Abstract
Purpose
To evaluate the surgical outcome of levator resection with suspensory ligament of the superior fornix (SLSF) suspension in severe congenital ptosis with poor levator function (LF).
Patients and methods
The medical records of 25 patients who underwent levator resection with SLSF suspension between March 2011 and January 2013 were retrospectively reviewed. All of the patients had severe congenital ptosis (>4 mm) and poor LF (<4 mm). The follow-up time ranged from 12 to 18 months (median, 15 months). Data regarding eyelid position, cosmetic outcomes, and postoperative complications were evaluated.
Results
The average preoperative margin reflex distance-1 (MRD1) measured −0.30±0.11 mm. The average postoperative MRD1 measured 3.1±1.25 mm at the last follow-up visit. There was a statistically significant difference between preoperative and postoperative MRD1 values (P<0.001). Excellent cosmetic results occurred in 14 patients, good cosmetic results occurred in eight patients and poor cosmetic results did not occur. Three patients (12%) underwent reoperation for residual ptosis. No serious postoperative complications occurred.
Conclusion
Levator resection with SLSF suspension is very effective in the treatment of severe congenital ptosis with poor LF. This surgery technique results in high functional and cosmetic successes in the long term.
Introduction
Surgical correction of severe congenital ptosis with poor levator function (LF) is challenging as undercorrection and poor cosmetic outcome are commonly occurring complications. Frontalis suspension, using autogenous, banked fascia lata or alloplastic materials, is one of the most common methods for the correction of congenital ptosis with poor LF.1 However, many clinical studies have shown that frontalis suspension procedures may cause inflammation, infection, extravasation, extrusion of the suspension material, lid distortion, and unnatural eyelid movement in a superior direction following overaction of the frontalis muscle.1, 2
Epstein et al3 reported that super-maximum levator resection is an effective technique for patients with severe unilateral congenital ptosis. In another study, they found that superior tarsectomy can augment super-maximum levator resection in correction of severe ptosis with poor LF.4 However, many surgeons prefer to avoid removing healthy tarsus given its functional roles in eyelid stability and tear secretion.1
The use of suspensory ligament of the superior fornix (SLSF) for correction of congenital ptosis was described first in 2002 by Holmström and Santanelis.5 They found that creating a link between the SLSF, which contains collagen fibers, elastin fibers smooth muscle fibers,6 and upper lid tarsus allows the SLSF to enable eyelid elevation. Clinical studies showed that SLSF suspension surgery is very effective for correcting eyelid ptosis.7, 8
We used levator aponeurosis, Muller's muscle and SLSF for correction of pediatric congenital ptosis with poor LF. The present study analyzed both functional and cosmetic outcomes of levator resection with SLSF suspension surgery in isolated cases of severe pediatric congenital ptosis.
Materials and methods
This retrospective, observational case series study was conducted at the Nanyang Eye Hospital, Henan, China. The research adhered to the tenets of Declaration of Helsinki for clinical research. This study was approved by the Institutional Review Board (IRB) of Nanyang Eye Hospital, Henan, China. The guardians of all children provided written informed consent for the possible publication of surgical information and eye photos.
Twenty-five well-documented medical records of patients who accepted levator resection with SLSF suspension to treat congenital ptosis with poor LF (<4 mm) between March 2011 and January 2013 were included in this study. Patients with blepharophimosis, Marcus Gunn jaw winking syndrome, myasthenia gravis, negative results of Bell symptom and patients who underwent prior ptosis corrective surgery, followed-up for less than 12 months were excluded from the study.
All patients underwent a complete ophthalmological evaluation, including visual acuity measurement, cycloplegic refraction, observation of Bell phenomenon, assessment for strabismus and amblyopia, and anterior and posterior segment examination. The degrees of ptosis, marginal reflex distance-1 (MRD-1) and LF were determined.
