Abstract
Background:
Dengue is an infectious disease associated with high mortality and morbidity. Being a viral disease, there is no specific drug available for treatment. There are some reports that Carica papaya leaf extract may improve the clinical condition of dengue patients; however, to support this, at present, there is no systematically searched and synthesized evidence available.
Objectives:
This systematic review and meta-analysis was designed to search the available evidence related to the efficacy and safety of C. papaya leaf extract in dengue and to synthesize the evidence in meaningful form through meta-analysis so that inference can be drawn.
Materials and Methods:
Randomized controlled trials related to the efficacy and safety of C. papaya leaf extract in dengue were searched from PubMed, Cochrane Clinical Trial Registry and Google Scholar. The primary endpoint was mortality, and secondary endpoints were increase in platelet count, hospitalization days, and Grade 3 and 4 adverse events. Data related to primary and secondary endpoints were pooled together and analyzed by review manager (Review Manager (RevMan) Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, Denmark) software. The random effect model was used. The bias was analyzed by the Cochrane risk of bias tool.
Results:
Total four trials enrolling 439 subjects were included in the analysis. Of 439 subjects, data of 377 subjects were available for analysis. C. papaya leaf extract was found to be associated with increase in platelet count in the overall analysis (mean difference [MD] =20.27 [95% confidence interval (CI) 6.21–34.73; P = 0.005]) and analysis after 4th day (MD = 28.25 [95% CI 14.14–42.37; P < 0.0001]). After 48 h, there was no significant difference between C. papaya and control group (MD = 13.38 [95% CI − 7.71–34.51; P = 0.21]). There was significant decrease in hospitalization days in the C. papaya group (MD = 1.90 [95% CI 1.62–2.18; P < 0.00001]). Because of nonavailability of data in published clinical trials, mortality, and adverse events cannot be pooled.
Conclusion:
C. papaya leaf extract can be considered as a potential candidate for increase in platelet count in patients of dengue, however; there is need of high-quality evidence in the form of large clinical trials before a decision related to the use of such extract is made.
Key words: Dengue hemorrhagic fever, platelets, thrombocytopenia, vascular leakage
INTRODUCTION
Dengue is an acute infectious disease caused by mosquito and associated with significant mortality and morbidity.[1] Today about 50% of the world's population, live in areas which are endemic for dengue transmission, and around 125 countries are endemic for the same.[2] Globally, around 50–200 million dengue infection, 500,000 episodes of severe dengue, and 20,000 dengue-related deaths are reported annually.[3] The incidence and prevalence of dengue infection are expected to increase in future because of changes in climate, travel, socioeconomic status, trade, and viral characteristics.[3] There is 40% risk of contracting dengue if one resides in the endemic area and out of these, only 0.5% has risk of developing a serious form of the disease. Clinically, dengue causes moderately high-grade fever, rash with severe aches, mostly severe backache, and pain behind the eyes. Following this, there is an apparent phase of improvement and in severe forms symptoms such as vomiting, pain in the abdomen, red spots, reduction in urine output, change in alertness, and bleeding can occur. The red flag sign, citing the severity in serious dengue is a fluid leak from blood vessels and capillaries from the nose, gums, skin, lung vessels, intra-abdominal areas, etc.[4]
Bleeding of variable severity is seen mainly in the severe form of dengue, i.e., dengue hemorrhagic fever. Pathogenesis of bleeding involves leakage of plasma from the blood vessels. It seems to be due to the destruction of platelets through complement system or depression of bone marrow due to dengue viral infection or both. It is also observed that platelets that escape from the destruction become nonfunctional or less functional.[5,6,7] Direct correlation between platelet count and prognosis of dengue is reported in many published studies.[5,6,8,9,10]
With the recent outbreak of dengue in India, there has reportedly been a sudden increase in the demand for papaya leaves juice across India. The print media, social network, and national media have started coming up with opinion pieces, news items, and blogs on the use of papaya in the treatment of dengue which was instantly taken up by the community due to its perceived beneficial effect on the platelet count.[11] Literature cites the therapeutic effects of aqueous extract of papaya (Carica papaya) leaves that are presumed to be due to several active components (flavonoids, alkaloids, enzymes, and minerals) which may have antioxidant and immunomodulatory effects.[12,13,14,15]
With the outpouring of above information, there was a need of systematic search and analysis of available evidence as a guideline for the use of papaya in the treatment of dengue; hence, this systematic review was planned to explore the efficacy and safety of C. papaya in dengue.
