Summary
Severe burn injuries often require specialized treatment at a burn center. It is known that prompt admission to an intensive care unit is essential for achieving good outcome. Nevertheless, very little is known about the duration of time before a patient is admitted to a specialized center after a burn injury in Germany, and whether the situation has improved over time. We retrospectively analyzed time from burn injury to admission to the burn intensive care unit in the Cologne-Merheim Medical Center - one of Germany’s specialized burn centers - over the last 25 years. Moreover, we analyzed the data based on differences according to time of injury and day of the week, as well as severity of the burn injury. There was no weekend effect with regard to transfer time; instead transfer time was particularly short on a Monday or on Sundays. Furthermore, patients with severe burn injuries of 40-89% total body surface area (TBSA) showed the least differences in transfer time. Interestingly, the youngest and the oldest patients arrived at the burn intensive care unit (BICU) the fastest. This study should help elucidate published knowledge regarding transfer time from the scene of the accident to admission to a BICU in Germany.
Keywords: admission time, BICU, TBSA
Abstract
Les brûlés graves ont fréquemment besoin d’une prise en charge spécialisée dans un centre de brûlés (CTB). Il est avéré qu’une admission rapide dans un service de réanimation pour brûlés (SRB) est un paramètre d’évolution favorable. Cependant, on ne sait que peu de chose sur le temps écoulé, en Allemagne, entre la brûlure et l’admission en CTB, et si ce délai s’est raccourci au fil du temps. Nous avons analysé le délai entre brûlure et arrivée dans le SRB de Cologne-Merheim sur une durée de 25 ans. Nous avons aussi étudié l’impact de la gravité de la brûlure, du jour et de l’heure de sa survenue sur ce délai. Il n’y a pas « d’effet week-end », et le délai est plus court les lundis et dimanches. Le délai est relativement homogène pour des surfaces brûlées de 40 à 89%. Les patients les plus jeunes et les plus âgés sont ceux qui arrivent le plus vite en SRB. Cette étude devrait aider à clarifier les données déjà publiées concernant le temps de transfert du lieu de l’accident au SRB en Allemagne.
Introduction
In the US, approximately 40,000 burn patients require hospitalization every year.1 Depending on severity, transfer to a specialized burn intensive care unit (BICU) is necessary for adequate treatment. The importance of prompt treatment within a few hours after the injury occurred is known to be a determining factor for good outcome and mortality reduction.2 Furthermore, studies from the United States have shown that the prognosis of burn patients initially transferred to primary care hospitals is poorer than the prognosis of patients directly transferred to a regional burn center.3 Ashworth et al. reported that the period between burn injury and admission to a burn center in the UK was ten hours on average. Most of the time was either spent at a local hospital or being transferred to the burn center; most patients arrived at the local hospital within 2.5 hours after injury. Optimal burn intensive care includes specialized facilities and specialized equipment, as well as specialized surgeons and nurses.4,5 Therefore, treatment at these centers results in clearly superior patient outcomes.2 Worldwide, for improved coordination, burn associations have established burn center referral criteria.1 Any patient with a burn injury >20% total body surface area (TBSA) is considered to have a severe injury.1 Furthermore, severe injury is assumed for: facial and hand burns; burns of the feet, genitalia or perineum; third degree burns of >10% TBSA; electrical or chemical burns; inhalation injuries; or burn injuries to patients with preexisting medical disorders.6,8
A survey conducted in Austria, Switzerland and Germany in 2000 showed that 70% of all patients admitted to certain burn units reached the BICU within a period of four hours.6,8 Apart from this, currently little is known about time from burn injury to admission to a BICU in Germany. Therefore, we retrospectively evaluated all burn patients admitted to the BICU at Cologne-Merheim Medical Center from 1989 through 2013, the aim being to identify the influence of week day, TBSA, patients’ age and artificial ventilation on time from injury to admission, and determine any changes that occurred over those 25 years
Patients and methods
Patients
A retrospective descriptive study was conducted on all patients admitted to the BICU at the Cologne-Merheim Medical Center, University Hospital of Witten/Herdecke from 1989 through 2013. Exclusion criteria were patients suffering from toxic epidermal necrolysis (TEN) or other injuries not associated with burns. Information on time from injury to admission and type of transport was documented for a total of 1,089 primary admission patients, admitted between 1989 and 2013; furthermore, information regarding 419 secondary admission patients was recorded for the same period.
