Summary
Burn injuries are a leading cause of morbidity and mortality, with 195,000 deaths annually. This study was conducted to identify the demographics of burn victims and the effect of different variables on the outcome of their injuries. 4016 patients admitted to the Burns Centre, Civil Hospital Karachi from January 2006 to December 2011 were retrospectively analyzed. Demographics, burn injury details and their outcome were recorded in a pre-designed questionnaire. Injuries were categorized as: fire, chemical, scald or electrical. To estimate total body surface area (TBSA) burned in adults, the rule of nines was used. For children and infants, the Lund-Browder chart was employed. SPSS v16.0 software was used for analysis. Frequencies and percentages of all variables, and the measure of central tendencies and dispersion for continuous variables were calculated. Cross tabs were used to assess mortality. Mean age was 28.13 years. More than half of the cases (n=2337, 58.2%) were aged between 16-30 years. Labourers, housewives and students were the most commonly affected groups. Burn injuries by flame/fire and electricity were most common. Most cases were accidental, followed by suicide attempts and homicides. Mean percentage of TBSA affected was 35.49%. Mean duration of hospital stay was 16.45 days. 50.6% of the expired cases were females. The mean age of expired patients was 30.07 while for patients who survived it was 27.01 years. The outcome of burn injuries is related to various demographic factors. Female gender, increasing age, burn injuries following suicide attempts and greater surface area involvement predict poor outcome.
Keywords: burns, electrical burn, inhalation injury, accidental, homicidal, suicidal, hospital stay
Abstract
Les brûlures sont l’une des principales causes de morbidité et de mortalité avec 195.000 morts annuellement. Cette étude a été entreprise pour identifier les facteurs démographiques des patients brûlés et les différentes variables sur les résultats thérapeutiques. 4016 patients ont été admis au Centre des Brûlés de l’Hôpital Civil de Karachi de janvier 2006 à décembre 2011 et leurs dossiers furent analysés rétrospectivement. Les facteurs démographiques, les détails de la brûlure et les résultats furent enregistrés sur un questionnaire; la cause étiologie de la brûlures était précisée: feu, chimique, ébouillantement, électrique. Pour évaluer la surface brûlée corporelle (TBSA), c’est la règle des 9 qui était utilisée chez les adultes, et la règle de Lund et Browder chez les enfants. SPSS v16.0 fut utilisée pour l’analyse. La fréquence et les pourcentages de tous les facteurs et la mesure des constantes et leur variation étaient calculées. Cross tabs furent utilisées pour évaluer la mortalité. La moyenne d’âge était de 28 ans; plus de la moitié des cas (n=2337, 58.2 %) étaient âgés de 16 à 30 ans. Ouvriers, femmes au foyer, et étudiants constituaient le groupe le plus important. Les brûlures par flamme et électriques étaient les plus fréquentes. La plupart des cas était de cause accidentelle, suivi par les tentatives de suicide, et les homicides. Le pourcentage moyen (TBSA) était de 35.49%. La moyenne du temps d’hospitalisation était de 16,45 jours. 50.6% des cas mortels étaient des femmes. L’âge moyen des patients décédés était de 30.07, alors que celle des survivants était de 27.01 années. Le résultat du traitement des brûlures dépend des divers facteurs démographiques. Le sexe féminin, le grand âge, les brûlures lors de tentatives de suicide, et les brûlures de grande surface sont de mauvais pronostic.
