Abstract
Background
Increases in insurance coverage and price cut of drugs are two important measures to make health care more accessible and affordable. As far as we know, this was the first study to explore the impact of anticancer drug price cut on health expenses and oncologist’s prescription decisions in China.
Methods
The 511 non-small cell lung cancer (NSCLC) patients were recruited from Qilu Affiliated Hospital of Shandong University from January 1, 2003 to December 31, 2010. We categorized the patients into five groups based on China’s fifth population census in 2000, including administrative group, workers and services group, peasants group, professionals group and others group. All statistical analyses were performed using SPSS (version 16.0), all statistic tests were two-tailed and P value ≤0.05 was considered significant.
Results
As for the first-line chemotherapy regimens prescribed during the study, 27.6% patients received vinorelbine + cisplatin (NP), 31.5% and 30.9% patients had gemcitabine + cisplatin (GC) and docetaxel + cisplatin (DC), respectively, while only 4.3% patients received paclitaxel + cisplatin or carboplatin (TP). Before price policy implementation, NP was the most popularly used regimen (44.6%). By contrast, doctors’ prescription choices changed significantly after drug price cut, GC took first place (42.0%). GC became the most expensive regimen (4,431.40 RMB per cycle, about 665.15 dollars per cycle), while NP cost the least (1,974.48 RMB per cycle, about 296.37 dollars per cycle) after price cut. No significant reduction could be seen for both the pharmaceutical spending and total expense per inpatient episode after drug price adjustment. One interesting phenomena was that doctors relied less on patient’s sex, age, histology to make their decisions, by contrast, more on patient’s occupation and health insurance type. And, the total drug cost was closely related to patient occupation and health insurance type.
Conclusions
The introduction of anticancer drug price control policy was found to be ineffective on the containment of hospital drug expenditures in one cancer center in China.
Keywords: Anticancer drugs price cut, physician’s prescription choices, advanced non-small cell lung cancer, China
Introduction
The high cost of medical care in China has been denounced widely and the problems of rapidly rising expenditures on drugs are urgent (1). In order to make health care more accessible and affordable, China has accelerated its health reforms in the past decades. Increases in insurance coverage and price cut of drugs are two of those important measures. By far, over 90% Chinese population have been covered by three health insurance schemes, including new rural cooperative medical scheme (NRCMS), urban resident basic medical insurance (URBMI), urban employee basic medical insurance (UEBMI). Such remarkable increases in insurance coverage and inpatient reimbursement have made great contribution to the equality in access of health services across China. Unfortunately, these improvements do not lead to reduction in catastrophic health expenses, which still reach to 12.9% of households averaging in 2011 (2,3). Even worse, controlling retail drug prices was also shown to have limited effect to contain hospitals’ drug expenditure in China (4). One important underlying cause stems from inappropriate incentives of China’s fee-for-service system in public hospitals, which leads to overuse of medicines and technology by doctors (5). At the same time, there is lack of health monitoring system to implement strong controls on quality, volumes of services and medicines prescribed or hospital fees, which exacerbates the overuse of medical resources and financial burden of household out-of-pocket health expenditure.
Cancer has become the major killer in today’s China, especially that lung cancer increased by 465% during the past 30 years, and became the leading cause of death (6). However, the war against cancer is not just finding cures and better treatments, but also being able to afford them. Total costs from cancer were 86.85 billion RMB (about 13.04 billion dollars) in 2003, which accounted for 7.23% of the total health expenses from diseases and projected to rise (7). In May 2006, the National Development and Reform Commission (NDRC) issued the most dramatic price reduction of anticancer drugs in China, which involved in chemotherapy drug price, infusion costs, clinic costs, physician visit reimbursement and so on. In this study, we mainly focus on the anticancer drugs price cut policy. Was the policy effective as expected? Whether the cancer drugs price cut was accompanied by reduction in health expenses in China is still largely unknown.
Experience in diseases other than cancer has shown that physicians would change their prescription habits in face of drug price reduction and use drugs with higher profit margins even when less costly alternatives were available, and add those expensive drugs without strong evidence of benefit (4). Unfortunately, such irrational use of drugs is common in health care facilities in China (8,9). Thus, the good intentions of anticancer drugs price reduction by policy makers will be at a great risk of being distorted as long as doctors’ income is dependent on drug selection and drug overuse. Therefore, investigating the possible impact of drug price cut on the selection of chemotherapy regimens by oncologists and inpatient expenses would be of paramount value for health policy makers from both social and economic standpoints. In this study, we choose lung cancer as an example to explore the efficiency of anticancer drug price reduction.
Lung cancer is the most prevalent and aggressive disease in China. More than 87% cases are non-small cell lung cancer (NSCLC). Patients are usually diagnosed in relatively late stages with little chance of cure (10). The median survival is generally less than 1 year for advanced NSCLC patients. Systemic chemotherapy remains the standard therapy in the past decade in spite of the paradigm shift according to EGFR mutation status and histopathology since 2009 (11). The major difference between platinum-based doublet chemotherapy, which consists of vinorelbine, paclitaxel, docetaxel or gemcitabine, is not in the outcomes, rather the side effects and cost. Since pemetrexed was not approved in NSCLC for first-line therapy before the drug price cut in 2006, it was not included in this study. The tyrosine kinase inhibitors were mainly prescribed for out-patients with EGFR mutation and were also excluded in this study. As far as we know, this was the first study to explore the impact of anticancer drug price cut on health expenses and oncologist’s prescription decisions in China.
