Abstract
Globally, tobacco smoke is the leading cause of preventable deaths. Smoking cessation counselling services are widely available in Canada. In British Columbia, our government-funded smoking cessation service offers counselling via phone, text, or email. In this study, we sought to determine whether age, gender, or motivation to quit affect a patient's choice of service modality.
We included all adults ≥ 18 years who had used tobacco within 30 days prior to their Emergency Department (ED) visit and who chose to receive phone, text, or email counselling services from November 2011–February 2013 at Vancouver General Hospital as part of a randomized-controlled trial (ClinicalTrials.gov, NCT0145437). A one-way ANOVA was used to compare the mean age of patients in each group. Chi-squared tests of independence were used to determine if gender or motivation to quit were associated with modality selection.
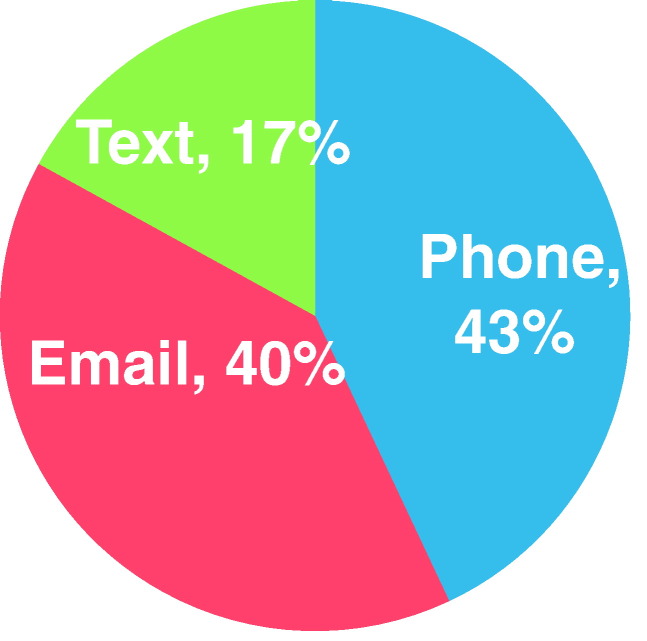
In total, 368 patients were included. The average age was 41.7 years and 67% were female. In our study, 44% chose phone, 17% chose text, and 40% chose email services. The average age for patients preferring text services (mean = 33.6 years) was significantly lower than both the email (mean = 41.3 years) and phone (mean = 45.1 years) groups (p < 0.001). Gender and motivation to quit were not associated with service modality choice.
Over 80% of ED smokers who accepted a referral to counselling services chose the phone or email modality. The lesser chosen text modality was more popular with younger patients. With further research, smoking cessation counselling services can refine their programs to meet the needs of the population they serve.
Keywords: Health promotion, Primary prevention, Smoking cessation
Highlights
-
•
Many smoking cessation quit lines offer counselling by phone, text, or internet.
-
•
> 80% of smokers in our study who accepted referral chose phone or internet counselling.
-
•
The lesser chosen text referral modality was more popular with younger patients.
-
•
Smoking cessation counselling services should work to meet their demographic's needs.
-
•
Counselling services that text should know they may attract a younger population.
1. Introduction
Tobacco smoke is the leading cause of preventable deaths worldwide causing about 6 million deaths per year (12% of all deaths) (World Health Organization, 2011). In Canada, > 37,000 die prematurely each year due to tobacco use (Reid et al., 2012). Many smokers visit the Emergency Department (ED) repeatedly for smoking-related medical conditions. The Society for Academic Emergency Medicine and the American College of Emergency Physicians recommend smoking cessation counselling in the ED (Rhodes et al., 2000, Stead et al., 2008). The ED visit may represent a “teachable moment” (McBride et al., 2003) in which sick individuals may be more motivated to quit smoking and be more receptive to counselling (Bernstein and Becker, 2002). To date, Canadian EDs have not officially endorsed smoking cessation counselling, and best practices for ED smoking cessation counselling have yet to be elucidated.