MATERIALS AND METHODS
Outcomes
The primary outcome was the comparison of mortality between C. papaya and control. Secondary outcomes included platelet counts, hospitalization time, and adverse events.
Search methods and identification of studies
A systematic search was performed in PubMed, Cochrane Clinical Trial Registry, and Google Scholar [Appendix 1]. References of published articles were hand searched to find new studies exploring the efficacy and safety of C. papaya in dengue.
Study selection
Randomized controlled trials exploring the role of C. papaya compared with any comparator for patients of dengue and dengue shock syndrome were eligible for inclusion. Case reports and observational studies were not included in the analysis. Two review authors (Jaykaran Charan and Deepak Saxena) assessed titles and abstracts followed by full text (using predefined inclusion criteria) independently. For any disagreement decision of third author (Jagdish Prasad Goyal) was considered final.
Data collection and analysis
Data extraction and management
Two review authors (Jaykaran Charan and Deepak Saxena) extracted the data from included trials using a standardized data extraction form independently. Data were collected on study characteristics, patient characteristics, treatment characteristics, risk of bias using Cochrane risk of bias tool, and outcome data (mortality, platelet counts, hospitalization time, adverse events, etc.).
Statistical analysis
Continuous data were summarized as mean difference (MD) and standardized MD (SMD) with 95% confidence interval (CI). The unit of MD was × 103/µl. In case of one clinical trial, the standard deviation of one follow-up parameter (increase in platelet count) was not given. On the basis of standard deviation of other parameter of same study and parameters of other studies, it was observed that there was not much difference in standard deviation between baseline and follow–up; hence, for that study (Yunita et al.), we considered follow-up standard deviation (SD) same as baseline SD during analysis results of Yunita et al. was given as subgroup to clarify the effect of this study on overall results. Dichotomous data was summarized as risk ratio (RR) with 95% CI. Random effect model was used for the analysis. Heterogeneity was calculated using I2 values. We set predecided criteria for significant heterogeneity (I2 > 50%).
We did not asses the publication bias as there were only four trials fulfilling the inclusion criteria, which were too less for assessing the publication bias. Review Manager version 5.3 software (Cochrane Collaboration) was used for analysis. This review was performed as per the standards of Cochrane Collaboration and reported as per PRISMA standards.[16]
RESULTS
Study characteristics
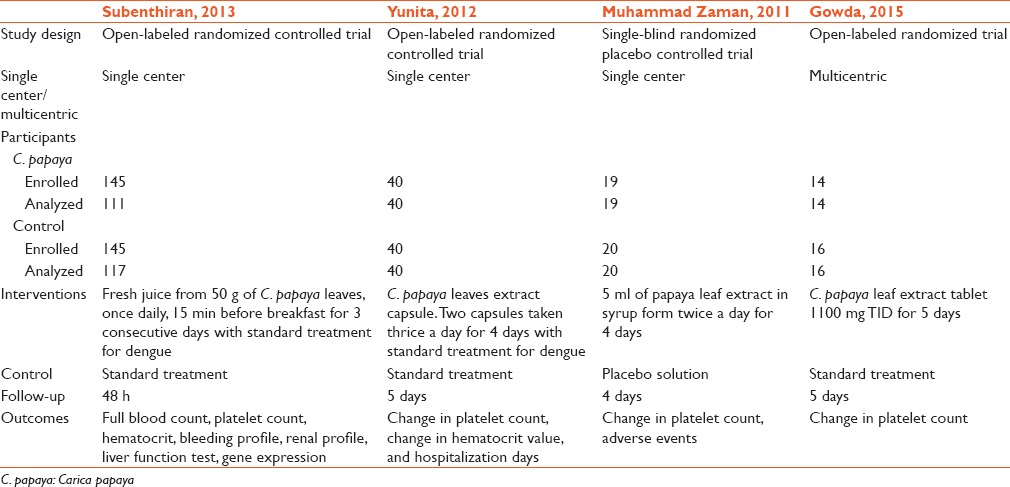
There were total four trials included in the analysis.[13,17,18,19] Step by step method of inclusion and exclusion of studies is depicted in Figure 1. All studies were single-center randomized trials, except one which was multicentric. No trial was double-blind. Only one trial was placebo controlled trial, and in rest, standard treatments were considered as control. C. papaya was used by the different method in each trial. In one trial, it was used as leaf extract juice, in the second trial, it was used as leaf extract tablet and in remaining two trials, it was used as leaf extract capsule and leaf extract syrup, respectively. Follow-up was not same in all trials. It was 2 days, 5 days, 4 days, and 5 days, respectively [Table 1].
