Abstract
A backbone-modified peptide derived from parathyroid hormone (PTH) is shown to function as an inhibitor and inverse agonist of parathyroid hormone receptor-1 (PTHR1) signaling. This receptor acts to regulate calcium and phosphate homeostasis, as well as bone turnover and development. PTH is a natural agonist of PTHR1, and PTH(1–34) displays full activity relative to the natural 84-residue hormone. PTH(1–34) is used clinically to treat osteoporosis. N-terminally truncated derivatives of PTH(1–34), such as PTH(7–34), are known to bind to PTHR1 without initiating intracellular signaling and can thus act as competitive antagonists of PTH-induced signaling at PTHR1. In some cases N-terminally truncated PTH derivatives also act as inverse agonists of PTHR1 variants that display pathologically high levels of signaling in the absence of PTH. Many analogues of PTH, however, are rapidly degraded by proteases, which may limit biomedical application. We show that backbone modification via periodic replacement of α-amino acid residues with homologous β-amino acid residues leads to an α/β-PTH(7–34) peptide that retains the antagonist and inverse agonist activities of the prototype α-peptide while exhibiting enhanced stability in the presence of aggressive proteases. These findings highlight the value of backbone-modified peptides derived from PTH as tools for investigating determinants of PTH metabolism and provide guidance for designing therapeutic agents for diseases arising from excessive ligand-dependent or ligand-independent PTHR1 activity.
INTRODUCTION
Parathyroid hormone receptor-1 (PTHR1) is a B-family GPCR that is highly expressed in kidney and bone.1 PTHR1 signaling is crucial for maintaining ionized calcium (Ca2+) concentrations within a narrow range in the bloodstream, and is thus activated by parathyroid hormone (PTH) in response to Ca2+ influx/efflux changes that occur on the minute timescale. In parallel, PTHR1 regulates bloodstream concentrations of inorganic phosphate (Pi) through the action of PTH. On longer timescales (days or weeks), PTHR1 activity modulates bone-building and bone-breakdown processes.2 Moreover, PTHR1 signaling regulates cell growth and differentiation programs during development, which occurs via parathyroid hormone-related protein (PTHrP)-mediates signaling. Thus, PTHR1 responds to two endogenous agonists, PTH and PTHrP. Activation of PTHR1 leads to production of intracellular cyclic adenosine monophosphate (cAMP), among other secondary messengers, and stimulates downstream processes.3 Dysregulation of PTHR1 signaling is implicated in several human diseases.4 Intermittent activation of PTHR1 via once daily subcutaneous injection of PTH(1–34) stimulates bone growth and is used to treat osteoporosis.2
Excessive activation of PTHR1 can lead to hypercalcemia and net bone breakdown.5 Overproduction of PTH by the parathyroid gland (primary hyperparathyroidism) is a common cause of hypercalcemia.6 Aberrant production of PTHrP by some types of cancer cells can also lead to hypercalcemia (humoral hypercalcemia of malignancy), and life-threatening complications.7 Agents that block activation of PTHR1 by PTH or PTHrP could, in principle, restore normal levels of blood calcium and ameliorate the associated symptoms.
Mutations in the gene encoding PTHR1 represent an alternative path to pathological signaling levels. Expression of PTHR1 variants with high basal levels of G-protein/cAMP signaling in the absence of any agonist causes Jansen’s Metaphyseal chondrodysplasia, a rare disorder associated with hypercalcemia and developmental irregularities affecting growth plates and bone.8 Agents that reverse the high levels of ligand independent signaling exhibited by these PTHR1 variants, i.e., inverse agonists of these receptors, could conceivably be used to treat this disease.
Removal of the first six N-terminal residues of PTH(1–34) reduces affinity of resulting analogues for PTHR1 by >100-fold and essentially abolishes the ability to stimulate intracellular cAMP production.9 Bovine PTH(7–34) [bPTH(7–34)] was shown to antagonize PTH(1–34)-stimulated physiological responses in rats lacking endogenous parathyroid hormone.10, 11 Subsequent studies found that replacing Gly with dTrp at position 12 in bPTH(7–34) enhances PTHR1 affinity and cAMP inhibitory activity by 10–20 fold.12 bPTH(7–34) dTrp12 acts as an inverse agonist of cAMP signaling at constitutively active PTHR1 variants,13 while bPTH(7–34), which has the native residue Gly at position 12, does not,14 Both the stereochemistry and identity of the side chain at position 12 are important for inverse agonist activity,14 indicating that inverse agonism likely results from a specific peptide-receptor interaction promoted by the Gly-to-dTrp12 replacement.
An analogue of bPTH(7–34) dTrp12, with Met-to-nLeu substitutions at positions 8 and 18 and a Phe-to-Tyr modification at position 34, inhibited responses to exogenously administered PTH(1–34) in thyroparathyroidectomized rats.15 However, administration of this derivative of bPTH(7–34) dTrp12 to humans with hyperparathyroidism and hypercalcemia did not induce reductions in blood calcium levels16.
The lack of a therapeutic effect following administration of a close analogue of bPTH(7–34) DTrp12 may, in part, reflect degradation of this inhibitory peptide by endogenous proteases.17 PTH(1–34) is rapidly degraded by purified proteases18 and in tissue homogenates19. Both PTH(1–34) and bPTH(7–34) dTrp12 disappear rapidly from the bloodstream when administered to animals.20, 21. It is especially noteworthy that a majority of a radiolabeled version of bPTH(7–34) dTrp12 analogue in the bloodstream was found to be degraded 10 minutes after intravenous injection20 despite the observation that radiolabeled PTH(1–34) is highly stable in plasma.22 These observations indicate that endogenous proteases catalyze the rapid degradation of injected PTH derivatives, but the specific cells, organs, and proteases responsible for this degradation, particularly for N-terminal fragments such as PTH(1–34), have not been unambiguously identified.23–27 The relevant proteolytic activity is not found in standard plasma preparations.22
The connection between proteolysis of PTH analogues and attenuation of biological activity is complicated by the observation that PTH fragments, such as PTH(1–34), are rapidly filtered from the bloodstream by the kidney22 and are endocytosed from the filtrate into endosomes, where degradation can occur, in proximal tubule epithelial cells via either the scavenger receptor megalin28 or PTHR1.23 It is not clear whether proteolytic degradation of PTH analogues directly causes attenuation of bioactivity, or whether degradation primarily occurs as a secondary consequence following renal filtration, with filtration serving as the primary mechanism for attenuation of PTH biological activity in vivo. Thus, modifications of bPTH(7–34) dTrp12 that do not interfere with inverse agonist activity but confer broad resistance to proteolysis should enable experiments that reveal whether proteolytic degradation is a primary cause of the lack of in vivo activity manifested by this peptide. Ultimately, insights from such studies should support efforts to develop PTHR1 antagonist/inverse agonist agents that display clinical utility.