Surgical technique
All surgeries were performed by the same surgeon (HN) under general anesthesia. The intended skin crease was marked on the upper eyelid before local infiltration of 1–2 ml of 1% lidocaine with 1:100000 epinephrine. After a skin incision was created on the upper eyelid, orbicularis oculi muscle was dissected and a small strip of pretarsal orbicularis oculi muscle was excised to expose the anterior surface of the tarsal plate. The orbital septum was cut at its lowest part and the protruding preaponeurotic fat was excised to expose the levator aponeurosis. After the eyelid was everted over a Desmarres retractor, the palpebral conjunctiva was infiltrated with local anesthetic to facilitate the detachment of Mueller's muscle from the conjunctival epithelium by causing the tissues to balloon up slightly. At the superior tarsal border, a vertical incision through the levator aponeurosis and Muller's muscle was creased temporally and nasally. The levator aponeurosis and Muller's muscle were carefully detached from the superior tarsal border and underlying conjunctival epithelium. Dissection was continued to the superior fornix until the smooth, thick and elastic SLSF appeared. The SLSF was then carefully dissected free from the underlying superior rectus muscle. After the horns of the aponeurosis-Muller's muscle and the SLSF were cut, the detached levator aponeurosis-Muller's muscle-SLSF composite flap was advanced and attached onto the anterior surface of the tarsus. Three temporary mattress sutures were placed with 7-0 nylon 2–3 mm inferior to the superior margin of the tarsus. When the lid height and contour were felt satisfactory, temporary knots were tied and the distal redundant portion of the advanced composite flap was trimmed (Figures 1 and 2). After levator aponeurosis Muller's muscle-SLSF composite flap was secured, skin sutures were placed with deep bites taken through the tarsal plate. Patients who required bilateral surgery were operated on simultaneously on both upper eyelids. At surgery, anatomical characteristic of the levator aponeurosis was observed.
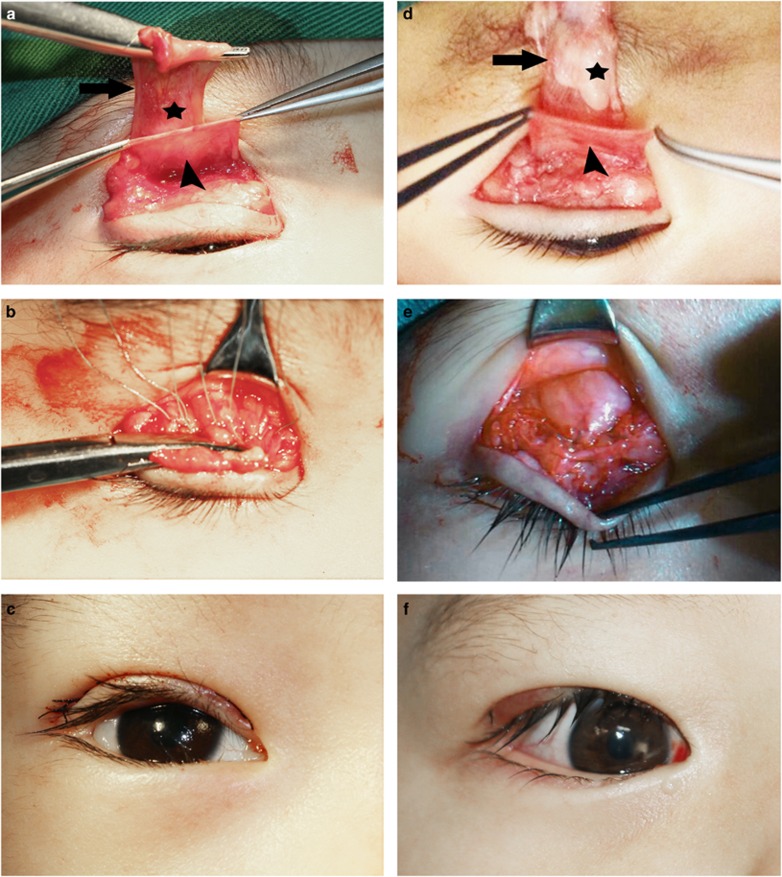
Figure 1.
Photographs of two patients who underwent levator resection and SLSF suspension. (a) Levator aponeurosis was found to be thin and fragile (*). Arrow, levator aponeurosis; arrowhead, SLSF. (d) Fatty degeneration was found in levator aponeurosis (*). Arrow, levator aponeurosis; arrowhead, SLSF. (b, e) Three mattress sutures were placed between the tarsal plate and the levator aponeurosis-SLSF composite flap. (c, f) Postoperative view.