Setting
The burn center at the Cologne-Merheim Medical Center is one of Germany’s specialized burn centers. Cologne is located in North-Rhine-Westphalia in the western part of Germany, with a population of >1 million. In Germany, all patients with severe burn injuries are triaged to specialized hospitals, according to the German Association for Burn Treatment guidelines.
Data collection
Clinical data of all patients admitted to the BICU for thermal, electrical or chemical injury were collected by the attending surgeon and entered into a web-based data collection platform that was specifically adapted for this purpose. Hereby a documentation of age and sex as well as primary or secondary admission was performed. Time of injury and time of admission to the BICU was recorded, as well as type of transportation, place of injury and type of injury. Furthermore, information regarding pre-hospital care was collected, including information on intubation. Data concerning TBSA was added during treatment in the BICU. Data integrity was evaluated via an assessment of missing values, range checks, plausibility checks and internal consistency.
Statistical analysis
Statistical analysis was conducted using the “open source” software “R” (Version 3.1.2 / http://www.r-project.com/). After analysis of regression and variance, p<0.05 was considered to indicate a statistically significant difference. The results were confirmed using the Kruskal-Wallis rank sum test and the Mann-Whitney U test.
Results
This study comprised 1,508 patients who were admitted to the burn intensive care unit (BICU) of the Cologne-Merheim Medical Center from 1989 through 2013; 1,089 patients were primary admissions and 419 were secondary. Patient age of the primary admissions ranged from 1 to 99 years old. Most of the admitted patients were aged 30–39 years (n=235). The numbers of small children from 0-9 years (n=23) and old patients aged 90-99 years (n=8) were the lowest.
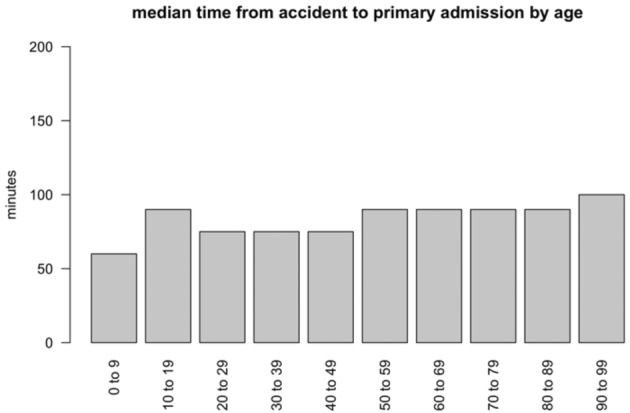
The influence of age on time to admission
The median time from injury to primary admission for children from 0-9 years was 60 minutes with an interquartile range (IQR) of 42.5 from injury to BICU admission. Patients aged 20-49 years arrived at the BICU after a median time of 75 minutes with an IQR of 60 for the first 2 and 64.5 for the latter (Fig. 1). Patients aged 90-99 years (n=8) had a median transportation time of 100 minutes and an IQR of 75 (Fig. 1). The difference in time to admission between the different age groups was not significant (p=0.25).
Fig. 1. Influence of age on the median time to admission.
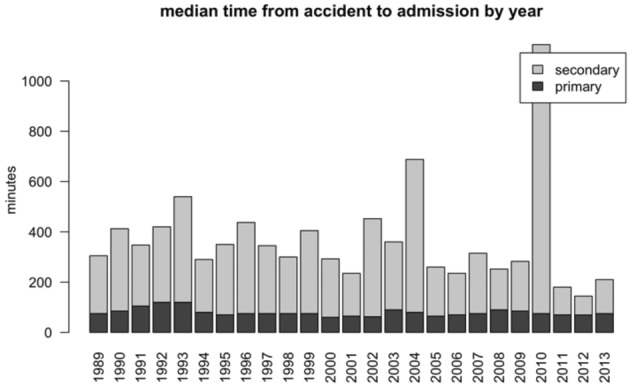
Primary versus secondary admission
We also analyzed the median time from accident to admission with a focus on primary and secondary admissions for each year. The duration of primary admissions (n=1,089) showed minimal variation over the last 25 years (p=0.09) (Fig. 2), with a median ranging between 60 minutes (2000) and 120 minutes (1991 and 1993). Overall, patients transferred from a different hospital (n=419; 27.8%) had a median transportation time ranging between 75 minutes (2012) and 1070 minutes (2010) (Fig. 2).