Altering the polypeptide backbone by replacing some α-amino acid residues with β residues to generate “α/β peptides” can confer substantial resistance to peptidase/protease action without loss of structural and functional properties.29 α/β-Peptides containing 25–33% β residues evenly distributed along the sequence adopt a helical conformation very similar to that of a canonical α-helix.30, 31,32 Carefully designed α/β-peptides can substitute for α-peptides in binding to specific protein partners. This approach has produced α/β-peptide mimics of BH3 domains that bind to Bcl-2 family proteins and induce apoptotic signaling,31 α/β-peptide mimics of the gp41 CHR domain that inhibit HIV membrane fusion30, 33 and most recently α/β-peptide mimics of peptide hormones that signal through B-family GPCRs.34, 35 In particular, we have described α/β-peptide analogues of PTH(1–34) containing up to seven α-to-β replacements that match the potency of PTH(1–34) itself in activating PTHR1, as judged by stimulation of cAMP production in a cell-based assay.34 Alternative approaches for providing PTH derivatives with non-native chemical functionalities, which may also alter proteolytic susceptibility, have been recently reported as well. A chemical ligation strategy that utilized the N-terminal serine residue in human PTH was used to generate a peptoid-PTH hybrid.36 A different strategy used a non-native cysteine residue to attach a lipid moiety to a truncated, weakly active PTH derivative to enhance biological potency and reduce proteolytic susceptibility.37
The work described here builds from one of the previously described α/β analogues of human PTH(1–34).34 This analogue contains α-to-β replacements at six sites extending inward from the C-terminus, with a repeating αααβ pattern. Specifically, β residues were placed at positions 14, 18, 22, 26, 30 and 34 [PTH(1–34) numbering]. At five of the sites, the native α residue was replaced with the β3 homologue, that is, with the β residue bearing the same side chain as the original α residue on the backbone carbon adjacent to nitrogen. At the sixth site, position 14, the α/β-peptide contained β3-homotryptophan (β3-hTrp), rather than β3-hHis (to mimic the His at position 14 in native PTH), since β3-hHis is not commercially available. This α/β analogue of PTH(1–34) binds to PTHR1 with affinity comparable to that of PTH(1–34) itself and is comparable to the α-peptide in terms of receptor activation (agonist potency and efficacy, as measured by cAMP production).34 The α/β-peptide also displays significantly prolonged bioactivity in mice relative to PTH(1–34), which correlates with a longer persistence of the α/β-peptide in the mouse bloodstream.34
The studies presented below are based on extension to bPTH(7–34) dTrp12 (1 in Figure 1) of the backbone modification strategy involving periodic α-to-β replacement. Peptide 1 was selected as a prototype in these studies for two reasons. First, this peptide is among the most potent antagonists of PTHR1 signaling known.3, 12 Close analogues of peptide 1 have undergone the most extensive biochemical and pharmacological characterization of any PTHR1 antagonists and have proven effective in animal model systems.12, 15, 16 This family of compounds has not been surpassed functionally by any other small peptide antagonists of PTHR1. Thus, comparisons between peptide 1 and new antagonists enable an assessment of antagonist activity relative to an efficacious standard. Second, peptide 1 is a potent inverse agonist14 of two PTHR1 variants that display high constitutive signaling activity and cause the rare genetic disorder Jansen’s Metaphyseal chondroplasia.38 Analogues of PTH(7–34) with improved metabolic stability could help to elucidate and potentially improve the pharmacological properties of PTHR1 inverse agonists/antagonists for treating diseases of PTHR1 overactivation.15, 16, 39 The identification of a proteolytically stabilized analogue of peptide 1 would thus provide a novel tool to assess the role of metabolic degradation in controlling in vivo PTHR1 antagonist efficacy, and provide a starting point for future efforts to develop more effective inhibitors. The tight coupling between structural modifications and inverse agonist activity provides a basis for exploring the utility of the backbone-modification strategy as a potentially general source of functional mimics of bioactive peptides.13, 14, 40
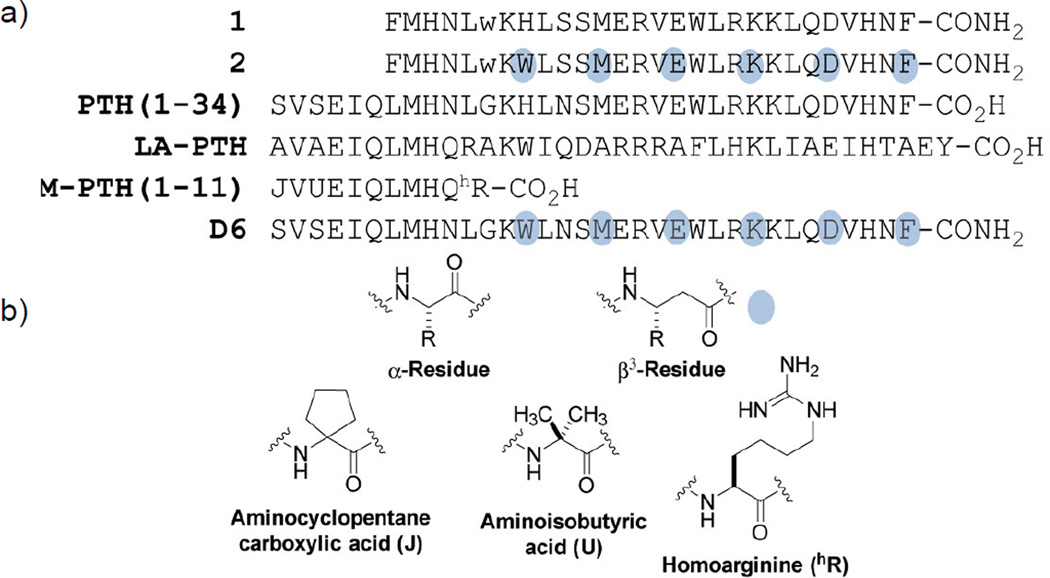
Figure 1. Structures of peptides derived from parathyroid hormone (PTH) used in this study.
(a) Sequences of peptides used in this study. The conventional single-letter code is used to indicate α residue identity. Blue dots indicate sites of α-to-β3 replacement; each β3 residue bears the side chain of the a residue indicated by the letter. D-tryptophan residues are represented with a lowercase “w”. (b) Structures of amino acid residues used in this study.
RESULTS AND DISCUSSION
Synthesis
bPTH(7–34) dTrp12 (1) and the α/β-peptide analogue 2 (Figure 1a) were synthesized using microwave-assisted solid phase chemistry30 based on Fmoc protection of backbone amino groups. Positions of α-to-β3 replacement in 2 are identical to the sites of α-to-β3 replacement in a previously described α/β-peptide mimic of PTH(1–34) (analogue D6, Fig. 1).34 α-Residues other than His 14, were replaced with homologous β3 amino acid residues, the building blocks for which are commercially available. Previous work demonstrated that replacing His 14 with Trp in PTH(1–14)41 or PTH(1–34) derivatives42 did not diminish the receptor affinity or bioactivity of these derivatives. Protected β3-hHis is not commercially available, so His 14 was replaced with β3-hTrp, which was shown to be tolerated in α/β-peptide derivatives of PTH(1–34).34
Binding to PTHR1
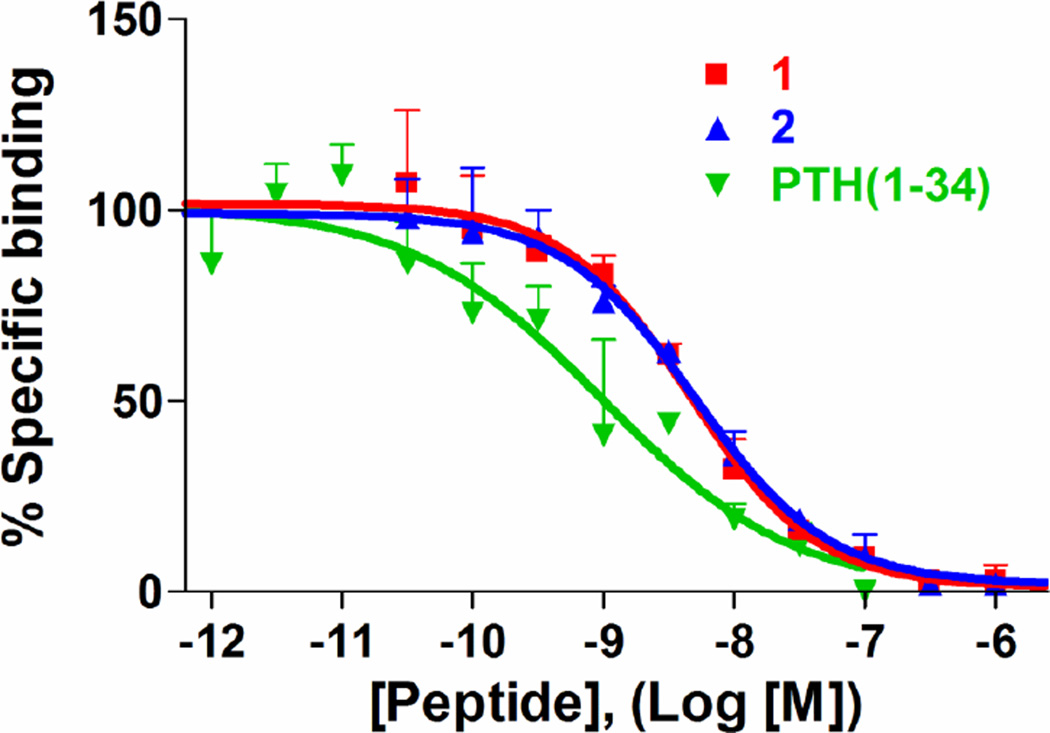
We evaluated the affinity of peptides 1 and 2 for PTHR1 using a well-established competition binding assay43, 44 that uses radiolabeled PTH(1–34) and membranes isolated from a HEK-293 cell line that stably expresses human PTHR1 (GP2.3 cell line34). A close analogue of 1, containing Tyr at position 34 instead of Phe [PTH(1–34) numbering], has previously been tested in radiolabel binding assays.12, 14 We included human PTH(1–34) (Figure 1a) as a positive control and point of comparison for peptides 1 and 2. Bound radioactivity resulting from association of radiolabeled PTH(1–34) with PTHR1 is diminished in a dose-dependent fashion following addition of unlabeled PTH(1–34), α-peptide 1, or α/β-peptide 2. α/β-Peptide 2 matches α-peptide 1 in affinity for PTHR1; peptides 1 and 2 both bind less tightly to the receptor than does PTH(1–34) (Figure 2 and Table 1), as expected based on previous findings with 1 and other truncated analogues.9, 12 This trend presumably reflects a loss of energetically important contacts between residues 1–6 of PTH(1–34) and PTHR1. The very similar behavior of peptides 1 and 2 is significant in light of previous findings that peptide 1 is among the most potent and effective PTHR1 antagonists known and can inhibit PTH-mediated biological responses in vivo.15
Figure 2. Binding of peptides at PTHR1.
Binding to PTHR1 was assessed using cell membrane preparations derived from a HEK-293 cell line stably transfected to express human PTHR1. Experiments were carried out in the presence of GTPγS (10−5 M) using 125I-PTH(1–34) as a tracer radioligand. Binding values are reported in Table 1. Data are presented as means (± SEM) of three experiments, with each condition assessed in duplicate in each experiment. Curves represent fitting of a sigmoidal dose response with variable slope model to the data.
Table 1.