Figure 1.
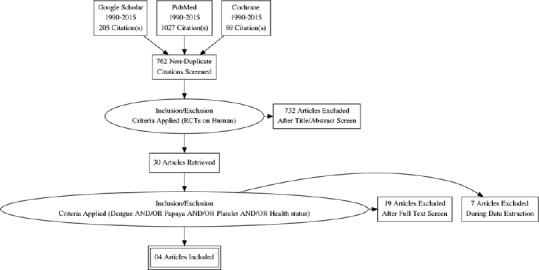
PRISMA chart
Table 1.
Study characteristics
Assessment of bias
Many of the parameters needed for the assessment of the risk of bias were not reported in these trials. As none of the trials was double-blinded; hence, there is a chance of bias, but at the same time, endpoints such as platelet counts are objective parameters; hence, incorporation of the bias by open labeling of the trial may not significantly affect the result [Figure 2].
Figure 2.
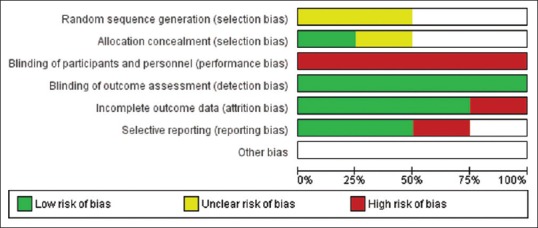
Risk of bias graph
Efficacy of intervention
Mortality
Data on mortality were not given in any trial; hence, the analysis could not be done for the primary endpoint.
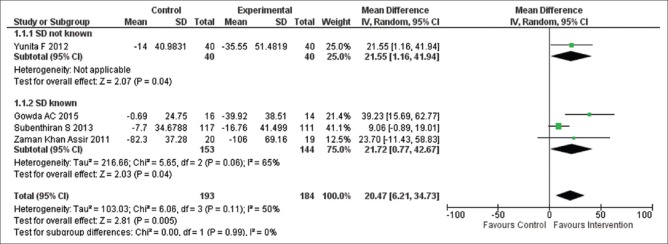
Change in platelet count for all follow-ups
Data were extracted from the four clinical trials (377 subjects) [Figure 3].[13,17,18,19] C. papaya compared with control was associated with a statistically significant increase in platelet count (MD = 20.27 [95% CI 6.21–34.73; P = 0.005]). There was significant heterogeneity (I2 = 50%). Similar results were obtained after excluding Yunita et al. [Figure 3]. Same results were obtained for the (SMD = 0.46 [95% CI 0.13–0.78; P = 0.006], I2 = 45%).
Figure 3.
Efficacy of Carica papaya on platelet count (mean difference) for all follow-ups
In the case of number of subjects whose platelet count reach to normal range, the data were extractable from only one study enrolling total 39 patients.[18] There was no significant difference between C. papaya and control for the subjects whose platelet count reached to the normal level (RR = 0.53, 95% CI 0.22–1.29; P = 0.16).
