Abstract
Background and objectives
Conservative management of adults with stage 5 CKD (eGFR<15 ml/min per 1.73 m2) is increasingly being provided in the primary care setting. We aimed to examine perceived barriers and facilitators for conservative management of older adults by primary care physicians.
Design, setting, participants, & measurements
In 2015, we conducted a cross–sectional, population–based survey of all primary care physicians in Alberta, Canada. Eligible participants had experience caring for adults ages ≥75 years old with stage 5 CKD not planning on initiating dialysis. Questionnaire items were on the basis of a qualitative descriptive study informed by the Behavior Change Wheel and tested for face and content validity. Physicians were contacted via postal mail and/or fax on the basis of a modified Dillman method.
Results
Four hundred nine eligible primary care physicians completed the questionnaire (9.6% response rate). The majority of respondents were men (61.6%), were ages 40–60 years old (62.6%), and practiced in a large/medium population center (68.0%). The most common barrier to providing conservative care in the primary care setting was the inability to access support to maintain patients in the home setting (39.1% of respondents; 95% confidence interval, 34.6% to 43.6%). The second most common barrier was working with nonphysician providers with limited kidney–specific clinical expertise (32.3%; 95% confidence interval, 28.0% to 36.7%). Primary care physicians indicated that the two most common strategies that would enhance their ability to provide conservative management would be the ability to use the telephone to contact a nephrologist or clinical staff from the conservative care clinic (86.9%; 95% confidence interval, 83.7% to 90.0% and 85.6%; 95% confidence interval, 82.4% to 88.9%, respectively).
Conclusions
We identified important areas to inform clinical programs to reduce barriers and enhance facilitators to improve primary care physicians’ provision of conservative kidney care. In particular, primary care physicians require additional resources for maintaining patients in their home and telephone access to nephrologists and conservative care specialists.
Keywords: Kidney Failure, Chronic; Therapeutics; Geriatrics; nephrology; Physicians, Primary Care; Surveys and Questionnaires; Conservative Care; Non-dialysis Care; geriatric nephrology; Adult; Alberta; Canada; Cross-Sectional Studies; Empathy; Humans; Male; Postal Service; Prevalence; Primary Health Care; renal dialysis; Renal Insufficiency, Chronic; Specialization; Telefacsimile; Telephone
Introduction
International clinical practice guidelines recommend that patients with eGFR of <30 ml/min per 1.73 m2 be referred to a nephrologist (1). However, in the interest of patient-centered care, referral may not always be necessary, and it will not always be a feasible option. For instance, the majority of patients with stage 5 CKD (eGFR<15 ml/min per 1.73 m2 or G5 category in CKD) (1) who are managed without RRT (i.e., conservative care) are older people (age ≥75 years old) (2), and their routine care is often provided by primary care physicians without seeing a nephrologist (2).
There are distinct conservative care populations: conservative kidney care, choice–restricted conservative care, and unrecognized G5 CKD (3). In this study, we focus on conservative kidney care: nondialysis management that is chosen or medically advised. Ideally, conservative kidney management involves a multidisciplinary team that provides symptom management, advance care planning, and psychologic support (3). Although primary care physicians are key health care providers for conservative care for older adults with kidney disease, there is a paucity of research regarding the barriers and facilitators of their clinical practice.
This study was part of a sequential and exploratory mixed methods study (4). The findings reported from a prior qualitative descriptive study identified barriers and strategies to enhancing conservative care by primary care physicians (5). These findings directly contributed to the development of the questionnaire examined in this paper. In the prior study, we found that primary care physicians’ perceived barriers to care included management of patient/family expectations, the complexity of medical management (especially challenges regarding the management of multimorbidity), and challenges arising from comanagement of patients with specialists. Respondents suggested that direct telephone access to conservative care experts, treatment decision aids, and a conservative care clinical pathway would be helpful to them. Building on this prior work, we sought to determine the prevalence of perceived barriers and facilitators to improving primary care physicians’ ability to conservatively manage older adults with stage 5 CKD who were not planning to initiate dialysis.
Materials and Methods
Study Participants
We undertook a population–based, cross–sectional survey of all primary care physicians (4521 family physicians or general practitioners) registered with the provincial regulatory College of Physicians and Surgeons of Alberta, Canada (6). Physicians were eligible for the study if they self-reported having provided care for adults ages ≥75 years old with stage 5 CKD who did not intend to initiate dialysis.