Methods
Data sources and data collection
We collected data from electronic medical record (EMR) system of Qilu Affiliated Hospital of Shandong University, which was one tertiary comprehensive 3,000-bed hospital and directly managed by the Ministry of Health in China. Patients of advanced NSCLC were identified from EMR of cancer center before and after the implementation of anticancer drug price cut (from January 1, 2003 to December 31, 2010). The inclusion criteria were the following, aged ≥18 years, histologically or cytologically confirmed, stage IIIB or IV, ECOG score 0 to 1, and chemotherapy-naïve. These patients received one of the following platinum-based combination chemotherapy, including vinorelbine + cisplatin (NP), gemcitabine + cisplatin (GC), paclitaxel + cisplatin or carboplatin (TP), docetaxel + cisplatin (DC). Other regimens mainly included the second generation drugs such as etoposide, vidensine, mitomycin and ifosfamide.
In total, 511 NSCLC patients met the above criteria. Data included the following information, such as sex, age, occupation, health insurance type, inpatient date, histology or cytology, chemotherapy regimen, and inpatient expenses including both drug and total cost. We categorized the patient occupations into five groups based on China’s fifth population census in 2000. Cadres, administrative and managerial were categorized into one group and named administrative. Patients who work in service and production, transportation and those manual workers were grouped into workers and services. Patients who work in agriculture, fishing and forestry were grouped as peasants. Intellectuals in education, science, artist and technology et al. were grouped as professionals. Those without detailed information of occupation or laid-off and unemployed were grouped into others. During this study time period, social health insurance underwent massive reforms in China and were summarized as following, three main payment methods described above, such as NRCMS, URBMI, UEBMI, and three other minor styles, such as publicly funded free medical care (PFFMC), payment from personal funds (PFPF), those whose payment information was unavailable (NA). Patients could get more reimbursement for URBMI and PFFMC than other insurance types in China. This study was approved by Ethics Committee of Qilu Hospital of Shandong University.
Medical costs
As for each chemotherapy regimen, the expected changes of anticancer drug expense after price cut was calculated in the following way and based on the following assumptions. Doublet regimen cost was calculated by combining the cost of each drug and each anticancer drug was given the dose and schedule recommended by NCCN and also used in our cancer center. For example, vinorelbine 25–30 mg/m2 on days 1 and 8, gemcitabine 1,000 mg/m2 on days 1 and 8, paclitaxel 135–175 mg/m2 on day 1, docetaxel 60–75 mg/m2 on day 1, cisplatin 75 mg/m2 on day 1 or in three days. The lower dose limit was used for cost estimation. Besides, each patient was assumed to have a body surface area of 1.6 m2.
In order to compare the actual drug and total inpatient expenses before and after drug price cut, data were collected from EMR in 306 patients who received one cycle of chemotherapy during hospital stay. Those who received multiple cycles of chemotherapy during one inpatient stay (205 cases) were excluded. In addition, in order to explore the factors related to costs, 229 out of 306 patients who received chemotherapy after price cut were included for analysis.
Statistical analyses
We first compared patients’ characteristics before and after anticancer drug price cut using Pearson chi-square test. We then used both univariate analysis and multinomial logistic regression to explore the correlation of physicians’ prescription patterns to policy implementation and patient characteristics. Considering the combination of docetaxel and cisplatin was one of the most used regimens both before and after price cut, it was chosen as a reference in the multinomial logistic regression model. In order to estimate precisely the changes of prescription patterns within this study period, we plotted the regression adjusted likelihood to receive one doublet chemotherapy regimen by year. T-test was used to compare the hospital expenses before and after drug price policy implementation. ANOVA was used to explore the factors related to the drug and hospital expenses. All statistical analyses were performed using SPSS (version 16.0), all statistic tests were two-tailed and P value ≤0.05 was considered significant.
Results
Patient characteristics
The demographic characteristics of NSCLC patients were shown in Table 1. Roughly 60% patients paid the hospital expenses by health insurance with different reimbursement ratios. However, there were still 20% patients who had to pay from their own pocket (PFPF). For those patients whose payment methods were unavailable, most of the expenses were also considered to be paid from their household. As for the first-line chemotherapy regimens prescribed during the study period from 2003 to 2010, 27.6% patients received NP, 31.5% and 30.9% patients had GC and DC, respectively, while only 4.3% patients received TP.