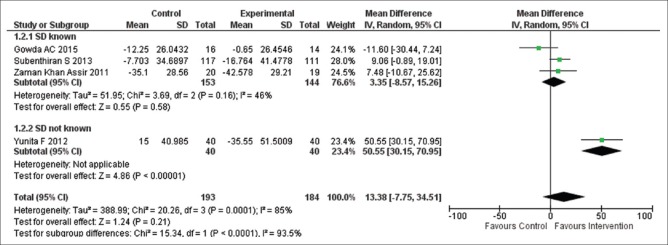
Change in platelet count after 48 h
Data were extracted from the four clinical trials (377 subjects) [Figure 4].[13,17,18,19] There was no significant difference in rise in platelet count between C. papaya and control (MD = 13.38 [95% CI − 7.71–34.51; P = 0.21]). There was significant heterogeneity between subgroups (I2 = 85%). On excluding Yunita et al. from the analysis MD and CI range got decreased, but the difference was still insignificant [Figure 4] and heterogeneity disappeared. Same results were obtained for the (SMD = 0.32 [95% CI − 0.21–0.86; P = 0.23], I2 = 79%).
Figure 4.
Efficacy of Carica papaya on platelet count (mean difference) after 48 h
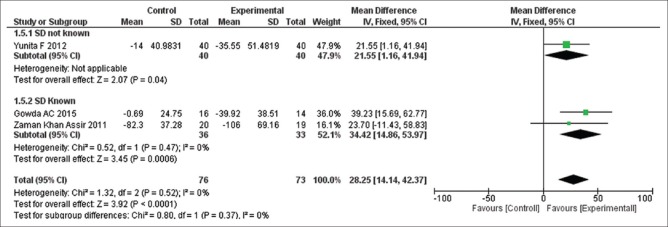
Change in platelet count after 4 days
Data were extracted from three clinical trials (149 subjects) [Figure 5].[17,18,19] C. papaya administration was significantly associated with increase in platelet count as compared to the control (MD = 28.25 [95% CI 14.14–42.37; P < 0.0001]). There was no heterogeneity observed (I2 = 0%), and similar results were obtained for the (SMD = 0.58 [95% CI 0.25–0.91; P < 0.0006], I2 = 31%).
Figure 5.
Efficacy of Carica papaya on platelet (mean difference) after 4 days
Hospitalization days
Data for this endpoint was extractable from one study enrolling total eighty subjects.[17] C. papaya was significantly associated with decrease in hospitalization days as compared to control (MD = 1.90 [95% CI 1.62–2.18; P < 0.00001]).
Safety of intervention
Adverse events
There were no specific data given about adverse events in the published studies. In two studies, it was mentioned that there were no significant adverse events observed in both intervention and control groups.[13,18]
DISCUSSION
On the basis of this review it can be summarized that C. papaya is significantly associated with the increase in platelet counts in the patients of dengue. The results are consistent even after excluding (Yunita et al. 2012) study in which standard deviation of platelet counts was not given in follow-up. Data related to the mortality and adverse events were not available.
The most important finding of this systematic review is increase in platelet count was significantly more in C. papaya group as compared to the control group. Platelet count is not considered among the criteria for severe dengue and considered as warning sign only as per the WHO guidelines; however, studies supported the predictive ability of platelet count for the severity of dengue.[8,20] Platelet count also correlates with vascular leakage of proteins and liver damage.[21] The major pathophysiological hallmark which determines dengue severity is vascular leakage.[22] Therefore, thrombocytopenia might be an important predictor of mortality. There was a modest rise in the platelet count in this review with wider CIs in all analysis which indicates inconsistency in the results. There are very few studies available, regarding actual mechanism of beneficial effect of C. papaya leaf extract in dengue. In a “in vitro” study by Ranasinghe et al., the C. papaya leaf extract found to be associated with the improvement of erythrocyte membrane stabilization.[23] A study done by bioinformatics methods found that flavonoids of C. papaya leaf extract can inhibit a protease involved in viral assembly.[14] The leaf extract of C. papaya has antioxidant and free radical scavenging property which can help in the prevention of hemolysis and bleeding.[24]
This is so far best available evidence for the use of C. papaya in dengue patients. Majority of the parameters, through which bias can be evaluated were not reported in these clinical trials. In the absence of these information authenticity of the results obtained in these clinical trials cannot be considered free of bias. However, platelet count is a laboratory parameter and not a subjective criteria; hence, chances of any bias due to open label nature of trials is less. These trials were conducted in Asian countries where the prevalence of dengue fever is high, so the results of these trials cannot be applied to other countries and people with different genetic makeups.