Summary of selected functional data for PTH analogs
| PTHR1 binding* by competition assay |
Antagonism of cAMP generation† in SGS72 cells, IC50, nM (± SEM) |
Protease stability‡, half life, minutes |
||||
|---|---|---|---|---|---|---|
| Peptide | IC50, nM (± SEM) | vs. PTH(1–34) | vs. LA-PTH | vs. M-PTH(1–11) | Proteinase K | Trypsin |
| 1 | 4.7 ± 1.2 | 4.28 ± 1.17 | 10.2 ± 1.9 | 0.44 ± 0.13 | 0.13 | 0.7 |
| 2 | 4.5 ± 1.2 | 6.15 ± 2.12 | 10.6 ± 3.2 | 2.07 ± 0.79 | 2.5 | >20§ |
| PTH(1–34) | 0.8 ± 0.5 | (−) | (−) | (−) | (−) | (−) |
Peptide concentration needed for 50% inhibition (IC50) of binding of 125I labelled PTH(1–34) tracer peptide to membranes derived from HEK-293 cells expressing PTHR1
Peptide concentration needed for 50% inhibition (IC50) of luminescence produced in response to intracellular cAMP production stimulated by PTHR1 agonists listed below
Peptide half life in the presence of the indicated protease under conditions described in the methods section
Peptide degradation curve shows poor fit with exponential decay model so half life estimated based upon measurements of intact peptide remaining after 20 minutes of incubation
(−) Peptide not analyzed using this assay in this study
Inhibition of PTHR1 activation
The abilities of α-peptide 1 and α/β-peptide 2 to inhibit PTH(1–34)-stimulated responses in cells were compared. A close analogue of 1 with Tyr at position 34 has previously been evaluated in cAMP inhibition assays.12, 14 Stimulation of cAMP production was monitored using SGS-72 cells, which were derived from osteoblastic SaOS-2 cells.45 These cells express endogenous PTHR1 and have been stably transfected to express a luciferase variant that is activated by intracellular cAMP.46, 47
The SGS-72 cell line was used to assess inhibition of PTHR1 activation instead of the HEK-293-derived GP2.3 cell line described above because preliminary studies showed that antagonist peptides more potently inhibited PTHR1-mediated cAMP responses in SGS-72 cells than in GP2.3 cells (data not shown). This difference in antagonist behavior may arise from lower levels of PTHR1 found on the surface of SGS-72 in comparison to GP2.3 cell lines (data not shown); a previous study of other PTH antagonist peptides found greater antagonist potencies in SaOS-2 cells than in a stable porcine kidney cell line (HKRK-B7) that expresses high levels of the human PTHR1.48 The greater sensitivity of the assay based on SGS-72 cells provides a more incisive comparison between PTHR1 antagonist agents.
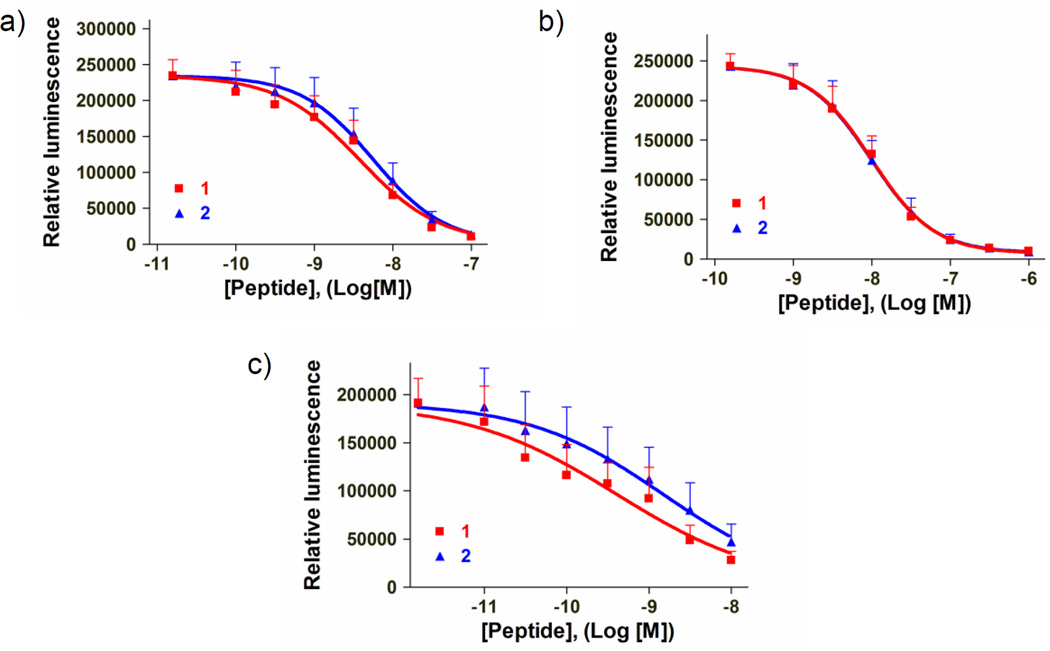
To mimic previous experiments showing that 1 inhibits cAMP production when administered before a PTHR1 agonist,12 we incubated varied concentrations of either 1 or 2 with SGS-72 cells for 15 minutes prior to addition of PTH(1–34) or other PTHR1 agonists (Figure 3, Table 1). Inhibition of M PTH(1–11) and LA-PTH (Figure 1a) agonism of PTHR1 was assessed because these peptides induce signaling responses in a manner different from that of PTH(1–34). M-PTH(1–11) and LA-PTH are both synthetic derivatives of PTH that were previously identified in structure-activity relationship studies49, 50. M-PTH(1–11) binds only to the transmembrane region (TMR) of PTHR1, whereas PTH(1–34) and LA-PTH bind to both the TMR and the extracellular domain (ECD) of this receptor.49 LA-PTH has higher affinity than does PTH(1–34) for the G-protein uncoupled state of PTHR1. This difference, in vitro, results in slower dissociation of LA-PTH from the receptor, relative to dissociation of PTH(1–34); in vivo LA-PTH induces longer biological responses than does PTH(1–34).50 Comparing the antagonistic effects of α/β-peptide 2 with those of α-peptide 1 on PTHR1 activation by agonist peptides with different modes of association was pursued to provide further insight into the extent to which 2 is a functional mimic of 1.
Figure 3. Inhibition of cAMP responses at PTHR1 by peptides.
PTHR1-mediated cAMP responses were assessed using a SaOS-2 derived cell line (SGS-72) that expresses PTHR1 at endogenous levels and is stably transfected to expresses a luciferase variant that is activated by intracellular cAMP. cAMP antagonism IC50 values are reported in Table 1. Antagonist peptides were incubated with cells at indicated doses for 15 minutes before addition of (a) human PTH(1–34), (b) LA-PTH, or (c) M-PTH(1–11) at final concentrations of 0.3 nM, 0.3 nM or 10 nM respectively. Maximum luminescence responses were then recorded 12–20 minutes after peptide addition and were used to generate dose response curves. Data are presented as means (± SEM) of five experiments. Curves represent fitting of a sigmoidal dose response with variable slope model to the data.
α/β-Peptide 2 matches the efficacy and potency of parent α-peptide 1 for inhibiting PTH(1–34)-stimulated cAMP responses in SGS 72 cells (Figure 3a). In addition, 2 is comparable to 1 in inhibiting intracellular cAMP responses stimulated by LA-PTH50 (Figure 3b), as well as M-PTH(1–11)49 (Figure 3c). The slightly weaker inhibition of M-PTH(1–11)-induced signaling by 2 in comparison to inhibition by 1 suggests that the α-to-β residue substitutions in 2 may alter interactions with the PTHR1 transmembrane region; however, any such differences result in only minor reductions in M-PTH(1–11) inhibition potency (< 5-fold, table 1) and are not reflected in binding assays using PTHR1 (Figure 1). These findings using agonists that bind PTHR1 via distinct modalities provide additional evidence that α/β-peptide 2 is a close functional mimic of α-peptide 1.
Control experiments show that neither α-peptide 1 nor α/β-peptide 2 substantially reduces the low basal cAMP levels seen in SGS-72 cells (Fig. S1a) or the stimulation of cAMP production caused by addition of isoproterenol, which activates the β2-adrenergic receptor, an A-family GPCR that is endogenously expressed in SGS-72 cells (Fig. S1b). Experiments using a different B-family GPCR agonist, vasoactive intestinal peptide (VIP), which activates VIP-receptor 1 (VIPR1) that is also endogenously expressed in SaOS-2 cells,51 show that both 1 and 2 weakly inhibit VIP induced cAMP production (IC50 > 1 µM; Fig. S1c). The origin of this behavior was not further explored, because 1 and 2 are approximately 1,000-fold less potent as antagonists of VIP-induced cAMP responses relative to their activity as antagonists of PTH(1–34) mediated cAMP responses. Thus, it is unlikely that inhibition of VIPR1-mediated cAMP production would be relevant in biological settings. We conclude that the antagonism of PTH-induced cAMP production observed for both α-peptide 1 and α/β-peptide 2 is specifically mediated by binding of these peptides to PTHR1.
Peptides 1 and 2 did not stimulate increases in cellular pools of phosphorylated extracellular signal-regulated kinases (ERKs)-1/2 in HEK-293-derived cells stably expressing PTHR1 (GP2.3 cells), while PTH(1–34) induced pronounced increases (Fig. S2). These results are generally consistent with the expected antagonist properties of N-terminally truncated PTH analogues,52 although a previous study using a different cell assay system found that an analogue of peptide 1 with Tyr at position 34 [PTH(1–34) numbering] could stimulate a moderate increase in ERK-1/2 phosphorylation via recruitment of β-arrestin to PTHR1.53 The findings thus leave open the possibility that the ERK-1/2 response to PTH ligands can vary depending on cell type and/or specific structural properties of the ligand.