Table 1. Demographic characteristics of the advanced NSCLC patients before and after drug price cut policy implementation.
| Characteristics | N (%) | Before the policy, N (%) | After the policy, N (%) | χ2 value | P value |
|---|---|---|---|---|---|
| Sex | 0.200 | 0.655 | |||
| Male | 355 (69.5) | 144 (70.6) | 211 (68.7) | ||
| Female | 156 (30.5) | 60 (29.4) | 96 (31.3) | ||
| Age (years) | 0.033 | 0.857 | |||
| ≥60 | 258 (50.5) | 102 (50.0) | 156 (50.8) | ||
| <60 | 253 (49.5) | 102 (50.0) | 151 (49.2) | ||
| Histology | 2.802 | 0.423 | |||
| Adenocarcinoma | 270 (52.8) | 108 (52.9) | 162 (52.8) | ||
| Squamous carcinoma | 179 (35.0) | 69 (33.8) | 110 (35.8) | ||
| Others | 32 (6.3) | 11 (5.4) | 21 (6.8) | ||
| Undefined | 30 (5.9) | 16 (7.8) | 14 (4.6) | ||
| Occupation | 19.753 | 0.001 | |||
| Professionals | 47 (9.2) | 21 (10.3) | 26 (8.5) | ||
| Administrative | 129 (25.2) | 70 (34.3) | 59 (19.2) | ||
| Worker and service | 127 (24.9) | 36 (17.6) | 91 (29.6) | ||
| Peasant | 154 (30.1) | 55 (27.0) | 99 (32.2) | ||
| Others | 54 (10.6) | 22 (10.8) | 32 (10.4) | ||
| Health insurance type | 54.746 | <0.001 | |||
| URBMI | 6 (1.2) | 1 (0.5) | 5 (1.6) | ||
| PFPF | 102 (20.0) | 38 (18.6) | 64 (20.8) | ||
| PFFMC | 79 (15.5) | 49 (24.0) | 30 (9.8) | ||
| NRCMS | 27 (5.3) | 3 (1.5) | 24 (7.8) | ||
| UEBMI | 192 (37.6) | 52 (25.5) | 140 (45.6) | ||
| NA | 105 (20.5) | 61 (29.9) | 44 (14.3) | ||
| Total | 511 (100.0) | 204 (100.0) | 307 (100.0) | – | – |
NSCLC, non-small cell lung cancer; NRCMS, new rural cooperative medical scheme; URBMI, urban resident basic medical insurance; UEBMI, urban employee basic medical insurance; PFFMC, publicly funded free medical care; PFPF, payment from personal funds; NA, those whose payment information was unavailable.
Some changes of patients’ characteristics were evident after price policy implementation. More workers and peasants (from 44.6% to 61.8%) were hospitalized and received chemotherapy for advanced NSCLC, which might result from more participation in health insurance due to health reform. The patients who paid the hospital charges by UEBMI or NRCMS increased from 27.0% to 53.4% after June 2006.
Changes of physician’s decision for first-line chemotherapy regimens after anticancer drugs price cut
As shown in Table 2, before price policy implementation, NP was the most popularly used regimen (44.6%). By contrast, doctors’ prescription choices changed significantly after drug price cut, GC took first place (42.0%). Figure 1 showed the time pattern of prescription changes during 2003 to 2010. NP was the most popularly used in 2004 (68.4%) and in the long run after drug price adjustment, NP was on the way out. DC experienced the most striking increase from 2004 to 2005 and climbed to the top of use in 2008 (47.6%). GC prescription increased dramatically in 2006 and coincided with the implementation of price cut. It took first place since 2009 and reached the climax in 2010 (60.1%). As for TP, it was the least commonly used in this study and did not change much with year. In addition, there was a significant decrease to prescribe second generation drugs since 2004, indicating that the second generation drugs withdrew their stage in a pre-existing trend and may be not associated with drugs price cut policy implementation in May 2006.
Table 2. Identification of these presented factors by univariate analysis to confirm which might influence the oncologist’s decisions on first-line chemotherapy regimens.