Fig. 2. Comparison of median time from injury to admission of primarily and secondary admitted patients from 1989 to 2013.
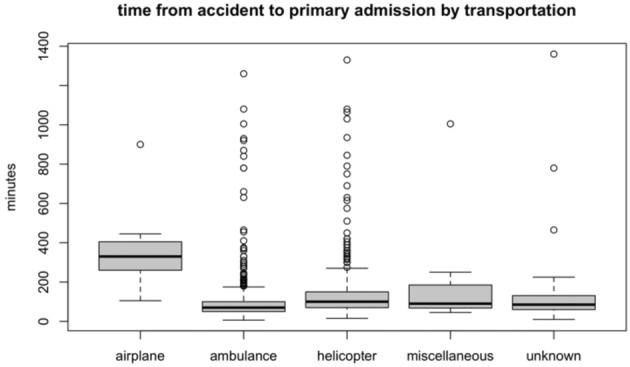
Type of transport
Altogether, patients in Cologne were most often transported by ambulance (n=655; 60.1%), with a median transport time of 70 minutes and an interquartile range (IQR) of 50 (Fig. 3). A total of 373 patients (34.2%) were transported by helicopter (median transport time: 100 minutes, IQR 80). Thirteen patients arrived by plane (median 330, IQR 145) (Fig. 3). Hereby the differences in transfer time were statistically significant between ambulance and plane (p<0.001), ambulance and helicopter (p<0.001) and helicopter and plane (p<0.001).
Fig. 3. Influence of type of transportation on time to admission of primarily admitted patients.
Influence of total burned surface area (TBSA) on transfer time for primarily admitted patients
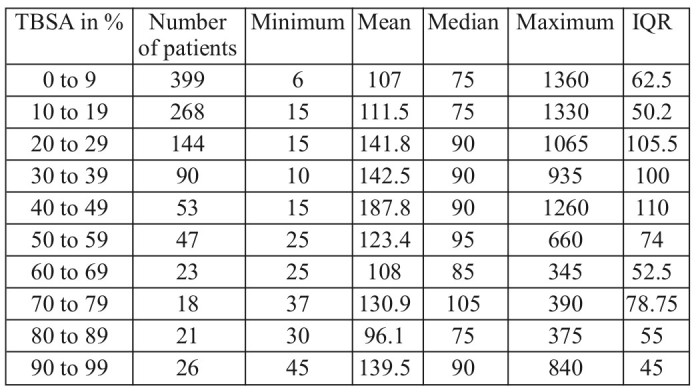
Patients with a TBSA ranging from 0-9% (n=399), of 10-19% (n=268) and 80-89% (n=21) reached the BICU after a median of 75 minutes (with an IQR of 62.5 for the first followed by 50.2 and 55 for the latter) (Fig. 4). Patients with a TBSA of 20-49% and 90-99% reached the BICU with a median duration of 90 minutes. Hereby the IQR was 105.5 for a TBSA of 20- 29%, 100 for a TBSA of 30-39%, 110 for a TBSA of 40-49% and 45 for a TBSA of 90-99%. The longest median transfer time was found for patients with 70-79 % TBSA (n=53; 105 minutes, IQR 78.75) (Fig. 4). A significant difference could not be found (p=0.12). The shortest individual time from injury to admission was 6 minutes and was found for a patient with a TBSA of 4%. Of all patients with a TBSA of 90-99%, the fastest arrival was after 45 minutes. Interestingly, the longest time from injury to admission was also a patient with a TBSA of 0-9%; it was 1,360 minutes (>22 hours). For patients with burns of 60-89% TBSA, it took a maximum duration of 390 minutes (approximately 6.5) hours to reach the hospital (Table I).
Fig. 4. Influence of TBSA on median time to admission of primarily admitted patients.
