Abstract
Background
African American women perform low levels of physical activity and are disproportionally burdened by associated cardiometabolic disease conditions (i.e. 57% are obese, 49% have cardiovascular disease) The marked health disparities among African American women indicate the need for innovative strategies to promote physical activity to help attenuate the chronic disease health disparities in this high-risk population. Culturally tailoring PA programs to address the sociocultural norms, values, beliefs, and behaviors of African American women is an advantageous strategy to enhance physical activity promotion efforts. The purpose of this article is to discuss critical aspects for researchers to consider when designing physical activity programs for African American women and to present a conceptual framework to guide intervention development.
Methods
Development of the framework was based on our previous physical activity research with African American women, seminal literature on the topics of cultural adaptation and health promotion, sociological and theoretical perspectives on the role of women in African American culture, and key determinants of physical activity engagement among African American women.
Results
Three key concepts are discussed in the conceptual framework: 1) Developmental milestones and life stage transitions of African American women, 2) Historical, social and cultural influences associated with physical activity engagement, and 3) Intervention delivery strategies.
Discussion
Using the framework to guide intervention development has the potential to enhance the physical activity and health outcomes of a physical activity program for African American women.
Keywords: Black, African American, Women, cultural tailoring, exercise, physical activity, culture
INTRODUCTION
African American women are one of the least active demographic groups in the United States. Recent self-report data from the National Health Interview Survey (NHIS) show that only 36% of African American (AA) women achieve the national physical activity (PA) guidelines of 150 minutes per week of at least moderate-intensity PA [1]. These levels are substantially lower than the PA level of the U.S. population as a whole (i.e., 50% achieve the recommended PA levels), as well was AA men (49%) and White women (49%). The low PA levels of AA women are concerning due to the disproportionate disease burdened exhibited in this population. For example, national data show that 57% are obese (BMI≥30) [2], with nearly half (48.9%) of all AA women in the United States having cardiovascular disease [3] and 9% having a diagnosis type II diabetes [4]. Given PA is an established mechanism to prevent and treat chronic disease conditions [5, 6], there is an urgent need to identify effective strategies to promote PA and help attenuate the development of cardiometabolic diseases in this high-risk population.
Over the past decade, there has been an increased focus in the development of culturally relevant PA interventions for AA women. Incorporating aspects of culture into the design of PA programs for AA women is believed to increase the acceptance, salience, and effectiveness of the program [7, 8]. While peripheral attention may be paid to cultural tailoring in intervention design, few researchers have clearly delineated how their culturally tailored PA programs have addressed sociocultural norms associated with PA engagement among AA women. A 2014 review of PA interventions targeting AAs published between 2009 and 2013, Whitt-Glover [8] and colleagues reported that only seven (5 of which targeted exclusively on AA women) of the 16 interventions reviewed were culturally-tailored at a “deep structure” level. Earlier reviews on this topic have reported similar outcomes [9–11]. “Deep structure” cultural tailoring involves recognizing a group’s shared history, cultural values, social norms, beliefs, and behaviors, and leveraging these aspects to promote behavior change [12]. Accordingly, we speculate that the modest results of PA programs targeting AA women to date may, in part, be related to the lack of ample cultural tailoring to this high-risk group.
This article will discuss critical aspects for researchers to consider when designing PA interventions for AA women. Specifically, we: a) present a conceptual framework for researchers to consider when designing PA promotion efforts for AA women, and b) highlight how the various aspects of AA culture can be incorporated into PA programs for AA women. We also provide practical examples to illustrate how culture can be successfully incorporated in PA promotion programs for AA women.
METHODS
Development of our framework was predicated on our PA intervention research among AA women [13–20], seminal literature focused on the topics of cultural adaptation and health promotion programs [21, 12, 22], sociological and theoretical perspectives on the role of women in AA culture (i.e., Womanist, Afrocentric, and Black Feminist) [23–25], and key determinants of PA engagement among AA women [26, 27]. We used a life course perspective [28] to inform model development because it allowed us to focus on generational/cohort characteristics of AA culture and life events that AA women experience throughout the life span. Giele and Elder [29] define the life course as "a sequence of socially defined events and roles that the individual enacts over time." Further, they explain that developmental transitions are rooted in norms and expectations related to age, developmental stage, and social transitions [30]. The implication here is that age-differentiated social phenomena are distinct from biologically-influenced life-cycle stages and the life span. While this is true, biology also plays a role and to understand the life course in various populations we need to develop a sense of how unique biologically-driven life course patterns might interact with cultural practices. Given culture is a continually evolving phenomenon that involves acceptance of new ideas while resisting change in others [31], a life course perspective provides the opportunity for us to examine cultural characteristics associated with PA engagement among AA women as a whole, while acknowledging that there may be subtle differences in cultural norms among AA women according to their development stage of life.
RESULTS
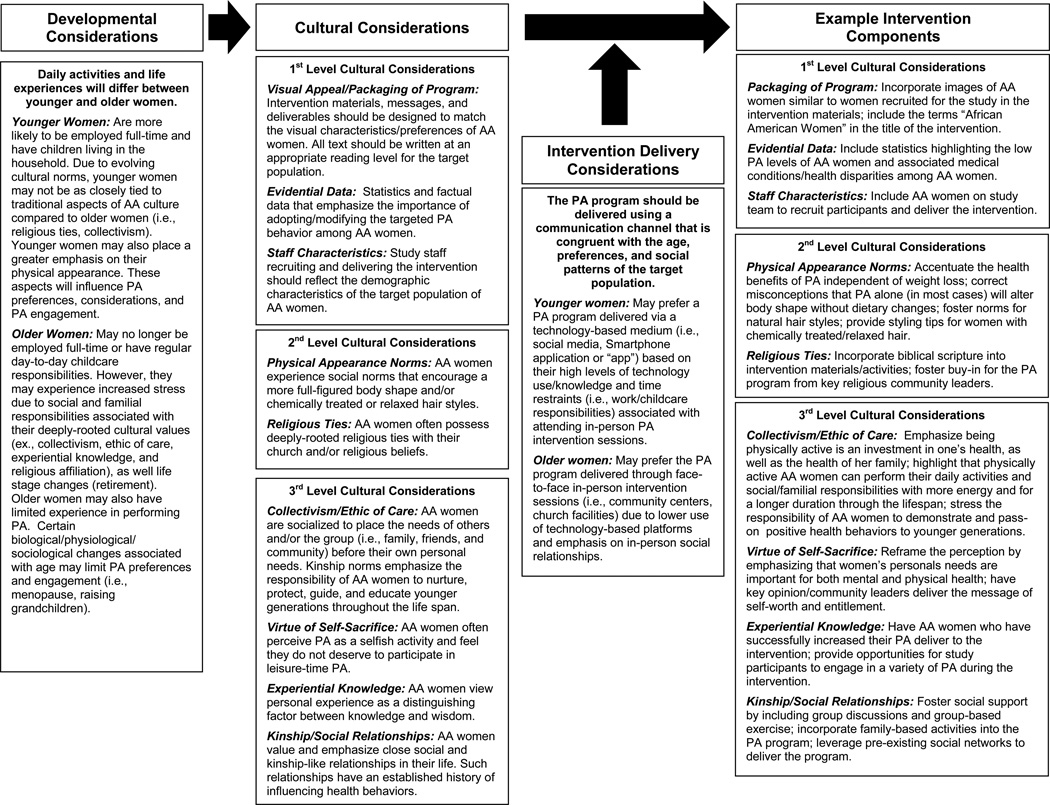
Figure 1 illustrates our framework for culturally tailoring PA programs for AA women. We propose 3 key aspects for researchers to consider when designing PA programs: 1) developmental stage of life of AA women, 2) lived cultural experiences and social norms of AA women, and 3) intervention delivery strategies.
Fig. 1.
Conceptual framework to guide development of cultural relevant physical activity programs for African American women
Developmental Considerations
When developing PA programs for AA women, researchers should consider the developmental stage of life of their intended population, as intervention materials and activities for younger women will likely differ from those targeting older women. For the purposes of the current article, we generally we refer to “younger” women as those between the approximate ages of a 18 and 60 years old and “older” women as 60 years and older. However, we acknowledge that there is some overlap in the PA-related concepts discussed between these two age groups discussed, particularly, among middle-aged AA women (i.e., women between the approximate ages of 50 and 70). Further, given an AA woman’s lifetime experiences with PA will vary widely according to her socioeconomic status, geographical region of residence, and family history, researchers should rely on their formative research with their target population to ensure aspects discussed in this section are relevant to their target population of AA women.
Younger women, regardless of race or ethnicity, are more likely to be employed full-time [32], have children living in the household [33], and have previous experience with performing a variety of physical activities. These aspects will influence their availability and motivation to perform PA. The biological/physiological development among younger women (independent of race) will also influence their preference and ability to engage in PA. Younger women are more likely to be willing to engage in vigorous and high impact physical activities (i.e., running, kickboxing, team sports) than older women [34]. However, despite these commonalities among young women of all races and ethnicities, many AA women face unique barriers to PA that are not commonly reported among women of other racial/ethnic backgrounds. Socialization trends of younger AA women may place a greater emphasis on physical appearance concerns (i.e., hair care maintenance and body shape preferences) associated with PA [35, 36] (see Cultural Considerations section below), which can limit their engagement in PA. Younger AA women may also not be as deeply tied to important aspects of AA culture (i.e., collectivism, religiosity; see Cultural Considerations section below) [37].