Questionnaire Development and Administration
Details regarding questionnaire development and survey administration are reported elsewhere (7). In brief, the questionnaire (Supplemental Appendix) included 32 questions. The major sections of the questionnaire focused on barriers to conservative care, facilitators to improving care, and demographic and clinical practice characteristics. Questionnaire items were informed by interviews with primary care physicians who had experience caring for the population of interest and the Behavior Change Wheel (8,9). The Behavior Change Wheel incorporates a theoretical system with three components for understanding behavior, namely capacity, opportunity, and motivation (the COM-B system), and the Theoretical Domains Framework for behavioral change and implementation research (10). All domains of the framework were reviewed, and three were identified as the most relevant COM-B components: psychological capability (knowledge skills), physical opportunity (opportunity afforded by the environment; e.g., resources), and reflective motivation (reflective processes involving plans/actions caused by beliefs about positive/negative outcome expectations) (9). Four nephrologists, one geriatrician, three primary care physicians, and 14 health services researchers evaluated the questionnaire for face and content validity (11). The feedback received from the evaluations comprised minor modifications that were incorporated, which improved the clarity and organization of the questionnaire.
After receipt of ethical approval from the Conjoint Health Research Ethics Board at the University of Calgary, primary care physicians were contacted between September and October of 2015 on the basis of contact information available from the provincial regulatory College of Physicians and Surgeons of Alberta. Using a modified Dillman method (12) with a sequential mixed mode approach (13), these physicians were contacted and expected to respond via mail, fax, and/or online methods. On the basis of previously conducted surveys among physicians in the Canadian setting, a mixed mode of data collection was deemed to be important for increasing the response rate, particularly when involving mailing methods (14–16). A mixed mode of data collection compensates for weaknesses of each mode alone (e.g., to reduce costs, improve timeliness of responses, and reduce selection bias caused by mode of data collection) (13). Up to three personal reminders were provided to nonresponders. Data collection was open for a period of 9 weeks. Questionnaire responses were confidential with implied consent.
Statistical Analyses
Descriptive statistics were used to report on the proportion of barriers and facilitators perceived by respondents to be particularly important in their provision of conservative care. Open-ended responses were analyzed by three researchers using conventional qualitative content analysis (17). Finally, using complete case analysis, associations between demographic/clinical practice characteristics and major barriers and facilitators were explored using modified Poisson regression with robust error variance (18); outcomes were collapsed as never/rarely a barrier versus sometimes/likely/definitely a barrier and definitely not/likely not a facilitator versus maybe/likely/definitely a facilitator. We used a backward elimination technique, manually excluding terms with P value ≥0.05. On the basis of a sample size calculation, we estimated that a sample of 371 eligible respondents would generate a 95% confidence interval (95% CI) equal to the sample proportion of each outcome (e.g., ability to access resources from the conservative clinic as a barrier to care) ±0.05 when the estimated proportion of each outcome is 0.50. All statistical analyses were conducted using Stata 11.2 (StataCorp., College Station, TX) (19).
Results
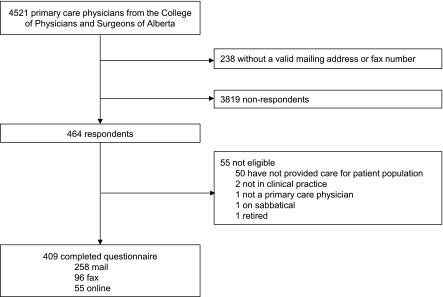
Four hundred nine primary care physicians were eligible and responded to the survey, representing 9.6% of all primary care physicians in the province (Figure 1). Of the 55 participants who were not eligible for the study, two were no longer in clinical practice, one was on sabbatical, one was retired, and one was not a primary care physician. The remainder did not have experience providing care for patients with the demographic and clinical characteristics specified for this survey. Overall, the majority of the respondents were men (61.6%), were ages 40–60 years old (62.6%), practiced in a large/medium population center (68.0%), and had extensive experience practicing in the primary care setting (i.e., 49.1% had >20 years of experience in primary care), and 91.4% dedicated >50% of their time to their clinical practice compared with research or administrative duties. In general, respondents had similar demographic and clinical characteristics as the overall population of primary care physicians in Alberta (Table 1).
Figure 1.
Flow diagram of respondents.
Table 1.