Inverse agonism in cells expressing constitutively active PTHR1 variants
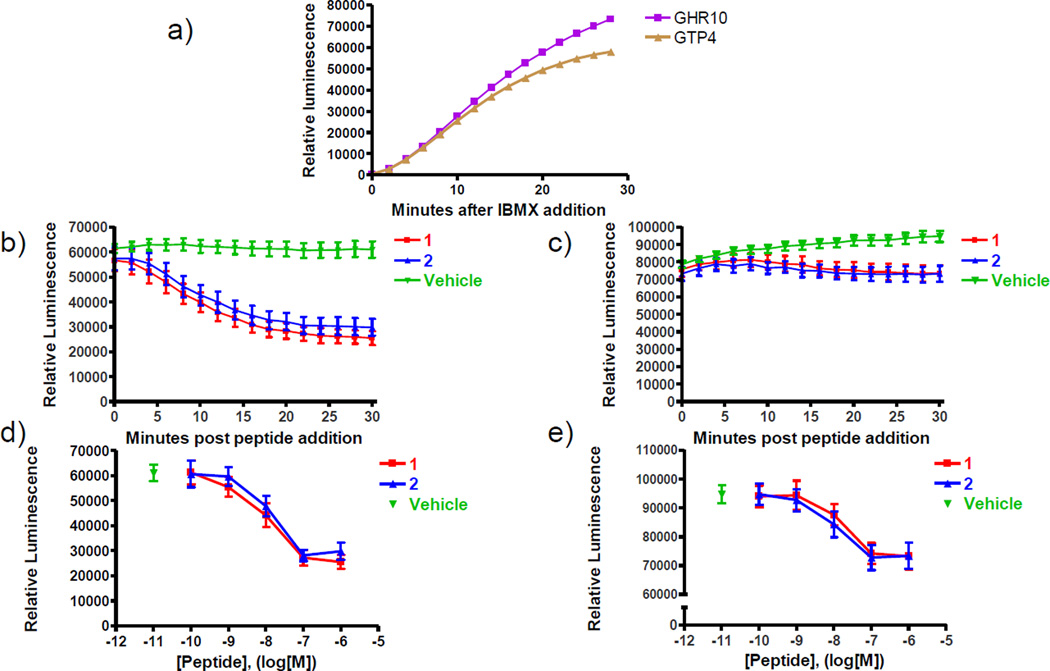
α-Peptide 1 suppresses spontaneous cAMP production by PTHR1 variants that cause formation of high basal (ligand-independent) levels of intracellular cAMP.14 This inverse agonist activity is dependent on the Gly-to-dTrp replacement at position 12, as bPTH(7–34) analogues with glycine at position 12 do not reduce basal signaling by these same constitutively active forms PTHR1 but instead act as neutral antagonists of PTHR1 activation.52 To test whether α/β peptide 2 mimics the inverse agonist activity of α-peptide 1, we evaluated the ability of this α/β peptide to reduce basal cAMP production in HEK293-based cell lines that stably express luciferase cAMP reporter47 and either the H223R or T410P mutant variant of the human PTHR1 (GHR10 or GTP4 cell lines, respectively).13 These two PTHR1 variants induce relatively high levels of cAMP production in the absence of a PTH agonist, and both are associated with the human disease Jansen’s Metaphyseal chondrodysplasia.38
Incubation of cells expressing PTHR1-H223R or PTHR1-T410P with isobutylmethylxanthine (IBMX), a cell-permeable inhibitor of cAMP hydrolysis, results in accumulation of substantial levels of intracellular cAMP, as indicated by a strong luminescence signal (Fig. 4a). Addition of either 1 or 2 inhibits further accumulation of intracellular cAMP in GHR10 or GTP4 cells in a time- and dose-dependent manner (Fig. 4b–e, Fig. S3). The similarity of the inverse agonist profiles of α peptide 1 and α/β-peptide 2 show that 2 retains the ability to engage the PTHR1 variants in a manner that suppresses constitutive signaling, despite the multiple α-to-β replacements.
Figure 4. Inverse agonism activity of peptides at constitutively active PTHR1 mutants.
Cells were incubated in CO2 independent media containing D-luciferin (0.5 M) and 3-isobutyl-1-methylxanthine (IBMX, 2 mM) for 30 minutes before addition of inverse agonist peptides (panel a). These experiments were performed in HEK-293 cells transfected to stably express either hPTHR1 T410P (GTP4 cell-line, panels b and d) or H223R (GHR10 cell line, panels c and e) variants. The time courses presented in panels b and c represent alterations in intracellular cAMP levels stimulated following addition of peptides at a final dose of 1 µM. Dose response plots presented in panels d and e represent relative luminescence levels recorded 30 minutes after addition of inverse agonist peptides or vehicle. The y-axis in panel e is presented using a discontinuity to highlight the dose response relationship observed. Data are presented as means (± SEM) of three experiments, with each condition assessed in duplicate in each experiment.
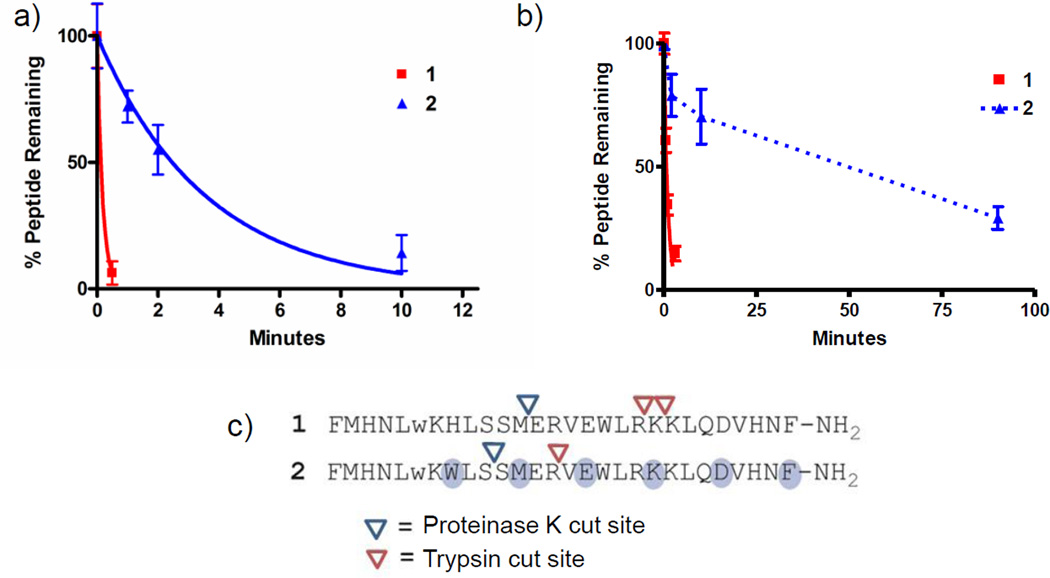
Proteolysis
To assess the consequences of backbone modification on susceptibility to cleavage by proteases, we incubated either α-peptide 1 or α/β-peptide 2 with either the digestive protease bovine trypsin or the fungal enzyme proteinase K. We used these model proteases instead of endogenous mouse proteases or plasma preparations because the protease(s) responsible for degradation of PTH derivatives in vivo have not been unambiguously identified, and PTH derivatives are stable in standard plasma preparations.22 Our experiments were intended to provide a general assessment of the susceptibility of peptides 1 or 2 to degradation by aggressive proteases. Trypsin shows a high preference for hydrolyzing amide bonds following lysine or arginine residues, while proteinase K prefers to hydrolyze amide bonds following aliphatic or aromatic residues.54 HPLC was used to determine the proportion of each peptide remaining intact after various periods of exposure to each protease.30
α/β-Peptide 2 is substantially more stable than is α-peptide 1 in the presence of trypsin (t1/2 >20 min vs. 0.7 min) or proteinase K (t1/2=2.5 min vs. 0.13 min, respectively) (Table 1, Fig. 5, Figure S4). Sites of proteolysis were determined via MALDI-TOF mass spectrometric analysis of protease reaction solutions. As expected, trypsin cut at sites following lysine or arginine in 1 and 2, although incorporation of α-to-β replacement altered the preferred site of protease activity between the two peptides (Figure 5c). An independent replicate of the proteolysis experiment using trypsin (Figure S4) shows that trends observed in these experiments are generally reproducible. A major site of proteinase K catalyzed cleavage in 2 was identified after Ser16 [PTH(1–34) numbering], which is found within the segment containing α-to-β replacements. Partial replacement of β3 residues with cyclically constrained β-residues near this susceptible site, which is known to enhance proteolytic stability in some cases,33 may provide an inverse agonist of PTHR1 with enhanced resistance to degradation by proteinase K.
Figure 5. Evaluation of peptide stabilities in the presence of proteinase K or trypsin.
Peptides were incubated with (a) proteinase K or (b) trypsin using conditions described in the methods section. The amount of peptide remaining intact at indicated time points was measured using an HPLC-based assay. Data are presented as means (± SD) from a single experiment, with each condition assessed in duplicate. Results were fitted to an exponential decay model constrained to a plateau value of zero, which showed good agreement between the model and experimental data (r2>0.95), except for peptide 2 in the presence of trypsin, which was not evaluated using this model. Data points for peptide 2 in panel b are connected by a broken line to reflect this difference. The exponential decay model was used to provide estimated peptide half-lives for degradation experiments, except for peptide 2 in the presence of trypsin. Peptide half-lives are reported in Table 1. A replicate trypsin proteolysis experiment yielding similar data is presented in figure S4. (c) Amide bonds susceptible to protease-catalyzed hydrolysis were identified through characterization of peptide fragments appearing after incubation with protease using MALDI-TOF masss pectrometry.
