. Adequate control of modifiable risk factors may help in reducing the disease burden caused by stroke.
Stroke is the second most common cause of death in the world after ischemic heart disease (the third only when neoplastic diseases are considered as a group).1 According to the expert consensus document of the American Heart Association and the American Stroke Association,2 the updated definition of ischemic stroke (IS) for the 21st century is an episode of neurological dysfunction caused by focal cerebral, spinal, or retinal infarction.
Approximately, 17 million people suffered a stroke in 2010.3 The number of strokes decreased by approximately 10% in the developed world, and increased by 10% in developing countries between 1990 and 2010.3 Previous studies from the Kingdom of Saudi Arabia (KSA) have shown the stroke incidence to be 30 to 40/100,000 population/year,4 with a prevalence of 186/100,000.5 Stroke is considered a major health problem leading to significant disability and mortality in the Middle East region, with an expected rising mortality rate that will double by 2030.6 Stroke has various recognized modifiable and non-modifiable risk factors. Non-modifiable risk factors are age, gender, ethnicity, heredity, and race. Modifiable risk factors include, but are not limited to hypertension, diabetes mellitus, hypercholesterolemia, atrial fibrillation, smoking, and alcoholism.7 The Kingdom of Saudi Arabia is established in the central region of the Arabian Peninsula. A stroke registry from the Eastern province of KSA4 including first ever stroke reported the following risk factors: hypertension (38%), diabetes mellitus (37%), heart disease including atrial fibrillation, ischemic heart disease, valvular heart disease, cardiomyopathy (27%), smoking (19%) and family history of stroke (14%); 69% of strokes in this registry were IS.4 Ischemic stroke has different etiologic subtypes, commonly classified as large artery atherosclerosis (LAA), cardio embolic (CE), small vessel occlusion (SVO), and stroke of other determined and undetermined etiologies. Stroke has become an alarming medical issue in KSA; yet there is a significant paucity of research in this field. The aim of this study was to determine the characteristics of acute IS and identify the frequency of various risk factors among these patients.
Methods
This retrospective, cross-sectional study was carried out at King Fahd Hospital of the University, which is a 500-bedded tertiary care, teaching and referral hospital located in Al-Khobar, KSA. The hospital provides multidisciplinary health care to the population of the Eastern province of KSA. It has an established 45 bedded neurology department with a well-organized team of consultants, registrars, and residents providing inpatient and outpatient clinical services around the clock. Thrombolysis and neurointervention services are also available at the center. The hospital operates an established electronic medical records data bank system with ICD (international classification of diseases) coding. We retrieved the records of 1320 patients through the electronic data bank system who were admitted under the neurology service from March 2008 till December 2015. Out of these, 400 were diagnosed as having ischemic cerebrovascular disease. The medical records of patients fulfilling the diagnostic criteria for acute stroke, as defined by the World Health Organization8 as rapidly developing clinical signs of focal or global disturbance of cerebral function, lasting more than 24 hours or leading to death, with no apparent cause other than that of vascular in origin were included in the study. Patients with transient ischemic attacks, old IS, cerebral venous sinus thrombosis, and hemorrhagic strokes were excluded. All patients were reviewed and assessed by a neurologist. A total of 343 records of both Saudi and non-Saudi patients were included. The demographic characteristics, subtypes of stroke, risk factors (hypertension, diabetes mellitus, hyperlipidemia, coronary artery disease, atrial fibrillation, valvular heart disease) and other relevant data were documented on pre-defined data sheets.
Ischemic stroke was classified into 5 categories: 1) LAA)/macroangiopathic, 2) SVO/microangiopathic, 3) CE, 4) stroke of other determined etiology, and 5) undetermined etiology according to TOAST (Trial of Org 10172 in Acute Stroke Treatment) classification. Anatomic localization of stroke was carried with the help of CT scan and/or MRI of the brain as total anterior circulation infarction (TACI), partial anterior circulation infarction (PACI), lacunar stroke (LAC), and posterior circulation infarction (POCI). The scans were reviewed and reported by qualified radiologists. The TACI was again sub classified as anterior cerebral artery (ACA), middle cerebral artery (MCA), and ACA along with MCA infarctions. Results of investigations such as fasting blood sugar, fasting lipid profile, electrocardiogram, echocardiogram, carotid ultrasound Doppler, magnetic resonance angiogram and conventional angiogram were also recorded.