Demographic and clinical characteristics of respondents and all primary care physicians in Alberta
| Characteristic, n (%) | Respondents, n=409 | All Primary Care Physicians in AB, n=4521 |
|---|---|---|
| Sex | ||
| Men | 252 (61.6) | 2609 (57.7) |
| Age, yr | ||
| <40 | 102 (24.9) | N/A |
| 40–60 | 256 (62.6) | N/A |
| >65 | 45 (11.0) | N/A |
| No response | 6 (1.5) | N/A |
| Years practicing in primary care | ||
| <10 | 127 (31.1) | 1932 (42.7) |
| 10–20 | 81 (19.8) | 1169 (25.9) |
| >20 | 201 (49.1) | 1420 (31.4) |
| Percentage of time in clinical practice | ||
| <25 | 17 (4.2) | N/A |
| 25–50 | 13 (3.2) | N/A |
| >50 | 374 (91.4) | N/A |
| No response | 5 (1.2) | N/A |
| Location of main clinical practice | ||
| North zone | 48 (11.7) | 344 (7.6) |
| Edmonton zone | 95 (23.2) | 1509 (33.4) |
| Central zone | 54 (13.2) | 434 (9.6) |
| Calgary zone | 163 (39.9) | 1927 (42.6) |
| South zone | 49 (12.0) | 307 (6.8) |
| Population size of main clinical practice | ||
| Large/medium | 278 (68.0) | 3464 (76.6) |
| Small/rural | 131 (32.0) | 1057 (23.4) |
| Practice interest in geriatrics or care of the elderly | 258 (63.1) | N/A |
| Percentage of patients ages ≥75 yr old | ||
| <25 | 141 (34.5) | N/A |
| 25–50 | 175 (42.8) | N/A |
| >50 | 88 (21.5) | N/A |
| No response | 5 (1.2) | N/A |
| Referral of patients to nephrology | ||
| Always | 237 (57.9) | N/A |
| Sometimes | 152 (37.20) | N/A |
| Never | 17 (4.2) | N/A |
| No response | 3 (0.7) | N/A |
| Referral of patients to palliative care | ||
| Always | 47 (11.5) | N/A |
| Sometimes | 230 (56.2) | N/A |
| Never | 127 (31.1) | N/A |
| No response | 5 (1.2) | N/A |
Practice interest in the care of the elderly or geriatrics was on the basis of clinical practice interests reported by respondents and the College of Physicians and Surgeons of Alberta. Medium/large population center: consisting of a population of >30,000 people; small population center/rural area: consisting of a population of <29,999 people. Referral questions are on the basis of patients ages ≥75 years old with eGFR≤15 ml/min per 1.73 m2 not planning on initiating dialysis. AB, Alberta; N/A, not available.
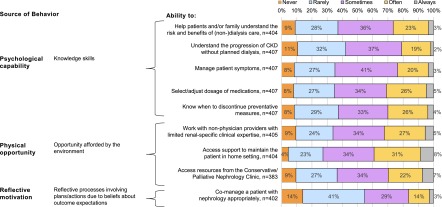
Barriers to Conservative Care
Thirty-nine percent of respondents (95% CI, 34.6% to 43.6%) indicated that their ability to access support to maintain patients in their home setting and avoid transitions of care was often/always a barrier to conservative care (i.e., the most prevalent barrier to care) (Figure 2). Approximately one third of respondents indicated that the following items were often/always a barrier: the extent to which they were able to select medications and adjust their dosages (31.0%; 95% CI, 26.7% to 35.2%), knowing when to discontinue preventative measures (30.0%; 95% CI, 25.7% to 34.2%), and helping patients/their family understand the risk/benefits of treatment options (26.5%; 95% CI, 22.4% to 30.6%). Also, about one third of respondents indicated that the following items were often/always a barrier: the extent to which they were able to work with health care providers without renal expertise (32.3%; 95% CI, 28.0% to 36.7%) and access to resources from the conservative management clinic (29.8%; 95% CI, 25.4% to 34.1%) (Figure 2).
Figure 2.
Reported frequency of barriers to conservative care.
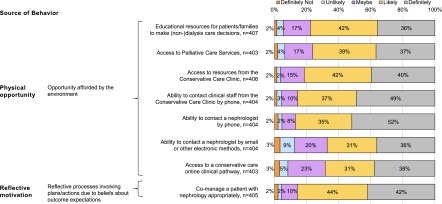
Facilitators for Enhancing Conservative Care
The major facilitators that respondents believed would likely/definitely enhance conservative care were their ability to contact a nephrologist by telephone (86.9%; 95% CI, 83.7% to 90.0%), their ability to contact clinical staff from the conservative management clinic by telephone (85.6%; 95% CI, 82.4% to 88.9%), and their ability to comanage patients with nephrologists in a manner meeting the primary care physicians’ expectations (85.4%; 95% CI, 82.2% to 88.7%) (Figure 3). Eighty-two percent of respondents (95% CI, 78.0% to 85.2%) indicated that improved access to conservative clinic services would likely or definitely enhance conservative care, 77.7% (95% CI, 73.8% to 81.5%) indicated that their ability to access educational resources to support treatment decision making for patients (and their family) would likely or definitely enhance conservative care, and 76.2% (95% CI, 72.3% to 80.2%) indicated that improved access to palliative care would likely or definitely enhance conservative care. The clinic mentioned above refers to a dedicated conservative management clinic in Alberta, which provides a novel and multidisciplinary program for patients who decide not to include dialysis in their treatment plan (20).
Figure 3.
Reported frequency of facilitators for enhancing conservative care.
Open-Ended Responses
Themes generated from the open-ended responses along with their exemplar quotations are provided in Table 2. Respondents reported educational barriers and challenges having access to and collaborating with nonphysician health care providers. The continuing medical education programs currently do not focus on conservative kidney management, and primary care physicians generally lacked personal knowledge and experience caring for the patient population of interest. As one physician indicated, “[there is a] barrier just because of my limited knowledge/experience.” In particular, respondents reported that they were unaware of the conservative management clinic, and they had a lack of knowledge about education and support resources for patients and their families. One respondent suggested such support for patients could be a priority: “I think having more educational resources for patients would help most. Once the initial decision [to pursue conservative care] is made, it is not as difficult to deal with issues as they arise.”