CONCLUSION
On the basis of this systematic review and meta-analysis, it can be concluded that C. papaya leafs extract has a definitive role in improving the platelet count in patients of dengue. Looking at the wider CI, the rise in platelet count may be very less and may not be clinically significant. There is a statistically significant positive effect on the rise of platelet count, but whether this rise is clinically significant or not? That can be explored further by designing high-quality clinical trials based on large sample size with all measures to prevent incorporation of bias.
Implications for practice
On the basis of this study, the use of C. papaya in dengue cannot be suggested as data of safety was not properly measured and reported in the included clinical trials. The rise in platelet count may also be too less to affect the outcome. More evidence needed in the form of well-designed clinical trials before a decision on the use of C. papaya leaf extract are made.
Implications for research
There are good indications that intervention may be useful in dengue patients; hence, the role of C. papaya leaf extract should be explored further through better designed clinical trials.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
APPENDIX 1
Steps for Search
Step-1: Dengue*
Step-2: “Dengue Fever”
Step-3: “Dengue” AND “treatment”
Step-4: “Dengue” AND “treatment” [ti/ab]
Step-5: “ Dengue” OR “Dengue fever” AND “treatment” [ti/ab] AND/OR “Papaya”
Step-6: “ Dengue” OR “Dengue fever” AND “treatment” OR “management” OR “health status” [ti/ab] AND/OR “Papaya”
Step-7: “ Dengue” OR “Dengue fever” AND “treatment” OR “management” OR “health status” [ti/ab] AND/OR “Papaya” AND Randomized Controlled Trial [ptyp]
REFERENCES
- 1.Guzmán MG, Kourí G. Dengue: An update. Lancet Infect Dis. 2002;2:33–42. doi: 10.1016/s1473-3099(01)00171-2. [DOI] [PubMed] [Google Scholar]
- 2.Gubler DJ. Dengue, urbanization and globalization: The unholy trinity of the 21st century. Trop Med Health. 2011;39(4 Suppl):3–11. doi: 10.2149/tmh.2011-S05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Murray NE, Quam MB, Wilder-Smith A. Epidemiology of dengue: Past, present and future prospects. Clin Epidemiol. 2013;5:299–309. doi: 10.2147/CLEP.S34440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ho TS, Wang SM, Lin YS, Liu CC. Clinical and laboratory predictive markers for acute dengue infection. J Biomed Sci. 2013;20:75. doi: 10.1186/1423-0127-20-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Makroo RN, Raina V, Kumar P, Kanth RK. Role of platelet transfusion in the management of dengue patients in a tertiary care hospital. Asian J Transfus Sci. 2007;1:4–7. doi: 10.4103/0973-6247.28065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Krishnamurti C, Kalayanarooj S, Cutting MA, Peat RA, Rothwell SW, Reid TJ, et al. Mechanisms of hemorrhage in dengue without circulatory collapse. Am J Trop Med Hyg. 2001;65:840–7. doi: 10.4269/ajtmh.2001.65.840. [DOI] [PubMed] [Google Scholar]
- 7.de Azeredo EL, Monteiro RQ, de-Oliveira Pinto LM. Thrombocytopenia in dengue: Interrelationship between virus and the imbalance between coagulation and fibrinolysis and inflammatory mediators. Mediators Inflamm. 2015;2015:313842. doi: 10.1155/2015/313842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jayashree K, Manasa GC, Pallavi P, Manjunath GV. Evaluation of platelets as predictive parameters in dengue fever. Indian J Hematol Blood Transfus. 2011;27:127–30. doi: 10.1007/s12288-011-0075-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Noisakran S, Chokephaibulkit K, Songprakhon P, Onlamoon N, Hsiao HM, Villinger F, et al. A re-evaluation of the mechanisms leading to dengue hemorrhagic fever. Ann N Y Acad Sci. 2009;1171(Suppl 1):E24–35. doi: 10.1111/j.1749-6632.2009.05050.x. [DOI] [PubMed] [Google Scholar]