Smoking cessation quitlines, text support, and internet counselling are all available in Canada. All 3 modalities of counselling have been shown to increase quit rates for community populations, but these services have not been studied thoroughly in the ED population. A meta-analysis of proactive quitlines demonstrated increased quit rates in the community (RR 1.27; 95% CI 1.20 to 1.36) (Stead et al., 2013). However, utilization of these resources is very low, with a median reach of 0.30% of all smokers (North American Quitline Consortium (NAQC), 2011). Text and email counselling services have been introduced more recently. A meta-analysis found increased long-term quit rates compared with control, primarily recruiting patients from the community (RR 1.71, 95% CI 1.47 to 1.99) (Whittaker et al., 2012); in one trial, text counselling doubled quit rates at 6 months (10·7% vs 4·9%, p < 0.0001) (Free et al., 2011). Finally, a review of tailored internet-based interventions (Civljak et al., 2013) showed increased quit rates (RR 1.48, 95% CI 1.11 to 2.78) (Haug et al., 2011, Elfeddali et al., 2012, Smit et al., 2012). However, there was high risk of bias and heterogeneity in the included studies. Results from two other studies comparing non-tailored interventions to control did not detect an effect (McDonnell et al., 2011, Humfleet et al., 2013). Among trials that compared tailored to non-tailored internet interventions, one trial detected evidence of a benefit from a tailored email (Strecher et al., 2005) (RR 1.26, 95% CI 1.10 to 1.44), whereas a second trial did not detect evidence of an effect (Stoddard et al., 2008). The authors concluded that some internet-based interventions can assist smoking cessation at six months or longer, particularly those which are tailored to individuals. None of the trials above included ED patients.
Some advocates of ED smoking cessation counselling have recommended an “ask, advise, and refer” approach, where patients are asked whether or not they are a smoker, advised to quit, and then referred to a quitline, text support service, or internet counselling (Schroeder, 2005). As increasing smoking cessation services become available, and as there is some evidence that tailored interventions may be more effective than non-tailored interventions, further research to refine these programs may increase effectiveness. The objective of this study was to examine the potential relationship between age, gender, or motivation to quit and a patient's quit counselling modality choice of phone, text, or email. It is currently unknown if these differing service modalities are equally appealing across participant age, gender, and motivation to quit. A more thorough understanding will optimize existing resources and may increase utilization.
2. Methods
Data for this study were collected as part of a randomized controlled trial looking at whether referral to a provincial smoking cessation counselling service would lead to increased 12 month quit rates in an ED population. Data were collected from a single tertiary care academic ED between November 1, 2011 and February 28, 2013. Medically stable patients aged 18 years and older who were able to give informed consent in English and who had used tobacco in the last 30 days were eligible for the study. Patients were ineligible if they lived out-of-province or were unable to provide a telephone number for follow-up. The current analysis includes patients who were randomized to the intervention arm of the trial, and who chose to receive either phone, text, or email counselling services.
Each patient randomized to the intervention arm of the trial received a community counselling service pamphlet, and was offered a brief ED intervention. This intervention consisted of the emergency physician reading the following statements verbatim to the patient, “Quitting smoking is the best thing you can do for your health. We know that many people who visit emergency departments want to quit smoking. [We have a community smoking cessation service that] is free in [our province], and they will help you quit smoking. I would like to refer you to [our community smoking cessation service]”. Patients who accepted referral were asked to choose to be contacted by the community service by phone, text, and/or email. No further information was provided to patients regarding the different modalities of service. Patients who chose to be contacted by phone were contacted by the quitline, and then followed up with a maximum of 8 additional calls by the community service. Patients who chose to be contacted by text were enrolled in the interactive text-based program, and patients who preferred to be contacted by email were sent an email with a link to the community service's website, which includes an interactive forum and access to a chat room monitored by the community service's quit counselors. In cases where the emergency physician did not open the intervention envelopes, research assistants conducted the brief intervention and referral, either in the ED or in a follow-up phone call.
Patient age, gender, motivation to quit, and choice of service (phone, text, or email) were recorded at time of enrolment. Patient motivation to quit was stratified to reflect the transtheoretical model of change (Prochaska et al., 2013). The original baseline responses were re-coded as follows: pre-contemplation (expect to quit never); contemplation (expect to quit someday, or within 6 months); preparation (expect to quit within 1 week to 1 month); and action (currently taking action, or quit for 1 or more weeks).
Continuous variables were described with means ± SD. Categorical variables were summarized using totals and proportions. A one-way analysis of variance was used to examine the association between patient age and quit counselling modality preference. Pearson's chi-squared test of independence was used to determine whether gender or motivation to quit was associated with quit counselling modality preference. All analyses were conducted with Stata 9 (StataCorp, 2005) and p values < 0.05 were considered significant.
3. Results
3.1. Characteristics of study population
In total, 662 ED smokers were randomized to the intervention arm of the randomized controlled trial. Of those who were offered the intervention, 410 (61.9%) accepted referral for smoking cessation counselling. Forty-two (10%) of these participants did not provide a discrete counselling preference and were excluded from the analysis, resulting in a sample size of 368.
