Abstract
Pediatric arterial aneurysm is rare disease. Among them, idiopathic-congenital arterial aneurysm is extremely rare. This is a case report of right common iliac artery idiopathic aneurysm with absence of right external iliac artery. A 4-year-old girl who had been complaining of intermittent abdominal pain since 2 years prior presented with a right lower abdominal mass that had been palpable since 6 months prior. Abdominal CT revealed a 5.2 cm × 4.5 cm × 5.1 cm, right-sided, partially thrombosed, saccular, iliac artery aneurysm. She underwent to operation, aneurismal resection. A pathological examination confirmed that it was a true aneurysm, considering that all layers of the vascular wall were stretched with no deficit. The patient was discharged 3 days after the surgery without any complication. Five months passed since the surgery, and the patient is doing well without any abdominal or leg pain.
Keywords: Aneurysm, Iliac aneurysm, Child, Vascular surgical procedure
INTRODUCTION
Arterial aneurysm is rare in children. Among all types of arterial aneurysm, isolated iliac artery aneurysm shows an estimated prevalence of 0.008% to 0.03% based on autopsy series reported in adults [1]. One third of iliac artery aneurysms are bilateral [2]. The incidence rate of iliac artery aneurysm in children is not known because only a few cases have been reported. Most cases of aneurysm are caused by infection, arteritis, collagen vascular disease, vascular malformation and trauma [3]. This report aims to describe an idiopathic right common iliac artery aneurysm in a 4-year-old girl who does not have a right external iliac artery.
CASE REPORT
A 4-year-old girl who had been complaining of intermittent abdominal pain since 2 years prior presented with a right lower abdominal mass that had been palpable since 6 months prior. At the time of her visit to Seoul National University Children's Hospital, the patient had no abdominal or leg pain. On examination, she had no fever but a 5-cm pulsatile mass-like lesion was palpable on her right lower abdomen. The patient was born, weighing 3.3 kg, by vaginal delivery after 38 weeks and 1 day of gestation. No other abnormalities were found in the screening test. The patient, who had been healthy with no special medical history after birth, had a medical history of hand-foot-and-mouth disease 1 year earlier. She had also been hospitalized to receive pneumonia treatment 12 months after birth and 1 month before visiting our hospital. She had no medical history of abdominal injury. No evidence of inflammation or collagen vascular disease was found in the blood test, and all test results were within their normal ranges.
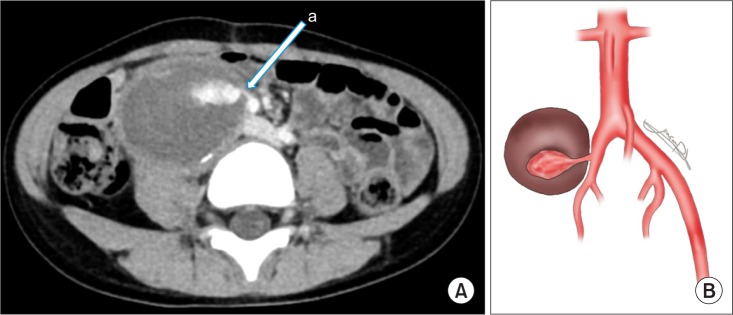
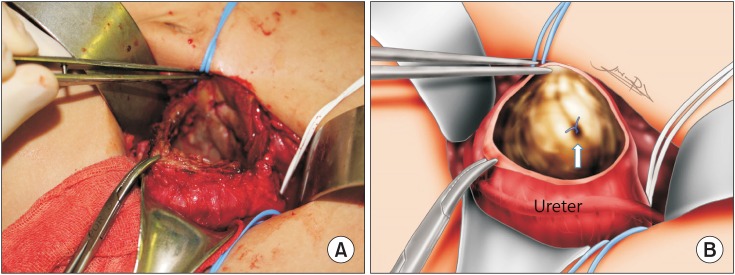
Abdominal ultrasonography revealed a 4.6 × 5.0-cm well-defined mass in the right lower quadrant, with large internal vascularity (Fig. 1). Abdominal CT revealed a 5.2 cm × 4.5 cm × 5.1 cm, right-sided, partially thrombosed, saccular, iliac artery aneurysm. The aneurysm could be observed at the aortic bifurcation level. The left iliac artery of the patient was normal. However, in the right iliac artery, a communication with the aneurysm, which was located at the level where the common iliac artery bifurcates into the internal and external iliac arteries, was confirmed with contrast enhancement during the CT (Fig. 2A). The aneurysm was pushing the internal iliac artery to the medial side, and the external iliac artery could not be traced (Fig. 2B). The right common femoral artery was found at the inguinal ligament level by joining of the deep circumflex iliac artery and inferior hypogastric artery, which were more prominent than those of the left side. The size of the right common femoral artery was equal compared to the left side femoral artery, and were located in the same anatomic position. Both iliac veins were normal.