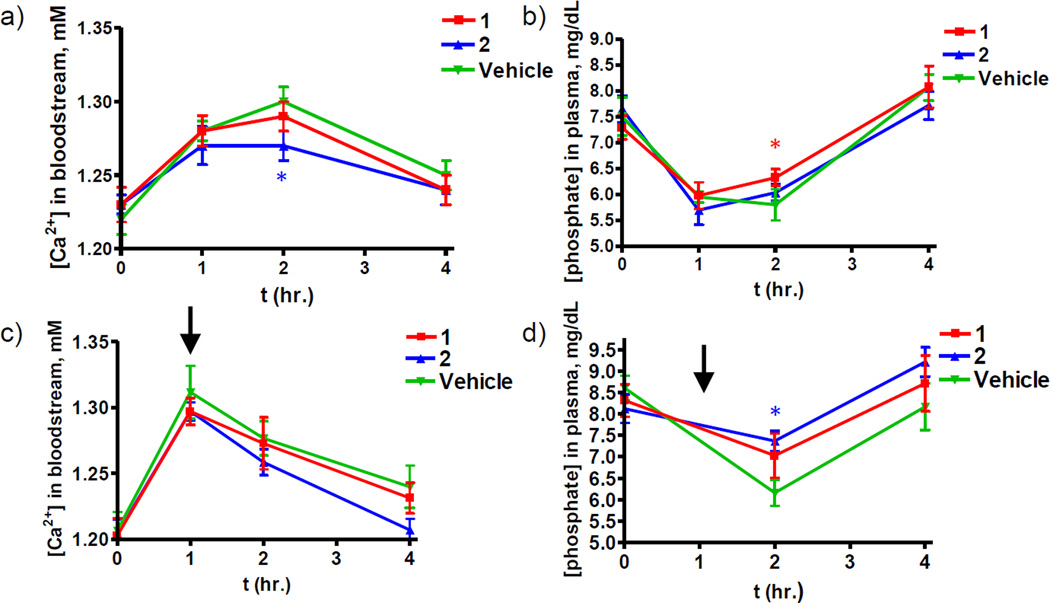
Assessment of antagonist activity in vivo
We sought to evaluate the capacity of α-peptide 1 and α/β-peptide 2 to function as antagonists in vivo by injecting them into mice and measuring their effects on PTH(1–34)-induced changes in blood ionized calcium (Ca2+) and inorganic phosphorus (Pi) levels. In the first experiment, the antagonist peptides were injected four minutes prior to injection of PTH(1–34). The antagonists were injected at a 50-fold excess relative to the agonist (500 nmol/kg vs. 10 nmol/kg). The excess of antagonist peptides administered relative to PTH(1–34) in this study (50-fold excess) is identical to that used in a past study in which a bPTH(7–34) dTrp12 analogue continuously infused at 50-fold excess relative to PTH(1–34) strongly inhibited PTH-mediated calcium mobilization in thyroparathyroidectomized rats.15 In vehicle-pretreated control mice, injection of PTH(1–34) induced the expected increases in blood Ca2+ and expected decreases in blood Pi levels, which appeared near-maximal at the one- and two-hour post-injection time points, and returned to baseline by four hours post-injection (Fig. 6 a, b). In mice pre-injected with peptide 1 or 2, there was a slight dampening of the hypercalcemic and hypophosphatemic responses induced by the injected PTH(1–34), as compared to the responses induced by the agonist in the vehicle-pretreated control mice. The dampening effect was most prominent for α/β-peptide 2 in the calcium response data, for which a level of statistical significance was attained at the two-hour time point (Fig. 6a–b). It is possible that higher doses of 1 or 2 could more effectively attenuate PTH(1–34)-stimulated responses in vivo; however, a previous study showed that infusion of a bPTH(7–34) dTrp12 antagonist analogue at 200-fold excess over PTH(1–34) was only moderately more effective in inhibiting in vivo responses than infusion of the same antagonist at 50-fold excess.15 This precedent suggests that moderately higher doses of 1 or 2 would probably not substantially alter the in vivo efficacy.
Figure 6. Assessment of peptides 1 and 2 as antagonists of PTH(1–34) induced calcemic and phosphatemic responses in mice.
Data points represent mean SEM. *p<0.05 versus vehicle in n = 6 or 7 female CD1 mice. Experiments were run according to the schematic provided in supporting figure S5.(a–b) Peptide 1 or 2 or vehicle was injected four minutes prior to PTH(1–34). See methods section for further experimental details. (a) Levels of ionized calcium within the bloodstream of mice treated with 1, 2, or vehicle. (b) Levels of inorganic phosphate within the bloodstream of mice treated with 1, 2, or vehicle.(c–d) Peptide 1 or 2 or vehicle was injected one hour after PTH(1–34). Experiments were run according to the schematic provided in supporting figure S5. See methods section for further experimental details. Black arrows represent the time at which 1, 2, or vehicle were injected. (c) Levels of ionized calcium with in the bloodstream of mice treated with 1, 2, or vehicle. (d) Levels of inorganic phosphate within the bloodstream of mice treated with 1, 2, or vehicle.
In a second approach, the antagonists were injected one hour after injection of PTH(1–34), again at a 50-fold excess relative to PTH(1–34) (500 nmol/kg vs. 10 nmol/kg). This approach was adopted based on prior pharmacokinetic/pharmacodynamic data showing that PTH(1–34) clears from the circulation with a half-life of about 5–10 minutes, yet elicits robust effects on blood Ca2+ and Pi levels for ~2–3 hours after injection.21 These findings raised the possibility that the capacity to detect the effects of a PTHR1 antagonist on PTH-induced Ca2+ and Pi mobilization might be enhanced by injecting the antagonist one hour after the agonist, when the blood concentrations of the latter peptide are diminished, but its pharmacodynamic effects are still apparent. The results of experiments using this approach revealed that peptides 1 or 2 again had only small effects on the PTH(1–34)-induced responses; the effects of α/β-peptide 2, nevertheless, appeared greater than those of 1, and reached statistical significance for reversal of the hypophosphatemic response (Fig. 6c–d). These findings suggest that the PTH-induced hypophosphatemic response may be more sensitive to modulation in levels of PTHR1 signaling, and thus easier to detect, than the corresponding hypercalcemic response, as suggested by the rapid phosphaturic response observed in a previous study.50
CONCLUSIONS
The PTHR1 agonist peptide, PTH(1–34), is an effective therapeutic agent for severe osteoporosis. Antagonists or inverse agonists of PTHR1 signaling are also of therapeutic interest, because they could be useful in the treatment of hyperparathyroidism, malignancy-associated hypercalcemia and/or Jansen’s Metaphyseal chondrodysplasia.4, 6–8 Past work in vitro identified a close analogue of α-peptide 1 as both an antagonist and an inverse agonist of PTHR1.12–15 However, an attempt to reverse PTH/PTHR1-mediated hypercalcemia in vivo with this peptide in patients with primary hyperparathyroidism, and thus high levels of endogenous PTH, was not successful.16 This lack of efficacy may result in part from a capacity of PTH to bind pseudo-irreversibly to PTHR1 and stimulate signaling from within endosomal compartments;55 antagonist peptides would be unlikely to gain access to endosomal PTH-PTHR1 complexes. Another possible cause of α-peptide inactivity in vivo is short half-life. In general, conventional, α-peptides such as PTH(1–34) or 1 show poor stability in biological contexts because they are rapidly cleaved by proteases.17, 19, 56 We thus wondered whether the failure of an α-peptide antagonist related to 1 to achieve efficacy in a clinical trial with patients with hyperparathyroidism16 could be explained, at least in part, by a rapid rate of proteolysis following administration in animals. The experiments described here were intended to explore this possibility.
Our in vitro results show that α/β-peptide 2 mirrors the established PTHR1 antagonist/inverse agonist α-peptide 1 in terms of PTHR1 affinity, antagonist activity and inverse agonist activity. Moreover, α/β-peptide 2 exhibits markedly greater stability in the presence of proteases. Our experiments in mice, however, did not reveal a dramatic difference between α-peptide 1 and α/β-peptide 2 in vivo in terms of blocking the hypercalcemic or hypophosphatemic effects of exogenously added PTH(1–34). In our previous studies,34 a substantial difference was shown between the durations of bloodstream residency for PTH(1–34) and for the analogous 34-residue α/β-peptide containing the same six α-to-β replacements used here in antagonist peptide 2 (D6, figure 1). These prior results led us to surmise that antagonist α/β-peptide 2 itself would persist longer in the mouse bloodstream than antagonist α-peptide 1. This hypothesis is indirectly supported by our in vitro finding that α/β-peptide 2 is significantly less susceptible to proteolysis than is α-peptide 1. Despite these favorable in vitro findings, however, we did not observe enhanced action of the α/β-peptide in vivo. It is currently not possible to test directly whether 2 persists for longer in the bloodstream than 1 because methods commonly used to detect PTH peptides in the bloodstream rely either on recognition of PTH fragments with specific antibodies, which are not usually suitable for detecting α/β-peptides,57 or on a bioassay approach to assess PTHR1-based signaling activity present in blood samples42, which so far is not feasible for PTHR1 antagonists.
The in vivo results reported here lead us to conclude that reducing the susceptibility of a PTHR1 antagonist to proteolysis does not, by itself, lead to a major enhancement in the capacity of the antagonist to block effects of an exogenously added PTH agonist ligand on Ca2+ and Pi mobilization. Because of their relatively small size, PTH(7–34) and the α/β analogue are likely to be removed rapidly from the bloodstream by the kidney,22 such that any enhancement of in vivo stability engendered by β-residue introduction may be masked by rapid kidney filtration.
We note that our assessment of the relative importance of proteolysis versus renal filtration in determining the biological activity of PTHR1 antagonists in mice was made possible by the identification of an α/β-peptide analogue that mirrors the prototype peptide in all tested biological properties but shows substantially higher stability in the presence of proteases. Our findings highlight the potential value of slowing renal filtration for the identification of improved PTHR1 antagonists. Larger proteins are less rapidly filtered from the blood by the kidney than small proteins,58 so increasing the size of small peptides offers a mechanism for attenuating the impact of renal filtration. Covalent appendage of polyethylene glycol polymers (PEG) to peptide and protein drugs has extended the duration of biological availability59 and efforts are currently underway to apply this approach to PTH and derivatives.60
The similarity of the inverse agonist activities exhibited by peptides 1 and 2 is significant in the context of efforts to design faithful mimics of polypeptides with specific biological signaling activities. Results presented here indicate that the incorporation of six α-to-β replacements does not significantly alter the ability of resulting α/β-peptide, 2, to associate with constitutively active variants of PTHR1 and promote adoption of a PTHR1 conformation with reduced basal signaling activity. This finding is noteworthy given that a specific side chain alteration (Gly-to-dTrp12) is necessary for realization of peptide-mediated inverse agonism14 of PTHR1 and that one α-to-β replacement (position 14) is quite close to this critical site. This finding encourages future efforts to apply the backbone modification strategy to create proteolytically stabilized mimics of other bioactive polypeptides.
