Abstract
Context:
Better understanding of the anatomical location and course of the mandibular canal is necessary to avoid damaging inferior alveolar nerve.
Aims:
The aim of this study was to investigate the buccolingual course of the inferior alveolar canal (IAC) in different mental foramen locations, using cone beam computed tomography.
Materials and Methods:
Three hundred and twelve hemimandibular images were evaluated in this study. The location of mental foramen in relation to the apices of mandibular premolar and molar teeth were recorded. Nine measurements (in millimeters) were taken at the level of the IAC and posterior mandibular premolar and molar root apices. Relative distances of IAC to buccal and lingual mandibular cortex were calculated for different mental foramen types.
Statistical Analysis Used:
Data were analyzed by one-way analysis of variance and P < 0.05 was considered to be statistically significant.
Results:
The distribution of subjects according to the type of mental foramen includes: Type 1 = 50.3% (at the level of second premolar apex), Type 2 = 33% (between the apices of first and second premolars), and Type 3 = 16.7% (between the apices of second premolars and first molars). The buccolingual ratio of the IAC position was statistically significant in different mental foramen types (P = 0.00).
Conclusion:
The position of IAC was affected by the location of the mental foramen. The direction of IAC gradually changed from lingual to buccal and from posterior to anterior.
Key words: Buccolingual, cone beam computed tomography, inferior alveolar canal, Iranian
INTRODUCTION
Entrance into the inferior alveolar canal (IAC) is one of the most serious complications during surgical procedures of the mandible.[1,2,3,4] To avoid this problem, a better understanding of the anatomical location and course of the mandibular canal before surgery is recommended.[1,2,3,4,5,6,7] One of the predicting factors of IAC course is the location of mental foramen.[8]
Cone beam computed tomography (CBCT) has been introduced as a three-dimensional (3D) imaging modality in the recent decades. The information obtained through the CBCT around specific area is reconstructed in the axial, sagittal, coronal planes and also panoramic and cross-sectional views.[7,8,9,10,11] Having less exposure than computed tomography (CT), CBCT can be considered as an ideal imaging modality for maxillofacial diagnosis.[7,8,9,10,11,12] This CBCT study evaluates the course of IAC, in different mental foramen location in a selected Iranian population.
MATERIALS AND METHODS
CBCT images of patients from June 2012 to May 2014, who underwent CBCT scan for different dental purposes were enrolled in this study. A database of 1840 hemimandibular CBCT scans was searched; 312 hemimandibular images with acceptable quality that conformed to inclusion and exclusion criteria were selected for the study. Inclusion criteria were: (1) The presence of the first and second premolars and molars and (2) those CBCT scans that contained the entire IAC. Exclusion criteria consisted of any pathology (radiolucencies that might represent cyst and tumor or periapical lesion), fracture, supernumerary, or impacted teeth in ROI, which might alter the IAC course or obscure visualization. Anatomic measurements were made by an experienced oral and maxillofacial radiologist.
CBCT scans were taken with NewTom VGi Scanner (NewTom QR srl, Verona, Italy) in standard resolution mode (110 kV, voxel size = 0.3 mm and with field of view ≥6 cm × 6 cm). The image acquisition protocol consisted of 360° rotation of the C-arm with an X-ray tube and a flat panel detector. The scans were viewed and measured using the NNT software version 4.0 (NewTom QR srl, Verona, Italy) supplied by the manufacturer and viewed on a flat-panel color active matrix TFT Medical Display (Nio Color 3 MP, Barco, Kortrijk, Belgium) 27 inch diagonally, with 1280 × 1024 pixel screen resolution. The volumes were displayed with a 0.3 mm thickness and 1 mm intervals. All volumes were standardized in the same orientation, with the sagittal plane parallel to the IAC and the coronal plane perpendicular to the IAC.