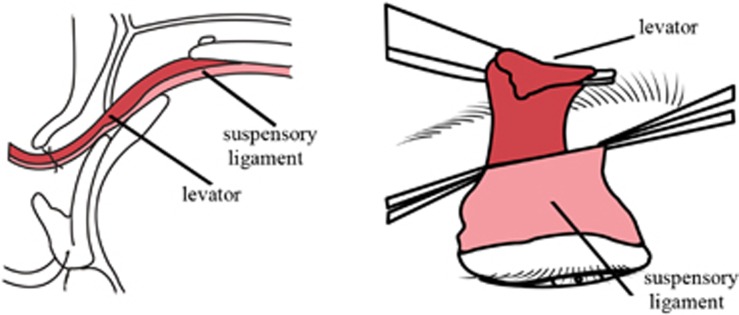
Figure 2.
Schematic view of levator resection with SLSF suspension. (left) Lateral view. (right) Anterior view.
Postoperative evaluation
Postoperative evaluation performed after a minimum follow-up period of 12 months included functional and cosmetic evaluation. In terms of functional evaluation, when the final palpebral superior margins were corrected above the pupillary margin in the primary gaze position without any serious complications, the correction was classified as functional success. In terms of cosmetic evaluation, symmetry of lid height, lid contour, and lid crease were graded as excellent, good, or poor by three masked observers, as has been described previously.2 Cosmetic results were judged as excellent when eyelid position achieved functional success at last follow-up visit, with good eyelid contour and crease, and asymmetry between both upper eyelid was <1 mm. The cosmetic outcome was defined as good if there was >1 mm or ≤2 mm difference in eyelid height or one of the three parameters (symmetry of lid height, lid contour, and lid crease) was not satisfactory. The cosmetic outcome was defined as poor if there was >2 mm difference in eyelid height or two of three parameters (symmetry of lid height, lid contour, and lid crease) were not satisfactory. The frequency of complications was also evaluated.
Statistical analysis
The Fisher exact test was performed to evaluate the cosmetic outcome at the last visit. Student's t-test was performed to evaluate the changes in degree of ptosis, MRD-1 and LF. The P-values <0.05 were considered statistically significant.
Results
Twenty-five patients (16 males and nine females, mean 3.6 years) underwent levator resection with SLSF suspension for severe congenital ptosis, 15 patients had bilateral surgery, and overall 40 surgeries were performed. Demographic characteristics of the study population are summarized in Table 1. The mean follow-up time was 15±1.6 months (range 12–18 months).
Table 1. Demographics of 25 patients (40 eyelids) with severe congenital ptosis who underwent levator resection with SLSF suspension with a minimum of 12 months of follow-up.
| Unilateral | Bilateral | |
|---|---|---|
| No.of patients | 10 | 15 |
| Age at operation (years) | 3.5 (range, 2–7) | 3.7 (range, 2–7) |
| Male gender (%) | 7 (70%) | 9 (60%) |
| Follow-up (mo, mean±SD) | 14±2.1 | 15.0±3.2 |
| Strabismus (no. of patients) | 5 (50%); XT (4), ET (1) | 3 (20%); XT (2), ET (1) |
| Amblyopia (no. of patients) | 8 | 7 |
| Gross anatomical defect of levator aponeurosis | ||
| Thin and fragile | 6 | 10 |
| Fatty degeneration | 4 | 5 |
Abbreviations: ET, esotropia; SLSF, suspensory ligament of the superior fornix; XT, exotropia.
Eight patients had strabismus on the ptosis eye. In two patients, strabismus was corrected before levator resection with SLSF suspension. Amblyopia was identified in 15 patients, visual acuities improved after the surgery with amblyopia therapy in nine patients at last follow-up visit.
At surgery, levator aponeurosis was found to be thin and fragile in 16 patients. Fatty degeneration in levator aponeurosis was found in nine patients (Table 1).