The inverse agonist action of α/β-peptide 2 has yet to be explored in vivo. Jansen’s Metaphyseal chondrodysplasia is a rare disease caused by PTHR1 gain-of-function variants, such as H223R, that exhibit elevated basal signaling. High levels of ligand-independent signaling diminish the capacity of the receptor to specifically respond to ligand and regulate key cell differentiation programs that operate in the developing skeleton and other tissues.8, 38 The mechanistic features of biological processes that are regulated by PTHR1 via paracrine-acting PTHrP during development, are likely to differ considerably from those that are regulated by PTHR1 via endocrine-acting PTH during the acute regulation of blood Ca2+ and Pi concentrations.61 It is thus conceivable that the capacity of a PTH antagonist/inverse agonist ligand to modulate one system versus the other would also differ. Since our current studies in vitro show that α/β-peptide 2 can suppress the basal signaling of PTHR1-H223R at least as effectively as can α-peptide 1, future studies aimed at assessing the capacity of peptide 2 to correct the skeletal defects seen in transgenic mice harboring the H223R allele62 seem warranted.
Peptide ligands that bind and inhibit signaling at PTHR1 can be modified using an α-to-β residue replacement strategy to provide α/β-peptides that retain the ability to bind receptor and inhibit signaling, but show improved stability in the presence of proteases. Although α/β-peptide 2 did not cause enduring antagonism of PTH activity in vivo, future efforts aimed at developing more effective antagonist and inverse agonist ligands of PTHR1 for therapeutic application will benefit from the availability of the approach described here for enhancing biological stability without substantially altering receptor-binding activity. Further exploration of backbone-modified peptides in the context of PTHR1 agonists, antagonists and/or inverse agonists may provide new paths toward agents with improved properties for treating a number of PTHR1-related diseases, including osteoporosis, hypoparathyroidism or Jansen’s metaphyseal chondrodysplasia.
METHODS
PTHR1 binding assays
Reported IC50 values are the average of 3 independent assays. Each assay consists of 11 data points (different concentrations) per peptide. Binding to PTHR1 was assessed by previously described competition assays44 performed in 96-well plates by using membranes from a HEK 293 derived cell line stably transfected with human PTHR1 (GP2.3 cell line). In brief, binding was assessed by using 125I-PTH(1–34) as tracer radioligand and including GTPγS in the reaction mixture (10 µM).
PTHR1 cAMP antagonism assays
cAMP antagonism was assessed using a cell line that endogenously expresses wild type PTHR1 (SGS-72 cells).46 These cells were both stably transfected with Glosensor cAMP reporter (Promega Corp.)47 Monolayers of confluent cells were pre-incubated with media (CO2 independent media, Life Sciences) containing d-luciferin (0.5 mM) in 96-well plates at room temperature until a stable baseline level of luminescence was established (30 min). Varying concentrations of antagonist peptides were then added for 15 minutes. Agonist peptides were then added, and luminescence responses were recorded using a Perkin Elmer plate reader. The maximal luminescence response (observed 12–20 min after ligand addition) was used for generating dose-response curves. Dose-response curves were fit to a sigmoidal dose-response model with variable slope.
ERK phosphorylation assays
Ligand effects on PTHR1-mediated signaling via the ERK-1/2 pathway were assessed in GP-2.3 cells. Intact cells in 96-well plates were treated with media alone (vehicle) or media containing a test ligand, and the plates were incubated at room temperature for 15 minutes. The cells were then rinsed, lysed and the lysates were analyzed for phosphorylated ERK-1/2 proteins using the antibody-based SureFire assay system (Perkin Elmer).
PTHR1 cAMP inverse agonism assays
cAMP inverse agonism was assessed using HEK-293-derived cell lines stably transfected to express Glosensor cAMP reporter and PTHR1 variants (H223R in the GHR10 cell line or T410P in the GTP4 cell line).13 These receptor variants induce high levels of cAMP signaling in the absence of ligands, relative to that induced by wild type PTHR1.13 Monolayers of confluent HEK 293 cells were incubated with buffer containing d-luciferin (0.5 mM) and isobutylmethylxanthine (2 mM) in 96-well plates at room temperature for 30 minutes. Varying concentrations of inverse agonist peptides were then added, and luminescence was recorded over 30 minutes using a Perkin Elmer plate reader. Luminescence readings were taken every two minutes. Readings made 30 minutes after inverse agonist addition were used to construct dose response curves.
In Vivo Pharmacology: Calcemic Response
Mice (CD1, female, age 9–12 weeks) were treated in accordance with the ethical guidelines adopted by Massachusetts General Hospital. Mice (n=6–7 per group) were injected subcutaneously with vehicle (10 mM citric acid/150 mM NaCl/0.05% Tween-80, pH 5.0) or vehicle containing agonist (human PTH(1–34)) at a dose of 10 nmol/kg body weight or antagonist (1 or 2) at a dose of 500 nmol/kg body weight. Prior to injection, mice were grouped according to basal blood calcium concentrations to ensure each group possessed similar average (mean) blood ionized calcium levels at t=0. Groups were not statistically different on basis of mean basal blood calcium concentration at t=0. Blood was withdrawn just prior to injection (t=0) or at times thereafter. Tail vein blood was collected and immediately used for analysis. Blood Ca2+ and phosphate concentration was measured with a Siemens RapidLab 348 Ca2+/pH analyzer.
Protease Susceptibility Assays
An HPLC assay was used to assess proteolytic susceptibility.30 See the supporting information detailed methodological protocols.
Peptide Synthesis and Purification
Peptides were synthesized as C-terminal amides on NovaPEG rink amide resin (EMD) using previously reported microwave-assisted solid-phase conditions, based on Fmoc protection of main chain amino groups.30 See supporting information for further methodological details.
Data calculations
Data were processed by using the Microsoft Excel and GraphPad Prism 4.0 software packages. Data from binding and cAMP dose–response assays were analyzed using a sigmoidal dose–response model with variable slope as previously used for analysis of data of this type.34 Data sets were statistically compared by using Student’s t test (two-tailed) assuming unequal variances for the two sets. Statistical calculations were carried out assuming Gaussian data distribution.
Supplementary Material
Acknowledgments
This research was supported by National Institutes of Health (NIH) grant P01-DK11794 (T.J.G) and R01 GM-056414 (S.H.G.). R.W.C. was supported in part by a Biotechnology Training Grant from NIGMS (T32 GM008349).
Footnotes
Supporting Information Available: Supplementary methods, supporting figures 1–6 and supporting table 1 are available free of charge at pubs.acs.org.
References
- 1.Urena P, Kong XF, Abou-Samra AB, Juppner H, Kronenberg HM, Potts JT, Jr, Segre GV. Parathyroid hormone (PTH)/PTH-related peptide receptor messenger ribonucleic acids are widely distributed in rat tissues. Endocrinology. 1993;133:617–623. doi: 10.1210/endo.133.2.8393771. [DOI] [PubMed] [Google Scholar]
- 2.Neer RM, Arnaud CD, Zanchetta JR, Prince R, Gaich GA, Reginster JY, Hodsman AB, Eriksen EF, Ish-Shalom S, Genant HK, Wang OH, Mitlak BH. Effect of parathyroid hormone (1–34) on fractures and bone mineral density in postmenopausal women with osteoporosis. N. Engl. J. Med. 2001;344:1434–1441. doi: 10.1056/NEJM200105103441904. [DOI] [PubMed] [Google Scholar]
- 3.Gardella TJ, Vilardaga J-P. International Union of Basic and Clinical Pharmacology. XCIII. The Parathyroid Hormone Receptors-Family B G Protein-Coupled Receptors. Pharmacol. Rev. 2015;67:310–337. doi: 10.1124/pr.114.009464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cheloha RW, Gellman SH, Vilardaga J-P, Gardella TJ. PTH receptor-1 signalling--mechanistic insights and therapeutic prospects. Nat. Rev. Endocrinol. 2015 doi: 10.1038/nrendo.2015.139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Uzawa T, Hori M, Ejiri S, Ozawa H. COMPARISON OF THE EFFECTS OF INTERMITTENT AND CONTINUOUS ADMINISTRATION OF HUMAN PARATHYROID HORMONE(1–34) ON RAT BONE. Bone. 1995;16:477–484. doi: 10.1016/8756-3282(95)90194-9. [DOI] [PubMed] [Google Scholar]