Table 2.
Barriers and facilitators to conservative care from open–ended survey questions
| Barriers and Facilitators | Exemplar Quotations |
|---|---|
| Barriers to conservative care | |
| Educational barriers | |
| Deficiencies in continuing medical education, personal knowledge, and experience | “Barrier just because of my limited knowledge/experience.” |
| “It [has] been an issue especially dealing with adults with cardiac risk factors as to when to stop the [nonsteroidal anti-inflammatory drugs] NSAIDs especially [acetylsalicylic acid] ASA or the statins. How does one strike the balance?” | |
| “This subject is not target[ed] very well and having information on how to manage symptoms if patients choose to not pursue dialysis would be helpful.” | |
| Lack of awareness of conservative management clinic | “Did not know conservative clinic existed. Need to promote the palliative nephrology clinic.” |
| “Never heard of the palliative nephrology clinic.” | |
| Deficiencies in education and support for patients and their families | “Patients are sometimes surprised that they have the right to refuse treatment.” |
| “I think having more educational resources for patients would help most. Once the initial decision is made, it is not as difficult to deal with issues as they arise.” | |
| Challenges having access to and collaborating with health care providers | |
| Difficulty communicating and collaborating with nephrology and other health care providers | “CKD clinic nurses have presented a significant barrier to care as they often counteract the discussions I have had with patients, their families and the homecare aids and nurses. They typically seem unable to accept that a patient has declined dialysis.” |
| “Communication between health providers is often a barrier—with suboptimal communication regarding what has been done, what is planned.” | |
| Long wait times in referral to nephrology | “Biggest barrier—wait times! [Alberta Health Services, a provincial health authority] AHS needs to hire more nephrologists.” |
| “Long wait times to see nephrologists.” | |
| “Consultant appointments are too far out and unavailable when I need them.” | |
| Travel and resource challenges specific to rural settings | “Only sometimes a trouble due to rural location and distance to dialysis center for consult with nephrology, even if conservative management.” |
| “Barriers to centralized services tend to be a problem in rural communities.” | |
| “Limited resources for care at home in rural areas.” | |
| Facilitators for improving conservative care | |
| Enhancing conservative management–related knowledge | |
| Need for continued education and clear guidelines | “Would be helpful to know when/why a nephrologist would treat a CKD/ESRD patient with conservative/palliative care, rather than choose dialysis. This might help inform future discussion with these patients prior to referral to nephrologist.” |
| “Provision of information about available services.” | |
| “I would really appreciate some educational resources for families and patients and myself.” | |
| Improving access to nephrology and palliative care services | |
| Improving communication and comanagement with nephrology | “I just want to be able to call someone for advice and not feel like I am wasting their time. I want a nephrologist to want to help me because I am in the trenches.” |
| “Shared care is essential especially given the workload of these patients. Not ‘my’ patient and not ‘your patient’. Our patient!” | |
| “Timely access and phone availability for consultation from 0800 to 2000 [hours] is important.” | |
| Better access to palliative support | “Palliative care in rural areas I find hard to access.” |
| “Insufficient after hours (palliative) nephrology resources and palliative physician resources overall.” | |
| Providing adequate resources to avoid transitions of care | |
| Need more support to keep patients at home | “Multi-system disease often requires considerable resources to keep patients in outpatient/home setting.” |
| “Home care service in [a small population center] is very poor … they say that are too busy to provide additional services for seniors. Often patients end up in the [emergency room] ER and/or hospital when early intervention could prevent this. Palliative care in this region is also poor. I have taken it on myself to do home visits, etc. to help people at home as long as the patient and family are comfortable.” |
Challenges to accessing and working with other health care providers included difficulties related to communication with other providers (e.g., CKD clinic nurses, nephrologists, and cardiologists), long wait times for a nephrology appointment, and issues specific to respondents who practice in rural settings. Respondents suggested potential strategies for improving care, including improvements in their knowledge and education related to conservative kidney management, improved access to nephrology and palliative care services, and having access to adequate resources for avoiding transitions of care (i.e., their ability to access support to maintain the patient in the home setting).
Associations between Respondent Characteristics and Barriers/Facilitators to Enhancing Care
We found associations between respondent characteristics and the ability to access support to maintain the patient at home, the most prevalent barrier to care (Table 3). Primary care physicians practicing in a metropolitan zone (versus nonmetropolitan zone), who are women, who are younger than 40 years of age, having >10 years of primary care experience, spending <25% of their time in clinical practice compared with research or administrative duties, and having <25% of their patients ages 75 years old or older were more likely to experience the barrier.
Table 3.