Older AA women, on the other hand, may experience a variety of different biological, social, and cultural phenomena that influence their engagement in PA. Menopause, reduced joint function, musculoskeletal pain, increased weight, and loss of balance and flexibility may influence an older women’s engagement in PA [38–41]. These physiological processes associated with aging will occur among all women independent of race or ethnic background. Likewise, older women, regardless of race or ethnicity, are more likely to be retired or no longer working in a full-time employment position [32]. Intuitively, this may be viewed as a benefit to researchers trying to promote PA, as older women may appear to have more available time to perform PA. However, older AA women, particularly those from lower socioeconomic backgrounds, report specific barriers to PA that are not as commonly reported among women of other races. For example, older AA report placing a greater emphasis on ensuring the needs of their family and friends and are met before their own personal needs [42–46], which can ultimately influence their time and motivation to perform PA. Older AA women are also frequently tasked with the caretaking responsibilities of their grandchildren and extended family members, which further limits their ability to engage in PA on a regular basis.
Socialization patterns of older AA women also will influence their perspective of- and motivation to engage in PA. Historically speaking, older AA women have had fewer opportunities to engage in PA than their White or younger AA counterparts. Segregation, discrimination, and negative childhood experiences have all been cited as reasons for lack of PA exposure and engagement [36, 47, 43]. Prevalent cultural norms and gender roles at the time when older AA women were children appear to have further discouraged PA. Older AA women report that PA was discouraged because it was not “ladylike” or because it was viewed as an activity for only White women [40]. Likewise, middle-aged-to-older AA women also have suggested that a historical lack of physically active AA role models influences their perception, awareness, and desire to perform PA [40, 43, 46, 48, 49–52].
In order to meet the PA needs and preferences of older AA women, researchers should be cognizant of the fact than many older AA have limited or no experience with leisure-time PA. Programs should be designed to acknowledge historical factors associated the lack of PA engagement among older AA women and use culturally sensitive strategies (see Cultural Considerations section below) to increase awareness and motivation to perform PA. Developmental issues associated with age should be carefully considered when promoting PA in older women. High-impact and complex movement activities (i.e., high intensity interval training, kickboxing) may not be appropriate for some older women due to age-related declines in motor control and reduced joint and muscular function. Instead less complex and lower impact activities such as walking, dancing, and resistance band strength training should be considered and have been reported as preferred PA modalities among older women [53–58]. Highlighting that various household chores (ex., mopping, vacuuming, and gardening) are considered moderate-to-vigorous PA may also resonate with older women, as previous research suggest some older AA women do not perceive such activities as PA or “exercise” [59, 60]. Moreover, asking older AA women to identify the types of PA they enjoy performing and potential strategies to overcome age-related constraints to PA during formative phases of intervention development will help ensure the types of PA encouraged by a program coincide with the preferences of the population.
Cultural Considerations
AA women possess a variety of sociocultural norms that can influence their engagement in PA. Here, we draw from and expand on the published literature focused on cultural tailoring behavior change interventions [12, 21, 22, 61, 62, 63, 64] and propose 3 levels of cultural considerations for researchers to take into account when developing culturally relevant PA programs for AA women (see Figure 1). First level considerations refer to the overt characteristics of an intervention that can influence the appeal, salience, and acceptance of the program among the target population. Considerations at this level include the visual appearance and packaging of a program (i.e., images included in study materials, color scheme, text size, fonts), as well as the physical and social characteristics of the research team. Second level considerations involve cultural aspects that are not necessarily deeply embedded into social patterns and norms of traditional AA culture, but play an important role in PA engagement among AA women. Example considerations at this level include body shape preferences, hair style concerns, and religious/spiritual ties. Third level considerations are those related to deeply-rooted sociocultural norms and behavioral patterns of AA women. Example third level considerations include an AA women’s ethic of caring (i.e., placing the needs of other before the needs of themselves), self-sacrificing behaviors, and emphasis on the importance of social and kinship-type relationships. In the subsequent paragraphs of this section, we will provide a more in-depth description of each of these cultural consideration levels and use practical examples to illustrate how these considerations can be incorporated into PA programs for AA women.
First Level Cultural Considerations
First level cultural considerations refer to matching the characteristics and packaging of the PA program to the social and behavioral characteristics of the target population. Considerations at this level have also been termed as “surface structure” [12] or “peripheral” [61] by other researchers. Attending to this first level of cultural relevance is imperative, as it enhances the perceived relevance and acceptance of the intervention among members of the target population [12, 61, 65]. If this level is not addressed, AA women may not perceive the PA program as designed for them, which can lead to disinterest in the program, as well as attrition. In this section, we discuss 3 first level considerations for researchers to consider: a) the visual appeal and packaging of the program, b) the use of evidential data, and c) staff characteristics.
Visual Appeal/Packaging of the Program
Intervention materials should be aesthetically pleasing and perceived as relevant by the target population. This includes the name of the program, as well as the images, videos, color schemes, and fonts included in the intervention materials [12, 63, 65]. Attention to the visual aspects of the program should also be considered when designing recruitment materials, as women who perceive that a PA program is designed for them are more likely to enroll [66].
When considering the name of a PA promotion, elicit feedback from members of the target population, as they can provide insight as to the use of acceptable terminology. Including terms such as “physical activity”, “exercise”, “African American women”, “Black women” in the title of the PA program will help convey salience of the intervention to the target group of AA women. When selecting images of AA women to include in intervention materials, researchers should consider images that reflect the diverse body shapes, skin tones, and hair styles of AA women [13, 67]. Likewise, we caution against the use of fitness models or overly photo shopped/edited images, as AA women prefer images that are relatable and look similar to themselves [13].
Evidential Data
The use of evidential data refers to use of relevant data and statistics to highlight the importance of engaging in PA among AA women [62]. Including such information increases awareness and salience of PA engagement among study participants [62]. In our research studies, we have found it beneficial to highlight the low prevalence of AA women who meet the 2008 National PA Guidelines (i.e., 34%; [68].), followed by statements emphasizing the myriad health conditions associated with low PA levels among AA women, including overweight/obesity, breast and colon cancers, cardiovascular disease, and type II diabetes. Example evidential statements include: “Only 34% of African American women achieve the national recommendations of 150 minutes of moderate-intensity PA each week”, “Four out of five African American women are either overweight or obese and over half [53%] are obese”, and “Forty-nine percent of African American women have cardiovascular disease”. When presenting evidential data, it is important to present the information as simple as possible, as some study participants may have low literacy and/or numeracy levels.
Staff Characteristics
The physical, social, and interpersonal characteristics of study staff also play a key role in the success of a PA program. Study staff act as the “face” of a PA program and are tasked with interacting with participants on a regular basis. Therefore, it is essential that staff are perceived as relatable, likeable, attentive, and respectful by study participants [69]. Previous research suggests that engaging key opinion leaders, community stakeholders, and/or community coalitions in recruitment and delivery of an intervention are advantageous strategies to enhance participant recruitment and engagement [63, 70]. Matching study staff to the demographic characteristics of a target population can also be enhance participant engagement [71, 72], as AA women enjoy to socialize and receive health information from women they perceive as similar or “like” themselves [13, 73, 74]. For example, if the goal a program is to promote PA among older low-income AA women, hiring older low-income women AA women to recruit and deliver the PA program is advised. We also note that matching staff characteristics to characteristics of the target study population may not always be necessary (as we have conducted several reasonably successful studies where staff were not matched to the target population of AA women [15, 16]). If staff are not matched to the demographic characteristics of the study population, the interpersonal characteristics and cultural competence of staff become increasingly important. However, these aspects are important regardless of matching.
Second Level Considerations
Second level cultural considerations represent an intermediate level of cultural relevance. Considerations at this level are sociocultural norms that influence PA engagement among AA women; however, these are not as deeply embedded into AA culture as aspects proposed in the third level of our framework. To provide some perspective, these considerations reside somewhere between the “surface structure” and “deep structure” characteristics of culture proposed by Resnicow and colleagues [12]. We propose two primary considerations at this level: a) physical appearance norms of AA women, and b) religious ties.
Physical Appearance Norms
Prevalent physical appearance norms and preferences can influence the PA patterns of AA women. Here, we discuss two prominent physical appearance norms that may impact PA engagement among AA women: 1) hair style preferences, and 2) body size preferences.
Although natural hairstyles are gaining in popularity among AA women, many prefer hairstyles that are straightened or chemically relaxed due to the ease of care and prevailing style. Furthermore, many AA women spend substantial money and time to maintain their straightened hair styles [75]. As a result, AA women report not engaging in PA because they do not want to “sweat out” or “mess up” their hair style [13, 43, 36, 48, 75–77]. To address hair-related concerns associated with PA, researchers should design intervention messages that acknowledge the importance of hair styles among AA women, while encouraging them to find a hairstyle that is both aesthetically pleasing and conducive to PA engagement. Likewise, providing strategies on how to style AA hair while performing PA that limits the negative effects of sweating such as wrap hair in a cotton scarf, wear a ponytail, or wear a protective style (e.g. braids) will likely resonate with this population.