Statistical analysis was performed using IBM SPSS Statistics for Windows, version 22 (IBM Corp., Armonk, NY, USA). Mean and standard deviation (+ SD) were computed for age and scaled data. Frequencies and percentages were calculated for categorical data. Scales variables were analyzed by Student t-test. In univariate analysis, Chi-square was used to compare between different TOAST classifications of stroke and age, gender, and risk factors. Statistical significance was defined as two-tailed with a p-value of 0.05 level or less.
Results
A total of 343 cases were identified; 221 (64.4%) were male and 122 (35.6%) were female with a male to female ratio of 1.8:1 (p-value: 0.02). The mean (+SD) age among males was 59.3+13.6 years, and 66.8+14.9 years among females (p=0.00). The most common presenting feature was hemiparesis, identified in 227 (68.8%) patients followed by speech difficulty (43%).
A plain CT scan was obtained for all patients, and an MRI was performed in some patients. In patients not showing acute lesion justifying the neurological deficit, either CT scan, or MRI was repeated on an average interval of 24-48 hours. Most patients had at least 2 CT scans performed. An ECG was performed in almost all cases, and 24 hours Holter monitoring was carried out in selected patients. Transthoracic echocardiogram was carried out in approximately 75% of cases, and trans esophageal echocardiogram in fewer (<10%) patients. A reduced ejection fraction was found in 25, clot in 10, valvular disease in 8, and cardiomyopathy in 3 cases. Carotid ultrasound Doppler studies were obtained in 60% of patients. Magnetic resonance angiography, CTA, and conventional cerebral angiogram were carried out in selected patients, and 9% of patients were found to have ipsilateral significant extra cranial artery disease (>50% stenosis) on carotid ultrasound Doppler.
The frequencies and percentages of different risk factors including hypertension, diabetes mellitus, hyperlipidemia, coronary artery disease, atrial fibrillation, smoking, and history of stoke are shown in Table 1. History of smoking was found only in 7.2% of patients, and these were active smokers.
Table 1.
Frequencies and percentages of different risk factors for all ischemic strokes.
| Risk factors | Frequency | (%) |
|---|---|---|
| Hypertension | 268 | (78.1) |
| Diabetes mellitus | 215 | (62.7) |
| Hyperlipidemia | 188 | (54.8) |
| Coronary artery disease | 83 | (24.2) |
| Atrial fibrillation | 45 | (13.1) |
| Past history of stroke | 35 | (10.2) |
| Smoking | 25 | (7.2) |
| Valvular heart disease | 8 | (2.3) |
In our study, SVO was identified as the most common subtype of stroke followed by CE and LAA subtypes. Percentages of different subtypes are shown in Figure 1. The mean age for males and females in different subtypes is shown in Figure 2. The highest male preponderance was observed in the SVO subtype (72%). The highest prevalence of hypertension and diabetes mellitus was found in SVO among all subtypes of IS. Stroke of other determined etiology was the least frequently identified subtype, and did not show any significantly associated risk factor. Frequencies and percentages of major risk factors in different etiologic subtypes are summarized in Table 2.
Figure 1.
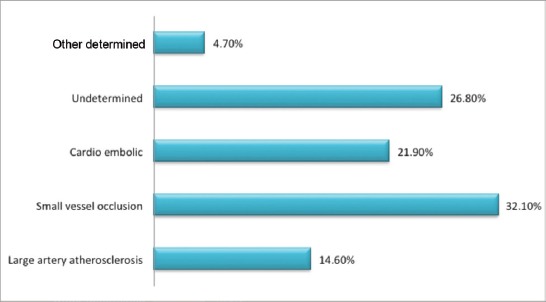
Etiologic subtypes of ischemic stroke.
Figure 2.
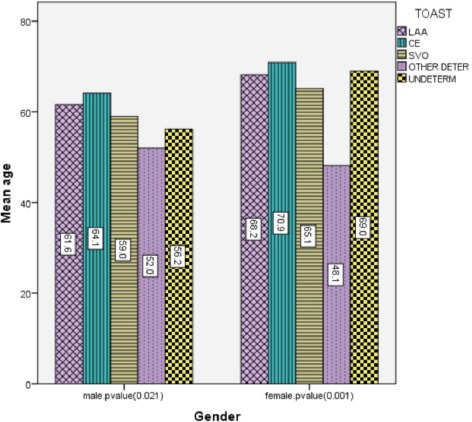
Mean age for males and females in different subtypes of stroke.