Introduction
Burn injuries are one of the leading causes of morbidity and mortality in the Eastern Mediterranean region of the World Health Organization (WHO).1,2 An estimated 195,000 deaths are caused by burns every year, and the vast majority of those deaths occur in developing countries.1,2,3 According to a systemic analysis by Othman et al., the incidence of burn injuries ranged from 112 to 518 per 100,000 per annum.3
In contrast to the developed world, where much has been accomplished in the primary and secondary prevention of burn injuries, developing countries like Pakistan lack adequate knowledge of epidemiological characteristics and associated risk factors and, thus, a sound infrastructure to prevent burn injuries.4 Several factors have been said to be associated with high incidence of burn injuries in developing countries, such as high population density, illiteracy and poverty.5
According to WHO, women in the South-East Asia Region have the highest incidence of burn injuries, accounting for 27% of deaths by burn injuries globally, and nearly 70% of burn deaths in the region.1,2 A study by Panjeshahin et al. reports that burn injuries were more frequent and larger with higher mortality in females than in males, and young females aged 20-29 years were most commonly inflicted.6 There is disagreement in the literature; according to some, children are the most vulnerable group, accounting for almost 50% of all burn patients.7 Othman et al. reported that approximately one third of victims were children aged 0-5 years.3
Outcome of burn injuries depends on many factors: the percent of total body surface area burned; the percent of fullthickness burn size; the presence of an inhalation injury, age and gender of the victims.8 According to Osler et al., age and burn percent are equally important in predicting mortality.9 Ryan et al. identified three risk factors for death: over 60 years of age, more than 40 percent of body-surface area burned, and inhalation injury.10
Burn injuries are most commonly due to flame and scalds. There is disagreement in the literature as to which is the most common cause of burns injuries.11,12 The most infrequent burns are those caused by electrocution and chemical injuries.11
Not only are burn injuries fatal, but they are also a leading cause of morbidity, including prolonged hospitalization, disfigurement and disability, often with resulting stigma and rejection. 1,2 Survivors of non fatal burns are burdened with lifelong physical and emotional scars.6 WHO reports that burns are among the leading causes of disability-adjusted life-years (DALYs) lost in low- and middle-income countries. In Bangladesh, Colombia, Egypt and Pakistan, 17% of children with burns have a temporary disability and 18% have a permanent disability.1,2
The Burns Centre in Karachi is the only specialized burn care unit in the province of Sindh, where patients from all over the country are catered for, managed and treated for burn injuries and their sequelae. This study was conducted to identify the demographic profile of the burn victims, and also the extent, the mode and cause of their injury. Moreover, the aim was to identify those factors such as age, gender, percentage of burn, mode and cause of burn that affect the outcome of the burn injuries.
Methods
This was a retrospective analysis of 4016 patients who presented with burn injury and were admitted, managed and treated at the Burns Centre, Karachi over a period of six years, from January 2006 to December 2011.
A pre-designed questionnaire was used to record the demographic details of the patients, such as their age, gender and residence. Detailed descriptions of the cause, percent of area affected and mode of the burn injury, along with duration of stay at the center, were also recorded. The outcome of the patient after treatment was recorded under the headings: treated and discharged, left against medical advice or dead.
Burn injury was defined as an injury to the skin or any tissue or organ primarily caused by heat or due to radiation, radioactivity, electricity, friction or contact with chemicals. Skin injuries due to ultraviolet radiation, radioactivity, electricity or chemicals, as well as respiratory damage resulting from smoke inhalation, were also considered to be a burn injury.13
Total body surface area (TBSA) burned was calculated using the rule of nines in adults, while in children and infants the Lund-Browder chart was used to assess the burned body surface area.14
Data was entered and analyzed using SPSS v16.0 software.
Simple frequencies and percentages were calculated for most of the variables. For continuous variables like age and duration of hospital stay, measures of central tendency and dispersion were calculated. Cross tabs were made employing chi-square test to calculate the association of age, gender, cause, mode of burns and TBSA burnt with mortality from burn injury. Cross tabs were also made between duration of stay and TBSA affected. Normality of continuous variables was assessed by Kolmogorov-Smirnov’s test and all variables were found skewed. Therefore, the Mann-Whitney test was performed to compare demographic and clinical variables of participants who survived and those who expired. Spearman’s correlation was used to assess the association between continuous variables. The variables which appeared to display significant association in univariate analyses were included in multivariate stepwise Cox regression model for assessing risk factors for the death of patients. A P value less than 0.05 was considered to show a significant effect of the variables.