One week after surgery, the functional success rates were 100%. However, three patients (three eyelids) showed undercorrection at the 1-month follow-up visit and the functional success rates decreased to 88%. Reoperation was performed in these patients for residual ptosis with further advancement of the composite flap at 6 months after the first surgery. Two patients had a good result 12 months after the reoperation. One patient who underwent reoperation had a recurrence of ptosis even after his second procedure. Six out of 10 (60%) unilateral cases showed excellent cosmetic outcomes and two (20%) showed good outcomes at the last follow-up visit. In contrast, excellent cosmetic outcomes were achieved in eight out of 15 bilateral cases (53.3%) and good outcomes were achieved in six cases (40%) (Figure 3). There was significant difference between the unilateral and bilateral ptosis groups in cosmetic success rates (8/10, 80.0%, vs 14/15, 93.3%, respectively, P<0.05) (Table 2).
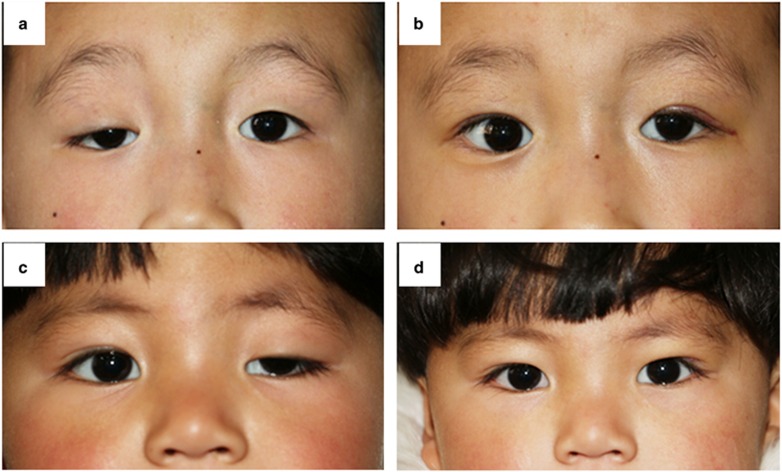
Figure 3.
(a) Preoperative photograph of 4-year-old boy with right eyelid congenital ptosis. (b) Photograph of the same patient 12 months after levator resection with SLSF suspension. Cosmetic outcome was graded as good because asymmetry between both upper eyelids was <2 mm with natural eyelid contour and crease. Note that the left upper eyelid dropped slightly at 12 months. This change in the position of left upper eyelid may be due to the integral role of levator muscle innervation in the definition of Hering's law. (c) Preoperative photograph of 5-year-old girl with left-eyelid congenital ptosis. (d) Photograph of the same patient 15 months after levator resection with SLSF suspension. Cosmetic outcome was graded as excellent because asymmetry between both eyelids was <1mm with natural eyelids contour and crease.
Table 2. Cosmetic outcomes of levator resection with SLSF suspension in patients with poor levator function at last follow-up visit.
| Unilateral | Bilateral | |
|---|---|---|
| Cosmetic outcomes (no. of patients) | ||
| Excellent | 6 | 8 |
| Good | 2 | 6 |
| Reoperation | 2 | 1 |
Abbreviation: SLSF, suspensory ligament of the superior fornix.
Preoperative and at postoperation degree of ptosis, MRD-1 and LF changes are shown in Table 3. Treatment reduced eyelid ptosis from preoperative 5.52±0.23 (range, 8.20–4.12 mm) mm to 2.20±1.23 mm (range, 3.21–0.13 mm) at last visit (P<0.01). The preoperative MRD1 of −0.30±0.11 mm (range, −3.2 to+1.2 mm) increased to 3.10±0.22 mm (range, −2.3 to 4.3 mm) at last follow-up visit (P<0.001).The mean preoperative LF was 2.61±1.60 mm (range, 3.11–0.22 mm), which increased to 4.32±1.21 mm (range, 6.28–2.17 mm) (P<0.01) (Table 3).
Table 3. Preoperative and last visit data in 40 cases operated for eyelid ptosis by levator resection with SLSF suspension.
| Data (mm) | Preoperative | Last visit | P |
|---|---|---|---|
| Degree of ptosis | 5.52±0.23 | 2.20±1.23 | <0.01 |
| MRD-1 | −0.30±0.11 | 3.10±0.22 | <0.001 |
| LF | 2.61±1.60 | 4.32±1.21 | <0.01 |
Abbreviations: LF, levator function; MRD-1, marginal reflex distance-1; SLSF, suspensory ligament of the superior fornix.