In reference to body size preferences, many AA women have a preference for a fuller, more curvaceous body shape [12, 60, 78–81]. This preference may serve as a barrier to PA because some AA women believe that engaging in PA will alter their preferred body shape [36, 47, 46, 48]. Intervention design strategies to overcome this barrier are similar to those that can be used to address hair care barriers. Careful consideration should be given to the design of intervention messages so that they acknowledge the preference for a larger body shape, while empowering AA women to become more physically active, even if it is at the cost of slightly altering their body shape. Strategies may include emphasizing that performing the national PA guidelines will not significantly alter one’s body shape unless dietary changes are also made [82, 83] and/or focusing intervention materials on the health benefits of PA independent of weight loss (e.g., decreased risk for chronic disease, improved quality of life, increased energy) [10].
Religious Ties
Religiosity and spirituality have a long history in AA culture. National data show that 94% of AAs are “absolutely” (83%) or “fairly” (11%) certain they believe in God and 75% rate religion as “very important” in their lives (compared to 50% of Whites, 59% of Latinos, and 36% of Asians) [84]. Given the importance of religion among many AA women, incorporating aspects of religion into PA promotion programs can be advantageous because it allows researchers to acknowledge the deeply-rooted religious beliefs and social networks of AA women and leverage them to promote PA [85]. A breadth of intervention research has incorporated aspects of religion into PA programs for AA women, with the majority reporting favorable PA outcomes [86]. PA programs that incorporate aspects of religion into intervention design can be generally classified as either faith-based or faith-placed. Faith-based programs are those that incorporate key features of religion, such as scripture and/or biblical stories, into PA promotion efforts. These types of programs are advantageous because they leverage already established belief systems of AA women and use these beliefs to promote positive health behaviors. Faith-placed programs, on the other hand, are interventions delivered via a religious institution (e.g., at a church), but do not necessarily incorporate religious beliefs, biblical stories, or scripture into intervention messages. Despite not incorporating religious beliefs or practices into intervention messages, faith-placed programs have the opportunity to harness the kinship and social ties, organizational structures, and collectivistic viewpoints of religious organizations by intervening within an established religious organization. We refer readers to a recent review conducted by Bopp and colleagues [86] for a more comprehensive overview of faith-based and faith-placed PA interventions, as a more in-depth discussion of this topic is beyond the scope of the current article. We also note that researchers can incorporate aspects of religion in to a PA program without being strictly classified as either a faith-based or faith-placed program. For example, including short, inspirational biblical verses judiciously throughout PA promotion programs provides a viable option for researchers to leverage aspects of religion without having to fully commit to either a faith-placed or faith-based intervention design. However, we note that incorporating religion into a PA program held outside of faith-based organization should be done with caution and only when formative research with the target population indicates this as both desired and acceptable; as incorporating religion into PA programs may alienate or even possibly offend women who do not associate with a religion.
Third Level Cultural Considerations
Third level cultural considerations are the deeply-rooted cultural, social, psychological, and historical factors that influence PA among AA women. Characteristics identified at this level coincide with the “deep structure” characteristics of culture as described by Resnicow and colleagues [12]. Addressing this level of culture is likely the most difficult part of developing PA programs for AA women because it requires researchers to have a deep understanding of AA culture. We propose four cultural considerations for PA programs targeting AA women at this level: 1) collectivism/ethic of care, 2) virtue of self-sacrifice, 3) experiential knowledge, and 4) kinship and social relationships.
Collectivism/Ethic of Care
AA women have a longstanding tradition of placing the needs of others, particularly the needs of their family and other kinship-type relationships, before the needs of themselves. This phenomenon has been termed as an “ethic of care” by previous researchers [87, 88]. While this phenomenon has been reported by women of all cultural and ethnic backgrounds, it appears to be more accentuated in the value system of AA women [25, 60]. Qualitative and quantitative research shows that AA women not only take great pride in, but are responsible for the majority of the household and caretaking responsibilities within their familial unit [36, 41, 43, 45, 46, 47, 48, 59, 75, 89, 90–94]. This involves meal preparation, household cleaning, laundry chores, child care, husband-care, and elder care. Moreover, an AA women’s “ethic of care” often extends beyond the immediate familial unit to include other kinship and community ties (i.e., extend family members, church members, friends, and neighbors, etc.). As a result of these extensive caretaking, household, community responsibilities, many AA women report they lack time [44, 45, 50, 59, 75, 90, 94–97] and energy [41, 46, 51, 75, 91, 90, 96] to engage in PA.
To integrate “ethic of care” in PA intervention design, researchers must recognize that an AA woman’s “ethic of care” is an integral component of her essence or inner being, and develop interventions that leverage this “ethic of care” and use it as a catalyst for PA engagement. Intervention messages that help AA women understand that their health is pertinent to their role as a caregiver is an ideal strategy to help accomplish this task [98]. For example, messages can emphasize that time spent performing PA is not time “taken away” from one’s familial and caretaking responsibilities, rather it is an investment in their own physical and mental health, as well as the health and well-being of her family. Underscoring that physically active AA women have more energy to perform their daily activities, are less likely to develop chronic disease, and are able to perform their caretaking responsibilities more efficiently throughout the lifespan will likely resonate with this population. Researchers can also highlight that is the responsibility of AA women to model, pass-on, and instill positive health behaviors (including PA) to her family and community members. Other intervention strategies to address AA women’s “ethic of care” may include incorporating family-based PA intervention components into a program that allow AA women to engage in PA with their families and demonstrating how AA women can incorporate PA into their daily caretaking and work-related activities (i.e., walking to the grocery store or post office instead of driving, walking their children to school/bus stop, exercising while their children play in the park as opposed to sitting and watching).
Virtue of Self-Sacrifice
Researchers suggest that many AA women feel they are not “worthy” or entitled to engage in leisure-time PA. Similar to the aforementioned “ethic of care” consideration, self-sacrifice has been reflected in the literature across women of all races and ethnic backgrounds [36, 43, 48, 99–101], but appears to be emphasized more in the AA community [43, 88]. Qualitative studies, albeit they are few in number and have focused mostly on AA of lower socioeconomic status, have reported that some AA women view PA as a “selfish” or “self-indulgent” behavior and believe that the time spent being engaging in PA is valuable time they could be spending with their family and friends [36, 48]. Similarly, AA women who have children have reported a feeling of “guilt” for asking others to watch their children in order for them to engage in PA [46].
Designing programs to address this lack of empowerment for PA will require researchers to develop interventions that instill a sense of “worth” and entitlement for PA. This can be achieved through tailoring intervention messages to portray AA women as “deserving” for self-care activities. Fostering a dialogue of self-worth and empowerment among study participants can support this goal. Researchers should also consider enlisting key opinion leaders within the AA community (i.e., local politicians, celebrities, clergy members) to deliver motivational and inspirational messages, as a breadth of research suggests that a key reason why AA women fail to perform PA is because they lack physically active AA women as role models [43, 46, 48–52].
Experiential Knowledge
Many AA women view lived experiences as a distinguishing feature between knowledge and wisdom [24]. This phenomenon has been referred to as “experiential knowledge” [24]. From this perspective, AA women perceive individuals who have personally experienced and lived the phenomena in which they appear to be experts as more trustworthy and credible than those who have only read or studied the topic [23, 102, 103]. This provides key implications for researchers to consider when designing PA programs for AA women. When selecting individuals to deliver PA promotion programs, researchers should select AA women who have successfully increased their PA. Including testimonials from AA women that illustrate their struggles and successes with PA can also help build credibility for the PA promotion program [13]. In reference to intervention activities, researchers should provide opportunities and encourage participants to engage in a variety of different physical activities. This will allow AA women to identify physical activities they enjoy performing, which can ultimately lead to enhanced motivation for PA engagement. Group-based exercise sessions (i.e., walking, Zumba®, cycling) represent an ideal strategy for researchers to accomplish this. Group-based exercise sessions also provide the opportunity for AA women to engage in PA with women who they perceive as similar or “like” themselves (which is an established motivator for PA among AA women; [40, 58, 104, 105]), while enhancing social support, self-efficacy, and self-regulatory skills for PA. For women who are unable to attend group-based sessions due to family, work, and/or community commitments, home-based exercise videos and/or demonstration manuals represent an ideal option, as they can provide women with experience of performing a variety of activities while allowing for flexibility of participant schedules.
Kinship and Social Relationships
Kinship, or close social relationships, have an established history for influencing the health behaviors of AA women. From a sociological perspective, scholars have suggested that the significance of kinship-like relationships among AAs materialized as a resilient and collective adaptation from the harsh political, social, and physical environments AAs have had to endure [106–108]. Kinship relationships of AA women often extend beyond the traditional familial unit (i.e., mother/father, children, grandparents, etc.) to include non-relatives who are considered family even though they may not be biologically related or related by marriage [109, 110]. The organizational structure of many AA religious institutions further support and replicate kinship-like relationships with the metaphoric use of kinship terms among members of the congregation (i.e., the term “father” is frequently used to refer to pastor or church leader, “brother” and “sister” are used to refer to members of the congregation) [17]. Given the emphasis on kinship and social relationships among many AAs, it is not surprising social support has emerged as a key determinant of PA engagement among AA women [36, 40, 48, 75, 89, 90, 92, 94, 91, 111].
Various intervention strategies can be used to leverage the kinship-like relationships of AA women to enhance social support for PA. One strategy is to foster a social support network among participants that enroll in a PA program. This can be achieved in a group-based intervention setting by allowing participants to informally interact with each other during intervention sessions, engage in structured PA together, and by group discussions. For PA programs delivered using technology-based platforms (i.e., websites, social networks, Smartphone applications), technology-mediated discussion forums that allow for participants to engage in group PA-related discussions is ideal. Another strategy to promote social support for PA is to leverage pre-existing social and kinships of AA women that enroll in a PA program. Strategies to accomplish this can include: a) developing family-based PA interventions where entire families receive intervention messages designed to promote PA, b) enrolling dyads of AA women into a PA program or allowing participants to identify a “buddy” or companion to also receive the PA intervention, or c) delivering PA interventions within pre-established communities or organizations (i.e., churches, community centers).