- 6.Fraser WD. Hyperparathyroidism. Lancet. 2009;374:145–158. doi: 10.1016/S0140-6736(09)60507-9. [DOI] [PubMed] [Google Scholar]
- 7.Stewart AF. Clinical practice. Hypercalcemia associated with cancer. N. Engl. J. Med. 2005;352:373–379. doi: 10.1056/NEJMcp042806. [DOI] [PubMed] [Google Scholar]
- 8.Schipani E, Kruse K, Juppner H. A CONSTITUTIVELY ACTIVE MUTANT PTH-PTHRP RECEPTOR IN JANSEN-TYPE METAPHYSEAL CHONDRODYSPLASIA. Science. 1995;268:98–100. doi: 10.1126/science.7701349. [DOI] [PubMed] [Google Scholar]
- 9.Rosenblatt M, Segre GV, Tyler GA, Shepard GL, Nussbaum SR, Potts JT. IDENTIFICATION OF A RECEPTOR-BINDING REGION IN PARATHYROID-HORMONE. Endocrinology. 1980;107:545–550. doi: 10.1210/endo-107-2-545. [DOI] [PubMed] [Google Scholar]
- 10.Horiuchi N, Holick MF, Potts JT, Rosenblatt M. A PARATHYROID-HORMONE INHIBITOR INVIVO - DESIGN AND BIOLOGICAL EVALUATION OF A HORMONE ANALOG. Science. 1983;220:1053–1055. doi: 10.1126/science.6302844. [DOI] [PubMed] [Google Scholar]
- 11.Doppelt SH, Neer RM, Nussbaum SR, Federico P, Potts JT, Rosenblatt M. INHIBITION OF THE INVIVO PARATHYROID HORMONE-MEDIATED CALCEMIC RESPONSE IN RATS BY A SYNTHETIC HORMONE ANTAGONIST. Proc. Natl. Acad. Sci. U. S. A. 1986;83:7557–7560. doi: 10.1073/pnas.83.19.7557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chorev M, Goldman ME, McKee RL, Roubini E, Levy JJ, Gay CT, Reagan JE, Fisher JE, Caporale LH, Golub EE, Caulfield MP, Nutt RF, Rosenblatt M. MODIFICATIONS OF POSITION-12 IN PARATHYROID-HORMONE AND PARATHYROID-HORMONE RELATED PROTEIN - TOWARD THE DESIGN OF HIGHLY POTENT ANTAGONISTS. Biochemistry. 1990;29:1580–1586. doi: 10.1021/bi00458a032. [DOI] [PubMed] [Google Scholar]
- 13.Carter PH, Dean T, Bhayana B, Khatri A, Rajur R, Gardella TJ. Actions of the Small Molecule Ligands SW106 and AH-3960 on the Type-1 Parathyroid Hormone Receptor. Mol. Endocrinol. 2015;29:307–321. doi: 10.1210/me.2014-1129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gardella TJ, Luck MD, Jensen GS, Schipani E, Potts JT, Jr, Juppner H. Inverse agonism of amino-terminally truncated parathyroid hormone (PTH) and PTH-related peptide (PTHrP) analogs revealed with constitutively active mutant PTH/PTHrP receptors. Endocrinology. 1996;137:3936–3941. doi: 10.1210/endo.137.9.8756569. [DOI] [PubMed] [Google Scholar]
- 15.Dresner-Pollak R, Yang QM, Behar V, Nakamoto C, Chorev M, Rosenblatt M. Evaluation in vivo of a potent parathyroid hormone antagonist: [Nle8,18,D-Trp12,Tyr34]bPTH(7–34)NH2. J. Bone Miner. Res. 1996;11:1061–1065. doi: 10.1002/jbmr.5650110804. [DOI] [PubMed] [Google Scholar]
- 16.Rosen HN, Lim M, Garber J, Moreau S, Bhargava HN, Pallotta J, Spark R, Greenspan S, Rosenblatt M, Chorev M. The effect of PTH antagonist BIM-44002 on serum calcium and PTH levels in hypercalcemic hyperparathyroid patients. Calcif. Tissue Int. 1997;61:455–459. doi: 10.1007/s002239900367. [DOI] [PubMed] [Google Scholar]
- 17.Vlieghe P, Lisowski V, Martinez J, Khrestchatisky M. Synthetic therapeutic peptides: science and market. Drug Discovery Today. 2010;15:40–56. doi: 10.1016/j.drudis.2009.10.009. [DOI] [PubMed] [Google Scholar]
- 18.Werle M, Samhaber A, Bernkop-Schnurch A. Degradation of teriparatide by gastro-intestinal proteolytic enzymes. J. Drug Targeting. 2006;14:109–115. doi: 10.1080/10611860600647934. [DOI] [PubMed] [Google Scholar]
- 19.Liao S, Qie JK, Xue M, Zhang ZQ, Liu KL, Ruan JX. Metabolic stability of human parathyroid hormone peptide hPTH (1–34) in rat tissue homogenates: kinetics and products of proteolytic degradation. Amino Acids. 2010;38:1595–1605. doi: 10.1007/s00726-009-0376-y. [DOI] [PubMed] [Google Scholar]
- 20.Schetz JA, Mayr CA, Taylor JE, Rosenblatt M, Chorev M, Davis TP. DISTRIBUTION AND PHARMACOKINETICS OF A POTENT PEPTIDE ANTAGONIST OF PARATHYROID-HORMONE AND PARATHYROID HORMONE-RELATED PROTEIN IN THE RAT. J. Pharmacol. Exp. Ther. 1995;274:1456–1462. [PubMed] [Google Scholar]
- 21.Kent GN, Loveridge N, Reeve J, Zanelli JM. PHARMACOKINETICS OF SYNTHETIC HUMAN PARATHYROID-HORMONE 1–34 IN MAN MEASURED BY CYTOCHEMICAL BIOASSAY AND RADIOIMMUNOASSAY. Clin. Sci. 1985;68:171–177. doi: 10.1042/cs0680171. [DOI] [PubMed] [Google Scholar]
- 22.Serada M, Sakurai-Tanikawa A, Igarashi M, Mitsugi K, Takano T, Shibusawa K, Kohira T. The role of the liver and kidneys in the pharmacokinetics of subcutaneously administered teriparatide acetate in rats. Xenobiotica. 2012;42:398–407. doi: 10.3109/00498254.2011.622811. [DOI] [PubMed] [Google Scholar]
- 23.Brown RC, Silver AC, Woodhead JS. BINDING AND DEGRADATION OF NH2-TERMINAL PARATHYROID-HORMONE BY OPOSSUM KIDNEY-CELLS. Am. J. Physiol. 1991;260:E544–E552. doi: 10.1152/ajpendo.1991.260.4.E544. [DOI] [PubMed] [Google Scholar]
- 24.Yamaguchi T, Fukase M, Kido H, Sugimoto T, Katunuma N, Chihara K. MEPRIN IS PREDOMINANTLY INVOLVED IN PARATHYROID-HORMONE DEGRADATION BY THE MICROVILLAR MEMBRANES OF RAT-KIDNEY. Life Sci. 1994;54:381–386. doi: 10.1016/0024-3205(94)00795-0. [DOI] [PubMed] [Google Scholar]
- 25.Bringhurst FR, Stern AM, Yotts M, Mizrahi N, Segre GV, Potts JT. PERIPHERAL METABOLISM OF PTH-FATE OF BIOLOGICALLY-ACTIVE AMINO TERMINUS INVIVO. Am. J. Physiol. 1988;255:E886–E893. doi: 10.1152/ajpendo.1988.255.6.E886. [DOI] [PubMed] [Google Scholar]
- 26.Diment S, Martin KJ, Stahl PD. CLEAVAGE OF PARATHYROID-HORMONE IN MACROPHAGE ENDOSOMES ILLUSTRATES A NOVEL PATHWAY FOR INTRACELLULAR PROCESSING OF PROTEINS. J. Biol. Chem. 1989;264:13403–13406. [PubMed] [Google Scholar]
- 27.Daugaard H, Egfjord M, Olgaard K. METABOLISM OF INTACT PARATHYROID-HORMONE IN ISOLATED PERFUSED RAT-LIVER AND KIDNEY. Am. J. Physiol. 1988;254:E740–E748. doi: 10.1152/ajpendo.1988.254.6.E740. [DOI] [PubMed] [Google Scholar]
- 28.Hilpert J, Nykjaer A, Jacobsen C, Wallukat G, Nielsen R, Moestrup SK, Haller H, Luft FC, Christensen EI, Willnow TE. Megalin antagonizes activation of the parathyroid hormone receptor. J. Biol. Chem. 1999;274:5620–5625. doi: 10.1074/jbc.274.9.5620. [DOI] [PubMed] [Google Scholar]
- 29.Werner HM, Cabalteja CC, Horne WS. Peptide Backbone Composition and Protease Susceptibility: Impact of Modification Type, Position, and Tandem Substitution. Chem Bio Chem. 2015;17:712–718. doi: 10.1002/cbic.201500312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Horne WS, Johnson LM, Ketas TJ, Klasse PJ, Lu M, Moore JP, Gellman SH. Structural and biological mimicry of protein surface recognition by alpha/beta-peptide foldamers. Proc. Natl. Acad. Sci. U. S. A. 2009;106:14751–14756. doi: 10.1073/pnas.0902663106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Boersma MD, Haase HS, Peterson-Kaufman KJ, Lee EF, Clarke OB, Colman PM, Smith BJ, Horne WS, Fairlie WD, Gellman SH. Evaluation of Diverse alpha/beta-Backbone Patterns for Functional alpha-Helix Mimicry: Analogues of the Bim BH3 Domain. J. Am. Chem. Soc. 2012;134:315–323. doi: 10.1021/ja207148m. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Checco JW, Kreitler DF, Thomas NC, Belair DG, Rettko NJ, Murphy WL, Forest KT, Gellman SH. Targeting diverse protein-protein interaction interfaces with alpha/beta-peptides derived from the Z-domain scaffold. Proc. Natl. Acad. Sci. U. S. A. 2015 doi: 10.1073/pnas.1420380112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Johnson LM, Mortenson DE, Yun HG, Horne WS, Ketas TJ, Lu M, Moore JP, Gellman SH. Enhancement of alpha-Helix Mimicry by an alpha/beta-Peptide Foldamer via Incorporation of a Dense Ionic Side-Chain Array. J. Am. Chem. Soc. 2012;134:7317–7320. doi: 10.1021/ja302428d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cheloha RW, Maeda A, Dean T, Gardella TJ, Gellman SH. Backbone modification of a polypeptide drug alters duration of action in vivo. Nat. Biotechnol. 2014;32:653–655. doi: 10.1038/nbt.2920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Johnson LM, Barrick S, Hager MV, McFedries A, Homan EA, Rabaglia ME, Keller MP, Attie AD, Saghatelian A, Bisello A, Gellman SH. A Potent alpha/beta-Peptide Analogue of GLP-1 with Prolonged Action in Vivo. J. Am. Chem. Soc. 2014;136:12848–12851. doi: 10.1021/ja507168t. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Levine PM, Craven TW, Bonneau R, Kirshenbaum K. Semisynthesis of Peptoid-Protein Hybrids by Chemical Ligation at Serine. Org. Lett. 2014;16:512–515. doi: 10.1021/ol4033978. [DOI] [PubMed] [Google Scholar]