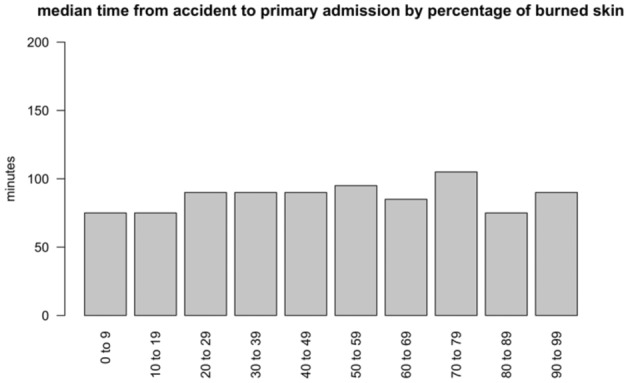
Table I. Influence of total body surface area (TBSA) burned on time from injury to admission of primarily admitted patients.
Intubation
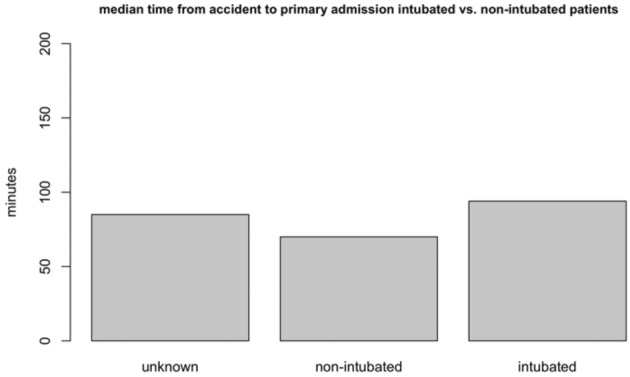
Overall, 420 primary admission patients (38.6%) were intubated when they arrived at the BICU with a median transfer time of 94 minutes and an IQR of 80, compared to a significantly lower median transfer time of 70 minutes and an IQR of 65 for patients who had not been intubated (n=652) (p<0.0001). For 17 patients, no information regarding intubation was available (Fig. 5).
Fig. 5. Influence of pre-hospital intubation on median time to admission of primarily admitted patients.
Influence of day of the week on time to admission
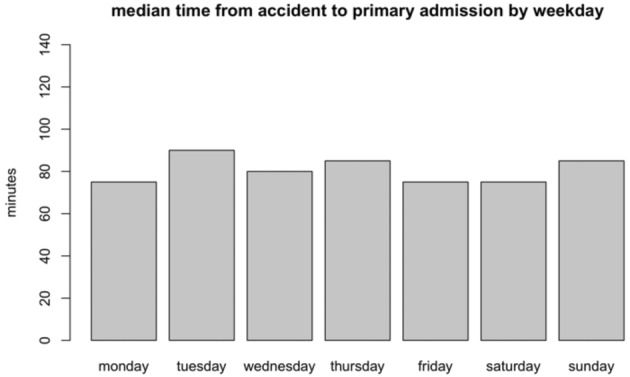
The highest number of patients (n=182) was admitted on a Saturday with a median time to admission of 75 minutes (IRQ=60) (Fig. 6). For Mondays, the median was 75 minutes with an IRQ of 40 (n=154). On Tuesdays, the median time to admission was 90 minutes for the 176 patients admitted, with an IQR of 70. The least number of patients (n=122) was admitted on a Sunday, with a median time of 85 minutes (IQR=67.5), followed by Fridays (128 patients and a median time to admission of 75 minutes with an IQR of 60) (Fig. 6). A significant difference in time to admission could not be found for the different weekdays (p=0,446).
Fig. 6. Influence of day of the week on median time from injury to admission of primarily admitted patients.
Discussion
Information was minimal regarding time from burn injury to admission with regard to change over time, seasonal variation, day of the week, size of the burn injury and intubation for patients admitted to the BICU at the Cologne-Merheim Medical Center from 1989 to 2013; therefore a retrospective evaluation was conducted to reveal weak points and optimize transfer time.