Panoramic reconstruction views of the volume studies were created in 5.1 mm thickness. Then, 1 mm thickness cross-sectional cuts from the interested region were produced. Nine measurements (in millimeters) were taken at the level of the IAC and mandibular premolar and molar root in cross-sectional cuts [Figure 1]. These measurements included: P2-L, M1-L, and M2-L, which were the distance between the outer margin of the lingual cortical plate and the center of the IAC at the level of the second premolar apex, median point of two root apices of first molar, and median point of two root apices of second molar, respectively; P2-B, M1-B, and M2-B, which were the distance between the outer margin of buccal cortical plate and the center of the IAC at the level of the second premolar apex, median point of two root apices of the first molar, and median point of two root apices of the second molar, respectively; P2-Width, M1-Width, and M2-Width, which were the total buccolingual width of mandibular body along the center of IAC at the level of the second premolar apex, median point of two root apices of the first molar, and median point of two root apices of second molar, respectively; P2-ratio(P2-B/P2width), M1-ratio(M1-B/M1-width), and M2-ratio(M2-B/M2-width) which are the relative buccolingual position of the IAC in mandibular body at the level of the second premolar apex, median point of two root apices of first molar and median point of two root apices of second molar, respectively, calculated by (P2-B/P2-width, M1-B/M1-width, M2-B/M2-width). Scans were randomly selected as to whether the right side or the left side was used for a single patient.
Figure 1.

Reformatted panoramic image providing reference for multiple narrow transaxial thin cross-sectional slices (a). Cross-sectional images of mandibular arch at the second premolar apex (b), median point of two root apices of the first molar (c) and median point of two root apices of the second molar (d)
Data were statistically analyzed using SPSS software (version 15.0 for Windows, Chicago, IL, USA). Descriptive statistics for each variable were calculated. The differences in each variable with respect to mental foramen type were tested with one-way analysis of variance between groups. P < 0.05 was considered to be statistically significant.
RESULTS
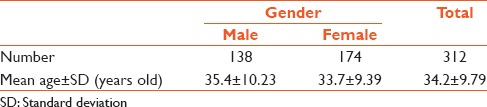
According to the inclusion and exclusion criteria, 312 hemimandibular CBCT images were enrolled in this study. The descriptive statistics of the study subjects are presented in Table 1. Mean age of all subjects was 34.2 (standard deviation: 9.79) ranging from 20 to 49. Of the 312 hemimandibular images analyzed, 138 belonged to males and 174 belonged to females.
Table 1.
Descriptive of the study subjects
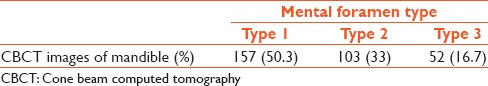
The results of mental foramen classification by anteroposterior position were - of the 312 mental foramens, 157 were Type 1, at the level of second premolar apex (50.3%) and 103 were Type 2, between the apices of the first and second premolars (33%) and 52 were Type 3, between the apices of the second and first molar (16.7%). The distribution of mental foramen types is shown in Table 2.
Table 2.
Frequency of mental foramen type
Detailed measurements of buccolingual position of IAC are presented in Table 3. Buccolingual ratio of IAC according to different mental foramen types were stated in Table 4. Buccolingual ratios were found to be significantly different between different mental foramen types.
Table 3.
Detailed measured distances according to mental foramen types

Table 4.
Buccolingual ratio of inferior alveolar canal according to mental foramen type

DISCUSSION
CBCT imaging has been introduced as a 3D imaging modality in the recent decades. Information can be obtained through the cone beam around a specific area and is reconstructed in the axial, sagittal, and coronal planes.[7,8,9,10,11] In addition, the information can be reconstructed in panoramic and cross-sectional views. Another notable feature of CBCT is the ability to correct magnification and perform precise measurements on the reconstructed information. Having less exposure than CT, CBCT can be considered as an ideal imaging modality for maxillofacial diagnosis.[7,8,9,10,11,12]
The vertical course of mandibular canal can be observed in routine panoramic radiography; the buccolingual course was emphasized in this study. All subjects in this study were of Iranian origin and therefore represented a very ethnically homogenous group. Evaluation of the location of the mental foramen regarding the mandibular posterior teeth in this study showed that the most common types of mental foramens were Type 1 (which was located below the apex of the second premolar) (50.31%) and Type 2 (which was located between the apices of the first and second premolars) (33%) and were in agreement with the results of Singh and Srivastav,[10] Genu et al.,[13] Pokhrel and Bhatnagar et al.,[14] Fujita and Suzuki,[15] Afkhami et al.,[16] Udhaya et al.,[17] Adejuwon et al.,[18] and Yesilyurt et al.'s[19] studies on different ethnic populations. On the other hand in other studies,[20,21,22] the most common positions of the mental foramen were reported to be Type 2 followed by Type 1. However, in all these studies, the Type 1 and Type 2 mental foramina had two top frequencies. The slight differences in the same population could be explained using different imaging techniques. Panoramic radiography provides a flat image of a curved structure and is not as accurate as CBCT in the horizontal localization of objects, especially in the premolar region.[23] Based on green's study, the relative position of the mental foramen to the mandibular teeth could be affected by the mesiodistal size of the teeth and attrition of their proximal surfaces.[24] In addition, Yesilhurt et al.[19] theorized that these differences might be due to the difference in dietary habits that affect the development of the mandible.