Baseline demographics are presented in Table 1. The average age of the study population was 41.7 years (SD = 14.29) and 66.6% of participants were female. With respect to the transtheoretical theory of change, 1.6% of participants were in the pre-contemplation stage, 50.5% were in the contemplation stage, 27.2% were in the preparation stage, and 11.7% of participants were in the action phase.
Table 1.
Baseline demographic characteristics.
| Age in years, mean ± SD | 41.7 ± 14.3 | |
|---|---|---|
| Gender | Male | 123 (33.4%) |
| Female | 245 (66.6%) | |
| Stage of change | Precontemplation | 6 (1.6%) |
| Contemplation | 219 (59.5%) | |
| Preparation | 100 (27.2%) | |
| Action | 43 (11.7%) |
Choice of service modality is presented in Fig. 1. Phone and email counselling were the most frequently selected modalities, with 43.5% and 40.0% of the 368 participants preferring these options respectively. Text counselling was favored by 16.6%.
Fig. 1.
Study participants' choice of smoking cessation counselling modality.
Data were collected from November 2011–February 2013 at Vancouver General Hospital in BC, Canada as part of a randomized-controlled trial (ClinicalTrials.gov, NCT0145437).
3.2. Measures of association
A one-way analysis of variance revealed a significant association between age and counselling modality preference (F (2, 365) = 15.54, p < 0.01). Tukey HSD analyses indicated that the average age of patients who selected text counselling (Mean = 33.6, SD = 10.0) was significantly lower than those who preferred phone counselling (Mean = 45.14, SD = 14.9, p < 0.001) or email counselling (Mean = 41.33, SD = 13.8, p < 0.001). (See Table 2).
Table 2.
Breakdown of service modality choice by age, gender, and motivation to quit.
| Phone | Text | p value | |||
|---|---|---|---|---|---|
| Age | Mean age (95% CI) | 45.1 (42.8–47.5) | 33.6 (31.1–36.2) | 41.3 (39.1–43.6) | < 0.01 |
| Gender | Male (n,%) | 113, 70.6% | 38, 62.3% | 94, 63.9% | < 0.34 |
| Female (n,%) | 47, 29.4% | 23, 37.7% | 53, 36.1% | ||
| Motivation to quit | Precontemplation (n,%) | 3, 1.9% | 2, 3.3% | 1, 0.7% | < 0.47 |
| Contemplation (n,%) | 88, 55.0% | 36, 59.0% | 95, 64.6% | ||
| Preparation (n,%) | 50, 31.3% | 14, 23.0% | 36, 24.5% | ||
| Action (n,%) | 19, 11.9% | 9, 14.8% | 15, 10.2% | ||
Neither gender (χ2 (2, 368) = 2.1, p < 0.34) nor motivation to quit (χ2 (6, 368) = 5.6, p < 0.47) were significantly associated with quit counselling modality choice.
4. Discussion
This is the first ever ED study looking at potential differences in population demographics among those who chose one of three possible counselling service modalities. As telephone, text, and email smoking cessation services become more readily available, it will become increasingly important to be aware of the specific populations that are drawn to these services so programs can be more personalized (Velicer et al., 2006). Personalized self-help materials (Hartmann-Boyce et al., 2014) and tailored web-based interventions (Strecher et al., 2005, Strecher et al., 2008, Te Poel et al., 2009) have been shown to increase quit rates compared to non-personalized interventions.
Each counselling modality has its own benefits. Telephone counselling offers users the opportunity to talk directly with a smoking cessation mentor, and discuss quit strategies in depth. Email and text-based smoking cessation interventions have their own advantages, which include ease of use at any time and place, the ability to send time-sensitive messages, the ability to deliver content that can distract the user from cravings, and greater anonymity compared to phone-based counselling (Chen et al., 2012). Text and email based systems are also less costly and easier to deliver to large populations regardless of location.
In our study, participants who chose the texting service were younger than those who chose the email and phone service. This is not surprising as younger mobile phone users are more likely to send or receive text messages (Canadian Wireless Telecommunication Association, 2011). Internet is fairly ubiquitous, with 82% of Canadians under age 35 and 67% of Canadians over age 65 using Internet at home. We did not find that those who chose the internet service were younger, and this may reflect that our study population was fairly young, with a mean age of 42 years old.