Results
Out of a total 4016 burn victims, the majority (n=2272, 56.6%) were male. Mean age of the participants was 28.13 ± 13.16 years. Most cases (n=2337, 58.2%) fell in the 16-30 yearold age category, followed by those who were aged between 31-45 years, accounting for up to 871 (21.7%) cases. 453 (11.3%) cases were aged between 1-15 years, while 262 (6.5%) were aged between 46-60 years. 74 (1.8%) cases were aged 61-75 years, and only 19 (0.5%) were aged over 75 years.
Labourers (n=1301, 32.4%), housewives (n=1293, 32.2%) and students (n=1036, 25.8%) most commonly suffered burn injuries, followed by less common categories like electricians (n=199, 5.0%) factory workers (n=63, 1.6%), unemployed (n=28, 0.7%) and others (n=96, 2.4%).
Most burns were due to flames/fire (n=3370, 83.9%), followed by electrical burns (n=318, 7.9%) and chemical burns (n=121, 3.0%). Scalds (n=205, 5.1%) were low on the list. Accidental burns were most common (n=3885, 96.7%) followed by burns due to suicide attempts (n=114, 2.8%) and homicide (n=17, 0.4%).
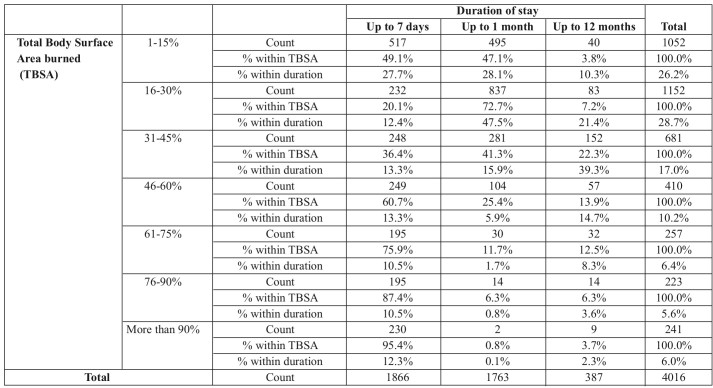
The mean percentage of total body surface area affected was 35.49 ± 27.26%. Percentage of total body surface area (TBSA) burned was categorized as: 1-15%, 16-30%, 31-45%, 46-60%, 61-75%, 76-90% and more than 90%. A little over 50% of the cases had TBSA burned in the range of 1-30%. Only 6% of cases had more than 90% TBSA burned (Fig. 1).
Fig. 1. Total Body Surface Area burned (in percent).
The average duration of stay in hospital was 16.45 ± 19.645 days. Most patients stayed for up to one week (n=1866, 46.5%), followed by up to one month (n=1763, 43.9%) and finally for up to one year (n=387, 9.6%).
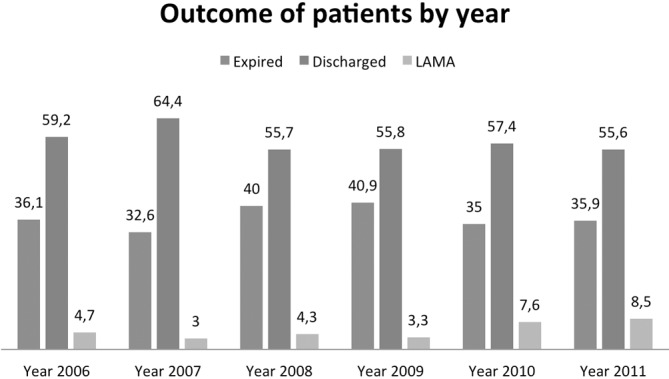
The outcome of the patients was categorized as; discharged and treated (n=2323 57.8%), left against medical advice (LAMA) (n=211, 5.3%) and expired (n=1482, 36.9%). Fig. 2 summarizes the outcome of the patients by year.
Fig. 2. Total Body Surface Area burned (in percent).