Association between respondent characteristics and perceived ability to access support for maintaining patients at home as a barrier to conservative care
| Demographic/Clinical Characteristic, n=392 | Unadjusted RR (95% CI) | Full Model RR (95% CI) | Reduced Model | |
|---|---|---|---|---|
| RR (95% CI) | P Value | |||
| Sex | ||||
| Men | Reference | Reference | Reference | 0.03 |
| Women | 1.19 (1.06 to 1.33) | 1.13 (1.01 to 1.27) | 1.14 (1.01 to 1.28) | 0.03 |
| Age, yr | ||||
| <40 | Reference | Reference | Reference | 0.01 |
| ≥40 | 0.89 (0.79 to 1.01) | 0.76 (0.62 to 0.92) | 0.76 (0.62 to 0.93) | 0.01 |
| Years in primary care | ||||
| <10 | Reference | Reference | Reference | 0.04 |
| ≥10 | 1.00 (0.88 to 1.14) | 1.25 (1.02 to 1.52) | 1.22 (1.06 to 1.39) | 0.04 |
| Provincial zone | ||||
| Nonmetropolitan zone | Reference | Reference | Reference | 0.004 |
| Metropolitan zone | 1.22 (1.06 to 1.40) | 1.17 (0.98 to 1.39) | 1.23 (1.01 to 1.51) | 0.004 |
| Population size | ||||
| Small/rural | Reference | Reference | — | — |
| Large/medium | 1.18 (1.02 to 1.36) | 1.07 (0.90 to 1.28) | — | — |
| Percentage of time in clinical practice | ||||
| <25 | Reference | Reference | Reference | <0.001 |
| ≥25 | 0.77 (0.67 to 0.88) | 0.76 (0.66 to 0.88) | 0.76 (0.78 to 0.98) | <0.001 |
| Clinical practice interest in the elderly | ||||
| No | Reference | Reference | — | — |
| Yes | 0.95 (0.89 to 1.00) | 0.97 (0.91 to 1.03) | — | — |
| Percentage of patients ages ≥75 yr old | ||||
| <25 | Reference | Reference | Reference | 0.03 |
| ≥25 | 0.87 (0.77 to 0.97) | 0.89 (0.79 to 1.00) | 0.88 (0.79 to 0.98) | 0.03 |
Nonmetropolitan zone includes north, central, and south zones and metropolitan zone includes Calgary and Edmonton zones according to Alberta Health Services, the health authority for Alberta, Canada. Medium/large population center: consisting of a population of >30,000 people; small population center/rural area: consisting of a population of <29,999 people. Practice interest in the care of the elderly or geriatrics was on the basis of clinical practice interests reported by respondents and the College of Physicians and Surgeons of Alberta. Outcomes: sometimes/often/always a barrier compared with never/rarely a barrier (reference). Analysis was conducted using modified Poisson regression, with robust error variance. RR, relative risk; 95% CI, 95% confidence interval; —, excluded term.
For the second most commonly reported barrier, working with health care providers with limited renal expertise, the only respondent characteristics associated with the barrier were being a woman and not having a clinical practice interest in the elderly. Women were more likely to experience the barrier, whereas respondents with a clinical practice interest in the elderly were less likely to experience the barrier. No associations were identified between demographic/clinical characteristics and the ability to contact clinical staff from the conservative care clinic by telephone as a potential facilitator to care or the ability to access an online conservative care clinical pathway as a facilitator to care.
Discussion
We report findings of a population-based survey to examine the frequency of barriers experienced by primary care physicians when conservatively managing older adults with stage 5 CKD and the potential strategies that they perceive to improve conservative patient care. Many of the barriers and strategies examined were found to be important areas for improving care, including their knowledge skills, the opportunities obtained from their environment, and their expectations of comanagement with nephrology. The most prevalent barrier to conservative kidney care was their ability to access support for maintaining their patients at home followed by their ability to work with nonphysician health care providers (e.g., care aids and home care nurses) who have limited renal–specific clinical expertise. Other barriers related to their knowledge skills, such as the extent to which they were able to select medications and adjust their dosages, were also common. The strategies most commonly reported as facilitators for improving care were the ability to have telephone contact for advice from nephrologists or conservative management clinical staff.
The major barrier to conservative kidney care, the primary care physicians’ ability to access support to maintain the patient at home, was a broad survey item intended to capture issues related to the prevention of transitions of care from the home setting. It encompassed the abilities to prevent hospitalizations, maintain functional independence, delay long-term or supportive care admissions, and enable death in the home setting. Prior studies have shown the importance that patients place on being able to be cared for and remain in their own homes. Patients are willing to trade 7 months of life expectancy to reduce admissions to the hospital (21), and many patients prefer to die at home (36.1%) or in an inpatient hospice (28.8%) rather than in an acute care hospital (22). Although a previous study reported that conservative care (compared with dialysis treatment) reduces hospitalization and increases likelihood of death at home or in a hospice (23), conservative management was examined in a setting managed by nephrologists.