Fig. 1. Abdominal ultrasonographic image showing a 4.6 × 5.0-cm well-defined mass in the right lower quadrant.
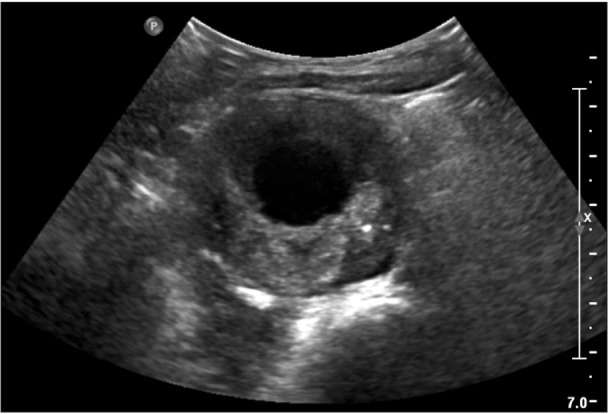
Fig. 2. (A) Contrast-enhanced computed tomographic image showing communication (arrow) between the aneurysm and the internal iliac artery. (B) Schematic anatomy of the right iliac artery aneurysm without a right external iliac.
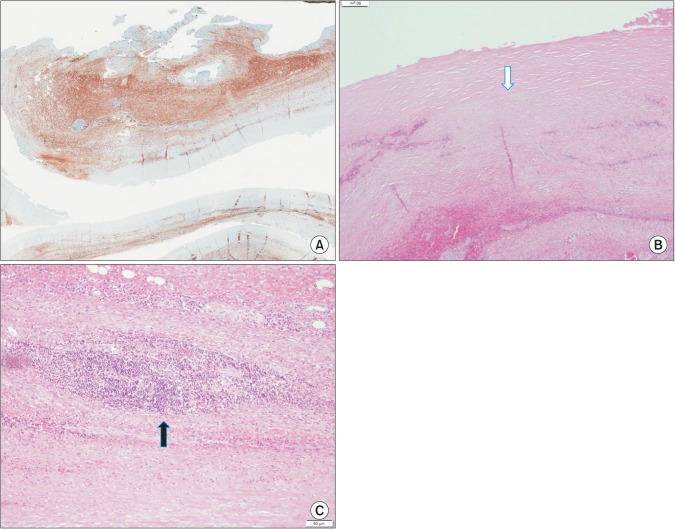
The surgery started with a transverse incision in the right lower abdomen. We reached near the iliac artery by retroperitoneal approach. An encapsulated pulsatile mass measuring 5 cm × 5 cm × 5 cm was found strongly adhered to the right common iliac artery and the surrounding tissues, particularly with the ureter. It was pushing the ureter to the anterolateral side. As it was difficult to separate the mass from the surrounding tissues, we placed vascular clamps on the proximal right common iliac artery and the distal right internal iliac artery. Then, we made an incision in the middle of the mass in the direction of the blood circulation. Large blood clot was found inside of the mass. The inside of the mass was covered with intima. As the mass had a pinpoint fistula with the right internal iliac artery on its medial side, primary closure of the fistula was performed by using a Prolene 6-0 suture (Fig. 3). No leakage was observed when the vascular clamps were removed, and normal distal flow was confirmed by checking the dorsalis pedis pulse. All of the aneurysm, except the parts that were strongly adhered to the surrounding tissues, was removed.