No association was found between gender and choice of service modality. Although descriptively, men are more likely than women to send and receive text messages (96% vs. 91%), own smartphones (51% to 45%), and have a data plan (50% to 45%) (Canadian Wireless Telecommunication Association, 2011), these differences are small. Finally, our study did not find any relationship between motivation to quit and choice of service modality. We had expected that participants who were less motivated to quit may prefer less “invasive” counselling services, and may therefore not have wanted to be phoned. The lack of any difference may reflect a more balanced use and reliance on phone, text, and email as modes of communication among our participants.
Currently, minimal evidence exists for ED smoking cessation counselling. However, more recently, an ED randomized controlled trial found an increased 3 month quit rate in their intervention group compared to controls (12.2% vs 4.9%, 95% CI 3.2%–11.5%) (Bernstein et al., 2015). The intervention group received motivational interviewing, a brochure, nicotine replacement therapy, a referral to a quitline, and a booster call. As community smoking cessation services including quitlines, text support programs, and internet counselling become more commonplace, tailoring programs to participants may increase effectiveness.
5. Limitations
This study was conducted at a single tertiary-care academic emergency department which services a large urban centre. As a result, this study may not be generalizable to all EDs, particularly those in rural areas where cell phone and internet usage rates may differ. Future research incorporating multiple sites is therefore needed to confirm the generalizability of our results. Furthermore, all data were derived from patients recruited into a randomized controlled trial (ClinicalTrials.gov, NCT01454375). As a requirement for enrolment into the trial, participants had to be able to provide consent in English, and to have access to a phone for study investigators to collect follow-up data. As part of this randomized controlled trial, specific baseline demographic factors were collected. However, patient factors including ethnicity, level of education, socioeconomic status, and details of individual phone plans were not collected; all these factors may also affect patient choice of service modality.
6. Conclusions
In our study, over 80% of ED smokers who accepted a referral to our provincial smoking cessation counselling service chose the phone or email modality. The lesser chosen text referral modality was more popular with younger patients. Gender and stage of change did not affect choice of service modality. Incorporating patient preferences and values is considered a key step in developing treatment guidelines and interventions in medicine (Krahn and Naglie, 2008). We hope that these findings will help to inform the development of future smoking cessation programs.
Conflict of interests statement
The authors declare that there are no conflicts of interest.
Acknowledgments
Thanks to the smoking study team at Vancouver General Hospital for their help with data collection.
References
- Bernstein S., Becker B. Preventive care in the emergency department: diagnosis and management of smoking and smoking-related illness in the emergency department: a systematic review. Acad. Emerg. Med. 2002;9(7):720–729. doi: 10.1111/j.1553-2712.2002.tb02153.x. [DOI] [PubMed] [Google Scholar]
- Bernstein S. Successful tobacco dependence treatment in low-income emergency department patients: a randomized trial. Ann. Emerg. Med. 2015;66(2):140–147. doi: 10.1016/j.annemergmed.2015.03.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Canadian Wireless Telecommunication Association Cell phone consumer attitudes study. 2011. http://www.cwta.ca/CWTASite/english/facts_figures_downloads/Consumer2011.pdf [Online] Available at: (Accessed 10 January 2016)
- Chen Y. Effectiveness and cost-effectiveness of computer and other electronic aids for smoking cessation: a systematic review and network meta-analysis. Health Technol. Assess. 2012;16(38):1–205. doi: 10.3310/hta16380. [DOI] [PubMed] [Google Scholar]
- Civljak M. Internet-based interventions for smoking cessation. Cochrane Database Syst. Rev. 2013;7 doi: 10.1002/14651858.CD007078.pub4. [DOI] [PubMed] [Google Scholar]