In the present study, the mean distances from the center of IAC to the buccal and lingual cortex of the mandible and also the buccal to lingual mandibular cortex distance along the IAC was measured at the level of the second premolar, first and second molar. The mean distance between the outer buccal and lingual cortex of the mandible along the IAC increased from the second premolar to the second molar region and the maximum value was at the second molar area. Regarding the anatomy of mandibular body, this finding would be expected. In this study, all the mandibular buccolingual distances were greater for males without exception. However, this difference was not statistically significant between both sexes. This finding is in accordance with Balaji et al.'s study.[25]
According to the results of this study, the greatest distance, from IAC to the buccal cortex existed at the second molar region, where the lingual distances in some cases reached zero. The maximum values of the buccal distances were reported at the second molar region, in the studies by Balaji et al.[25] Nagadia et al.,[26] Al-Siweedi et al.,[27] and Shokri et al.[28] The results of this study also showed that buccal distances increased significantly from the second premolar to the second molar region while lingual distances decreased. This is similar to the results of various studies.[7,25,26,27,28,29,30] Balaji et al.[25] reported no statistically significant difference in mean values of buccal and lingual distances between both sexes and different age groups, whereas Levine et al. suggested that the buccolingual position of IAC was age-related.[6] In all these studies, the mean buccal and lingual distances were measured to be less than those of this study. This difference could be due to different reference points. In the current study, the distance between buccal/lingual cortexes of the mandible of the IAC was measured, whereas in other studies, buccal/lingual borders of the IAC were used for measurements.
In the current study, the relative buccolingual position of the mandibular canal was calculated as 0.83, 0.71, and 0.53 at the second molar, first molar, and second premolar regions, respectively. This showed that the IAC progresses from the lingual to the buccal side clearly, from the second molar to the second premolar region. In Pyun et al.'s[2] study, this ratio was 0.68, 0.64, and 0.47, respectively, but the change in direction from the lingual to the buccal side was less prominent from the second molar to the first molar. The studies of Simonton et al.[4] and Balaji et al.[25] were also evaluated and the buccolingual ratios from their average measurements were calculated. In Balaji et al.'s[25] study, this ratio was 0.30 and 0.31 at the first and second molar regions, respectively. Their ratios were dramatically less than that of the present study (0.71 and 0.83) because they used the inner buccal cortex of the mandible and buccal border of the IAC. However, this result indicates a gradual change in the course of IAC from lingual to buccal, when it comes to the anterior of the mandible. The study of Simonton et al.[4] calculated the buccolingual ratio of the IAC position, as 0.61 and 0.66 at the mesial and distal roots of the first molar, respectively.[2,25]
This study also found that in the buccolingual dimension, in many cases, the IAC was near or in contact with the lingual cortex and in some cases, the lingual distance reached to zero. Another important finding of this study is the relationship between the location of mental foramen and the buccolingual position of the IAC. At all regions (second premolar, first molar, and second molar), the more distally the mental foramen was located, the more buccally the IAC progressed in the mandibular body. In Pyun et al.'s[2] study, this was true just about the second premolar region. In the current study, the minimum values for the buccolingual ratio of the canal at all regions were found in Type 1 (in which the mental foramen was located below the second premolar). In this type of mental foramen, the second premolar region seems to be subjected to high risk of damage to the inferior alveolar nerve during implant placements or endodontic surgeries.
CONCLUSION
Based on the CBCT findings of this study, there was a relation between the buccolingual position of the IAC and the location of the mental foramen. In the first type of mental foramen, the most common type, buccolingual ratio of IAC was equal to 0.45 at the second premolar region. This is where the IAC, approximately passes through half the distance between the buccal and lingual mandibular cortex.
The general course of the IAC changes smoothly from lingual to buccal from the mandibular second molar to the second premolar and exits from the mental foramen, at the buccal part of the mandible bone. The horizontal location of the mental foramen which was seen in routine radiographs such as panoramic would be helpful for surgeons to estimate the risk of inferior alveolar nerve injury, even before using advanced imaging techniques such as CBCT.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The authors would like to thank Mr. M.H. Ahmadie for his help with statistical design and analysis.