Table 2.
Distribution of risk factors among major categories of stroke.
| Risk factor | SVO | CE | LAA n (%) |
Undetermined | P-value |
|---|---|---|---|---|---|
| Hypertension | 93 (84.0) | 60 (80.0) | 39 (78) | 69 (75.0) | 0.007 |
| Diabetes mellitus | 86 (78.1) | 47 (62.4) | 30 (60) | 50 (54.9) | 0.000 |
| Hyperlipidemia | 67 (61.9) | 36 (48.0) | 27 (54) | 52 (56.5) | 0.600 |
| Ischemic heart disease | 17 (15.4) | 40 (53.3) | 10 (20) | 15 (16.3) | 0.000 |
| History of stroke | 8 (7.2) | 13 (17.3) | 6 (12) | 6 (6.5) | 0.49 |
SVO - small vessel occlusion, CE - cardio embolic, LAA - large artery atherosclerosis
One hundred and thirteen (32.9%) patients had TACI with MCA being the most affected territory (85%). The ACA was affected in 10.6%, and ACA along with MCA in 4.4% of TACI. One hundred and one patients (29.4%) had LAC, 55 (16%) had PACI, 59 (17.2%), had POCI, and 3% had both anterior and posterior circulation infarctions.
Discussion
The results of our study showed IS to be significantly more common in males than females (p=0.021). Similar observations were found in most hospital-based studies from KSA,9-11 except one from Hofuf12 in which the male to female ratio was 1:1. However, both ischemic and hemorrhagic strokes were included in all these studies. A large prospective multicenter hospital based stroke registry including only IS also showed male predominance,13 and another hospital based, retrospective study showed an equal proportion of males and females.14
The mean age for males was lower compared with females (59.3+13.6 versus 66.85+14.9). This finding is dissimilar to other studies from KSA in which stroke occurred at a younger age in women than men,9,12 but is similar to international studies.15,16
Small vessel occlusion was the most common subtype of IS in our study followed by CE and LAA. Twenty-six percent of cases were categorized to stroke of undetermined etiology because of incomplete diagnostic work up. This differs from the multicenter hospital based stroke data bank, which found the CE category as the most common subtype (25.6%), followed by LAA (20.9%), and SVO (20.5%).15 The CE subtype was also found in greater proportion than either lacunar or LAA in a prospective, single center cohort study.16 Bahou et al,17 reported 200 patients with IS from Jordan, of whom 64% had lacunar infarction.17 Stroke registries from Taiwan (National Taiwan University Stroke Registry)18 reported lacunar infarction as the most common subtype (29%), followed by CE (20%), and LAA (17%), which is similar to our study. The stroke registry from Japan also reported lacunar infarction as the most frequent subtype (54.1%) followed by CE (31.5%).19
Two prospective stroke registries on subtypes of IS from Arabian Gulf Countries (AGC)13 and Kuwait20 reported LAA as the most frequent etiologic subtype of IS. In study from the AGC, LAA was the most common category (38.1%) followed by SVO (34.7%).13 The increased frequency of SVO in our study can possibly be explained by the significantly higher prevalence of hypertension and diabetes mellitus in our patients. A retrospective study from the National Guard Community in KSA,9 including both ischemic and hemorrhagic strokes, found IS in 76.2% of patients, among which 52% had large infarcts, and 24.2% had lacunar infarcts. Other clinical studies including only IS from Arab countries reported lacunar infarction as the most common subtype,14,17 similar to our study findings. Hemiparesis/hemiplegia was the most common presenting symptom as also reported in other studies,10,21 followed by speech difficulties.10
The CE category was found to have a higher mean age compared with other categories, as also reported in another study.15 One study from KSA showed a higher mean age in the lacunar infarction subtype.9
A significant gender distribution difference was also observed in the etiologic subtype. We found the highest men preponderance in the microangiopathic category (72% men versus 28% women), followed by the macroangiopathic (68% men versus 32% women), and CE category (57.3% men versus 42.6% women). This is in contrast to other studies, in which the highest male preponderance was observed in the macroangiopathic category,13,15 and a slight female preponderance was observed in the CE category.15 This finding can be explained by the fact that males are more likely to have LACs because of their higher incidence of risk factors for small vessel disease.16 Differences in pattern of IS in genders can be attributed to difference in etiology and risk factors profile.22