Fig. 3. (A) Intraoperative picture of the iliac arterial aneurysm. (B) Schematic anatomy of the intraoperative findings. The pinpoint fistula was repaired with a Prolene 6-0 suture (white arrow).
A pathological examination confirmed that it was a true aneurysm, considering that all layers of the vascular wall were stretched with no deficit (Fig. 4A). An intimal fibroplasia was confirmed (Fig. 4B), and an organizing thrombus was accompanied by chronic inflammation (Fig. 4C). Although myxoid degeneration was observed, we found no evidence of vasculitis. In addition, no bacteria were identified from the bacterial culture of the blood clot found from the aneurysm.
Fig. 4. (A) Smooth muscle actin stain [low power field, ×40] shows the all layers of the vascular wall without deficit. (B) Intimal fibroplasia (white arrow), [H&E, ×200] (C) Chronic inflammation (black arrow), [H&E, ×400].
The patient was discharged 3 days after the surgery without any complication. Five months passed since the surgery, and the patient is doing well without any abdominal or leg pain.
DISCUSSION
Aneurysms are rare in children. They should be carefully evaluated because they can be caused by collagen vascular diseases, arteritis, vascular malformation, trauma, or severe infections. In children, primary iliac arterial aneurysm is rare and is commonly associated with multiple congenital syndrome or Ehlers-Danlos syndrome. The least common type is idiopathic iliac aneurysm, which is not associated with any of the aforementioned disorders [4].
Sarkar et al. [3] reported a clinicopathological classification of childhood arterial aneurysm in 1991. According to the study, idiopathic-congenital aneurysm is a rare, with only 6 of 165 case reviews reporting it at that time. Until 2013, only 13 cases had been reported [2]. A common feature of this type of aneurysm is intimal fibroplasia, which suggests that idiopathic-congenital aneurysm is a secondary process rather than a change caused by any particular reason. The pathological findings in this case also showed intimal fibroplasia. It is advisable to consider this as an idiopathic-congenital aneurysm because the patient had no history of underlying diseases such as cardiac problems, vasculitis, collagen vascular diseases or trauma.
Surgical treatment of aneurysm should be planned upon consideration of the location of the aneurysm and its relationship with surrounding blood vessels and vital organs. Moreover, the patient's age and native vessel diameter should also be considered. Various vascular reconstruction materials can be used, and the materials reported so far include prosthetic grafts, reversed saphenous veins and cryopreserved arteries [5]. In this case, through the contrast enhancement in CT, a communication with the aneurysm was detected in the right common iliac artery at the level where it bifurcates into the internal and external iliac arteries. The aneurysm did not show any connectivity to other organs or blood vessels, except the iliac artery. Although the patient's external iliac artery was not visible, aneurysmal excision was planned because the right common femoral artery, which was the same size as the one on the left, could be found at the upper thigh level using the collateral arteries.
Mycotic aneurysm refers to an aneurysm or pseudoaneurysm caused by bacteria or other infectious agents [6]. The most common causes include Staphylococcus aureus and Salmonella species [7]. Mycotic aneurysm is a disease that is particularly rare in children. Bacterial endocarditis used to be the most common cause in the past, but owing to the recent advances in antibiotics, it is now known to occur in association with neonatal umbilical artery catheterization [6,8,9]. Although the patient in this case had a history of undergoing inpatient pneumonia treatment twice, she did not have any special medical history during the neonatal period and no cardiac problem was found in the preoperative examinations.