In California, USA, Hagstrom et al. evaluated 41 patients admitted to a burn center and found a mean transfer time from injury to admission of <6.3 hours.9 Klein et al. evaluated transfer times for 424 patients from 2000-2003 in Washington State, USA, and found times to admission of up to 7.2 hours.10 A study from Central Malawi conducted from July 2008 through June 2009 on 370 burn patients reported the admission of 74% of the patients to the Kamuzu Central Hospital within 8 hours.11 Different factors are involved in a long duration from injury to hospital admission. They include time-consuming pre-hospital treatment, long distances, and lack of an efficient transport method. Cologne is located in North-Rhine-Westphalia in the western part of Germany with a population of >1 million. Although many patients are admitted from North-Rhine-Westphalia, and especially from Cologne and Bonn, burn patients from all areas of Germany are transferred to Cologne if no closer burn center has the treatment ability. Unfortunately, a long transfer time can complicate the treatment of severe, lifethreatening problems.12 Sheridan et al. analyzed 1,999 patients with a delayed transfer time during their clinical stay and found that these patients suffered from more renal dysfunction, a greater incidence of wound sepsis, more cases of bacteremia, higher mean number of central venous catheter days, longer duration until 95% of all wounds were closed, more pneumonia, increased presence of resistant organisms, and higher mean number of ventilation days. These factors can result in a longer length of stay and an increased mortality, compared to patients without delayed transfer.13,14
Influence of age on time to admission
Young and elderly patients especially require prompt medical treatment because they are more sensitive to injury and they develop hypothermia more quickly.15-17 In agreement with these factors, Theodorou et al. reported that the proportion of elderly patients (>60 years) with burns has increased, and recommended liberal referral to a burn center.13 Despite this fact, unfortunately, long median transfer times were found for elderly patients although they were not significant. Fortunately, the primary admission times of young patients were low compared to the other age groups in our study.
Time to admission for primary versus secondary admissions
Estimation of burn size is important in the decision regarding whether a patient is transferred to a burn center and whether he or she receives fluid resuscitation.10 Unfortunately, previous studies have shown that TBSA is often over- and underestimated. Data from Australia showed that in nearly 60% of all patients, the calculated TBSA differed between referral hospitals and burn centers.3 Incorrect burn size estimation can lead to the patient being transferred to a regional hospital instead of directly to a burn center. In 1987, Palmer et al. determined that 35% of all children and 79% of all adults admitted to the Regional Burns Center for South East Scotland at Bangour Hospital and the Royal Hospital for Sick Children in Edinburgh were transferred from another hospital rather than transported directly to a burn center.12 In a retrospective analysis from Korea on 19,157 patients, less than 40% of the patients were admitted directly to the burn unit.18 Compared to this, over 2/3 of all admissions in Cologne were primarily to the burn unit. Additionally, in Cologne, most patients reached the BICU on the day of injury, which is faster than the time reported in other studies. In this context, patients admitted to the burn unit of Massachusetts USA had a mean transport time from the primary care hospital of 16.3 days ± 3.4 days after injury14 which is longer than the admission time to the burn unit in Singapore, with 0 to 3.05 days.19 Similar data was found for Nepal where the majority of cases reached the burn unit >24 hours after burn injury.20 Studies from the UK and the US regarding secondary admissions to a burn center showed that most of the time was spent at the local hospital21 or being transported to the burn center; the patients with burn injuries reached the local hospital at an average of 2.5 hours after injury.22 Similar transport times for primarily admitted patients were found for Cologne. Most of the long transport times found for secondary admitted patients were due to admission of patients from outside of Europe who requested medical aid.
It has often been discussed if a longer time until admission to a burn center has any influence on patient outcome. An analysis from 2000-2003 on 1,877 patients in the USA showed that long transportation times did not impact patient outcome, even if the transfer was longer than 9 hours.10 Cassidy et al. found a rise in mortality after 16 hours for patients with an inhalation injury who were transported from a primary care facility; they therefore stressed that patients with an inhalation injury should be transferred to a burn unit within 16 hours after the event.23
Time from injury to admission with regard to type of transport