Hypertension was the most frequently identified risk factor in all subtypes of IS, except for stroke of other determined etiology, which is consistent with the published literature.13,15,19 One prospective study on traditional and non-traditional risk factors for IS reported hypertension as the most powerful predictor for all IS subtypes.23 Hypertension has also been described as the most commonly identified risk factor for both ischemic and hemorrhagic strokes in studies from Arab countries.9,12,24
In our study, hypertension was more frequent in SVO (84%) than LAA (78%), as also reported by Yaqub et al.24 In their study, the percentage of hypertension was 81% in patients with lacunar infarction; however, this finding is not similar to other studies.13,15 The Takashima Stroke Registry did not find any significant difference in the prevalence of hypertension across IS subtypes.19 A systemic review25 concluded that apparent excess of hypertension described in lacunar stroke could be because of studies including hypertension in the definition of IS subtype.25
Diabetes mellitus has been reported to be more closely associated with small vessel disease than with other subtypes.15,23 One study from KSA found diabetes to be equally common among patients with infarctions in superficial and deep branches of the anterior or posterior circulation, and patients with lacunar infarction.24 A higher prevalence of diabetes was reported in the microangiopathic category (35.5%), than the macroangiopathic (29.%), or CE (28.1%) category by Grau et al.15 We also found diabetes to be more prevalent in SVO (78%) than LAA (60%). Elevated low-density lipoprotein cholesterol and triglyceride levels are significant risk factors in patients with atherothrombotic cerebrovascular disease presenting as stroke or transient ischemic attack. Hypercholesterolemia is a recognized risk factor for stroke due to LAA.26 No statistically significant difference could be identified in the prevalence of dyslipidemia across IS subtypes in our study. The prevalence of ischemic heart disease (24.2%) in our study was higher than a study from Hofuf, KSA (5.5%),12 similar to study from Kuwait (24.2%),14 but higher than reported in other studies.24,27 We found ischemic heart disease to be significantly more frequent in CE than in LAA, which is in contrast to Deleu et al’s findings of higher frequency in LAA.13 The frequency of atrial fibrillation was relatively higher than other studies.12,14 Smoking, dyslipidemia, and past history of stroke did not show association with any particular subtype.
Approximately 15% of all strokes are heralded by a transient ischemic attack.28 A history of transient ischemic attack was elicited in only 2% of cases in our study, which is similar to reports by El Sayed et al.12 The localization of IS in our study was similar to other studies from KSA,9,12 apart from some variation that can be explained by using different classifications in different studies, although POCI was less frequent. The MCA was the most commonly involved territory in the anterior circulation as mentioned by Yaqub et al.24
One of the major limitations of our study was its retrospective nature, which limits the certainty of appropriate diagnostic evaluation in all patients. The documentation in the patient charts was not always sufficient to ascertain the TOAST classification. Holter monitoring or long term cardiac monitoring was not available in a large number of patients. Performance of transesophageal echocardiogram in some of the patients may have changed the TOAST classification.
Relatively young age at onset and male preponderance are the important findings of our study, and requires verification by further population based prospective studies. The higher prevalence of potentially modifiable risk factors in particular hypertension, diabetes mellitus, and dyslipidemia warrant an urgent need to emphasize the importance of implementation of programs at the national and regional level to control these factors. Furthermore, it is predicted that the proportion of people in KSA aged 60 or more will be around 25% of the total population by the end of 2050, and health expenditure will increase.29 Improving awareness in the general population regarding modification of life style, adapting healthy dietary habits, and regular medical follow up for screening purposes in a younger age group may play an important pivotal role in reducing the disease burden caused by stroke.
In conclusion, hypertension, diabetes mellitus, and hyperlipidemia were important modifiable risk factors for all subtypes of IS. There is an urgent need for adequate preventive measures to control these risk factors to reduce the overall burden of stroke. Males were found to be affected at a relatively younger age when compared with females. Further large prospective studies are required to better understand the relationship between the etiologic subtypes of IS and the risk factors.
Footnotes
Disclosure.