We found that primary care physicians practicing in metropolitan zones compared with nonmetropolitan zones were more likely to report that their ability to maintain the patient at home was a barrier to conservative care, consistent with previous research. Studies examining older adults treated with RRT found that those living in predominately metropolitan areas had a higher likelihood of hospitalizations, intensive care unit admissions, and interventional procedures during the last month of their lives (24), and they were more likely to die in the hospital (25).
As reported in the prior qualitative study (5), a facilitator of conservative care was to establish patient/family expectations of stage 5 CKD early, and this is supported by discussions on resuscitation status. Hence, a potential explanation for the challenge in maintaining the conservatively managed patient at home may be because of the lack of advance care planning. Advance care planning is an ongoing formal process of communication between the patient, family, and health care provider regarding the patient’s end of life care goals and treatment preferences should the patient lose the ability to speak for themselves (26,27). Although advance care planning is associated with reduced hospitalization and increased death in a location preferred by the patient (28–30), previous work has illustrated that advance care planning is not systematically integrated into the care of patients with stage 5 CKD (22). In addition to advance care planning, community–based complex interventions may address this chief barrier to conservative care. On the basis of a systematic review of randomized, controlled trials, complex health and social interventions involving an interdisciplinary team can help to maintain physical function and independence among older adults (31).
Top strategies preferred by primary care physicians for improving conservative management were direct telephone access to nephrologists and conservative management clinical staff members. Telephone consultations have been identified as an important tool for rural primary care physicians and specialists (32–34) to obtain advice on routine management and organize semiurgent or urgent referrals (32). We found that primary care physicians supported telephone consultations from other providers within the conservative care clinic, regardless of whether they practiced in a rural or urban setting. There are, however, potential issues that may arise from the use of telephone consultations, including reduced ability to develop trust between providers, the extent to which specialists can provide advice without seeing the patient, and the accuracy of advice and effect on patient outcomes (32,35,36).
Some limitations should be considered when interpreting the results of our study. We were not able to determine the true denominator of eligible physicians from the physician listing provided; the reported response rate is considered to be a conservative estimate, because we anticipate that only a subset and unknown proportion of physicians would meet the eligibility criteria of our study. Although the response rate was relatively low, respondent characteristics were similar to those of the overall population, minimizing the potential for response bias. The modified Dillman method used in this study provided a practical guideline for improving the response rate, although future work is needed to examine strategies for improving the trend of lower response rates among primary care physicians (37–41).
To reduce time required to complete the questionnaire, ensure feasibility for practicing primary care physicians, and direct future areas of research, the questionnaire items were intentionally broad and only examined a selection of key sources of behavior. Although conservative care is increasingly provided by nephrology within Alberta (via only one dedicated conservative care clinic and as part of predialysis programs in the province), a large proportion of nondialysis care is still not provided by nephrology (2). Hence, conservative care is not well established compared to other settings (42), and barriers and facilitators reported by primary care physicians in this paper are likely to be generalizable to similar settings where established conservative care practices are minimal. It is also important to note that our study was focused on a specific age group with stage 5 CKD, although older adults are the majority of patients managed conservatively (2).
In conclusion, we identified important barriers and strategies and examined the extent to which primary care physicians consider them to be important in the care of older adults with stage 5 CKD not planning to initiate dialysis. Future work is needed to address the following common areas of concern to improve conservative kidney management. There is a need to enhance access to support for maintaining the patient in the home setting to avoid transitions of care, which could be accomplished, in part, through advance care planning. There is also a need to provide a broad spectrum of educational support for patients, family members, and primary care providers. Furthermore, there is a need to increase telephone access by primary care physicians for direct and timely communication with nephrologists and experts in conservative kidney care.
Disclosures
None.
Supplementary Material
Acknowledgments
We thank Dr. Jayna Holroyd-Leduc, Ms. Maoliosa Donald, and Mr. James Zhang for their contribution to the study design. We also thank Ms. Vanessa Steinke, Dr. Konrad Fassbender, Dr. John Chmelicek, Dr. Turin Chowdhury, Ms. Sarah Gil, Ms. Brenda Green, and Ms. Sarah Gillis for their support with data collection and Ms. Pam LeBlanc, Ms. Jo Anne Plested, and Mr. Robert Weaver for their assistance with data analysis.
H.T. is supported by the Alberta Innovates—Health Solutions Graduate Studentship, and this study is supported by the Interdisciplinary Chronic Disease Collaboration.
An abstract stemming from this study was presented at the 48th Annual Canadian Society of Nephrology General Meeting (May 12–14, 2016) in Halifax, Nova Scotia, Canada.
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
This article contains supplemental material online at http://cjasn.asnjournals.org/lookup/suppl/doi:10.2215/CJN.04510416/-/DCSupplemental.