Cologne is located in North-Rhine-Westphalia in the western part of Germany, with a population of >1 million. It has a good infrastructure, which allows the ambulance to be an appropriate vehicle to transport patients over short distances. This is underscored by the fact that most of the patients arrive at our BICU by ambulance, which is the fastest method of transport. In Edinburgh and Southeast Scotland in 1987, Palmer et al. found that 68% of all 124 primarily admitted adult patients were transported by ambulance to the hospital. Interestingly, 61% of the admitted 152 children with burn injuries were transported in private cars, and only 1% of the adult patients reached the hospital by helicopter.12 During rush hours with heavy traffic or for transport outside of the city, transport via helicopter to the BICU in Cologne is common and takes a mean 147.1 ± 159.9 minutes. In comparison, the time from injury to arrival at the regional burn unit in Birmingham, UK had a mean 148 minutes for all 27 patients arriving by helicopter during the three-year study period (2004-2007).21 The reasons for transport by helicopter are often multifactorial and not solely based on clinical findings.24 A major factor is the distance to the burn unit. In a 2002 study by Slater et al. in Pittsburgh, Pennsylvania, 80 of 98 patients who had been transported by helicopter were flown further than 25 miles.24 Distances <90 miles can often be reached by helicopter. For greater distances, airplanes are often used.10 It was reported that, in the UK, within a 180- mile radius, transport by helicopter is not appreciably faster than by ambulance and burn patients do not benefit clinically.21 Interestingly, patients transferred by air often have a higher percentage of burned skin and/or smoke inhalation injury.24,25
Influence of total body surface area (TBSA) burned on time until admission of primarily admitted patients
Interestingly, the highest variation in time to admission was found for primarily admitted patients with the smallest TBSA. This might reflect the fact that the people in contact with patients that have severe burn injuries might call the emergency department faster if TBSA is higher. Change in time from injury to admission due to intubation Altogether, 38.6% of all primarily admitted patients that arrived at the BICU in Cologne were intubated. Similar data can be found in the literature. In this context, Pegg et al. stated that many patients with burn injuries are intubated for safety reasons prior to transport.26 Due to the time-consuming procedure of intubation, the need must be fully verified. This factor is also underscored by our data. We found patients intubated at the accident site reached the burn center with a significant median delay of 24 minutes, compared to patients who had not been intubated. Interestingly, Romanowski et al. showed that many burn patients are intubated unnecessarily.27 Unnecessary intubation furthermore represents an avoidable risk.28 Severe complications have been described, like tracheal rupture29,30 or tracheal laceration,31,32 and should be avoided if possible.
Influence of day of the week on time from injury to admission
Minimal information is available regarding the influence of day of the week on transfer time. Since many patients are transported by ambulance, traffic might have an influence on how long it takes. This would also counter a “weekend effect” regarding transport time, since there is often less traffic on weekends. Our data showed there was no statistical difference in time to admission with regard to a specific day of the week. Taira et al. analyzed mortality rates due to the time of admission rather than the difference in transport time between admission during off hours and admission during the week (or weekdays). Nevertheless, no significant differences were found.33 Similar findings were reported by Carmody in California, USA.34 Interestingly, Barnett et al. found a modestly higher risk of mortality and length of hospital stay for patients admitted on the weekend, followed by the patients admitted on a Monday or a Friday. They suggested that less staff might be the reason for their results.35 However, this phenomenon does not seem to have an impact on weekend transfer.
Conclusion
Over the 25 years analyzed, no significant change could be found regarding time to admission. Additionally, we can state that a weekend effect on time to admission could not be confirmed by our data. Furthermore, our data suggests that intubation is a statistically significant time-consuming procedure, and the need for it must be evaluated carefully. We are hopeful that our study will further elucidate published knowledge regarding transfer time from the scene of the accident to admission to the BICU in Germany.
Acknowledgments
Funding.the authors received no financial support for the research, authorship, and/or publication of this article.
Conflict of interest statement.the authors declare no potential conflicts of interest in regard to research, authorship, and/or publication of the article.