References
- 1.Di Carlo A. Human and economic burden of stroke. Age Ageing. 2009;38:4–5. doi: 10.1093/ageing/afn282. [DOI] [PubMed] [Google Scholar]
- 2.Sacco RL, Kasner SE, Broderick JP, Caplan LR, Connors JJ, Culebras A, et al. An updated definition of stroke for the 21st century:a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013;44:2064–2089. doi: 10.1161/STR.0b013e318296aeca. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Feigin VL, Forovzanfar MH, Krishnamurthi R, Mannash GA, Connor M, Benette DA, et al. Global and regional burden of stroke during 1990-2010:findings from the Global Burden of Disease Study 2010. Lancet. 2014;383:245–254. doi: 10.1016/s0140-6736(13)61953-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.AL-Rajesh S, Larbi E, Bademosi O, Awada A, Yousef A, Al-Fareihi H, et al. Stroke register:experience from the eastern province of Saudi Arabia. Cerebrovasc Dis. 1998;8:86–9. doi: 10.1159/000015823. [DOI] [PubMed] [Google Scholar]
- 5.al Rajeh S, Bademosi O, Ismail H, Awada A, Dawodu A, al-Freihi H, et al. A community survey of neurological disorders in Saudi Arabia:the Thugbah study. Neuroepidemiology. 1993;12:164–78. doi: 10.1159/000110316. [DOI] [PubMed] [Google Scholar]
- 6.Tran J, Mirzaei M, Anderson L, Leeder SR. The epidemiology of stroke in the Middle East and North Africa. J Neurol Sci. 2010;295:38–40. doi: 10.1016/j.jns.2010.05.016. [DOI] [PubMed] [Google Scholar]
- 7.Sacco RL, Benjamin EJ, Broderick JP, Dyken M, Easton JD, Feinberg WM, et al. American Heart Association Prevention Conference. IV. Prevention and Rehabilitation of Stroke. Risk factors. Stroke. 1997;28:1507–1517. doi: 10.1161/01.str.28.7.1507. [DOI] [PubMed] [Google Scholar]
- 8.Aho K, Harmsen P, Hatano S, Marquardsen J, Simirnov WE, Strasser T. Cerebrovascular disease in the community:results of a WHO collaborative study. Bull World Health Organ. 1980;58:113–130. [PMC free article] [PubMed] [Google Scholar]
- 9.Al-Rajeh S, Awada A, Niazi G, Larbi E. Stroke in a Saudi Arabian National Guard community. Analysis of 500 consecutive cases from a population-based hospital. Stroke. 1993;24:1635–1639. doi: 10.1161/01.str.24.11.1635. [DOI] [PubMed] [Google Scholar]
- 10.Qari FA. Profile of stroke in a teaching university hospital in the western region. Saudi Med J. 2000;21:1030–1033. [PubMed] [Google Scholar]
- 11.Al-Jadid M, Robert AA. Determinants of length of stay in an inpatient stroke rehabilitation unit in Saudi Arabia. Saudi Med J. 2010;31:189–192. [PubMed] [Google Scholar]
- 12.El Sayed MM, Adeuja GO, El-Nahrawy E, Olaish M. Characteristics of stroke in Hofuf, Saudi Arabia. Ann Saudi Med. 1999;19:27–31. doi: 10.5144/0256-4947.1999.27. [DOI] [PubMed] [Google Scholar]
- 13.Deleu D, Inshasi J, Akhtar N, Ali J, Vurgese T, Ali S, et al. Risk factors, management and outcome of subtypes of ischemic stroke:a stroke registry from the Arabian Gulf. J Neurol Sci. 2011;300:142–147. doi: 10.1016/j.jns.2010.08.023. [DOI] [PubMed] [Google Scholar]
- 14.Al-Shammri S, Shahid Z, Ghali A, Mehndiratta MM, Swaminathan TR, Chadha G, et al. Risk factors, subtypes and outcome of ischaemic stroke in Kuwait--a hospital-based study. Med Princ Pract. 2003;12:218–223. doi: 10.1159/000072287. [DOI] [PubMed] [Google Scholar]
