Dear Sir,
Dengue is a viral infection caused by an arbovirus of the Flaviviridae family. Epidemics frequently occur in tropical and subtropical countries, and it is a grave public health problem. It may present in many forms. The most common classical form of dengue causes fever, myalgias, headache, nausea, vomiting, diarrhea, arthralgia, and rash lasting for a week. Dengue hemorrhagic fever is a severe form of the disease that can progress to severe hemorrhagic manifestations, hypovolemic shock, and death. Various neurologic complications of dengue viral infection have been reported, including central and peripheral nervous system involvement. Encephalopathy, encephalitis, seizures, mononeuropathy, polyneuropathy, and Guillain–Barré or Miller–Fisher syndromes have been seen. However, spinal cord involvement associated with dengue viral infection has been rarely mentioned.[1,2]
An 8-month-old male child presented with fever for 3 days. Initial complete blood counts showed severe anemia and thrombocytopenia, and the blood sample was positive for IgM antibody of dengue. Five days later, the child developed areflexia along with urinary retention and bowel incontinence and severe respiratory distress. On examination, the pupils were sluggishly reactive, and there was no response to pain. There were generalized petechiae in both lower limbs. Other systems were completely normal. Other laboratory parameters showed mildly raised liver enzymes and normal blood sugar, electrolytes, and kidney function tests. Serologic testing for malaria, typhoid, HIV, and syphilis were negative. Due to the acute presentation of the bowel and bladder dysfunction, magnetic resonance imaging of the spinal cord was done, which showed diffuse hyperintensity on T2-Weighted and short tau inversion recovery images extending from C4 level up to the termination of spinal cord [Figure 1a]. There was also formation of syrinx above the C4 level [Figure 1b]. On postcontrast images, there was mild patchy enhancement of the spinal cord at C4 and C5 levels [Figure 1c].
Figure 1.
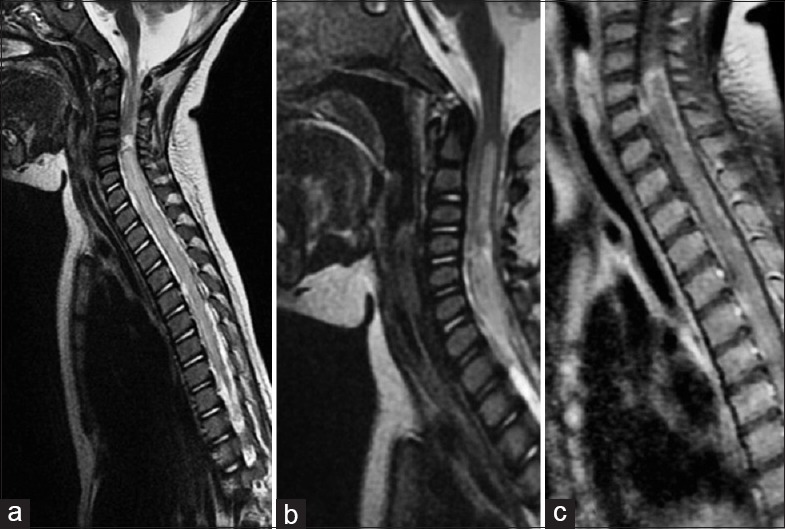
(a and b) Sagittal T2 weighted images showing diffuse hyperintensity in spinal cord extending from c4 (1a) and syrinx above c4 (1b). (c) Sagittal T1 weighted post contrast images showing patchy enhancement in cord
On the basis of imaging findings, a diagnosis of diffuse acute transverse myelitis with syringohydromyelia in association with dengue viral infection was made. Due to severe respiratory distress, the child was given ventilatory support, and intravenous (IV) methylprednisolone was started. After 6 days of ventilatory support, the child improved. Hence, gradually, he was extubated and after that he recovered well.
In the past few years, numerous neurological complications related to dengue fever have been reported, and these can lead to a significant morbidity and mortality. Neurological complications occur in 0.5–6% of the cases with dengue fever.[3] Dengue encephalopathy could be caused by cerebral edema, cerebral hemorrhage, hyponatremia, hypoxia, renal and hepatic insult. Acute myelitis as a consequence of dengue fever is a rare phenomenon and has been published through anecdotal case reports. Transverse myelitis is a clinical syndrome, which can be associated with a number of different conditions. It is, therefore, necessary to identify a direct infection, a systemic disease, or an autoimmune (postinfectious or postvaccinal) process.[4] The clinical picture includes partial or complete paraplegia or quadriplegia, decrease or loss of deep reflexes, sensory impairment, and varying degrees of bladder and bowel disturbance. Usually, the full-blown disease is reached within 4 weeks after onset, but in most cases, the peak occurs in the 1st week with the level of involvement set at the onset.[5] In a few patients, however, the disease has an ascending course with the risk of asphyxia when the upper cervical segments (C3–C5) are involved. In the present case, the onset was sudden and the upper cervical spinal cord was immediately involved. Early diagnosis of the condition and early initiation of corticosteroid treatment are very important as it results in rapid recovery.[4] Timely diagnosis and treatment of the condition with IV corticosteroids decreases mortality and morbidity and favors good outcome as seen in our case.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Renganathan A, Keong W, Tin TC. Transverse myelitis in association with dengue infection. Neurol J Southeast Asia. 1996;1:61–3. [Google Scholar]
- 2.Leão RN, Oikawa T, Rosa ES, Yamaki JT, Rodrigues SG, Vasconcelos HB, et al. Isolation of dengue 2 virus from a patient with central nervous system involvement (transverse myelitis) Rev Soc Bras Med Trop. 2002;35:401–4. doi: 10.1590/s0037-86822002000400018. [DOI] [PubMed] [Google Scholar]
- 3.Hendarto SK, Hadinegoro SR. Dengue encephalopathy. Acta Paediatr Jpn. 1992;34:350–7. doi: 10.1111/j.1442-200x.1992.tb00971.x. [DOI] [PubMed] [Google Scholar]
- 4.Lahat E, Pillar G, Ravid S, Barzilai A, Etzioni A, Shahar E. Rapid recovery from transverse myelopathy in children treated with methylprednisolone. Pediatr Neurol. 1998;19:279–82. doi: 10.1016/s0887-8994(98)00065-4. [DOI] [PubMed] [Google Scholar]
- 5.Solomon T, Dung NM, Vaughn DW, Kneen R, Thao LT, Raengsakulrach B, et al. Neurological manifestations of dengue infection. Lancet. 2000;355:1053–9. doi: 10.1016/S0140-6736(00)02036-5. [DOI] [PubMed] [Google Scholar]