Iliac artery aneurysm accompanied by other anatomical abnormalities, which was observed in the present case, has not yet been reported. In 2004, Milas et al. [10] reported 2 cases of iliac artery injury associated with blunt trauma, and both cases were caused by vehicle collision. The first patient, a 12-year-old, showed incomplete transection of the left common iliac artery, and hypogastric artery interposition graft was performed. The second patient showed complete transection of the aorta and avulsion of the right iliac artery in the aorta and bilateral iliac arteries. For this patient, the hypogastric artery was used as an interposition patch and right iliac-left arterial anastomosis was performed. However, in the present case, the patient had no history of trauma.
Aneurysm is rare in children. Although it does not cause any symptom and is mostly found incidentally, prompt surgical treatment is essential because of fatal complications such as rupture or peripheral embolization. In cases where the cause of the aneurysm cannot be elucidated, as in the present case, long-term follow-up is necessary to check for possible recurrence of the aneurysm or new aneurysms occurring elsewhere.
Footnotes
CONFLICTS OF INTEREST: No potential conflict of interest relevant to this article was reported.
References
- 1.Brunkwall J, Hauksson H, Bengtsson H, Bergqvist D, Takolander R, Bergentz SE. Solitary aneurysms of the iliac arterial system: an estimate of their frequency of occurrence. J Vasc Surg. 1989;10:381–384. doi: 10.1067/mva.1989.13733. [DOI] [PubMed] [Google Scholar]
- 2.Chithra R, Sundar RA, Velladuraichi B, Sritharan N, Amalorpavanathan J, Vidyasagaran T. Pediatric isolated bilateral iliac aneurysm. J Vasc Surg. 2013;58:215–216. doi: 10.1016/j.jvs.2012.11.036. [DOI] [PubMed] [Google Scholar]
- 3.Sarkar R, Coran AG, Cilley RE, Lindenauer SM, Stanley JC. Arterial aneurysms in children: clinicopathologic classification. J Vasc Surg. 1991;13:47–56. [PubMed] [Google Scholar]
- 4.Moritz MW. Primary iliac artery aneurysm in a two-year-old girl. Ann Vasc Surg. 1986;1:392–395. doi: 10.1016/S0890-5096(06)60143-X. [DOI] [PubMed] [Google Scholar]
- 5.Kaye AJ, Slemp AE, Chang B, Mattei P, Fairman R, Velazquez OC. Complex vascular reconstruction of abdominal aorta and its branches in the pediatric population. J Pediatr Surg. 2008;43:1082–1088. doi: 10.1016/j.jpedsurg.2008.02.035. [DOI] [PubMed] [Google Scholar]
- 6.Bergsland J, Kawaguchi A, Roland JM, Pieroni DR, Subramanian S. Mycotic aortic aneurysms in children. Ann Thorac Surg. 1984;37:314–318. doi: 10.1016/s0003-4975(10)60737-0. [DOI] [PubMed] [Google Scholar]
- 7.Restrepo MS, Turek JW, Reinking B, Bergen NV. Mycotic aneurysm in a child with history of coarctation of the aorta repair. Ann Pediatr Cardiol. 2014;7:138–141. doi: 10.4103/0974-2069.132493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Monahan DA, Neville HL, Saigal GM, Perez EA, Sola JE. Infected common iliac artery aneurysm repaired in an infant with cadaveric vein graft. J Pediatr Surg. 2012;47:606–608. doi: 10.1016/j.jpedsurg.2012.01.011. [DOI] [PubMed] [Google Scholar]
- 9.Malloy MH, Nichols MM. False abdominal aortic aneurysm: an unusual complication of umbilical arterial catheterization for exchange transfusion. J Pediatr. 1977;90:285–286. doi: 10.1016/s0022-3476(77)80652-5. [DOI] [PubMed] [Google Scholar]
- 10.Milas ZL, Dodson TF, Ricketts RR. Pediatric blunt trauma resulting in major arterial injuries. Am Surg. 2004;70:443–447. [PubMed] [Google Scholar]