All patients had early incomplete eyelid closure, which resolved at 1 month after surgery. Six patients presented exposure keratopathy at 1 week after surgery, which was well managed with lubricants. No other postoperative complications such as overcorrection, wound infection, upper eyelid entropion, or conjunctival prolapse were found in the follow-up period.
Discussion
Various surgical techniques have been developed for the treatment of pediatric congenital ptosis with poor LF. However, undercorrection and poor cosmetic outcomes are still commonly occurring complications. The surgical technique of levator resection with SLSF suspension has been used for 5 years in our department for correction of severe pediatric congenital ptosis. In the present study, the surgical results were reviewed with regard to 40 eyelids of 25 consecutive cases of severe pediatric congenital ptosis. We have shown that this surgcal technique is very effective in the treatment of severe congenital ptosis with poor LF.
The frontalis suspension procedures using autogenous fascia lata, banked fascia lata, or synthetic materials, forming a connection between the frontalis muscle and the tarsus of the upper eyelid have been shown to be very effective for correcting severe congenital ptosis with poor LF1. Simon et al9 evaluated ptosis recurrence rate of frontalis suspension surgery with a variety of suture materials. They found that autogenous fascia and polytetrafluoroethylene resulted in a lower recurrence rate. Although autogenous fascia lata has been considered an ideal suture material because of its lasting effects, a recent study has found that cosmetic outcomes of frontalis suspension surgery with autogenous fascia lata can deteriorate over time, even when functional outcomes remain consistently good.2
The most common cause of congenital ptosis is levator dysgenesis.10, 11 The obvious advantage of levator resection for correction of congenital ptosis is the ability to customize the amount of eyelid elevation and producing natural elevating motion of the physiological eyelid in a superior-posterior direction.4, 12 In a comparative study of direct frontalis transfer vs levator resection, it has been shown that levator resection can be used to treat ptosis patients with poor LF as effectively as direct frontalis transfer.13 In the same study, it has been noted that direct frontalis transfer surgery predisposed patients to more severe complications, both esthetically and functionally. Epstein and Putterman3 described super-maximum resection of levator for correction of congenital ptosis with poor LF (<4 mm). In another study, they reported that super-maximum levator resection alone resulted in 70% incidence of substantial undercorrection, whereas in the eyes treated with super-maximum levator resection with superior tarsectomy, the incidence of substantial undercorrection was reduced to 12.5%.4 However, removal of normal tarsal tissue may damage tarsal stability and tear secretion.
The SLSF has been used to correct eyelid ptosis.5, 7 It has been shown that suspension of the eyelid to the SLSF is quite successful in raising the level of the upper eyelid in congenital ptosis.5 In the present study, we selected to combine SLSF suspension with the levator resection. To our knowledge, this is the first reported consecutive series examining the effects of SLSF on the ptosis corrective ability of the levator resection for cases of severe congenital ptosis with poor LF.
We evaluated ptosis after treatment with levator resection with SLSF suspension. The mean postoperative ptosis of eyelids was 2.20±1.23 mm compared with a mean preoperative ptosis of 5.52±0.23 mm (P<0.01). The average preoperative MRD-1 measured −0.30±0.11 mm, the average postoperative MRD-1 measured 3.10±0.22 mm at last follow-up visit (P<0.001). The recurrence rate was low (12%). Cosmetic outcomes regarding lid contour, symmetry, and lid crease were very successful at last follow-up visit. In addition, no serious complications were found during the follow-up period. Taken together, this study has demonstrated that simultaneous advancement of the levator aponeurosis, Muller's muscle, and SLSF composite as flap can produce stronger power to correct severe pediatric congenital ptosis.
We assessed the change in LF after levator resection with SLSF suspension. The result showed that the mean preoperative LF was 2.61±1.60 mm, which increased postoperatively to 4.32±1.21 mm at the last visit (P<0.01). Göncü et al14 evaluated the surgical outcome of levator resection in congenital ptosis. They found that levator resection resulted in substantial improvement of postoperative levator muscle functioning. They suggested that improvement of LF may have an additive effect on the surgical success, especially for those with poor LF. Our results support this observation.