50.6% (p value<0.001) of the expired cases were females. A greater percentage of female patients expired compared to males, i.e. 43.1% against 32.4%. Most expired cases (59.9% p value<0.001) were aged between 16-30, followed by those aged between 31 and 45 years (22.1% p value<0.001). 93.5% (p value<0.001) of the expired cases were injured by flame/fire, followed by electricity (3.2% p value<0.001) and scalds (2.3% p value<0.001). In terms of mortality rate, fire/flame burns were the deadliest. 41.3% cases of fire burn expired as opposed to 15.1% cases who were burnt by electricity and 11.6 % cases of chemical burn. 16.6 cases affected by scald expired.
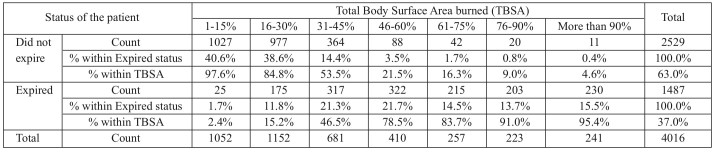
Mode of injury was significantly associated with outcome, as 77.2% (p value<0.001) of the suicide attempts and 64.7% (p value<0.001) of homicidal burns expired, while only 35.7% (p value<0.001) of the accidental cases of burns expired. 49.1% (p value<0.001) and 47.1% (p value<0.001) cases with TBSA 1-15% stayed in hospital for up to one week and one month respectively. 72.7% (p value<0.001) cases with TBSA 16-30% stayed for up to a month. 60.7% (p value<0.001) cases with 46-60% TBSA stayed for up to a week. Most cases with TBSA over 60% stayed for up to a week (Table I).
Table I. Cross tab between Total Body Surface Area and duration of stay.
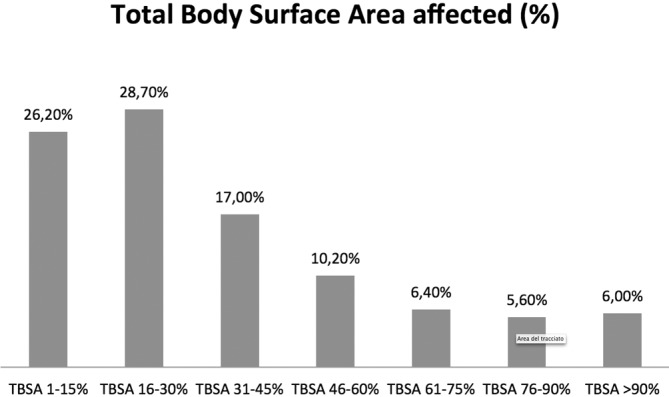
Percentage of mortality was highest (95.4% p value<0.001) among those with more than 90% total body surface area burned, followed by 76-90% (91.0% p value<0.001) and 61-75% (83.7% p value<0.001) (Table II).
Table II. Cross tab between Total Body Surface Area burned with outcome of the patient in terms of mortality.
Those who expired were older than those who were discharged or LAMA (P < 0.0001). The mean age of expired patients was 30.07 ± 13.85 with median 27 (15) while for surviving patients it was 27.01 ± 12.61 and 25 (15.25) respectively. Most patients expired within a week (mean: 7.30 ± 11.18, median: 4.5 (5)) whereas, the duration of treatment of survivng patients was 2 to 3 weeks (mean: 21.80 ± 21.47, median: 15 (15)). The statistical results also implied highly significant difference in the duration of stay and the outcome of the patients (P < 0.0001). TBSA burnt was 21.62% ± 15.62% in patients who survived. In comparison, TBSA affected was much higher in expired patients (P < 0.0001).
The correlation analysis showed that higher age was associated with higher percentage of burn, and percentage of burn was negatively associated with duration of treatment (r = - 0.225, P < 0.001).