- Elfeddali I. Preventing smoking relapse via web-based computer-tailored feedback: a randomized controlled trial. J. Med. Internet Res. 2012;14(4):e109. doi: 10.2196/jmir.2057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Free C. Smoking cessation support delivered via mobile phone text messaging (txt2stop): a single-blind, randomised trial. Lancet. 2011;378(9785):49–55. doi: 10.1016/S0140-6736(11)60701-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartmann-Boyce J., Lancaster T., Stead L. Print-based self-help interventions for smoking cessation. Cochrane Database Syst. Rev. 2014;6 doi: 10.1002/14651858.CD001118.pub3. [DOI] [PubMed] [Google Scholar]
- Haug S., Meyer C., John U. Efficacy of an internet program for smoking cessation during and after inpatient rehabilitation treatment: a quasi-randomized controlled trial. Addict. Behav. 2011;36(12):1369–1372. doi: 10.1016/j.addbeh.2011.08.004. [DOI] [PubMed] [Google Scholar]
- Humfleet G., Hall S., Delucchi K., Dilley J. A randomized clinical trial of smoking cessation treatments provided in HIV clinical care settings. Nicotine Tob. Res. 2013;15(8):1436–1445. doi: 10.1093/ntr/ntt005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krahn M., Naglie G. The next step in guideline development: incorporating patient preferences. JAMA. 2008;300:436–438. doi: 10.1001/jama.300.4.436. [DOI] [PubMed] [Google Scholar]
- McBride C., Emmons K., Lipkus I. Understanding the potential of teachable moments: the case of smoking cessation. Health Educ. Res. 2003;18(2):156–170. doi: 10.1093/her/18.2.156. [DOI] [PubMed] [Google Scholar]
- McDonnell D., Kazinets G., Lee H., Moskowitz J. An internet-based smoking cessation program for Korean Americans: results from a randomized controlled trial. Nicotine Tob. Res. 2011;13(5):336–343. doi: 10.1093/ntr/ntq260. [DOI] [PubMed] [Google Scholar]
- North American Quitline Consortium (NAQC) Results from the NACQ annual survey of quitlines. 2011. http://www.naquitline.org/resource/resmgr/2010_survey/0714final2010surveyresults.ppt [Online] Available at: (Accessed 5 January 2016)
- Prochaska J., Norcross J., Diclemente C. Applying the stages of change. Psychother. Austr. 2013;19(2):10–15. [Google Scholar]
- Reid J., Hammond D., Burkhalter R., Ahmed R. Propel Centre for Population Health Impact, University of Waterloo; Waterloo, ON: 2012. Tobacco Use in Canada: Patterns and Trends. [Google Scholar]
- Rhodes K., Gordon J., Lowe R. Preventive care in the emergency department, part I: clinical preventive services–are they relevant to emergency medicine? Acad. Emerg. Med. 2000;7(9):1036–1041. doi: 10.1111/j.1553-2712.2000.tb02097.x. [DOI] [PubMed] [Google Scholar]
- Schroeder S. What to do with a patient who smokes. JAMA. 2005;294(4):482–487. doi: 10.1001/jama.294.4.482. [DOI] [PubMed] [Google Scholar]
- Smit E., Hoving C., Cox V., De Vries H. Influence of recruitment strategy on the reach and effect of a web-based multiple tailored smoking cessation intervention among Dutch adult smokers. Health Educ. Res. 2012;27(2):191–199. doi: 10.1093/her/cyr099. [DOI] [PubMed] [Google Scholar]
- StataCorp . StataCorp LP; College Station, TX: 2005. Stata Statistical Software: Release 9. [Google Scholar]
- Stead L., Bergson G., Lancaster T. Physician advice for smoking cessation. Cochrane Database Syst. Rev. 2008;2 doi: 10.1002/14651858.CD000165.pub3. [DOI] [PubMed] [Google Scholar]
- Stead L., Hartmann-Boyce J., Perera R., Lancaster T. Telephone counselling for smoking cessation. Cochrane Database Syst. Rev. 2013;8 doi: 10.1002/14651858.CD002850.pub3. [DOI] [PubMed] [Google Scholar]
- Stoddard J., Augustson E., Moser R. Effect of adding a virtual community (bulletin board) to smokefree.gov: randomized controlled trial. J. Med. Internet Res. 2008;10(5):e53. doi: 10.2196/jmir.1124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strecher V., Shiffman S., West R. Randomized controlled trial of a web-based computer-tailored smoking cessation program as a supplement to nicotine patch therapy. Addiction. 2005;100(5):682–688. doi: 10.1111/j.1360-0443.2005.01093.x. [DOI] [PubMed] [Google Scholar]
- Strecher V. Web-based smoking-cessation programs: results of a randomized trial. Am. J. Prev. Med. 2008;34:373–381. doi: 10.1016/j.amepre.2007.12.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Te Poel F., Bolman C., Reubsaet A., de Vries H. Health Educ. Res. 2009;24(6):930–940. doi: 10.1093/her/cyp036. [DOI] [PubMed] [Google Scholar]
- Velicer W., Prochaska J., Redding C. Tailored communications for smoking cessation: past successes and future directions. Drug Alcohol Rev. 2006;25:49–57. doi: 10.1080/09595230500459511. [DOI] [PubMed] [Google Scholar]
- Whittaker R. Mobile phone-based interventions for smoking cessation. Cochrane Database Syst. Rev. 2012;11 doi: 10.1002/14651858.CD006611.pub3. [DOI] [PubMed] [Google Scholar]
- World Health Organization . World Health Organization; Geneva: 2011. WHO Report on the Global Tobacco Epidemic: 2011. [Google Scholar]