In summary, the results of this retrospective study demonstrate that levator resection with SLSF suspension is very effective in treatment of severe congenital ptosis with good functional and cosmetic outcomes.
Acknowledgments
This work was supported by grants from the National Natural Science Foundation of China (NSFC no 81470660), the Xiamen Science and Technology Plan Projects (no 3502Z20131017 and no 3502Z20159017) and the Natural Science Foundation of Fujian Province of China (no 2015-ZQN-ZD-34 and 2016D13). The research received no specific grant from any funding agency in the public, commercial or not for profit sector.
The authors declare no conflict of interest.
References
- SooHoo JR, Davies BW, Allard FD, Durairaj VD. Congenital ptosis. Surv Ophthalmol 2014; 59(5): 483–492. [DOI] [PubMed] [Google Scholar]
- Lee SY, Yonn JS. Long-term functional and cosmetic outcomes after frontalis suspension using autogenous fascia lata for pediatric congenital ptosis. Ophthalmology 2009; 116: 1405–1414. [DOI] [PubMed] [Google Scholar]
- Epstein GA, Putterman AM. Super-maximum levator resection for severe unilateral congenital blepharoptosis. Ophthalmic Surg 1984; 15: 971–979. [PubMed] [Google Scholar]
- Putterman AM, Shields M, Pak J. Superior tarsectomy augment super-maximum levator resection in correction of severe blepharoptosis with poor levator function. Ophthalmology 2006; 113: 1201–1208. [DOI] [PubMed] [Google Scholar]
- Holmström H, Santanelis F. Suspension of the eyelid on the check ligament of the superior for congenital blepharoptosis. Scand J Plast Reconstr Surg Hand Surg 2002; 36: 149–156. [DOI] [PubMed] [Google Scholar]
- Holmström H, Bernström-Lundberg C, Oldfors A. Anatomical study of the structures at the roof of the orbit with the special reference to the check ligament of the superior fornix. Scand J Plast Reconstr Surg Hand Surg 2002; 36: 157–159. [DOI] [PubMed] [Google Scholar]
- Santanelli F, Paolini G, Renzi LF, Longo B, Pagnoni M, Holmström H. Correction of myopathic blepharoptosis by check ligamentsuspension: Clinical evaluation of 89 eyelids. J Plast Surg Hand Surg 2011; 45: 194–199. [DOI] [PubMed] [Google Scholar]
- Pan E, Zhang Y, Li L, Shen SY, Wang XY, Wang HY et al. [Check ligament suspension for correction of congenital severe blepharoptosis]. Zhonghua Zheng Xing Wai Ke Za Zhi 2011; 27: 253–256. [PubMed] [Google Scholar]
- Simon B, Macedo AA, Schwacz RM, Wang DY, McCann JD, Goldberg RA. Frontalis suspension for upper eyelid ptosis: evaluation of different surgical designs and suture material. Am J Ophthalmol 2005; 140: 877–885. [DOI] [PubMed] [Google Scholar]
- Edmunds B, Manners RM, Weller PO, Steart P, Collin JR. Levator palpebrae superioris fibre size in normal and patients with congenital ptosis. Eye 1998; 12: 47–50. [DOI] [PubMed] [Google Scholar]
- Baldwin HC, Manners RM. Congenital blepharoptosis: a literature review of the histology of levator palpebrae superioris muscle. Ophthal Plast Reconstr Surg 2002; 18: 301–307. [DOI] [PubMed] [Google Scholar]
- Baik BS, Ha W, Lee JW, Ji SY, Yang WS, Park D et al. Adjunctive techniques to traditional advancement procedures for treatement severe blepharoptosis. Plast Reconstr Surg 2014; 133: 887–896. [DOI] [PubMed] [Google Scholar]
- Pak DH, Choi WS, Yoon SH, Shim JS. Comparison of levator resection and frontalis muscle transfer in the treatment of severe blepharoptosis. Ann Plast Surg 2007; 59: 388–392. [DOI] [PubMed] [Google Scholar]
- Göncü T, Cakmak S, Akal A, Karaismailoğlu E. Improvement in levator function after anterior levator resection for the treatment of congenital ptosis. Ophthal Plast Reconstr Surg 2015; 31: 197–201. [DOI] [PubMed] [Google Scholar]