- 15.Grau AJ, Weimar C, Buggle F, Heinrich A, Goertler M, Neumaier S, et al. Risk factors, outcome, and treatment in subtypes of ischemic stroke:the German stroke data bank. Stroke. 2001;32:2559–2566. doi: 10.1161/hs1101.098524. [DOI] [PubMed] [Google Scholar]
- 16.Acciarresi M, De Luca P, Caso V, Agnelli G, D’Amore C, Alberti A, et al. Acute stroke symptoms:do differences exist between sexes? J Stroke Cerebrovasc Dis. 2014;23:2928–2933. doi: 10.1016/j.jstrokecerebrovasdis.2014.07.044. [DOI] [PubMed] [Google Scholar]
- 17.Bahou Y, Hamid H, Raqab MZ. Ischemic stroke in Jordan 2000 to 2002;a two year;hospital – based study. J Stroke Cerebrovasc Dis. 2004;13:81–84. doi: 10.1016/j.jstrokecerebrovasdis.2004.02.004. [DOI] [PubMed] [Google Scholar]
- 18.Yip PK, Jeng JS, Lee TK, Chang YC, Huang ZS, Ng SK, et al. Subtypes of ischemic stroke. A hospital-based stroke registry in Taiwan (SCAN -IV) Stroke. 1997;28:2507–2512. doi: 10.1161/01.str.28.12.2507. [DOI] [PubMed] [Google Scholar]
- 19.Turin TC, Kita Y, Rumana N, Nakamura Y, Takashima N, Ichikawa M, et al. Ischemic stroke subtypes in a Japanese population:Takashima Stroke Registry 1988-2004. Stroke. 2010;41:1871–1876. doi: 10.1161/STROKEAHA.110.581033. [DOI] [PubMed] [Google Scholar]
- 20.Abdul-Ghaffar NU, el-Sonbaty MR, el-Din Abdul-Baky MS, Marafie AA, al-Said AM. Stroke in Kuwait:a three-year prospective study. Neuroepidemiology. 1997;16:40–47. doi: 10.1159/000109669. [DOI] [PubMed] [Google Scholar]
- 21.El Tallawy HN, Farghaly WM, Badry R, Hamdy NA, Shehata GA, Rageh TA, et al. Epidemiology and clinical presentation of stroke in Upper Egypt (desert area) Neuropsychiatr Dis Treat. 2015;11:2177–2183. doi: 10.2147/NDT.S87381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Forster A, Gass A, Kern R, Wolf ME, Ottomeyer C, Zohsel K, et al. Gender differences in acute ischemic stroke:etiology, stroke patterns and response to thrombolysis. Stroke. 2009;40:2428–2432. doi: 10.1161/STROKEAHA.109.548750. [DOI] [PubMed] [Google Scholar]
- 23.Ohira T, Shahar E, Chambless LE, Rosamond WD, Mosley TH, Folsan AR. Risk factors for ischemic stroke subtypes:the Atherosclerosis Risk in Communities study. Stroke. 2006;37:2493–2498. doi: 10.1161/01.STR.0000239694.19359.88. [DOI] [PubMed] [Google Scholar]
- 24.Yaqub BA, Shamena AR, Kolawole TM, Patel PJ. Cerebrovascular disease in Saudi Arabia. Stroke. 1991;22:1173–1176. doi: 10.1161/01.str.22.9.1173. [DOI] [PubMed] [Google Scholar]
- 25.Jackson C, Sudlow C. Are lacunar strokes really different?A systematic review of differences in risk factor profiles between lacunar and nonlacunar infarcts. Stroke. 2005;36:891–901. doi: 10.1161/01.STR.0000157949.34986.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hachinski V, Graffagnino C, Beaudry M, Bernier G, Buck C, Donner A, et al. Lipids and stroke:a paradox resolved. Arch Neurol. 1996;53:303–308. doi: 10.1001/archneur.1996.00550040031011. [DOI] [PubMed] [Google Scholar]
- 27.Awada A, Al Rajeh S. The Saudi Stroke Data Bank. Analysis of the first 1000 cases. Acta Neurol Scand. 1999;100:265–269. [PubMed] [Google Scholar]
- 28.Hankey GJ. Impact of treatment of people with transient ischemic attack on stroke incidence and public health. Cerebrovasc Dis. 1996;6:26–33. [Google Scholar]
- 29.Bloom DE, Canning D, Fink G. Implication of population ageing for economic growth. Oxf Rev Econ Policy. 2010;26:283–612. [Google Scholar]