- 37.Liu Y, Cai Y, Liu W, Li X-H, Rhoades E, Yan ECY. Triblock peptide-linker-lipid molecular design improves potency of peptide ligands targeting family B G protein-coupled receptors. Chem. Commun. 2015;51:6157–6160. doi: 10.1039/c5cc00301f. [DOI] [PubMed] [Google Scholar]
- 38.Schipani E, Langman CB, Parfitt AM, Jensen GS, Kikuchi S, Kooh SW, Cole WG, Juppner H. Constitutively activated receptors for parathyroid hormone and parathyroid hormone-related peptide in Jansen's metaphyseal chondrodysplasia. N. Engl. J. Med. 1996;335:708–714. doi: 10.1056/NEJM199609053351004. [DOI] [PubMed] [Google Scholar]
- 39.Goldring SR, Roelke MS, Bringhurst FR, Rosenblatt M. DIFFERENTIAL-EFFECTS OF PARATHYROID-HORMONE RESPONSIVE CULTURED HUMAN-CELLS ON BIOLOGICAL-ACTIVITY OF PARATHYROID-HORMONE AND PARATHYROID-HORMONE INHIBITORY ANALOGS. Biochemistry. 1985;24:513–518. doi: 10.1021/bi00323a040. [DOI] [PubMed] [Google Scholar]
- 40.Carter PH, Petroni BD, Gensure RC, Schipani E, Potts JT, Jr, Gardella TJ. Selective and nonselective inverse agonists for constitutively active type-1 parathyroid hormone receptors: evidence for altered receptor conformations. Endocrinology. 2001;142:1534–1545. doi: 10.1210/endo.142.4.8103. [DOI] [PubMed] [Google Scholar]
- 41.Shimizu M, Potts JT, Gardella TJ. Minimization of parathyroid hormone - Novel amino-terminal parathyroid hormone fragments with enhanced potency in activating the type-1 parathyroid hormone receptor. J. Biol. Chem. 2000;275:21836–21843. doi: 10.1074/jbc.M909861199. [DOI] [PubMed] [Google Scholar]
- 42.Okazaki M, Ferrandon S, Vilardaga JP, Bouxsein ML, Potts JT, Gardella TJ. Prolonged signaling at the parathyroid hormone receptor by peptide ligands targeted to a specific receptor conformation. Proc. Natl. Acad. Sci. U. S. A. 2008;105:16525–16530. doi: 10.1073/pnas.0808750105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hoare SRJ, Gardella TJ, Usdin TB. Evaluating the signal transduction mechanism of the parathyroid hormone 1 receptor - Effect of receptor-G-protein interaction on the ligand binding mechanism and receptor conformation. J. Biol. Chem. 2001;276:7741–7753. doi: 10.1074/jbc.M009395200. [DOI] [PubMed] [Google Scholar]
- 44.Dean T, Linglart A, Mahon MJ, Bastepe M, Juppner H, Potts JT, Gardella TJ. Mechanisms of ligand binding to the parathyroid hormone (PTH)/PTH-related protein receptor: Selectivity of a modified PTH(1–15) Radioligand for G alpha(S)-coupled receptor conformations. Mol. Endocrinol. 2006;20:931–943. doi: 10.1210/me.2005-0349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Rodan SB, Imai Y, Thiede MA, Wesolowski G, Thompson D, Barshavit Z, Shull S, Mann K, Rodan GA. CHARACTERIZATION OF A HUMAN OSTEOSARCOMA CELL-LINE (SAOS-2) WITH OSTEOBLASTIC PROPERTIES. Cancer Res. 1987;47:4961–4966. [PubMed] [Google Scholar]
- 46.Lee S, Mannstadt M, Guo J, Kim SM, Yi H-S, Khatri A, Dean T, Okazaki M, Gardella TJ, Jüppner H. A Homozygous [Cys25]PTH(1–84) Mutation That Impairs PTH/PTHrP Receptor Activation Defines a Novel Form of Hypoparathyroidism. J. Bone Miner. Res. 2015:1803–1813. doi: 10.1002/jbmr.2532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Binkowski BF, Butler BL, Stecha PF, Eggers CT, Otto P, Zimmerman K, Vidugiris G, Wood MG, Encell LP, Fan F, Wood KV. A Luminescent Biosensor with Increased Dynamic Range for Intracellular cAMP. ACS Chem. Biol. 2011;6:1193–1197. doi: 10.1021/cb200248h. [DOI] [PubMed] [Google Scholar]
- 48.Jonsson KB, John MR, Gensure RC, Gardella TJ, Juppner H. Tuberoinfundibular peptide 39 binds to the parathyroid hormone (PTH)/PTH-related peptide receptor, but functions as an antagonist. Endocrinology. 2001;142:704–709. doi: 10.1210/endo.142.2.7945. [DOI] [PubMed] [Google Scholar]
- 49.Shimizu M, Carter PH, Khatri A, Potts JT, Gardella TJ. Enhanced activity in parathyroid hormone-(1–14) and -(1–11): Novel peptides for probing ligand-receptor interactions. Endocrinology. 2001;142:3068–3074. doi: 10.1210/endo.142.7.8253. [DOI] [PubMed] [Google Scholar]
- 50.Maeda A, Okazaki M, Baron DM, Dean T, Khatri A, Mahon M, Segawa H, Abou-Samra AB, Jueppner H, Bloch KD, Potts JT, Jr, Gardella TJ. Critical role of parathyroid hormone (PTH) receptor-1 phosphorylation in regulating acute responses to PTH. Proc. Natl. Acad. Sci. U. S. A. 2013;110:5864–5869. doi: 10.1073/pnas.1301674110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Togari A, Arai M, Mizutani S, Koshihara Y, Nagatsu T. Expression of mRNAs for neuropeptide receptors and beta-adrenergic receptors in human osteoblasts and human osteogenic sarcoma cells. Neurosci. Lett. 1997;233:125–128. doi: 10.1016/s0304-3940(97)00649-6. [DOI] [PubMed] [Google Scholar]
- 52.Cupp ME, Nayak SK, Adem AS, Thomsen WJ. Parathyroid hormone (PTH) and PTH-related peptide domains contributing to activation of different PTH receptor-mediated signaling pathways. J. Pharmacol. Exp. Ther. 2013;345:404–418. doi: 10.1124/jpet.112.199752. [DOI] [PubMed] [Google Scholar]
- 53.Gesty-Palmer D, Flannery P, Yuan L, Corsino L, Spurney R, Lefkowitz RJ, Luttrell LM. A beta-Arrestin-Biased Agonist of the Parathyroid Hormone Receptor (PTH1R) Promotes Bone Formation Independent of G Protein Activation. Science Translational Medicine. 2009;1 doi: 10.1126/scitranslmed.3000071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Rawlings ND, Waller M, Barrett AJ, Bateman A. MEROPS: the database of proteolytic enzymes, their substrates and inhibitors. Nucleic Acids Res. 2014;42:D503–D509. doi: 10.1093/nar/gkt953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Vilardaga JP, Jean-Alphonse FG, Gardella TJ. Endosomal generation of cAMP in GPCR signaling. Nat. Chem. Biol. 2014;10:700–706. doi: 10.1038/nchembio.1611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Werle M, Bernkop-Schnurch A. Strategies to improve plasma half life time of peptide and protein drugs. Amino Acids. 2006;30:351–367. doi: 10.1007/s00726-005-0289-3. [DOI] [PubMed] [Google Scholar]
- 57.Cheloha RW, Sullivan JA, Wang T, Sand JM, Sidney J, Sette A, Cook ME, Suresh M, Gellman SH. Consequences of Periodic alpha-to-beta(3) Residue Replacement for Immunological Recognition of Peptide Epitopes. ACS Chem. Biol. 2015;10:844–854. doi: 10.1021/cb500888q. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Maack T, Johnson V, Kau ST, Figueiredo J, Sigulem D. RENAL FILTRATION, TRANSPORT, AND METABOLISM OF LOW-MOLECULAR-WEIGHT PROTEINS - REVIEW. Kidney Int. 1979;16:251–270. doi: 10.1038/ki.1979.128. [DOI] [PubMed] [Google Scholar]
- 59.Turecek PL, Bossard MJ, Schoetens F, Ivens IA. PEGylation of Biopharmaceuticals: A Review of Chemistry and Nonclinical Safety Information of Approved Drugs. J. Pharm. Sci. 2016;105:460–475. doi: 10.1016/j.xphs.2015.11.015. [DOI] [PubMed] [Google Scholar]
- 60.Jun G, Ashok K, Thomas D, Monica R, Braden AC, John TP, Harald WJ, Thomas JG. Prolonged Pharmacokinetic and Pharmacodynamic Actions of a Pegylated Parathyroid Hormone Peptide Fragment, In. Endocr. Rev. 2016:SUN-361–SUN-361. Endocrine Society. [Google Scholar]
- 61.Vilardaga JP, Romero G, Friedman PA, Gardella TJ. Molecular basis of parathyroid hormone receptor signaling and trafficking: a family B GPCR paradigm. Cell. Mol. Life Sci. 2011;68:1–13. doi: 10.1007/s00018-010-0465-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Schipani E, Lanske B, Hunzelman J, Luz A, Kovacs CS, Lee K, Pirro A, Kronenberg HM, Juppner H. Targeted expression of constitutively active receptors for parathyroid hormone and parathyroid hormone-related peptide delays endochondral bone formation and rescues mice that lack parathyroid hormone-related peptide. Proc. Natl. Acad. Sci. U. S. A. 1997;94:13689–13694. doi: 10.1073/pnas.94.25.13689. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.