| Characteristics | First line chemotherapy regimens | P value | ||||
|---|---|---|---|---|---|---|
| NP (%) | DC (%) | GC (%) | TP (%) | Others (%) | ||
| Sex | 0.714* | |||||
| Female | 46 (29.5) | 43 (27.6) | 53 (34.0) | 7 (4.5) | 7 (4.5) | |
| Male | 95 (26.8) | 115 (32.4) | 108 (30.4) | 15 (4.2) | 22 (6.2) | |
| Age (years) | 0.055* | |||||
| <60 | 85 (33.6) | 72 (28.5) | 74 (29.3) | 10 (4.0) | 12 (4.7) | |
| ≥60 | 56 (21.7) | 86 (33.3) | 87 (33.7) | 12 (4.7) | 17 (6.6) | |
| Histopathology | 0.821* | |||||
| Adenocarcinoma | 82 (30.4) | 76 (28.1) | 86 (31.9) | 12 (4.4) | 14 (5.2) | |
| Squamous carcinoma | 45 (25.1) | 58 (32.4) | 58 (32.4) | 8 (4.5) | 10 (5.6) | |
| Others | 6 (18.8) | 12 (37.5) | 10 (31.2) | 2 (6.2) | 2 (6.2) | |
| Undefined | 8 (26.7) | 12 (40.0) | 7 (23.3) | 0 | 3 (10.0) | |
| Occupation | <0.001* | |||||
| Professionals | 13 (27.7) | 13 (27.7) | 18 (38.3) | 0 | 3 (6.4) | |
| Administrative | 30 (23.3) | 33 (25.6) | 50 (38.8) | 13 (10.1) | 3 (2.3) | |
| Workers and services | 26 (20.5) | 40 (31.5) | 55 (43.3) | 2 (1.6) | 4 (3.1) | |
| Peasant | 62 (40.3) | 49 (31.8) | 28 (18.2) | 3 (1.9) | 12 (7.8) | |
| Others | 10 (18.5) | 23 (42.6) | 10 (18.5) | 4 (7.4) | 7 (13.0) | |
| Health insurance | <0.001** | |||||
| URBMI | 0 | 5 (83.3) | 1 (16.7) | 0 | 0 | |
| PFPF | 22 (27.8) | 13 (16.5) | 33 (41.8) | 9 (11.4) | 2 (2.5) | |
| PFFMC | 40 (39.2) | 37 (36.3) | 18 (17.6) | 2 (2.0) | 5 (4.9) | |
| NRCMS | 10 (37.0) | 8 (29.6) | 7 (25.9) | 1 (3.7) | 1 (3.7) | |
| UEBMI | 32 (16.7) | 71 (37.0) | 82 (42.7) | 3 (1.6) | 4 (2.1) | |
| NA | 37 (35.2) | 24 (22.9) | 20 (19.0) | 7 (6.7) | 17 (16.2) | |
| Policy | <0.001* | |||||
| Before the policy | 91 (44.6) | 51 (25.0) | 32 (15.7) | 11 (5.4) | 19 (9.3) | |
| After the policy | 50 (16.3) | 107 (34.9) | 129 (42.0) | 11 (3.6) | 10 (3.3) | |
| Total | 141 (27.6) | 158 (30.9) | 161 (31.5) | 22 (4.3) | 29 (5.7) | – |
*, Chi-square test; **, Fisher exact test; NSCLC, non-small cell lung cancer; NRCMS, new rural cooperative medical scheme; URBMI, urban resident basic medical insurance; UEBMI, urban employee basic medical insurance; PFFMC, publicly funded free medical care; PFPF, payment from personal funds; NA, those whose payment information was unavailable.
Figure 1.
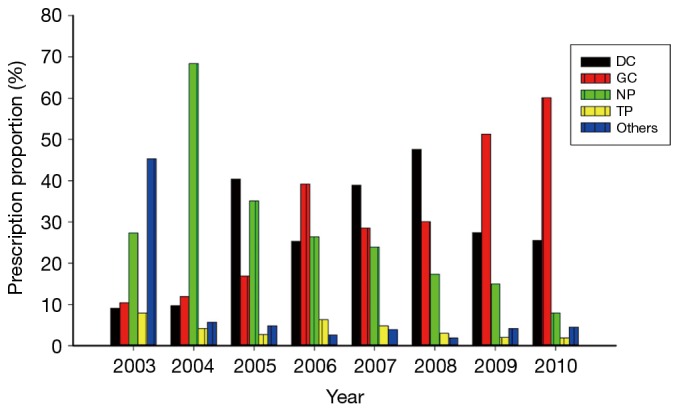
The time pattern of prescription changes during 2003 to 2010.
Changes of drug cost and total health expenditure per inpatient episode in advanced NSCLC patients after price adjustment
As shown in Table 3, among the regimens, the price of paclitaxel was reduced the most, vinorelbine the next, docetaxel the third, and gemcitabine the least. GC became the most expensive regimen (4,431.40 RMB per cycle, about 665.15 dollars per cycle), while NP cost the least (1,974.48 RMB per cycle, 296.37 dollars per cycle) after price cut.
Table 3. Changes in sales price (RMB) of generic single and combined anticancer drugs after price adjustment.
| Drug sales price (RMB) | Before June, 2006 | After June, 2006 | Changes of price (%) |
|---|---|---|---|
| Single drugs | |||
| Vinorelbine (10 mg) | 303.40 | 223.06 | −26.50 |
| Docetaxel (20 mg) | 857.30 | 712.00 | −16.95 |
| Gemcitabine (0.20g) | 1,396.50 | 1,235.00 | −11.56 |
| Gemcitabine (1g) | 319.00 | 294.40 | −7.71 |
| Paclitaxel (30 mg) | 936.00 | 555.00 | −40.71 |
| Cisplatin (20 mg) | 37.10 | 32.50 | −12.40 |
| Combination regimens | |||
| NP | 2,649.80 | 1,974.48 | −25.49 |
| DC | 4,509.10 | 3,782.60 | −16.11 |
| GC | 4,929.60 | 4,431.40 | −10.11 |
| TP | 6,774.60 | 4,080.00 | −39.78 |
NSCLC, non-small cell lung cancer; NRCMS, new rural cooperative medical scheme; URBMI, urban resident basic medical insurance; UEBMI, urban employee basic medical insurance; PFFMC, publicly funded free medical care; PFPF, payment from personal funds; NA, those whose payment information was unavailable; NP, vinorelbine + cisplatin; DC, docetaxel + cisplatin; GC, gemcitabine + cisplatin; TP, paclitaxel + cisplatin or carboplatin. RMB at an exchange rate of 6.66 to US$ 1 on Aug 2016.