REFERENCES
- 1.Angelopoulos C, Thomas SL, Hechler S, Parissis N, Hlavacek M. Comparison between digital panoramic radiography and cone-beam computed tomography for the identification of the mandibular canal as part of presurgical dental implant assessment. J Oral Maxillofac Surg. 2008;66:2130–5. doi: 10.1016/j.joms.2008.06.021. [DOI] [PubMed] [Google Scholar]
- 2.Pyun JH, Lim YJ, Kim MJ, Ahn SJ, Kim J. Position of the mental foramen on panoramic radiographs and its relation to the horizontal course of the mandibular canal: A computed tomographic analysis. Clin Oral Implants Res. 2013;24:890–5. doi: 10.1111/j.1600-0501.2011.02400.x. [DOI] [PubMed] [Google Scholar]
- 3.Starkie C, Stewart D. The intra-mandibular course of the inferior dental nerve. J Anat. 1931;65(Pt 3):319–23. [PMC free article] [PubMed] [Google Scholar]
- 4.Simonton JD, Azevedo B, Schindler WG, Hargreaves KM. Age- and gender-related differences in the position of the inferior alveolar nerve by using cone beam computed tomography. J Endod. 2009;35:944–9. doi: 10.1016/j.joen.2009.04.032. [DOI] [PubMed] [Google Scholar]
- 5.Scarfe WC, Farman AG, Sukovic P. Clinical applications of cone-beam computed tomography in dental practice. J Can Dent Assoc. 2006;72:75–80. [PubMed] [Google Scholar]
- 6.Levine MH, Goddard AL, Dodson TB. Inferior alveolar nerve canal position: A clinical and radiographic study. J Oral Maxillofac Surg. 2007;65:470–4. doi: 10.1016/j.joms.2006.05.056. [DOI] [PubMed] [Google Scholar]
- 7.Ozturk A, Potluri A, Vieira AR. Position and course of the mandibular canal in skulls. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012;113:453–8. doi: 10.1016/j.tripleo.2011.03.038. [DOI] [PubMed] [Google Scholar]
- 8.Worthington P. Injury to the inferior alveolar nerve during implant placement: A formula for protection of the patient and clinician. Int J Oral Maxillofac Implants. 2004;19:731–4. [PubMed] [Google Scholar]
- 9.Katakami K, Mishima A, Shiozaki K, Shimoda S, Hamada Y, Kobayashi K. Characteristics of accessory mental foramina observed on limited cone-beam computed tomography images. J Endod. 2008;34:1441–5. doi: 10.1016/j.joen.2008.08.033. [DOI] [PubMed] [Google Scholar]
- 10.Singh R, Srivastav AK. Study of position, shape, size and incidence of mental foramen and accessory mental foramen in Indian adult human skulls. Int J Morphol. 2010;28:1141–6. [Google Scholar]
- 11.Agthong S, Huanmanop T, Chentanez V. Anatomical variations of the supraorbital, infraorbital, and mental foramina related to gender and side. J Oral Maxillofac Surg. 2005;63:800–4. doi: 10.1016/j.joms.2005.02.016. [DOI] [PubMed] [Google Scholar]
- 12.Mraiwa N, Jacobs R, Moerman P, Lambrichts I, van Steenberghe D, Quirynen M. Presence and course of the incisive canal in the human mandibular interforaminal region: Two-dimensional imaging versus anatomical observations. Surg Radiol Anat. 2003;25:416–23. doi: 10.1007/s00276-003-0152-8. [DOI] [PubMed] [Google Scholar]
- 13.Genu PR, de Hollanda Vasconcellos RJ, de Oliveira BP, de Vasconcellos BC, da Cruz Delgado NC. Analysis of anatomical landmarks of the mandibular interforaminal region using CBCT in a Brazilian population. Braz J Oral Sci. 2014;13:303–7. [Google Scholar]
- 14.Pokhrel R, Bhatnagar R. Position and number of mental foramen in dry human mandibles: Comparison with respect to sides and sexes. OA Anat. 2013;1:31. [Google Scholar]
- 15.Fujita A, Suzuki T. Computed tomographic analysis of the mental foramen and nerve in Japanese patients. Implant Dent. 2014;23:471–6. doi: 10.1097/ID.0000000000000105. [DOI] [PubMed] [Google Scholar]