Intervention Delivery Considerations
The communication channel used to deliver a PA intervention to AA women should be congruent with the age, preferences, and social patterns of the target population. When selecting a method to deliver a PA program, researchers should rely on formative research with their target population, as well as the lessons learned and research findings from interventions targeting similar populations. For example, researchers conducting PA programs targeting middle-aged and older AA women have traditionally used face-to-face (i.e., one-on-one counseling and group-based programs), telephone, or mailed print-based intervention delivery strategies [8, 11]. Scholars conducting these studies cite using these approaches because they were identified as the preferred method of intervention delivery by their target populations and/or because previous studies using similar approaches have reported favorable PA outcomes [75, 112–114]. Similarly, in some of our previous research with college-aged and young adult AA women (i.e., women between the ages of 19 and 49) [14–16], we have used a variety of technology-based mediums (i.e., websites, social media, text messaging) to deliver culturally-relevant PA programs. These delivery channels were selected because the target populations identified these channels as their preferred method to receive a PA program, national data suggesting that AA women use these technologies at high levels [115–118], and the breadth of research suggesting that technology-delivered PA programs are efficacious strategies to promote PA among predominately White populations [119–123]. We also emphasize that the delivery channel of a PA program should not be considered the intervention itself; rather it should be viewed as a sub-component of a much larger intervention. We believe that delivery of a culturally relevant PA program for AA women should be able to be modified in order to meet the preferences and needs of the population, without compromising the cultural and theoretical underpinnings of a program.
Additional Considerations: The Physical Environment, Literacy, Issues of Race and Power, and Use of Behavioral Theory
There are a variety of other aspects researchers should consider when designing culturally relevant PA programs for AA women. While in-depth discussion of many of these considerations supersedes the scope of the current article, it would be remiss if they were not briefly acknowledged. The environmental context in which the target population resides cannot be minimized. Physical environment characteristics, including safety concerns, weather characteristics, and the presence or absence of sidewalks, parks, and community centers, will all influence the frequency and mode of PA performed [26]. For example, women who reside in areas of high crime or in geographic regions with extreme weather conditions (i.e., extreme heat or cold, snow, etc.) will not likely be receptive to outdoor modes of PA. Therefore, PA programs targeting these women should encourage activities that can be performed indoors (i.e., home-based exercise videos, treadmill or mall walking, and group-based exercise classes). Extensive attention should also be paid to the literacy levels of the target population. Given most US adults read below the 10th grade level [124], materials should be written at the lowest grade level feasibly possible (ex., 5th grade level), which has been found to even be acceptable for those of high literacy [125]. Moreover, accompanying print-based materials with oral presentations and/or audio-visual illustrations (i.e., videos, podcast) can help overcome issues associated with low literacy.
Power imbalances between researchers and study participants and issues of scientific mistrust should also be considered. A power differential will almost always exist between researchers and study participants (i.e., researchers will be perceived as having superiority, authority, or undue influence on study participants). However, this issue appears to be exacerbated when study participants are members of a racial/ethnic minority [126, 127] and when there is a gender mismatch between the research team and participants (i.e., when intervention staff is male and participants are female). Power imbalances will persist, although perhaps to a lesser extent, even if the research team is comprised of AA women [7]. Such imbalances can result in moral and methodological issues, including coerced participation, social desirability bias, and resentment towards the research team/staff. Distrust of the scientific community may also be a concern. Many AA women are hesitant to participate in research studies due to historical discrimination and mistreatment of AAs in research (i.e., Tuskegee Syphilis Study) [128–130]. This can result in recruitment challenges and difficulty obtaining outcome measures that require blood draws or other medical procedures. To help minimize issues associated with power imbalances and scientific mistrust, researchers should develop a research team that includes members of diverse racial and socioeconomic backgrounds (including AA women) [130, 131] and provide detailed information regarding the study purpose, value of the research, and utility of all study procedures [126]. The inclusion of an advisory board with stakeholders important to AA women such as social and health organizations is a critical element of research engagement with AA women and a community-based participatory research approach may help address issues of trust.
Last, researchers should leverage behavioral health theory when designing PA programs for AA women. Given the breadth of research suggesting that theoretically-based behavior interventions are more effective than those that are atheoretical [120, 132–134], the importance of grounding PA interventions in behavioral theory should not be overlooked. When selecting theories and/or constructs to underpin PA promotion efforts, relevance of the theoretical frameworks to AA women should be considered. For example, constructs of social support, self-regulation, and self-efficacy from Bandura’s Social Cognitive theory [135, 136] are evidence-based constructs to promote PA [137–139] and are ideal when designing intervention activities to address cultural considerations of collectivism/ethic of care, experiential knowledge, and kinship. Similarly, First Level cultural considerations focused on the visual appeal/packaging of the program and evidential data can be addressed by leveraging constructs of outcome expectations and behavioral capability. Researchers should rely on their formative research with their target population and evidence-based theoretical backgrounds when deciding on an appropriate theory to underpin their PA promotion efforts.
DISCUSSION
This report provides a framework to guide the development of culturally-relevant PA programs for AA women. Aspects discussed coincide with other models and perspectives designed to promote health-enhancing behaviors and outcomes among minority women. For example, the Community Energy Balance Framework (CEB) proposed by Kumanyika and colleges [7] emphasizes the importance of understanding the historical and social context and cultural and psychosocial processes of AAs in order to successfully promote energy balance and reduce the disparate obesity prevalence among AA women. Similarly, a recently published model by Keller and colleagues [140] acknowledges the role that culture and traditions play in the PA behaviors of Hispanic women. Our framework complements and extends these previous works in several ways. First, our model focuses exclusively on the PA behaviors of AA women. This narrow focus allowed us to expand-on specific issues associated with PA engagement among AA women not previously included in other PA promotion models. Second, our framework specifies explicit sociocultural phenomena, beliefs, and behaviors that can influence the PA behaviors of AA women and we provide real-world examples to illustrate how researchers can leverage these aspects to increase PA. In comparison, the CEB, while comprehensive in nature, provides a more global perspective on the behavioral, cultural, environmental, and policy determinants associated with obesity/energy balance and does not include detailed examples of how researchers can engage AA women through sensitivity to their unique sociocultural values to leverage PA interventions. Lastly, our framework underscores the importance of using a life course perspective when designing PA promotion programs for AA women. Keller and colleagues [140] used a life course perspective when developing their PA promotion framework for Hispanic women; however, this perspective was only peripherally mentioned in the CEB framework. Women will face different barriers and challenges to PA as they progress through lifespan. Life events of younger women, including childbirth, children living in the household, and managing work and family-life responsibilities will all play a role in a woman’s availability, desire, and preference for PA. Similarly, older women will face different barriers to PA as they age, experience menopause, and transition into retirement. Tailoring interventions to address the intersectionality of these developmental milestones along with the role of women in AA culture is necessary to develop effective PA programs for AA women [88, 141, 142].
A comprehensive approach was used in designing our framework. However, we acknowledge some aspects presented in this article may not be relevant or applicable to all AA women. The term “AA women” refers to a broad group of people with African ancestry, which can be quite diverse according to the geographical region one’s ancestors originated and the duration in which AA women and their families have lived in the U.S. [7]. Likewise, AA women residing in one geographical region of the U.S. may have different sociocultural norms than those in another region. Local adaption of culturally-relevant PA interventions for AA women may also be necessary [64]. Researchers should look to their formative research with their target population, as well as well-designed, successful PA programs (i.e., programs that resulted in increased PA) conducted by other researchers to determine the most relevant considerations to address through their PA promotion efforts.
Designing culturally relevant PA promotion programs for AA women is not a simple task. Creating such programs requires researchers to have a deep understanding of the historical, cultural, and social phenomena associated with PA engagement, and the ability to leverage these phenomena to promote PA within this group. While this task may be difficult, we believe that attending to these aspects is imperative for the successful promotion of sustained high PA levels among AA women. This is critical, as sustained high PA levels are compulsory for chronic disease prevention and reducing the myriad PA-related health disparities among AA women (i.e., obesity, cardiovascular disease, type II diabetes, and colon and breast cancers). This article provides a comprehensive overview of many of the factors associated with PA engagement among AA women and presents a framework for the development of culturally relevant PA programs for this high-risk and understudied population.
Acknowledgments
Preparation of this manuscript was supported by funding from the National Institutes of Health/National Heart, Lung, and Blood Institute (NIH/NHLBI), award K99 HL129012-01 (R. Joseph, P.I.) and the National Institutes of Health/National Institute on Nursing Research (NIH/NINR), award T32 1T32NR012718-01 Transdisciplinary Training in Health Disparities Science (C. Keller, P.I.). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH, NHLBI, or NINR.
Contributor Information
Rodney P. Joseph, College of Nursing and Health Innovation, Arizona State University, 500 N. 3rd Street, Phoenix, AZ 85004, Phone: 602-496-0772, Fax: 602-496-0448, Rodney.Joseph@asu.edu.
