Philosophically, the concept of peer review of a debate on the merits of oral anticoagulation [specific agent unspecified] for end-stage renal disease patients with atrial fibrillation on hemodialysis (1,2) is a bit nebulous, because the outcome of debates depends on more than enumerating facts and factoids—the medium is indeed part of the message or massage. It is worth reviewing the back story contributing to the discussion of the issue of anticoagulation in patients on hemodialysis with atrial fibrillation, in part to add some nuanced corrections to the comments made in the opposing papers. As the only cardiologist participating in the 2005 Kidney Disease Outcomes Quality Initiative (KDOQI) Clinical Practice Guidelines for Cardiovascular Disease in Dialysis Patients (3) and cochair (with Eberhard Ritz) of the 2010 Kidney Disease Improving Global Outcomes (KDIGO) Cardiovascular Controversies Conference (4), I have a unique 15-year perspective on the topic. The KDOQI task force began its work in 2001 and eventually published a comprehensive guideline statement in 2005 (3). It generally concurred with existing American Heart Association (AHA) guidelines, including with regard to antithrombotic therapy (warfarin and aspirin; the latter therapy, which is actually an antiplatelet agent, was subsequently downgraded to “placebo-like” status or worse versus warfarin; although aspirin monotherapy was once perceived to be of benefit, it is not currently [5]). The guideline said that “antithrombotic therapy should be considered for patients with nonvalvular atrial fibrillation, based on their risk of embolism and risk of bleeding complications” (3); an additional caveat noted increased risk of bleeding and necessity for careful monitoring of patients on dialysis (strength of recommendation was C) (3). The rationale for this approach in guideline 9 was that, failing evidence to the contrary to overturn existing AHA guidelines, the KDOQI task force concurred with established precedent in the general population.
In 2010, our KDIGO perspective was altered by newer observational data (discussed by the respondents). Con cocounsels Keskar and Sood (2) have subtly altered the nuanced pronouncement of the KDIGO conference (citing the KDIGO information in the work by Herzog et al. [4]) in their brief: “This is consistent with KDIGO recommendations against the use of routine anticoagulation of CKD 5D patients with atrial fibrillation for primary prevention of stroke” (2). Missing from their brief citing from KDIGO is the key contextual statement of intent: “These observations prompted reconsideration of the value of warfarin for stroke prevention in CKD 5D patients with atrial fibrillation. Weighing the available evidence, the benefit of warfarin anticoagulation for primary prevention of stroke in CKD 5D patients is questionable” (4). Given the uncertainty in 2010 (with only dabigatran, a new oral anticoagulant [NOAC], having recently been approved in the United States), KDIGO rescinded the recommendation for routine anticoagulation of patients with CKD stage 5D and atrial fibrillation for primary prevention of stroke, pending new data.
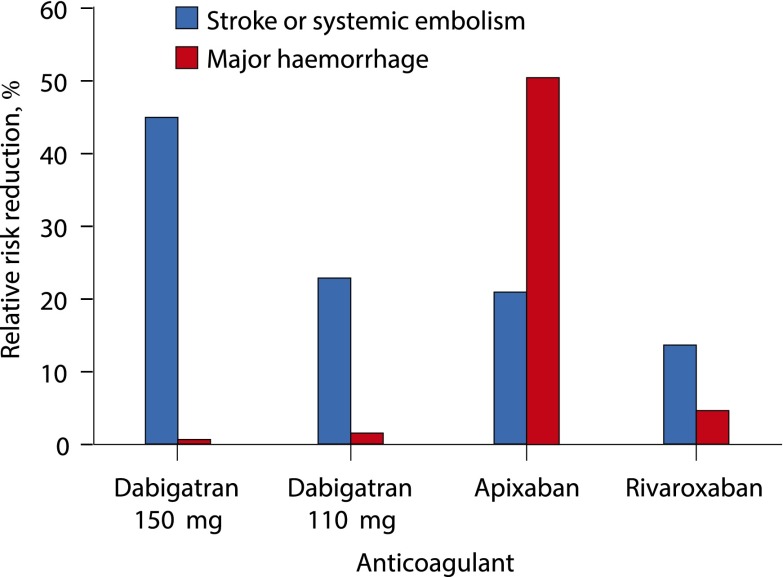
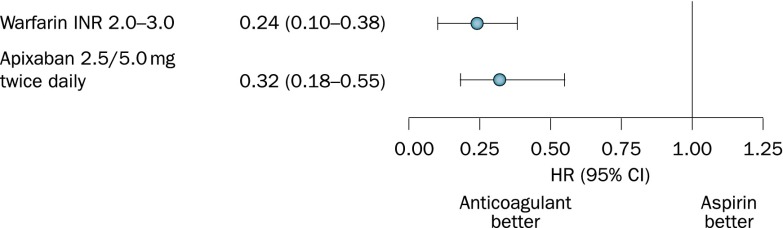
Since 2010, we have amassed new data of interest pertaining to nondialysis-dependent CKD. A convincing case (Figure 1) can be made for the clinical superiority of NOACs to warfarin with respect to a composite of efficacy and safety on the basis of post hoc analyses of large clinical trials (6). There is no suggestion that warfarin is either safer or more efficacious than NOACs. As shown in Figure 2, post hoc analysis of the Apixaban versus Acetylsalicylic Acid to Prevent Stroke in Atrial Fibrillation Patients study (and the Stroke Prevention in Atrial Fibrillation III study) suggests that therapeutic anticoagulation with apixaban is superior to anticoagulation with aspirin (or with warfarin versus aspirin and low-dose warfarin) (6). In the context of both Figures 1 and 2 (NOACs seem better than warfarin, and warfarin or apixaban seems better than ineffective anticoagulation), it is not unreasonable for the bench to conclude that NOACs are a reasonable option for primary prevention of stroke in nondialysis-dependent patients with CKD and atrial fibrillation (providing support for the pro counsel position of McCullough et al. [1]). Thanks to the US Food and Drug Administration (FDA; which effectively tips the balance in favor of the pro counsel position of McCullough et al. [1]), patients with ESRD (patients on dialysis) have been included on the official apixaban label since January of 2014, and new guidance on dosing rivaroxaban in patients with dialysis appeared in May of 2016, both now with caveats regarding the absence of clinical trial data.