References
- 1.Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group : KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int Suppl 3: 1–150, 2013 [Google Scholar]
- 2.Prevalence of Severe Kidney Disease, and Use of Dialysis and Transplantation across Alberta, 2004–2013: Annual Kidney–Strategic Clinical Network Report Calgary, Alberta, Canada, Kidney-Strategic Clinical Network, 2015, p 1–27
- 3.Davison SN, Levin A, Moss AH, Jha V, Brown EA, Brennan F, Murtagh FE, Naicker S, Germain MJ, O’Donoghue DJ, Morton RL, Obrador GT; Kidney Disease: Improving Global Outcomes : Executive summary of the KDIGO Controversies Conference on Supportive Care in Chronic Kidney Disease: Developing a roadmap to improving quality care. Kidney Int 88: 447–459, 2015 [DOI] [PubMed] [Google Scholar]
- 4.Creswell JW, Plano Clark VL: Designing and Conducting Mixed Methods Research, Los Angeles, CA, SAGE Publications, 2011 [Google Scholar]
- 5.Tam-Tham H, Hemmelgarn BR, Campbell DJ, Thomas CM, Fruetel K, Quinn RR, King-Shier KM: Primary care physicians’ perceived barriers, facilitators and strategies to enhance conservative care for older adults with chronic kidney disease: A qualitative descriptive study [published online ahead of print December 17, 2015]. Nephrol Dial Transplant [DOI] [PubMed]
- 6.College of Physicians and Surgeons of Alberta: 2013 CPSA Annual Report, 2013. Available at: http://www.cpsa.ab.ca/annualreport/2013-cpsa-annual-report. Accessed July 23, 2014
- 7.Tam-Tham H, Hemmelgarn B, Campbell D, Thomas C, Quinn R, Fruetel K, King-Shier K: Primary care physicians’ perceived barriers and facilitators to conservative care for older adults with chronic kidney disease: Design of a mixed methods study. Can J Kidney Health Dis 3: 17, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Michie S, van Stralen MM, West R: The behaviour change wheel: A new method for characterising and designing behaviour change interventions. Implement Sci 6: 42, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Michie S, Atkins L, West R: The Behaviour Change Wheel: A Guide to Designing Interventions, 2014. Available at: http://www.behaviourchangewheel.com/about-book. Accessed June 1, 2016
- 10.Cane J, O’Connor D, Michie S: Validation of the theoretical domains framework for use in behaviour change and implementation research. Implement Sci 7: 37, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Burns KEA, Duffett M, Kho ME, Meade MO, Adhikari NKJ, Sinuff T, Cook DJ; ACCADEMY Group : A guide for the design and conduct of self-administered surveys of clinicians. CMAJ 179: 245–252, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dillman D: Mail and Telephone Surveys: The Total Design Method, New York, John Wiley & Sons, 1978 [Google Scholar]
- 13.Bethlehem J: Applied Survey Methods: A Statistical Perspective, edited by Groves R, Kalton G, Rao JN, Schwarz N, Skinner C, New York, John Wiley & Sons, Ltd, 2009 [Google Scholar]
- 14.Health Quality Council of Alberta: Review of the Quality of Care and Safety of Patients Requiring Access to Emergency Department Care and Cancer Surgery and the Role and Process of Physician Advocacy, 2012. Available at: https://d10k7k7mywg42z.cloudfront.net/assets/53221424d6af6808200002c3/EDCAP_FINAL_REPORT.pdf. Accessed June 1, 2016
- 15.Wiebe ER, Kaczorowski J, MacKay J: Why are response rates in clinician surveys declining? Can Fam Physician 58: e225–e228, 2012 [PMC free article] [PubMed] [Google Scholar]
- 16.Lemaire JB, Wallace JE: How physicians identify with predetermined personalities and links to perceived performance and wellness outcomes: A cross-sectional study. BMC Health Serv Res 14: 616, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hsieh H-F, Shannon SE: Three approaches to qualitative content analysis. Qual Health Res 15: 1277–1288, 2005 [DOI] [PubMed] [Google Scholar]
- 18.Zou G: A modified Poisson regression approach to prospective studies with binary data. Am J Epidemiol 159: 702–706, 2004 [DOI] [PubMed] [Google Scholar]
- 19.StataCorp : Stata Statistical Software: Release 11, College Station, TX, StataCorp LP, 2009 [Google Scholar]
- 20.Southern Alberta Renal Program: Conservative Management Care. Available at: https://informalberta.ca/public/service/serviceProfileStyled.do?serviceQueryId=1056957. Accessed April 13, 2016