References
- 1.Carter JE, Neff LP, Holmes IV JH. Adherence to burn center referral criteria: are patients appropriately being referred? J Burn Care Res. 2010;31:26–30. doi: 10.1097/BCR.0b013e3181cb8efb. [DOI] [PubMed] [Google Scholar]
- 2.Klein MB, Nathens AB, Heimbach DM, Gibran NS. An outcome analysis of patients transferred to a regional burn center: transfer status does not impact survival. . Burns. 2006;32:940–945. doi: 10.1016/j.burns.2006.04.001. [DOI] [PubMed] [Google Scholar]
- 3.Bell N, Simons R, Hameed SM, Schuurman N, Wheeler S. Does direct transport to provincial burn centres improve outcomes? A spatial epidemiology of severe burn injury in British Columbia, 2001–2006. Can J Surg. 2012;55:110–110. doi: 10.1503/cjs.014708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Warden GD. Regionalization of burn care - a concept whose time has come. J Burn Care Res. 2003;24:173–174. doi: 10.1097/01.BCR.0000066784.94077.C6. [DOI] [PubMed] [Google Scholar]
- 5.Gibran NS, Klein MB, Engrav LH, Heimbach DM. UW Burn Center: A model for regional delivery of burn care. Burns. 2005;31:S36–S39. doi: 10.1016/j.burns.2004.10.003. [DOI] [PubMed] [Google Scholar]
- 6.Burn center referral criteria. Chicago: Association AB; 2011. [Google Scholar]
- 7.Büttemeyer R, Steen M, Donnersmarck GHv, Germann G. Establishing a baseline for organisation and outcome in burn care - basic data compiled by German Burn Centres, 1991–2000. Burns. 2004;30:115–120. doi: 10.1016/j.burns.2003.08.008. [DOI] [PubMed] [Google Scholar]
- 8.Rennekampf H, Berger A. Pathophysiologie der Verbrennung. In: Bruck JC, Müller FE, Steen M (Eds) ‘Handbuch der Verbrennungstherapie’, 43-50. Ecomed, Landsberg. 2002 [Google Scholar]
- 9.Hagstrom M, Wirth GA, Evans GR, Ikeda CJ. A review of emergency department fluid resuscitation of burn patients transferred to a regional, verified burn center. Ann Plast Surg. 2003;51:173–176. doi: 10.1097/01.SAP.0000058494.24203.99. [DOI] [PubMed] [Google Scholar]
- 10.Klein MB, Nathens AB, Emerson D, Heimbach DM. An analysis of the long-distance transport of burn patients to a regional burn center. J Burn Care Res. 2007;28:49–55. doi: 10.1097/BCR.0B013E31802C894B. [DOI] [PubMed] [Google Scholar]
- 11.Samuel J, Campbell E, Mjuweni S, Muyco A et al. The epidemiology, management, outcomes and areas for improvement of burn care in central Malawi: an observational study. J Int Med Res. 2011;39:873–879. doi: 10.1177/147323001103900321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Palmer JH, Sutherland AB. Problems associated with transfer of patients to a regional burns unit. Injury. 1987;18:250–257. doi: 10.1016/0020-1383(87)90008-8. [DOI] [PubMed] [Google Scholar]
- 13.Theodorou P, Xu W, Weinand C, Perbix W et al. Incidence and treatment of burns: A twenty-year experience from a single center in Germany. Burns. 2013;39:49–54. doi: 10.1016/j.burns.2012.05.003. [DOI] [PubMed] [Google Scholar]
- 14.Sheridan R, Weber J, Prelack K, Petras L et al. Early burn center transAnnals fer shortens the length of hospitalization and reduces complications in children with serious burn injuries. J Burn Care res. 1999;20:347–350. doi: 10.1097/00004630-199909000-00002. [DOI] [PubMed] [Google Scholar]
- 15.Mlcak R, Cortiella J, Desai MH, Herndon DN. emergency management of pediatric burn victims. Pediatr emerg Care. 1998;14:51–54. doi: 10.1097/00006565-199802000-00013. [DOI] [PubMed] [Google Scholar]
- 16.Fein M, Quinn J, Watt K, nichols t et al. Prehospital paediatric burn care: new priorities in paramedic reporting. Emerg Med Australas. 2014;26:609–615. doi: 10.1111/1742-6723.12313. [DOI] [PubMed] [Google Scholar]
- 17.Singer AJ, Taira BR, thode Jr HC, McCormack Je et al. the association between hypothermia, prehospital cooling, and mortality in burn victims. Acad emerg Med. 2010;17:456–459. doi: 10.1111/j.1553-2712.2010.00702.x. [DOI] [PubMed] [Google Scholar]