Colleen Keller, College of Nursing and Health Innovation, Arizona State University, 500 N. 3rd Street, Phoenix, AZ 85004, Colleen.Keller@asu.edu.
Oliva Affuso, Department of Epidemiology, School of Public Health, University of Alabama at Birmingham, 1720 2nd Ave South, Birmingham, AL 35294-0022, oaffuso@uab.edu.
Barbara E. Ainsworth, School of Nutrition and Health Promotion, College of Health Solutions, Arizona State University, 550 N. 3rd Street, Phoenix, AZ 85004, Barbara.Ainsworth@asu.edu.
REFERENCES
- 1.Centers for Disease Control and Prevention. National Center for Health Statistics, Health Data Interactive. [Accessed August 1 2015];2015 www.cdc.gov/nchs/hdi.htm.
- 2.Ogden CL, Carroll MD, Flegal KM. Prevalence of obesity in the United States. JAMA. 2014;2:189–190. doi: 10.1001/jama.2014.6228. [DOI] [PubMed] [Google Scholar]
- 3.Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Borden WB, et al. Heart disease and stroke statistics—2013 update: a report from the American Heart Association. Circulation. 2013;127:e6–e245. doi: 10.1161/CIR.0b013e31828124ad. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention. Age-Adjusted Rates of Diagnosed Diabetes per 100 Civilian, Non-institutionalized Population, by Race and Sex, United States, 1980–2014. [Accessed 10 Dec 2015]; http://www.cdc.gov/diabetes/statistics/prev/national/figraceethsex.htm.
- 5.Knowler WC, Fowler SE, Hamman RF, Christophi CA, Hoffman HJ, Brenneman AT, et al. 10-year follow-up of diabetes incidence and weight loss in the Diabetes Prevention Program Outcomes Study. Lancet. 2009;374(9702):1677–1686. doi: 10.1016/S0140-6736(09)61457-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lee IM, Shiroma EJ, Lobelo F, Puska P, Blair SN, Katzmarzyk PT. Effect of physical inactivity on major non-communicable diseases worldwide: an analysis of burden of disease and life expectancy. Lancet. 2012;380(9838):219–229. doi: 10.1016/S0140-6736(12)61031-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kumanyika SK, Whitt-Glover MC, Gary TL, Prewitt TE, Odoms-Young AM, Banks-Wallace J, et al. Expanding the obesity research paradigm to reach African American communities. Prev Chronic Dis. vol 4. United States. 2007:A112. [PMC free article] [PubMed] [Google Scholar]
- 8.Whitt-Glover MC, Keith NR, Ceaser TG, Virgil K, Ledford L, Hasson RE. A systematic review of physical activity interventions among African American adults: evidence from 2009 to 2013. Obes Rev. 2014;15(Suppl 4):125–145. doi: 10.1111/obr.12205. [DOI] [PubMed] [Google Scholar]
- 9.Pekmezi D, Jennings E. Interventions to Promote Physical Activity Among African Americans. American Journal of Lifestyle Medicine. 2009;3:173–184. [Google Scholar]
- 10.Banks-Wallace J, Conn V. Interventions to promote physical activity among African American women. Public Health Nurs. 2002;19(5):321–335. doi: 10.1046/j.1525-1446.2002.19502.x. [DOI] [PubMed] [Google Scholar]
- 11.Whitt-Glover MC, Kumanyika SK. Systematic review of interventions to increase physical activity and physical fitness in African-Americans. Am J Health Promot. 2009;23(6):S33–S56. doi: 10.4278/ajhp.070924101. [DOI] [PubMed] [Google Scholar]
- 12.Resnicow K, Baranowski T, Ahluwalia JS, Braithwaite RL. Cultural sensitivity in public health: defined and demystified. Ethn Dis. 1999;9(1):10–21. [PubMed] [Google Scholar]
- 13.Durant N, Joseph R, Cherrington A, Cuffee Y, Knight B, Lewis D, et al. Recommendations for a Culturally Relevant Internet-Based Tool to Promote Physical Activity Among Overweight Young African American Women, Alabama, 2010–2011. Preventing Chronic Disease. 2014;11(130169) doi: 10.5888/pcd11.130169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Joseph RP, Pekmezi DW, Lewis T, Dutton G, Turner LW, Durant NH. Physical activity and Social Cognitive Theory outcomes of an Internet-enhanced physical activity intervention for African American female college students. Journal of Health Disparities Research and Practice. 2013;6(2):18. [PMC free article] [PubMed] [Google Scholar]
- 15.Joseph RP, Pekmezi D, Dutton GR, Cherrington AL, Kim YI, Allison JJ, et al. Results of a Culturally Adapted Internet-Enhanced Physical Activity Pilot Intervention for Overweight and Obese Young Adult African American Women. J Transcult Nurs. 2016;27(2):136–146. doi: 10.1177/1043659614539176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Joseph RP, Keller C, Adams MA, Ainsworth BE. Print versus a Culturally-Relevant Facebook and Text Message Delivered Intervention to Promote Physical Activity in African American Women: A Randomized Pilot Trial. BMC Women's Health. 2015;15:30. doi: 10.1186/s12905-015-0186-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Coe K, Keller C, Walker JR. Religion, kinship and health behaviors of african american women. Journal of religion and health. 2015;54(1):46–60. doi: 10.1007/s10943-013-9784-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Keller CS, Robinson B, Pickens L. Comparison of two walking frequencies in African American postmenopausal women. ABNF J. 2004;15(1):3–9. [PubMed] [Google Scholar]
- 19.Walker J, Ainsworth B, Hooker S, Keller C, Fleury J, Chisum J, et al. Optimal Health (Spirit, Mind, and Body): A Feasibility Study Promoting Well-Being for Health Behavior Change. Journal of religion and health. 2014 doi: 10.1007/s10943-014-9890-7. [DOI] [PubMed] [Google Scholar]
- 20.Affuso O, Cox TL, Durant NH, Allison DB. Attitudes and beliefs associated with leisure-time physical activity among African American adults. Ethn Dis. 2011;21(1):63–67. [PMC free article] [PubMed] [Google Scholar]
- 21.Hawkins RP, Kreuter M, Resnicow K, Fishbein M, Dijkstra A. Understanding tailoring in communicating about health. Health Educ Res. 2008;23(3):454–466. doi: 10.1093/her/cyn004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Castro FG, Barrera M, Jr, Martinez CR., Jr The cultural adaptation of prevention interventions: resolving tensions between fidelity and fit. Prevention science : the official journal of the Society for Prevention Research. 2004;5(1):41–45. doi: 10.1023/b:prev.0000013980.12412.cd. [DOI] [PubMed] [Google Scholar]
- 23.Taylor JY. Womanism: a methodologic framework for African American women. ANS Advances in nursing science. 1998;21(1):53–64. doi: 10.1097/00012272-199809000-00006. [DOI] [PubMed] [Google Scholar]
- 24.Banks-Wallace J. Womanist ways of knowing: theoretical considerations for research with African American women. Advances in Nursing Science. 2000;22(3):33–45. doi: 10.1097/00012272-200003000-00004. [DOI] [PubMed] [Google Scholar]
- 25.Jones LV, Hopson LM, Gomes A-M. Intervening with African-Americans: Culturally Specific Practice Considerations. Journal of Ethnic And Cultural Diversity in Social Work. 2012;21(1):37–54. [Google Scholar]
- 26.Joseph RP, Ainsworth BE, Keller C, Dodgson JE. Barriers to physical activity among African American women: An integrative review of the literature. Women & Health. 2015 doi: 10.1080/03630242.2015.1039184. Online First. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fleury J, Lee SM. The social ecological model and physical activity in African American women. Am J Community Psychol. 2006;37(1–2):129–40. doi: 10.1007/s10464-005-9002-7. [DOI] [PubMed] [Google Scholar]
- 28.Elder GH., Jr Time, Human Agency, and Social Change: Perspectives on the Life Course. Social Psychology Quarterly. 1994;57(1):4–15. [Google Scholar]
- 29.Giele JZ, Edler GH. Life Course Research: Development of a Field. In: Giele JZ, Edler GH, editors. Methods of Life Course Research. Thousand Oaks, California: Sage Publications; 1998. p. 22. [Google Scholar]
- 30.Giele JZ, Edler GH. Life Course Research: Development of a Field. In: Giele JZ, Edler GH, editors. Methods of Life Course Research. Thousand Oaks, California: Sage Publications; 1998. p. iv. [Google Scholar]
- 31.Flinn MV. Culture and the evolution of social learning. Evolution and Human Behavior. 1997;18(1):23–67. doi: http://dx.doi.org/10.1016/S1090-5138(96)00046-3. [Google Scholar]
- 32.United States Department of Labor. Household Data: Annual Averages: Employment Status of the Civilian Noninstitutional population by Age, Sex, and Race. [Accessed 2 Feb 2016]; http://www.bls.gov/cps/cpsaat03.pdf.
- 33.United States Census Bureau. Families and Living Arrangements: 2014: Family Households (F table series) [Accessed 22 Jan 2016];Table F1. Family Households BT, Age Of Own Children, Age Of Family Members, And Age, Race And Hispanic Origin Of Householder: 2014, ed. Available at http://www.census.gov/hhes/families/data/cps2014F.html.