In spite of anticancer drugs price cut, as shown in Table 4, drugs expenditure still accounted for the majority of the health cost in NSCLC patients and reached about 70%. No significant reduction could be seen for both the pharmaceutical spending and total expense per inpatient episode after drug price adjustment when 306 patients were analyzed together. Overuse of drugs other than chemotherapy regimens, such as thymosin and some traditional Chinese medicines (data not shown) without strong evidence of survival benefit, might be one important reason that offset the benefit of anticancer price cut.
Table 4. Changes in both drug utilization and total inpatient cost per inpatient episode for advanced NSCLC patients after drug price cut.
| Regimen | Drug cost (RMB, mean ± SD) | P value | Total inpatient cost (RMB, mean ± SD) | P value | ||||
|---|---|---|---|---|---|---|---|---|
| Before June, 2006 | After June, 2006 | Changes (%) | Before June, 2006 | After June, 2006 | Changes (%) | |||
| NP | 5,955.12±2,308.14 | 3,556.04±803.97 | −40.29 | <0.001 | 7,815.42±2,934.38 | 5,345.01±1,494.64 | −31.61 | <0.001 |
| DC | 6,972.82±2,635.83 | 5,822.31±1,700.81 | −16.50 | 0.007 | 8,324.73±2,976.17 | 8,583.71±7,704.62 | 3.11 | 0.915 |
| GC | 7,600.71±1,852.48 | 7,959.04±2,213.61 | 4.71 | 0.699 | 9,060.92±1,975.04 | 10,737.54±.3,133.66 | 18.43 | 0.200 |
| TP | 8,440.74±1,883.73 | 9,337.61±4,999.31 | 10.63 | 0.717 | 9,666.94±2,238.03 | 12,831.07±8,731.45 | 32.73 | 0.348 |
| All regimens | 6,787.83±2,465.53 | 6,278.50 ±2,528.29 | −8.10 | 0.714 | 8,669.43±2,821.47 | 8,870.86±5,697.99 | 23.23 | 0.217 |
NSCLC, non-small cell lung cancer; SD, standard deviation; NRCMS, new rural cooperative medical scheme; URBMI, urban resident basic medical insurance; UEBMI: urban employee basic medical insurance; PFFMC, publicly funded free medical care; PFPF, payment from personal funds; NA: those whose payment information was unavailable. RMB at an exchange rate of 6.66 to US$ 1 on Aug, 2016.
As far as each regimen was concerned, the total drug cost was reduced in patients who received NP or DC. In contrast, for patients who received the GC or TP, the drug expenditure did not change much. As for the total inpatient expenses, only patients who received NP experienced significant reduction after price cut, while patients in other groups still had to pay for high inpatient cost as before.
Factors influencing physician’s first choice of chemotherapy regimens in advanced NSCLC patients
According to Tables 2 and 5, we believed that price adjustment policy itself was one of the most important factors that influenced doctors’ prescription either in univariate analysis or multinomial logistic regression analysis. One interesting phenomena was that doctors relied less on patient’s sex, age, histology to make their decisions, by contrast, more on patient’s occupation and health insurance type. Prescription of NP combination regimen was mostly for peasants who were supposed to have relatively lower income and those who had to pay hospital cost from their own pockets (PFPF), while GC was predominantly given to administrative staff, workers and those who had PFFMC and UEBMI.
Table 5. Factors related to physicians’ final decision of regimens in the multinomial logistic regression model.