- 18.Han T-H, Kim J-H, Yang M-S, Han K-W et al. retrospective analysis of 19,157 burns patients: 18-year experience from Hallym Burn Center in Seoul, Korea. Burns. 2005;31:465–470. doi: 10.1016/j.burns.2004.11.014. [DOI] [PubMed] [Google Scholar]
- 19.Chong S, Song C, Tan T, Kusumawijaja G, Chew K. Multi-variate analysis of burns patients in the Singapore General Hospital Burns Centre (2003–2005). Burns. 2009;35:215–220. doi: 10.1016/j.burns.2008.06.014. [DOI] [PubMed] [Google Scholar]
- 20.Sharma NP, Duke JM, Lama BB, thapa B et al. Asia Pac J Public Health. Vol. 2015. Descriptive epidemiology of unintentional burn injuries admitted to a tertiary-level government hospital in nepal gender-specific patterns. [DOI] [PubMed] [Google Scholar]
- 21.Chipp E, Warner RM, McGill DJ, Moiemen NS. Air ambulance transfer of adult patients to a UK regional burns centre: Who needs to fly? Burns. 2010;36:1201–1207. doi: 10.1016/j.burns.2010.05.023. [DOI] [PubMed] [Google Scholar]
- 22.Ashworth H, Cubison T, Gilbert P, Sim K. treatment before transfer: the patient with burns. Emerg Med J. 2001;18:349–351. doi: 10.1136/emj.18.5.349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cassidy TJ, Edgar DW, Phillips M, Cameron P et al. transfer time to a specialist burn service and influence on burn mortality in Australia and new Zealand: A multi-centre, hospital based retrospective cohort study. Burns. 2015;41:735–741. doi: 10.1016/j.burns.2015.01.016. [DOI] [PubMed] [Google Scholar]
- 24.Slater H, O’Mara M, Goldfarb I. Helicopter transportation of burn patients. Burns. 2002;28:70–72. doi: 10.1016/s0305-4179(01)00069-9. [DOI] [PubMed] [Google Scholar]
- 25.Saffle JR, Edelman L, Morris SE. regional air transport of burn patients: a case for telemedicine? Journal of trauma and Acute Care Surgery. 2004;57:57–64. doi: 10.1097/01.ta.0000103992.21727.8f. [DOI] [PubMed] [Google Scholar]
- 26.Pegg SP, Seawright AA. Burns due to cooking oils - an increasing hazard. Burns. 1983;9:362–369. doi: 10.1016/0305-4179(83)90085-2. [DOI] [PubMed] [Google Scholar]
- 27.Romanowski KS, Palmieri TL, Sen S, Greenhalgh DG. More than one third of intubations in patients transferred to burn centers are unnecessary: proposed guidelines for appropriate intubation of the burn patient. J Burn Care Res. 2015 doi: 10.1097/BCR.0000000000000288. [DOI] [PubMed] [Google Scholar]
- 28.Alanazi A. Intubations and airway management: An overview of Hassles through third millennium. J emerg trauma Shock. 2015;8:99–99. doi: 10.4103/0974-2700.145401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Reichman EF, Lanan BJ. tracheal rupture: A rare complication of endotracheal intubation. Pediatric Emergency Care. 2015 doi: 10.1097/PEC.0000000000000279. [DOI] [PubMed] [Google Scholar]
- 30.Miñambres E, Burón J, Ballesteros MA, Llorca J et al. tracheal rupture after endotracheal intubation: a literature systematic review. eur J Cardio-Thorac Surg. 2009;35:1056–1062. doi: 10.1016/j.ejcts.2009.01.053. [DOI] [PubMed] [Google Scholar]
- 31.Üzümcügil F, Babaoğlu G, Denizci E, Sarıcaoğlu F, Kanbak M. Tracheal laceration as a complication of out-of-hospital emergency tracheal intubation in a patient with COPD. Am J emerg Med. 2015;33:128. e1–128. e3. doi: 10.1016/j.ajem.2014.06.021. [DOI] [PubMed] [Google Scholar]
- 32.Sakles JC, Deacon JM, Bair AE, Keim SM, Panacek EA. Delayed complications of emergency airway management: a study of 533 emergency department intubations. West J emerg Med. 2008;9:190–190. [PMC free article] [PubMed] [Google Scholar]
- 33.Taira BR, Meng H, Goodman MS, Singer AJ. Does “off-hours” admission affect burn patient outcome? Burns. 2009;35:1092–1096. doi: 10.1016/j.burns.2009.04.023. [DOI] [PubMed] [Google Scholar]
- 34.Carmody IC, Belmahos JrGC. Day for night: should we staff a trauma center like a nightclub? Am Surg, 2002;68:1048–1048. [PubMed] [Google Scholar]
- 35.Barnett MJ, Kaboli PJ, Sirio CA, Kaboli PJ, Rosenthal GE. Day of the week of intensive care admission and patient outcomes: a multisite regional evaluation. Med Care. 2002;40:530–539. doi: 10.1097/00005650-200206000-00010. [DOI] [PubMed] [Google Scholar]