- 34.Fan JX, Kowaleski-Jones L, Wen M. Walking or dancing: patterns of physical activity by cross-sectional age among U.S. women. J Aging Health. 2013;17:1182–1203. doi: 10.1177/0898264313495561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Versey HS. Centering perspectives on Black women, hair politics, and physical activity. American journal of public health. 2014;104(5):810–815. doi: 10.2105/AJPH.2013.301675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Im EO, Ko Y, Hwang H, et al. "Physical activity as a luxury": African American women's attitudes toward physical activity. West J Nurs Res. 2012;34(3):317–339. doi: 10.1177/0193945911400637. [DOI] [PubMed] [Google Scholar]
- 37.Lukwago SN. Measurement and health-related correlates of collectivism, spirituality, racial pride and time orientation in urban Black women. Ann Arbor: Saint Louis University. 2001 [Google Scholar]
- 38.Harley AE, Rice J, Walker R, Strath SJ, Quintiliani LM, Bennett GG. Physically active, low-income African American women: an exploration of activity maintenance in the context of sociodemographic factors associated with inactivity. Women Health. 2014;54(4):354–372. doi: 10.1080/03630242.2014.896440. [DOI] [PubMed] [Google Scholar]
- 39.Bowen PG, Eaves YD, Vance DE, Moneyham LD. A phenomenological study of obesity and physical activity in southern african american older women. J Aging Phys Act. 2015;2:221–229. doi: 10.1123/japa.2013-0039. [DOI] [PubMed] [Google Scholar]
- 40.Wilcox S, Oberrecht L, Bopp M, Kammermann SK, McElmurray CT. A qualitative study of exercise in older African American and white women in rural South Carolina: perceptions, barriers, and motivations. J Women Aging. 2005;17(1–2):37–53. doi: 10.1300/J074v17n01_04. [DOI] [PubMed] [Google Scholar]
- 41.Zunker C, Cox TL, Wingo BC, Knight B, Jefferson WK, Ard JD. Using formative research to develop a worksite health promotion program for African American women. Women Health. 2008;48(2):189–207. doi: 10.1080/03630240802313514. [DOI] [PubMed] [Google Scholar]
- 42.Keller C, Larkey L, Distefano JK, Boehm-Smith E, Records K, Robillard A, et al. Perimenopausal obesity. J Womens Health (Larchmt) 2010;19(5):987–996. doi: 10.1089/jwh.2009.1547. [DOI] [PubMed] [Google Scholar]
- 43.Henderson KA, Ainsworth BE. Sociocultural perspectives on physical activity in the lives of older African American and American Indian women: a cross cultural activity participation study. Women Health. 2000;31(1):1–20. doi: 10.1300/J013v31n01_01. [DOI] [PubMed] [Google Scholar]
- 44.Walcott-McQuigg JA, Prohaska TR. Factors influencing participation of African American elders in exercise behavior. Public Health Nurs. 2001;18(3):194–203. doi: 10.1046/j.1525-1446.2001.00194.x. [DOI] [PubMed] [Google Scholar]
- 45.Dunn MZ. Psychosocial mediators of a walking intervention among African American women. J Transcult Nurs. 2008;19(1):40–46. doi: 10.1177/1043659607309138. [DOI] [PubMed] [Google Scholar]
- 46.Sanderson B, Littleton M, Pulley L. Environmental, policy, and cultural factors related to physical activity among rural, African American women. Women Health. 2002;36(2):75–90. doi: 10.1300/j013v36n02_06. [DOI] [PubMed] [Google Scholar]
- 47.Young DR, He X, Harris J, Mabry I. Environmental, policy, and cultural factors related to physical activity in well-educated urban African American women. Women Health. 2002;36(2):29–41. doi: 10.1300/J013v36n02_03. [DOI] [PubMed] [Google Scholar]
- 48.Harley AE, Odoms-Young A, Beard B, Katz ML, Heaney CA. African American social and cultural contexts and physical activity: strategies for navigating challenges to participation. Women Health. 2009;49(1):84–100. doi: 10.1080/03630240802690861. [DOI] [PubMed] [Google Scholar]
- 49.Wilbur J, Chandler P, Dancy B, Choi J, Plonczynski D. Environmental, policy, and cultural factors related to physical activity in urban, African American women. Women Health. 2002;36(2):17–28. doi: 10.1300/J013v36n02_02. [DOI] [PubMed] [Google Scholar]
- 50.Ingram D, Wilbur J, McDevitt J, Buchholz S. Women's walking program for African American women: expectations and recommendations from participants as experts. Women Health. 2011;51(6):566–582. doi: 10.1080/03630242.2011.606357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Richter DL, Wilcox S, Greaney ML, Henderson KA, Ainsworth BE. Environmental, policy, and cultural factors related to physical activity in African American women. Women Health. 2002;36(2):91–109. doi: 10.1300/j013v36n02_07. [DOI] [PubMed] [Google Scholar]
- 52.Doldren MA, Webb FJ. Facilitators of and barriers to healthy eating and physical activity for Black women: a focus group study in Florida, USA. Critical Public Health. 2013;23(1):32–38. [Google Scholar]
- 53.Paxton RJ, Nayak P, Taylor WC, Chang S, Courneya KS, Schover L, et al. African-American breast cancer survivors' preferences for various types of physical activity interventions: a Sisters Network Inc. web-based survey. Journal of cancer survivorship : research and practice. 2014;8(1):31–38. doi: 10.1007/s11764-013-0307-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Wanko NS, Brazier CW, Young-Rogers D, Dunbar VG, Boyd B, George CD, et al. Exercise preferences and barriers in urban African Americans with type 2 diabetes. Diabetes Educ. 2004;30(3):502–513. doi: 10.1177/014572170403000322. [DOI] [PubMed] [Google Scholar]
- 55.Nies MA, Troutman-Jordan M, Branche D, Moore-Harrison T, Hohensee C. Physical activity preferences for low-income sedentary urban African American older adults. J Gerontol Nurs. 2013;39(6):20–29. doi: 10.3928/00989134-20130408-01. quiz 30-1. [DOI] [PubMed] [Google Scholar]
- 56.Daley A, Stokes-Lampard H, Wilson S, Rees M, Roalfe A, Macarthur C. What women want? Exercise preferences of menopausal women. Maturitas. 2011;68(2):174–178. doi: 10.1016/j.maturitas.2010.11.011. [DOI] [PubMed] [Google Scholar]
- 57.Rossi A, Moadel-Robblee A, Garber CE, Kuo D, Goldberg G, Einstein M, et al. Physical activity for an ethnically diverse sample of endometrial cancer survivors: a needs assessment and pilot intervention. J Gynecol Oncol. 2015;2:141–147. doi: 10.3802/jgo.2015.26.2.141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Henderson KA, Ainsworth BE. A synthesis of perceptions about physical activity among older African American and American Indian women. American journal of public health. 2003;93(2):313–317. doi: 10.2105/ajph.93.2.313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Eyler AA, Baker E, Cromer L, King AC, Brownson RC, Donatelle RJ. Physical activity and minority women: a qualitative study. Health Educ Behav. 1998;25(5):640–652. doi: 10.1177/109019819802500510. [DOI] [PubMed] [Google Scholar]
- 60.Eyler AA, Matson-Koffman D, Vest JR, Evenson KR, Sanderson B, Thompson JL, et al. Environmental, policy, and cultural factors related to physical activity in a diverse sample of women: The Women's Cardiovascular Health Network Project--summary and discussion. Women Health. 2002;36(2):123–134. [PubMed] [Google Scholar]
- 61.Kreuter MW, Lukwago SN, Bucholtz RD, Clark EM, Sanders-Thompson V. Achieving cultural appropriateness in health promotion programs: targeted and tailored approaches. Health Educ Behav. 2003;30(2):133–146. doi: 10.1177/1090198102251021. [DOI] [PubMed] [Google Scholar]
- 62.Kreuter MW, McClure SM. The role of culture in health communication. Annu Rev Public Health. 2004;25:439–455. doi: 10.1146/annurev.publhealth.25.101802.123000. [DOI] [PubMed] [Google Scholar]
- 63.Kreuter MW, Haughton LT. Integrating Culture Into Health Information for African American Women. The American Behavioral Scientist. 2006;49(6):794–811. [Google Scholar]
- 64.Castro FG, Barrera M, Jr, Holleran Steiker LK. Issues and challenges in the design of culturally adapted evidence-based interventions. Annual review of clinical psychology. 2010;6:213–239. doi: 10.1146/annurev-clinpsy-033109-132032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Resnicow K, Soler R, Braithwaite RL, Ahluwalia JS, Butler J. Cultural sensitivity in substance use prevention. Journal of Community Psychology. 2000;28(3):271–290. [Google Scholar]
- 66.Yancey AK, Ortega AN, Kumanyika SK. Effective recruitment and retention of minority research participants. Annu Rev Public Health. 2006;27:1–28. doi: 10.1146/annurev.publhealth.27.021405.102113. [DOI] [PubMed] [Google Scholar]
- 67.Joseph RP, Pekmezi D, Allison JJ, Durant NH. Lessons learned from the development and implementation two Internet-enhanced culturally relevant physical activity interventions for young overweight African American women. Journal of the National Black Nurses Association. 2014;25(1):42–47. [PMC free article] [PubMed] [Google Scholar]