The significant factors age, gender, occupations, type of burn, mode of burn and percentage of burn were included in a multivariate regression model. Using stepwise regression, age, gender, mode and percentage of burns were found to be significant predictors. Females had a 1.25-times higher risk of dying than males. After 31 years of age, the risk of mortality increased significantly. The victims with 16–30% TBSA had a 4.86-times greater risk of dying than those with TBSA less than 15%. Similarly, victims with 30-45% TBSA had a 16.02-times greater risk, while patients with over 90% TBSA were 98.66- times more likely to die.
Discussion
Burn injuries are a considerable cause of both mortality and morbidity, leaving the victims with lifelong physical, psychological and emotional disability.1 We conducted this study to identify the pattern of burn injuries in Karachi, and the most important factors associated with outcome of burn injuries.
In our study, male to female ratio of the burn victims was nearly 1:1. This is in contrast to WHO reports that 70% of burn deaths in South East Asia are women.1 However, reports from India, a developing country like ours with a similar cultural and social background, are consistent with our findings.13,14
Most cases (58.2%) in our study were aged 16-30 years, followed by those aged between 31-45 years. A study by Gupta et al. reported that the majority (79%) of the cases were in the 15-45 age group.15 Shanmugakrishnan et al. reported that men in the 25-34 age group and women aged 15-24 years suffered from burns significantly more than the other age group.16 We therefore conclude that people aged 16-45 years are more likely to suffer from burn injuries than any other age group.
Labourers and housewives were the most commonly affected group in our study. This may be attributable to the absence of safety measures and poor fire control measures in our setup. According to Gupta et al., 72% sustained burns in a closed space, 52% of them in the kitchen.15 Song et al. reported a reduction of 9.5% in occupational burns due to an improvement in fire prevention and management in the industrial sector. 12 Significant decrease in burn injuries can be achieved by strict legislation and implementation of fire control measures, especially in the industrial sector. Fires at home can be prevented by using safe stoves and educating women about safety measures while cooking. According to Shanmugakrishnan et al., flame burns were accidental in 45 cases: 24 of them were due to a kerosene stove explosion, and 10 people sustained burns while cooking food using firewood.16
The burns were most commonly due to flames/fires (83.9%), followed by electrical burns (7.9%) and chemical burns (3.0%). Scalds (5.1%) were low on the list. This is consistent with a study by Gupta et al.15 However, according to Song et al., scalds were the most common cause of burn, followed by flames,12 and those caused by electrocution or chemicals were most infrequent.11 Relatively speaking, a large number of chemical and electrical burns may be explained by a lack of safety measures taken by electricians and factory workers at work.
In our study, accidental burns were most common (96.7%), followed by suicide (2.8%) and homicide attempt burns (0.4%). Our findings are consistent with previous literature,17,18 and they stress the need for safety measures and proper infrastructure to prevent accidental burns, at home and at work.
In most cases (28.7%), total body surface area (TBSA) burned was 16-30%. Mean percentage of total body surface area burned was 35.49 ± 27.276%, which is consistent with a study by Lari et al., that reported mean body surface area burned to be 30.6%.18
According to our study, most patients (46.5%) stayed in hospital for up to one week, followed by those who stayed up to one month (43.9%), and mean duration of stay in the hospital was 16.45 ± 19.645 days. Lari et al. reported a mean stay of 16.7 days.18
57.8% cases were discharged and 36.9% cases expired. A study by Subrahmanyam et al.17 reported 56.5% mortality, while another study by Soltani et al.19 reported 51% mortality in males and 69% in females. Our study reported a much lower mortality rate than the aforementioned studies.
Groohi et al. reported that female gender is associated with high mortality in burn victims.20 In our study, females were at higher risk of mortality than males. Our findings are thus consistent with previous literature.6,20,21
Mortality was significantly associated with homicide and suicide burns. A systemic review by Othman et al. reported that intentional self-harm burns, particularly involving women, were associated with a very high mortality of up to 79%.3 Thus, mode of burn injury is an important factor in determining the outcome of patients. Our study reported that 77.2% of the cases with self-inflicted burns expired.