| Demographic factors | Physician’s choice of chemotherapy regimens with DC as a reference regimen | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| NP vs. DC | GC vs. DC | TP vs. DC | Others vs. DC | ||||||||
| OR (95% CI) | P | OR (95% CI) | P | OR (95% CI) | P | OR (95% CI) | P | ||||
| Male (female as reference) | 0.80 (0.46–1.42) | 0.455 | 0.67 (0.38–1.19) | 0.175 | 0.59 (0.20–1.68) | 0.319 | 1.24 (0.46–3.36) | 0.668 | |||
| Age ≥60 (age <60 as reference) (years) | 2.11 (1.25–3.57) | 0.005 | 1.37 (0.81–2.31) | 0.240 | 1.31 (0.50–3.43) | 0.579 | 0.84 (0.35–2.02) | 0.696 | |||
| Histology (SC as reference) | |||||||||||
| Adenocarcinoma | 1.34 (0.77–2.33) | 0.307 | 1.08 (0.62–1.88) | 0.797 | 1.12 (0.40–3.12) | 0.827 | 1.07 (0.42–2.73) | 0.892 | |||
| Others | 0.66 (0.19–2.20) | 0.495 | 0.69 (0.24–2.00) | 0.492 | 0.80 (0.13–4.87) | 0.805 | 0.68 (0.11–4.14) | 0.675 | |||
| Undefined | 0.79 (0.26–2.40) | 0.674 | 1.06 (0.35–3.21) | 0.920 | NA | 1.44 (0.30–6.94) | 0.892 | ||||
| Health insurance type (PFPF as reference) | |||||||||||
| PFFMC | 1.08 (0.43–2.72) | 0.874 | 6.47 (2.37–17.68) | <0.001 | 11.52 (1.96–67.66) | 0.007 | 0.68 (0.11–4.30) | 0.685 | |||
| UEBMI | 0.38 (0.19–0.74) | 0.005 | 1.96 (0.95–4.06) | 0.070 | 0.67 (0.10–4.31) | 0.672 | 0.40 (0.10–1.62) | 0.199 | |||
| NRCMS | 1.82 (0.59–5.58) | 0.296 | 1.52 (0.43–5.45) | 0.519 | 2.36 (0.18–30.76) | 0.513 | 1.22 (0.12–12.63) | 0.866 | |||
| NA | 1.14 (0.54–2.42) | 0.729 | 2.06 (0.84–5.10) | 0117 | 5.16 (0.93–28.58) | 0.060 | 4.32 (1.35–13.90) | 0.014 | |||
| Price policy implementation (before price cut as reference) | 0.32 (0.19–0.56) | <0.001 | 3.29 (1.84–6.27) | <0.001 | 1.16 (0.42–3.23) | 0.777 | 0.35 (0.14–0.87) | 0.024 | |||
NSCLC, non-small cell lung cancer; NRCMS, new rural cooperative medical scheme; URBMI, urban resident basic medical insurance; UEBMI, urban employee basic medical insurance; PFFMC, publicly funded free medical care; PFPF, payment from personal funds; NA, those whose payment information was unavailable. Given that patient occupation was closely related to health insurance type (chi-square value =682.7, P<0.001), only health insurance type was entered into the multinomial logistic regression model in this study in order to maximize the stability of this model.
Factors influencing drug cost and total inpatient expenses in advanced NSCLC patients
As shown in Table 6, the total drug cost was closely related to patient occupation and health insurance type. Patients who were in the higher income bracket in China, such as professionals or administrative, or those who could get better reimbursement from health insurance such as URBMI and PFFMC, spent more money on drugs than the peasants or workers with relatively lower income or reimbursement from health insurance. The total inpatient expenses also showed a similar correlation to patient occupation and insurance types in spite of not reaching statistical significance.
Table 6. Factors related to drug cost and total inpatient cost in patients of advanced NSCLC patients.
| Characteristics | Drug cost (RMB, mean ± SD) | P value | Total inpatient cost (RMB, mean ± SD) | P value |
|---|---|---|---|---|
| Sex | 0.269 | 0.131 | ||
| Male | 6,469.90±2,734.72 | 9,572.50±7,020.80 | ||
| Female | 6,059.20±2,329.48 | 8,271.0±3,073.38 | ||
| Age (years) | 0.102 | 0.173 | ||
| >60 | 6,621.70±2,641.06 | 9,703.70±7,570.32 | ||
| ≤60 | 6,055.20±2,566.47 | 8,607.80±4,002.87 | ||
| Histology | 0.711 | 0.893 | ||
| Adenocarcinoma | 6,497.50±3,000.49 | 9,199.20± 4,526.55 | ||
| Sqamous carcinoma | 6,158.70±2,154.76 | 9,365.70±8,507.82 | ||
| Others | 5,876.20±1,894.75 | 8,150.80±3,453.65 | ||
| Undefined | 6,537.10±1,896.00 | 8,628.20±1,676.13 | ||
| Occupation | <0.001 | 0.279 | ||
| Professionals | 6,925.50±1,814.25 | 9,080.00±1,882.16 | ||
| Administrative | 7,730.90±2,771.50 | 10,436.00±3,736.57 | ||
| Worker and service | 6,338.40±2,613.75 | 9,732.20±4,429.15 | ||
| Peasant | 5,279.70±2,304.12 | 8,416.50±8,582.40 | ||
| Others | 5,492.70±1,128.88 | 7,392.50±1,879.26 | ||
| Health insurance type | <0.001 | 0.119 | ||
| URBMI | 4,700.40±471.69 | 5,792.40±571.59 | ||
| PFFMC | 7,972.20±3,143.1 | 10,382.00±4,346.07 | ||
| PFPF | 5,251.20±2,111.51 | 8,772.60±10,063.89 | ||
| NRCMS | 5,565.50±2,299.80 | 7,955.10±294.66 | ||
| UEBMI | 7,153.50±2,575.34 | 10,032.00±4,090.47 | ||
| NA | 4,952.60±1,831.76 | 6,797.80±2,357.19 |
NSCLC, non-small cell lung cancer; SD, standard deviation; NRCMS, new rural cooperative medical scheme; URBMI: urban resident basic medical insurance; UEBMI, urban employee basic medical insurance; PFFMC: publicly funded free medical care; PFPF, payment from personal funds; NA, those whose payment information was unavailable. RMB at an exchange rate of 6.66 to US$ 1 on Aug, 2016.