- 16.Afkhami F, Haraji A, Boostani HR. Radiographic localization of the mental foramen and mandibular canal. J Dent (Tehran) 2013;10:436–42. [PMC free article] [PubMed] [Google Scholar]
- 17.Udhaya K, Saraladevi KV, Sridhar J. The morphometric analysis of the mental foramen in adult dry human mandibles: A study on the South Indian population. J Clin Diagn Res. 2013;7:1547–51. doi: 10.7860/JCDR/2013/6060.3207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Adejuwon SA, Akinlosotu F, Omowunmi M, Salawu OT. Variations in the mandibular foramina of Yoruba ethnic group of Nigeria. J Med Sci. 2012;12:188–92. [Google Scholar]
- 19.Yesilyurt H, Aydinlioglu A, Kavakli A, Ekinci N, Eroglu C, Hacialiogullari M, et al. Local differences in the position of the mental foramen. Folia Morphol (Warsz) 2008;67:32–5. [PubMed] [Google Scholar]
- 20.Amorim MM, Borini CB, de Castro Lopes SL, Haiter-Neto F, Caria PH. Morphological description of mandibular canal in panoramic radiographs of Brazilian subjects: Association between anatomic characteristic and clinical procedures. Int J Morphol. 2009;27:1243–8. [Google Scholar]
- 21.Chen Z, Chen D, Tang L, Wang F. Relationship between the position of the mental foramen and the anterior loop of the inferior alveolar nerve as determined by cone beam computed tomography combined with mimics. J Comput Assist Tomogr. 2015;39:86–93. doi: 10.1097/RCT.0000000000000166. [DOI] [PubMed] [Google Scholar]
- 22.Neiva RF, Gapski R, Wang HL. Morphometric analysis of implant-related anatomy in Caucasian skulls. J Periodontol. 2004;75:1061–7. doi: 10.1902/jop.2004.75.8.1061. [DOI] [PubMed] [Google Scholar]
- 23.Khojastepour L, Mirbeigi S, Mirhadi S, Safaee A. Location of mental foramen in a selected Iranian population: A CBCT assessment. Iran Endod J. 2015;10:117–21. [PMC free article] [PubMed] [Google Scholar]
- 24.Green RM. The position of the mental foramen: A comparison between the Southern (Hong Kong) Chinese and other ethnic and racial groups. Oral Surg Oral Med Oral Pathol. 1987;63:287–90. doi: 10.1016/0030-4220(87)90191-5. [DOI] [PubMed] [Google Scholar]
- 25.Balaji SM, Krishnaswamy NR, Kumar SM, Rooban T. Inferior alveolar nerve canal position among South Indians: A cone beam computed tomographic pilot study. Ann Maxillofac Surg. 2012;2:51–5. doi: 10.4103/2231-0746.95319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nagadia R, Tay AB, Chan LL, Chan ES. The spatial location of the mandibular canal in Chinese: A CT study. Int J Oral Maxillofac Surg. 2011;40:1401–5. doi: 10.1016/j.ijom.2011.07.904. [DOI] [PubMed] [Google Scholar]
- 27.Al-Siweedi SY, Nambiar P, Shanmuhasuntharam P, Ngeow WC. Gaining surgical access for repositioning the inferior alveolar neurovascular bundle. ScientificWorldJournal. 2014;2014:719243. doi: 10.1155/2014/719243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Shokri A, Shakibaei Z, Langaroodi AJ, Safaei M. Evaluation of the mandibular canal visibility on cone-beam computed tomography images of the mandible. J Craniofac Surg. 2014;25:e273–7. doi: 10.1097/SCS.0000000000000654. [DOI] [PubMed] [Google Scholar]
- 29.Massey ND, Galil KA, Wilson TD. Determining position of the inferior alveolar nerve via anatomical dissection and micro-computed tomography in preparation for dental implants. J Can Dent Assoc. 2013;79:d39. [PubMed] [Google Scholar]
- 30.Nair UP, Yazdi MH, Nayar GM, Parry H, Katkar RA, Nair MK. Configuration of the inferior alveolar canal as detected by cone beam computed tomography. J Conserv Dent. 2013;16:518–21. doi: 10.4103/0972-0707.120964. [DOI] [PMC free article] [PubMed] [Google Scholar]