- 68.Centers for Disease Control and Prevention. Health data interactive. Atlanta, GA: Centers for Disease Control and Prevention, National Center for Health Statistics; 2014. [Accessed 2 Feb 2016]. http://www.cdc.gov/nchs/hdi.htm. [Google Scholar]
- 69.Harris KJ, Ahluwalia JS, Catley D, Okuyemi KS, Mayo MS, Resnicow K. Successful recruitment of minorities into clinical trials: The Kick It at Swope project. Nicotine & Tobacco Research. 2003;5(4):575–584. doi: 10.1080/1462220031000118540. [DOI] [PubMed] [Google Scholar]
- 70.Heller C, Balls-Berry JE, Nery JD, Erwin PJ, Littleton D, Kim M, et al. Strategies addressing barriers to clinical trial enrollment of underrepresented populations: a systematic review. Contemp Clin Trials. 2014;39(2):169–182. doi: 10.1016/j.cct.2014.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Fryer CS, Passmore SR, Maietta RC, Petruzzelli J, Casper E, Brown NA, et al. The Symbolic Value and Limitations of Racial Concordance in Minority Research Engagement. Qual Health Res. 2015 doi: 10.1177/1049732315575708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Rivers D, August EM, Sehovic I, Lee Green B, Quinn GP. A systematic review of the factors influencing African Americans' participation in cancer clinical trials. Contemporary Clinical Trials. 2013;35(2):13–32. doi: 10.1016/j.cct.2013.03.007. doi: http://dx.doi.org/10.1016/j.cct.2013.03.007. [DOI] [PubMed] [Google Scholar]
- 73.Kalichman SC, Coley B. Context framing to enhance HIV-antibody-testing messages targeted to African American women. Health Psychol. 1995;14(3):247–254. doi: 10.1037//0278-6133.14.3.247. [DOI] [PubMed] [Google Scholar]
- 74.Lopes C, Sussman S, Galaif E, Crippins D. The impact of a videotape on smoking cessation among African American women. American Journal of Health Promotion. 1995;9:3. doi: 10.4278/0890-1171-9.4.257. [DOI] [PubMed] [Google Scholar]
- 75.Pekmezi D, Marcus B, Meneses K, Baskin ML, Ard JD, Martin MY, et al. Developing an intervention to address physical activity barriers for African-American women in the deep south (USA) Womens Health (Lond Engl) 2013;9(3):301–312. doi: 10.2217/whe.13.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Price AE, Greer B, Tucker A. Older black women's experiences initiating and maintaining physical activity: implications for theory and practice. J Aging Phys Act. 2013;21(3):348–366. doi: 10.1123/japa.21.3.348. [DOI] [PubMed] [Google Scholar]
- 77.Hall RR, Francis S, Whitt-Glover M, Loftin-Bell K, Swett K, McMichael AJ. Hair care practices as a barrier to physical activity in African American women. JAMA Dermatol. 2013;149(3):310–314. doi: 10.1001/jamadermatol.2013.1946. [DOI] [PubMed] [Google Scholar]
- 78.Im EO, Ko Y, Hwang H, Chee W, Stuifbergen A, Walker L, et al. Racial/Ethnic Differences in Midlife Women's Attitudes Toward Physical Activity. Journal of Midwifery & Womens Health. 2013;58(4):440–450. doi: 10.1111/j.1542-2011.2012.00259.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Overstreet N, Quinn D, Agocha VB. Beyond Thinness: The Influence of a Curvaceous Body Ideal on Body Dissatisfaction in Black and White Women. Sex Roles. 2010;63(1–2):91–103. [Google Scholar]
- 80.Greenberg DR, LaPorte DJ. Racial differences in body type preferences of men for women. International Journal of Eating Disorders. 1996;19(3):275–278. doi: 10.1002/(SICI)1098-108X(199604)19:3<275::AID-EAT6>3.0.CO;2-J. [DOI] [PubMed] [Google Scholar]
- 81.Allan JD, Mayo K, Michel Y. Body size values of white and black women. Res Nurs Health. 1993;16(5):323–333. doi: 10.1002/nur.4770160503. [DOI] [PubMed] [Google Scholar]
- 82.Jakicic JM. Physical activity and weight loss. Nestle Nutrition Institute workshop series. 2012;73:21–36. doi: 10.1159/000341283. [DOI] [PubMed] [Google Scholar]
- 83.Jakicic JM, Otto AD. Physical activity considerations for the treatment and prevention of obesity. Am J Clin Nutr. vol 1 Suppl. United States. 2005:226S–229S. doi: 10.1093/ajcn/82.1.226S. [DOI] [PubMed] [Google Scholar]
- 84.Pew Research Center. Religious Landscape Study: Racial and Ethnic Composition. Washington, DC: Pew Research Center; 2015. [Accessed April 7 2016]. http://www.pewforum.org/religious-landscape-study/racial-and-ethnic-composition/ [Google Scholar]
- 85.Quinn ME, Guion WK. A faith-based and cultural approach to promoting self-efficacy and regular exercise in older African American women. Gerontology & geriatrics education. 2010;31(1):1–18. doi: 10.1080/02701960903578311. [DOI] [PubMed] [Google Scholar]
- 86.Bopp M, Fallon E. A Comprehensive Review of Faith-Based Physical Activity Interventions. American Journal of Lifestyle Medicine. 2012;6:18. [Google Scholar]
- 87.Gilligan C. In a different voice. Cambridge, MA: Harvard University Press; 1982. [Google Scholar]
- 88.Henderson K, Allen K. The ethic of care: Leisure possibilities and constraints for women. Loisi et Societe [Society and Leisure] 1991;14:97–113. [Google Scholar]
- 89.Bopp M, Wilcox S, Oberrecht L, Kammermann S, McElmurray CT. Correlates of strength training in older rural African American and Caucasian women. Women Health. 2004;40(1):1–20. doi: 10.1300/J013v40n01_01. [DOI] [PubMed] [Google Scholar]
- 90.Bopp M, Lattimore D, Wilcox S, Laken M, McClorin L, Swinton R, et al. Understanding physical activity participation in members of an African American church: a qualitative study. Health Educ Res. 2007;22(6):815–826. doi: 10.1093/her/cyl149. [DOI] [PubMed] [Google Scholar]
- 91.Evans LK. Rural Black women's thoughts about exercise. Appl Nurs Res. 2011;24(4):200–206. doi: 10.1016/j.apnr.2009.09.005. [DOI] [PubMed] [Google Scholar]
- 92.Kirchhoff AC, Elliott L, Schlichting JA, Chin MH. Strategies for physical activity maintenance in African American women. Am J Health Behav. 2008;32(5):517–524. doi: 10.5555/ajhb.2008.32.5.517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Nies MA, Vollman M, Cook T. African American women's experiences with physical activity in their daily lives. Public Health Nurs. 1999;16(1):23–31. doi: 10.1046/j.1525-1446.1999.00023.x. [DOI] [PubMed] [Google Scholar]
- 94.Walcott-McQuigg JA, Zerwic JJ, Dan A, Kelley MA. An ecological approach to physical activity in African American women. Medscape Womens Health. 2001;6(6):3. [PubMed] [Google Scholar]
- 95.James DC, Pobee JW, Oxidine D, Brown L, Joshi G. Using the health belief model to develop culturally appropriate weight-management materials for African-American women. J Acad Nutr Diet. 2012;112(5):664–670. doi: 10.1016/j.jand.2012.02.003. [DOI] [PubMed] [Google Scholar]
- 96.Hoebeke R. Low-income women's perceived barriers to physical activity: focus group results. Appl Nurs Res. 2008;21(2):60–65. doi: 10.1016/j.apnr.2006.06.002. [DOI] [PubMed] [Google Scholar]
- 97.Mama SK, McCurdy SA, Evans AE, Thompson DI, Diamond PM, Lee RE. Using Community Insight to Understand Physical Activity Adoption in Overweight and Obese African American and Hispanic Women: A Qualitative Study. Health Educ Behav. 2014 doi: 10.1177/1090198114557128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Gans KM, Kumanyika SK, Lovell HJ, Risica PM, Goldman R, Odoms-Young A, et al. The development of SisterTalk: a cable TV-delivered weight control program for black women. Prev Med. 2003;37(6 Pt 1):654–667. doi: 10.1016/j.ypmed.2003.09.014. [pii] [DOI] [PubMed] [Google Scholar]
- 99.Wilcox S, Richter DL, Henderson KA, Greaney ML, Ainsworth BE. Perceptions of physical activity and personal barriers and enablers in African-American women. Ethn Dis. 2002;12(3):353–362. [PubMed] [Google Scholar]
- 100.Currie J. Motherhood, stress and the exercise experience: freedom or constraint? Leisure Studies. 2004;23(3):225–242. [Google Scholar]
- 101.Bialeschki MD. Reentering Leisure: Transition Within The Role Of Motherhood. Journal of Leisure Research. 1994;26:57–74. [Google Scholar]
- 102.Barbee E. A Black Feminist approach to nursing research. Western Journal of Nursing Research. 1994;16(5):11. doi: 10.1177/019394599401600504. [DOI] [PubMed] [Google Scholar]
- 103.Collins P. Black Feminist Thought: Knowledge, Consciousness, and the Politics of Empowerement. Boston, MA: Unwin Hyman; 1990. [Google Scholar]
- 104.Henderson KA, Ainsworth BE. Enablers and constraints to walking for older African American and American Indian women: the Cultural Activity Participation Study. Res Q Exerc Sport. 2000;71(4):313–321. doi: 10.1080/02701367.2000.10608914. [DOI] [PubMed] [Google Scholar]
- 105.Krans EE, Chang JC. A will without a way: barriers and facilitators to exercise during pregnancy of low-income, African American women. Women Health. 2011;51(8):777–794. doi: 10.1080/03630242.2011.633598. [DOI] [PubMed] [Google Scholar]
- 106.Scannapieco M, Jackson S. Kinship care: the African American response to family preservation. Soc Work. 1996;41(2):190–196. doi: 10.1093/sw/41.2.190. [DOI] [PubMed] [Google Scholar]