Discussion
There are two major findings in our study. One is that patient’s occupation and health insurance type strongly influenced physicians in their choices of first-line chemotherapy regimens in advanced NSCLC patients, which might be associated with anticancer drug price adjustment. The second finding is that the desired effect of relieving the patients’ economic burden by anticancer drugs price cut was not met. A combination of factors might contribute to these findings, which mainly included a switching of doctors’ prescription to a costly regimen without strong evidence of benefit.
Experience in other countries in lung cancer therapy came to the similar conclusions (12-14). Jacobson assessed how the reductions in reimbursement for chemotherapy drugs to physicians affected the likelihood of chemotherapy treatment for medicare beneficiaries with lung cancer, as well as the types of agents they received. One important finding in their study was that physicians switched from dispensing the drugs that experienced the largest cuts in profitability, carboplatin and paclitaxel, to other high-margin drugs, like docetaxel (13). Of note, there have been big differences in the commonly used chemotherapy regimens in NSCLC between China and America. Although treatment with paclitaxel and carboplatin was substantially expensive in America (15), according to the data from Cancer Research Network (CRN, 2000–2007), paclitaxel and carboplatin was the most popularly used and accounted for 57.1% (16). For other regimens, such as gemcitabine and carboplatin, gemcitabine and cisplatin, docetaxel and carboplatin, vinorelbine and carboplatin, their use was no more than 5%. By contrast, in our study, only 4.3% patients received paclitaxel and carboplatin or cisplatin, while the doublet of gemcitabine with cisplatin or carboplatin took first place and accounted nearly 60% by 2010. Such prescription differences among countries may be due to a number of factors including differences in oncologist practice style, patient preferences, drug retail prices and pharmaceutical market competition. But coincidently, doctors from different countries tend to use more expensive drugs in their own countries.
What drives oncologists change their behaviors after price cut? Economic dimension is emerging as a crucial factor in our understanding of cancer treatment. To our knowledge, little information is available on the changes of doctors’ behavior after drug policy implementation in cancer therapy in China. Similar studies have been done in patients with cerebral infarction or hypertension in China (17,18). Physicians also changed their prescription decisions and used drugs with higher profit margins instead when facing price reductions, even those expensive drugs without strong evidence of benefit. In this study, a striking switching trend to use costly anticancer drugs was evident during the period from 2003 to 2010, but we could not identify the major coincident changes in practice guidelines of lung cancer that can plausibly explain our results. No matter the changes were in a pre-existing trend or driven by price adjustment, they undoubtedly reflected physicians’ incentives to use the more expensive drugs.
These distorted incentives were criticized to root from misguided governmental pharmaceutical policies in China (9,19,20). As long as physicians’ income was related to drug profits, the drug price adjustment policy would not be expected to work effectively, especially with the lack of strict regulations of drug prescriptions and weakly evidence-based culture of medicine in China. The high percentages of drug expenditure in our study also reflected the dysfunction of drug price control policy. Thus, it is impractical to control rising health cost only by drug price cut in cancer patients in China. The key to control healthcare costs requires not only abolishing the distorting policies, but also changing doctors’ behavior by establishing a rightly directed financial reward in the practice of medicine and also an evaluating system to implement strong controls on quality, volumes of health services.
There are a few limitations in this study. First, we did not investigate the impact of patients’ education and comorbidities on doctors’ regimens selection and health costs. The possibility existed that some patients might make decisions themselves and asked for drugs by name. Comorbidities were also supposed to influence treatment and survival in lung cancer patients (21). Second, although Chinese public hospitals have similar expenditure, income and incentive structures throughout the country, caution should be paid to generalizing the finding from one hospital to all the others at a country level. Third, we did not adjust drug inflation when comparing the expenditure changes, given that the prices of medical service would not notably fluctuate together with the change in consumer price index.
Conclusions
The introduction of anticancer drug price control policy was found to be ineffective on the containment of hospital drug expenditures in one cancer center in China. A switching of doctors’ prescription to a costly regimen and overuse of expensive drugs without strong evidence of benefit might be the most important contributors. Physicians should be encouraged to base their decisions on evidence-based medicine and patients’ preferences, rather than the profits from drugs. It is urgent to establish a rightly directed financial reward in the practice of medicine and also a nation-wide evaluating system to implement strong controls on quality, volumes of services and deter inappropriate prescription.
Acknowledgements
Funding: We thank the financial support from Shandong University self-innovation grant (2012TS173).