- 10.Potts JA, Gibbons RV, Rothman AL, Srikiatkhachorn A, Thomas SJ, Supradish PO, et al. Prediction of dengue disease severity among pediatric Thai patients using early clinical laboratory indicators. PLoS Negl Trop Dis. 2010;4:e769. doi: 10.1371/journal.pntd.0000769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jha DN. Doctors Unsure but Papaya a Hit for Dengue Treatment. The Times of India. 2015 Sep 16; [Google Scholar]
- 12.Sarala N, Paknikar S. Papaya extract to treat dengue: A novel therapeutic option? Ann Med Health Sci Res. 2014;4:320–4. doi: 10.4103/2141-9248.133452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Subenthiran S, Choon TC, Cheong KC, Thayan R, Teck MB, Muniandy PK, et al. Carica papaya leaves juice significantly accelerates the rate of increase in platelet count among patients with dengue fever and dengue haemorrhagic fever. Evid Based Complement Alternat Med. 2013;2013:616737. doi: 10.1155/2013/616737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Senthilvel P, Lavanya P, Kumar KM, Swetha R, Anitha P, Bag S, et al. Flavonoid from Carica papaya inhibits NS2B-NS3 protease and prevents dengue 2 viral assembly. Bioinformation. 2013;9:889–95. doi: 10.6026/97320630009889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dharmarathna SL, Wickramasinghe S, Waduge RN, Rajapakse RP, Kularatne SA. Does Carica papaya leaf-extract increase the platelet count? An experimental study in a murine model. Asian Pac J Trop Biomed. 2013;3:720–4. doi: 10.1016/S2221-1691(13)60145-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. Ann Intern Med. 2009;151:W65–94. doi: 10.7326/0003-4819-151-4-200908180-00136. [DOI] [PubMed] [Google Scholar]
- 17.Yunita F, Hanani E, Kristianto J. The effect of Carica papaya L. leaves extract capsules on platelets count and hematocrit level in dengue fever patient. Int J Med Aromat Plants. 2012;2:573–8. [Google Scholar]
- 18.Assir MZ, Nasir NU, Mansoor H, Waseem T, Ahmed HI, Riaz F, et al. Effect of Carica papaya leaf extract on platelet count in dengue fever: A randomized controlled tirals (PLEAD TRIAL) J Allama Iqbal Med Coll. 2011;9:6–9. [Google Scholar]
- 19.Gowda A, Kumar NV, Kasture P, Sr, Nagabhushan K. A pilot study to evaluate the effectiveness of Carica papaya leaf extract in increasing the platelet count in cases of dengue with thrombocytopenia. Indian Med Gaz. 2015;3:109–16. [Google Scholar]
- 20.WHO Dengue: Guideline for Diagnosis, Treatment, Prevention and Control: World Health Organization. 2009. [Last cited on 2015 Oct 09]. Available from: http://www.whqlibdoc.who.int/publications/2009/9789241547871_eng.pdf . [PubMed]
- 21.Mourão MP, Lacerda MV, Macedo VO, Santos JB. Thrombocytopenia in patients with dengue virus infection in the Brazilian Amazon. Platelets. 2007;18:605–12. doi: 10.1080/09537100701426604. [DOI] [PubMed] [Google Scholar]
- 22.Srichaikul T, Nimmannitya S. Haematology in dengue and dengue haemorrhagic fever. Baillieres Best Pract Res Clin Haematol. 2000;13:261–76. doi: 10.1053/beha.2000.0073. [DOI] [PubMed] [Google Scholar]
- 23.Ranasinghe P, Ranasinghe P, Abeysekera WP, Premakumara GA, Perera YS, Gurugama P, et al. In vitro erythrocyte membrane stabilization properties of Carica papaya L. leaf extracts. Pharmacognosy Res. 2012;4:196–202. doi: 10.4103/0974-8490.102261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Okoko T, Ere D. Reduction of hydrogen peroxide-induced erythrocyte damage by Carica papaya leaf extract. Asian Pac J Trop Biomed. 2012;2:449–53. doi: 10.1016/S2221-1691(12)60074-4. [DOI] [PMC free article] [PubMed] [Google Scholar]