- 21.Morton RL, Snelling P, Webster AC, Rose J, Masterson R, Johnson DW, Howard K: Factors influencing patient choice of dialysis versus conservative care to treat end-stage kidney disease. CMAJ 184: E277–E283, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Davison SN: End-of-life care preferences and needs: Perceptions of patients with chronic kidney disease. Clin J Am Soc Nephrol 5: 195–204, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Carson RC, Juszczak M, Davenport A, Burns A: Is maximum conservative management an equivalent treatment option to dialysis for elderly patients with significant comorbid disease? Clin J Am Soc Nephrol 4: 1611–1619, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wong SPY, Kreuter W, O’Hare AM: Treatment intensity at the end of life in older adults receiving long-term dialysis. Arch Intern Med 172: 661–663, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.O’Hare AM, Rodriguez RA, Hailpern SM, Larson EB, Kurella Tamura M: Regional variation in health care intensity and treatment practices for end-stage renal disease in older adults. JAMA 304: 180–186, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Davison SN: Advance care planning in patients with chronic kidney disease. Semin Dial 25: 657–663, 2012 [DOI] [PubMed] [Google Scholar]
- 27.Luckett T, Sellars M, Tieman J, Pollock CA, Silvester W, Butow PN, Detering KM, Brennan F, Clayton JM: Advance care planning for adults with CKD: A systematic integrative review. Am J Kidney Dis 63: 761–770, 2014 [DOI] [PubMed] [Google Scholar]
- 28.Molloy DW, Guyatt GH, Russo R, Goeree R, O’Brien BJ, Bédard M, Willan A, Watson J, Patterson C, Harrison C, Standish T, Strang D, Darzins PJ, Smith S, Dubois S: Systematic implementation of an advance directive program in nursing homes: A randomized controlled trial. JAMA 283: 1437–1444, 2000 [DOI] [PubMed] [Google Scholar]
- 29.Teno JM, Gruneir A, Schwartz Z, Nanda A, Wetle T: Association between advance directives and quality of end-of-life care: A national study. J Am Geriatr Soc 55: 189–194, 2007 [DOI] [PubMed] [Google Scholar]
- 30.Wright AA, Zhang B, Ray A, Mack JW, Trice E, Balboni T, Mitchell SL, Jackson VA, Block SD, Maciejewski PK, Prigerson HG: Associations between end-of-life discussions, patient mental health, medical care near death, and caregiver bereavement adjustment. JAMA 300: 1665–1673, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Beswick AD, Rees K, Dieppe P, Ayis S, Gooberman-Hill R, Horwood J, Ebrahim S: Complex interventions to improve physical function and maintain independent living in elderly people: A systematic review and meta-analysis. Lancet 371: 725–735, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hollins J, Veitch C, Hays R: Interpractitioner communication: Telephone consultations between rural general practitioners and specialists. Aust J Rural Health 8: 227–231, 2000 [DOI] [PubMed] [Google Scholar]
- 33.Power R, Williams B: Rural access line: A tool for improving communication between rural GPs and hospital specialists in Western Australia. Med J Aust 160: 450, 1994 [PubMed] [Google Scholar]
- 34.Smego RA, Khakoo RA, Burnside CA, Lewis MJ: The benefits of telephone-access medical consultation. J Rural Health 9: 240–245, 1993 [DOI] [PubMed] [Google Scholar]
- 35.Burden M, Sarcone E, Keniston A, Statland B, Taub JA, Allyn RL, Reid MB, Cervantes L, Frank MG, Scaletta N, Fung P, Chadaga SR, Mastalerz K, Maller N, Mascolo M, Zoucha J, Campbell J, Maher MP, Stella SA, Albert RK: Prospective comparison of curbside versus formal consultations. J Hosp Med 8: 31–35, 2013 [DOI] [PubMed] [Google Scholar]
- 36.Kirsh SR, Ho PM, Aron DC: Providing specialty consultant expertise to primary care: An expanding spectrum of modalities. Mayo Clin Proc 89: 1416–1426, 2014 [DOI] [PubMed] [Google Scholar]
- 37.Abdulaziz K, Brehaut J, Taljaard M, Émond M, Sirois M-J, Lee JS, Wilding L, Perry JJ: National survey of physicians to determine the effect of unconditional incentives on response rates of physician postal surveys. BMJ Open 5: e007166, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Grava-Gubins I, Scott S: Effects of various methodologic strategies: Survey response rates among Canadian physicians and physicians-in-training. Can Fam Physician 54: 1424–1430, 2008 [PMC free article] [PubMed] [Google Scholar]
- 39.Kellerman SE, Herold J: Physician response to surveys. A review of the literature. Am J Prev Med 20: 61–67, 2001 [DOI] [PubMed] [Google Scholar]
- 40.Nicholls K, Chapman K, Shaw T, Perkins A, Sullivan MM, Crutchfield S, Reed E: Enhancing response rates in physician surveys: The limited utility of electronic options. Health Serv Res 46: 1675–1682, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.VanGeest JB, Johnson TP, Welch VL: Methodologies for improving response rates in surveys of physicians: A systematic review. Eval Health Prof 30: 303–321, 2007 [DOI] [PubMed] [Google Scholar]
- 42.Okamoto I, Tonkin-Crine S, Rayner H, Murtagh FE, Farrington K, Caskey F, Tomson C, Loud F, Greenwood R, O'Donoghue DJ, Roderick P: Conservative care for ESRD in the United Kingdom: A national survey. Clin J Am Soc Nephrol 10: 120–126, 2015 [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.