Ethical Statement: Our study obtained ethics approval by Qilu Affiliated Hospital of Shandong University (No. 2015040) and written informed consent was obtained from all patients.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.Chen Y, Schweitzer SO. Issues in drug pricing, reimbursement, and access in China with references to other Asia-Pacific region. Value Health 2008;11 Suppl 1:S124-9. 10.1111/j.1524-4733.2008.00376.x [DOI] [PubMed] [Google Scholar]
- 2.Meng Q, Xu L, Zhang Y, et al. Trends in access to health services and financial protection in China between 2003 and 2011: a cross-sectional study. Lancet 2012;379:805-14. 10.1016/S0140-6736(12)60278-5 [DOI] [PubMed] [Google Scholar]
- 3.Long Q, Xu L, Bekedam H, et al. Changes in health expenditures in China in 2000s: has the health system reform improved affordability. Int J Equity Health 2013;12:40. 10.1186/1475-9276-12-40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Meng Q, Cheng G, Silver L, et al. The impact of China's retail drug price control policy on hospital expenditures: a case study in two Shandong hospitals. Health Policy Plan 2005;20:185-96. 10.1093/heapol/czi018 [DOI] [PubMed] [Google Scholar]
- 5.Yip WC, Hsiao W, Meng Q, et al. Realignment of incentives for health-care providers in China. Lancet 2010;375:1120-30. 10.1016/S0140-6736(10)60063-3 [DOI] [PubMed] [Google Scholar]
- 6.Ministry of Health of the P.R. China. China's health care statistics yearbook. Beijing: Peking Union Medical College Press, 2009. [Google Scholar]
- 7.Zhao P, Dai M, Chen W, et al. Cancer trends in China. Jpn J Clin Oncol 2010;40:281-5. 10.1093/jjco/hyp187 [DOI] [PubMed] [Google Scholar]
- 8.Dong L, Yan H, Wang D. Drug prescribing indicators in village health clinics across 10 provinces of Western China. Fam Pract 2011;28:63-7. 10.1093/fampra/cmq077 [DOI] [PubMed] [Google Scholar]
- 9.Tian L, Liu J. Irrational Drug Use in China: Current Status and Countermeasures. Asian Journal of Social Pharmacy 2009;4:112-6. [Google Scholar]
- 10.William WN, Jr, Lin HY, Lee JJ, et al. Revisiting stage IIIB and IV non-small cell lung cancer: analysis of the surveillance, epidemiology, and end results data. Chest 2009;136:701-9. 10.1378/chest.08-2968 [DOI] [PubMed] [Google Scholar]
- 11.Leighl NB. Treatment paradigms for patients with metastatic non-small-cell lung cancer: first-, second-, and third-line. Curr Oncol 2012;19:S52-8. 10.3747/co.19.1114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Newcomer LN. Changing physician incentives for cancer care to reward better patient outcomes instead of use of more costly drugs. Health Aff (Millwood) 2012;31:780-5. 10.1377/hlthaff.2012.0002 [DOI] [PubMed] [Google Scholar]
- 13.Jacobson M, Earle CC, Price M, et al. How Medicare's payment cuts for cancer chemotherapy drugs changed patterns of treatment. Health Aff (Millwood) 2010;29:1391-9. 10.1377/hlthaff.2009.0563 [DOI] [PubMed] [Google Scholar]
- 14.Neumann PJ, Palmer JA, Nadler E, et al. Cancer therapy costs influence treatment: a national survey of oncologists. Health Aff (Millwood) 2010;29:196-202. 10.1377/hlthaff.2009.0077 [DOI] [PubMed] [Google Scholar]
- 15.Clegg A, Scott DA, Hewitson P, et al. Clinical and cost effectiveness of paclitaxel, docetaxel, gemcitabine, and vinorelbine in non-small cell lung cancer: a systematic review. Thorax 2002;57:20-8. 10.1136/thorax.57.1.20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ritzwoller DP, Carroll NM, Delate T, et al. Patterns and predictors of first-line chemotherapy use among adults with advanced non-small cell lung cancer in the cancer research network. Lung Cancer 2012;78:245-52. 10.1016/j.lungcan.2012.09.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chu HL, Liu SZ, Romeis JC. Assessing the effects of drug price reduction policies on older people in Taiwan. Health Serv Manage Res 2011;24:1-7. 10.1258/hsmr.2010.010016 [DOI] [PubMed] [Google Scholar]
- 18.Huang SH, Hsu CN, Yu SH, et al. Impact of drug price adjustments on utilization of and expenditures on angiotensin-converting enzyme inhibitors and angiotensin receptor blockers in Taiwan. BMC Public Health 2012;12:288. 10.1186/1471-2458-12-288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fan R. Corrupt practices in chinese medical care: the root in public policies and a call for Confucian-market approach. Kennedy Inst Ethics J 2007;17:111-31. 10.1353/ken.2007.0012 [DOI] [PubMed] [Google Scholar]
- 20.Sun Q, Santoro MA, Meng Q, et al. Pharmaceutical policy in China. Health Aff (Millwood) 2008;27:1042-50. 10.1377/hlthaff.27.4.1042 [DOI] [PubMed] [Google Scholar]
- 21.Grose D, Devereux G, Milroy R. Comorbidity in lung cancer: important but neglected. a review of the current literature. Clin Lung Cancer 2011;12:207-11. 10.1016/j.cllc.2011.03.020 [DOI] [PubMed] [Google Scholar]