- 107.Waites C. Building on strengths: intergenerational practice with African American families. Soc Work. 2009;54(3):278–287. doi: 10.1093/sw/54.3.278. [DOI] [PubMed] [Google Scholar]
- 108.Christian CM. Black sage: The African American experience. Boston, MA: Houghton Mifflin; 1995. [Google Scholar]
- 109.Chatters LM, Taylor RJ, Jayakody R. Fictive kinship relations in black extended families. Journal of Comparative Family Studies. 1994;25:16. [Google Scholar]
- 110.Taylor RJ, Chatters LM, Woodward AT, Brown E. Racial and Ethnic Differences in Extended Family, Friendship, Fictive Kin, and Congregational Informal Support Networks. Family Relations. 2013;62(4):609–624. doi: 10.1111/fare.12030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Johnson ER, Carson TL, Affuso O, Hardy CM, Baskin ML. Relationship between social support and body mass index among overweight and obese African American women in the rural deep South, 2011–2013. Prev Chronic Dis. 2014;11:E224. doi: 10.5888/pcd11.140340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Whitt-Glover MC, Goldmon MV, Karanja N, Heil DP, Gizlice Z. Learning and Developing Individual Exercise Skills (L.A.D.I.E.S.) for a better life: a physical activity intervention for black women. Contemp Clin Trials. 2012;33(6):1159–1171. doi: 10.1016/j.cct.2012.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Migneault JP, Dedier JJ, Wright JA, Heeren T, Campbell MK, Morisky DE, et al. A culturally adapted telecommunication system to improve physical activity, diet quality, and medication adherence among hypertensive African-Americans: a randomized controlled trial. Ann Behav Med. 2012;43(1):62–73. doi: 10.1007/s12160-011-9319-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Zoellner J, Connell C, Madson MB, Thomson JL, Landry AS, Fontenot Molaison E, et al. HUB city steps: a 6-month lifestyle intervention improves blood pressure among a primarily African-American community. J Acad Nutr Diet. 2014;114(4):603–612. doi: 10.1016/j.jand.2013.11.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Smith A. Smartphone Ownership- 2013 Update. [Accessed September 13 2013];Pew Research Center. 2013 http://pewinternet.org/Reports/2013/Smartphone-Ownership-2013.aspx. [Google Scholar]
- 116.Duggan M. Cell Phone Activities 2013. [Accessed September 19 2013];Pew Research Center. 2013 http://pewinternet.org/Reports/2013/cell-activities.aspx. [Google Scholar]
- 117.Duggan M, Brenner J. Demographics of Social Media Users- 2012. [Accessed August, 2 2013];Pew Internet and American Life Project. 2013 http://pewinternet.org/Reports/2013/Social-media-users.aspx. [Google Scholar]
- 118.Lenhart A. Cell phones and American adults. [Accessed September 19 2013];Pew Research Center. 2010 http://pewinternet.org/Reports/2010/cell-phones-and-american-adults.aspx. [Google Scholar]
- 119.Joseph RP, Durant NH, Benitez TB, Pekmezi DW. Internet-based physical activity interventions. American Journal of Lifestyle Medicine. 2013 doi: 10.1177/1559827613498059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Davies CA, Spence JC, Vandelanotte C, Caperchione CM, Mummery WK. Meta-analysis of internet-delivered interventions to increase physical activity levels. Int J Behav Nutr Phys Act. 2012;9:52. doi: 10.1186/1479-5868-9-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Vandelanotte C, Spathonis KM, Eakin EG, Owen N. Website-delivered physical activity interventions a review of the literature. Am J Prev Med. 2007;1:54–64. doi: 10.1016/j.amepre.2007.02.041. [DOI] [PubMed] [Google Scholar]
- 122.Maher CA, Lewis LK, Ferrar K, Marshall S, De Bourdeaudhuij I, Vandelanotte C. Are health behavior change interventions that use online social networks effective? A systematic review. J Med Internet Res. 2014;16(2):e40. doi: 10.2196/jmir.2952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Norman GJ, Zabinski MF, Adams MA, Rosenberg DE, Yaroch AL, Atienza AA. A review of eHealth interventions for physical activity and dietary behavior change. Am J Prev Med. 2007;33(4):336–345. doi: 10.1016/j.amepre.2007.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.National Center for Education Statistics. The condition of education 2007. In: U.S. Department of Education, Institute of Education Sceicne, National Center of Education Statistics, editor. National Center for Education Statistics; 2007. https://nces.ed.gov/pubsearch/pubsinfo.asp?pubid=2007064. [Google Scholar]
- 125.Plimpton S, Root J. Materials and strategies that work in low literacy health communication. Public Health Rep. 1994;109(1):86–92. [PMC free article] [PubMed] [Google Scholar]
- 126.BeLue R, Taylor-Richardson KD, Lin J, Rivera AT, Grandison D. African Americans and participation in clinical trials: Differences in beliefs and attitudes by gender. Contemporary Clinical Trials. 2006;27(6):498–505. doi: 10.1016/j.cct.2006.08.001. doi: http://dx.doi.org/10.1016/j.cct.2006.08.001. [DOI] [PubMed] [Google Scholar]
- 127.Peek ME, Wilson SC, Gorawara-Bhat R, Odoms-Young A, Quinn MT, Chin MH. Barriers and facilitators to shared decision-making among African-Americans with diabetes. J Gen Intern Med. 2009;24(10):1135–1139. doi: 10.1007/s11606-009-1047-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Whaley AL. Cultural Mistrust and Mental Health Services for African Americans: A Review and Meta-Analysis. The Counseling Psychologist. 2001;29(4):513–531. [Google Scholar]
- 129.King WD. Examining African Americans' Mistrust of the Health Care System: Expanding the Research Question. Commentary on "Race and Trust in the Health Care System". Public Health Reports (1974-) 2003;118(4):366–367. doi: 10.1093/phr/118.4.366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Chandra A, Paul DP., 3rd African American participation in clinical trials: recruitment difficulties and potential remedies. Hospital topics. 2003;81(2):33–38. doi: 10.1080/00185860309598020. [DOI] [PubMed] [Google Scholar]
- 131.Kennedy BMBM. Cultural characteristics of African Americans: implications for the design of trials that target behavior and health promotion programs. Ethnicity & disease. 2007;17(3):548. [PubMed] [Google Scholar]
- 132.Glanz K, Bishop DB. The role of behavioral science theory in development and implementation of public health interventions. Annu Rev Public Health. 2010;31:399–418. doi: 10.1146/annurev.publhealth.012809.103604. [DOI] [PubMed] [Google Scholar]
- 133.Levy RL, Finch EA, Crowell MD, Talley NJ, Jeffery RW. Behavioral intervention for the treatment of obesity: strategies and effectiveness data. Am J Gastroenterol. 2007;102(10):2314–2321. doi: 10.1111/j.1572-0241.2007.01342.x. [DOI] [PubMed] [Google Scholar]
- 134.Noar SM, Benac CN, Harris MS. Does tailoring matter? Meta-analytic review of tailored print health behavior change interventions. Psychol Bull. 2007;133(4):673–693. doi: 10.1037/0033-2909.133.4.673. [DOI] [PubMed] [Google Scholar]
- 135.Albert B. Social Learning Theory. Englewood Cliffs, NJ: Prentice Hall; 1977. [Google Scholar]
- 136.Bandura A. Social foundations of thought and action: A social cognitive framework. Englewood Cliffs, NJ: Prentice Hall; 1986. [Google Scholar]
- 137.Michie S, Abraham C, Whittington C, McAteer J, Gupta S. Effective techniques in healthy eating and physical activity interventions: a meta-regression. Health Psychol. 2009;6:690–701. doi: 10.1037/a0016136. [DOI] [PubMed] [Google Scholar]
- 138.Chase JA. Physical activity interventions among older adults: a literature review. Res Theory Nurs Pract. 2013;27(1):53–80. doi: 10.1891/1541-6577.27.1.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Bélanger-Gravel A, Godin G, Vézina-Im LA, Amireault S, Poirier P. The effect of theory-based interventions on physical activity participation among overweight/obese individuals: a systematic review. Obes Rev. 2011;12(6):430–439. doi: 10.1111/j.1467-789X.2010.00729.x. [DOI] [PubMed] [Google Scholar]
- 140.Keller CS, Coe K, Moore N. Addressing the demand for cultural relevance in intervention design. Health Promot Pract. 2014;15(5):654–663. doi: 10.1177/1524839914526204. [DOI] [PubMed] [Google Scholar]
- 141.Henderson KA. Physical activity among African American women: changes and ways of knowing. Quest. 2011;63:11. [Google Scholar]
- 142.Kumanyika SK, Obarzanek E, Stettler N, et al. Population-based prevention of obesity: the need for comprehensive promotion of healthful eating, physical activity, and energy balance: a scientific statement from American Heart Association Council on Epidemiology and Prevention, Interdisciplinary Committee for Prevention (formerly the expert panel on population and prevention science) Circulation. 2008;4:428–464. doi: 10.1161/CIRCULATIONAHA.108.189702. [DOI] [PubMed] [Google Scholar]