Figure 1.
Relative risk reductions in stroke or systemic embolism and major hemorrhage by novel oral anticoagulants versus warfarin in patients with moderate CKD. Patients with CKD had estimated creatinine clearances of 30–49 ml/min, except for those treated with apixaban (25–50 ml/min). Risk reductions were statistically significant for dabigatran (150 mg) on stroke and apixaban on major hemorrhage. Reprinted from reference 6, with permission.
Figure 2.
Hazard ratios (HRs) for subgroups of patients with CKD stage 3 from two randomized trials comparing anticoagulation with aspirin. For warfarin comparison from the SPAF III Study, the outcome was ischemic stroke and systemic embolism, and the aspirin group additionally received low ineffective doses of warfarin. For apixaban, the outcome was stroke and systemic embolism. 95% CI, 95% confidence interval; INR, international normalized ratio SPAF III, Stroke Prevention in Atrial Fibrillation. Reprinted from reference 6, with permission.
Although some might argue that the debate on the merits of anticoagulation should hinge on warfarin (due to the available pool of observational data), the bench is not persuaded by this line of reasoning. First, the paucity of robust (i.e., clinical trial) data renders the debate (regarding warfarin) moot. Second, the train has left the station (or the horse is out of the barn if you live in a rural district) due to the FDA’s decision to officially sanction two NOACs in patients on dialysis, effectively trivializing a debate focused on warfarin. The difficulty of maintaining patients on dialysis in a therapeutic range with warfarin is particularly vexing to clinicians; the bar for considering an NOAC over warfarin is low (especially after the FDA’s guidance on apixaban and rivaroxaban). Third, warfarin is a particularly unappealing choice of anticoagulant in a patient population already at risk for accelerated vascular calcification (or worse, calciphylaxis). Fourth, the data on NOACs in nondialysis-dependent patients with CKD are reasonably robust and of material interest in this debate: NOACs seem to provide better safety and efficacy than warfarin in this CKD population (Figure 1). It is not unreasonable to infer that NOACs would be superior (or at least noninferior) to warfarin in CKD stage 5D.
McCullough et al. (1) and Keskar and Sood (2) have admirably argued their positions. The reviewer panel labored over the summer, weighing and massaging the facts and factoids. Verdict 2 is found in favor of the McCullough et al. (1) pro counsel team. The bench strongly concurs with both teams regarding the necessity for randomized clinical trials on anticoagulation in patients on dialysis with atrial fibrillation (particularly given the scope of the problem, with small studies using implantable loop recorders suggesting under-recognition of paroxysmal atrial fibrillation in patients on hemodialysis). It will be challenging to complete a well designed, adequately powered clinical trial that will provide definitive guidance on the safety and efficacy of anticoagulation for primary prevention of ischemic stroke and systemic embolism in patients with CKD stage 5D and atrial fibrillation. It should not just be a safety trial on the noninferiority of NOACs versus warfarin, but one that will hopefully inform clinicians (and future guideline task forces) on the wisdom of anticoagulation in this challenging patient population.
Disclosures
C.A.H. has an equity interest in Johnson & Johnson (New Brunswick, NJ), and he received an honorarium from Bristol Myers Squibb (New York, NY) for participation in an advisory board meeting in 2015.
Acknowledgments
This work was supported by the Chronic Disease Research Group, Minneapolis Medical Research Foundation.
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
References
- 1.McCullough PA, Ball T, Cox KM, Assar MD: Use of oral anticoagulation in the management of atrial fibrillation in patients with ESRD: Pro. Clin J Am Soc Nephrol 11: 2079–2084, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Keskar V, Sood MM: Use of oral anticoagulation in the management of atrial fibrillation in patients with ESRD: Con. Clin J Am Soc Nephrol 11: 2085–2092, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.K/DOQI Workgroup : K/DOQI clinical practice guidelines for cardiovascular disease in dialysis patients. Am J Kidney Dis 45[Suppl 3]: S1–S153, 2005 [PubMed] [Google Scholar]
- 4.Herzog CA, Asinger RW, Berger AK, Charytan DM, Díez J, Hart RG, Eckardt KU, Kasiske BL, McCullough PA, Passman RS, DeLoach SS, Pun PH, Ritz E: Cardiovascular disease in chronic kidney disease. A clinical update from Kidney Disease: Improving Global Outcomes (KDIGO). Kidney Int 80: 572–586, 2011 [DOI] [PubMed] [Google Scholar]
- 5.Qamar A, Bhatt DL: Stroke prevention in atrial fibrillation in patients with chronic kidney disease. Circulation 133: 1512–1515, 2016 [DOI] [PubMed] [Google Scholar]
- 6.Hart RG, Eikelboom JW, Ingram AJ, Herzog CA: Anticoagulants in atrial fibrillation patients with chronic kidney disease. Nat Rev Nephrol 8: 569–578, 2012 [DOI] [PubMed] [Google Scholar]