Percentage of mortality was highest (95.4%) among those with TBSA of more than 90%, followed by those with a burned area ranging between 76-90% (91.0%) and 61-75% (83.7%). TBSA and depth of burn are perhaps the most important predictors of survival.22 Othman et al. reported the same.3 Shanmugakrishnan et al. reported that none of the cases with TBSA<30% died, while all those with >55% TBSA burns died.16 Thus, TBSA burnt is an extremely important factor in predicting the outcome of burn victims.
Age is also an important factor in determining the outcome of burn injuries, and according to Osler et al., age is as important as TBSA in predicting the outcome of patients.9 Our results show that the chances of dying increased significantly after 31 years of age. Similar to our findings, Panjeshahin et al. reported that mortality was highest in the elderly aged over 80.6
Attia et al. summarized the following factors that affect outcome in burn patients and are associated with increased mortality: age over 60 years, TBSA burnt, female gender, depth of burn and delay in receiving medical care affect the outcome of the patients and are associated with increased mortality.22 Groohi et al. reported that TBSA, flame, female gender and age are associated with mortality in burn victims.20 Our results are, in general, consistent with previous literature.
A possible limitation in our study was that there was no information available on the depth of burn and presence or absence of inhalation injury. Moreover, information on the site of the body affected by burns was also not available.
References
- 1.World Health Organization, Fact sheet N°365. [Internet] Available from: http://www.who.int/mediacentre/factsheets/fs365/en/ [Google Scholar]
- 2.Al-Ibran E., Rao M.H., Ali S.A., Saleem A. Epidemiologic Profile and Outcome of Hospitalized Burn Patients: 5 Year Experience at Burns Centre, Civil Hospital, Karachi. Journal of the Dow University of Health Sciences Karachi. 2012;6 (1):29–31. [Google Scholar]
- 3.Othman N., Kendrick D. Epidemiology of burn injuries in the East Mediterranean Region: a systematic review. BMC Public Health. 2010;10 doi: 10.1186/1471-2458-10-83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Forjuoh SN. Burns in low- and middle-income countries: a review of available literature on descriptive epidemiology, risk factors, treatment, and prevention. Burns. 2006;32(5):529–537. doi: 10.1016/j.burns.2006.04.002. [DOI] [PubMed] [Google Scholar]
- 5.Ahuja RB, Bhattacharya S. Burns in the developing world and burn disasters. BMJ. 2004;21:447–449. doi: 10.1136/bmj.329.7463.447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Panjeshahin MR, Lari AR, Talei A, Shamsnia J, Alaghehbandan R. Epidemiology and mortality of burns in the South West of Iran. Burns. 2001;27(3):219–226. doi: 10.1016/s0305-4179(00)00106-6. [DOI] [PubMed] [Google Scholar]
- 7.Dissanaike S, Rahimi M. Epidemiology of burn injuries: highlighting cultural and socio-demographic aspects. Int Rev Psychiatry. 21(6):505–511. doi: 10.3109/09540260903340865. [DOI] [PubMed] [Google Scholar]
- 8.O’Keefe GE, Hunt JL, Purdue GF. An evaluation of risk factors for mortality after burn trauma and the identification of gender-dependent differences in outcomes. J Am Coll Surg. 2001;192(2):153–160. doi: 10.1016/s1072-7515(00)00785-7. [DOI] [PubMed] [Google Scholar]
- 9.Osler T, Glance LG, Hosmer DW. Simplified estimates of the probability of death after burn injuries: extending and updating the baux score. J Trauma. 2010;68(3):690–697. doi: 10.1097/TA.0b013e3181c453b3. [DOI] [PubMed] [Google Scholar]
- 10.Ryan CM, Schoenfeld DA, Thorpe WP, Sheridan RL et al. Objective estimates of the probability of death from burn injuries. N Engl J Med. 1998;338(6):362–366. doi: 10.1056/NEJM199802053380604. [DOI] [PubMed] [Google Scholar]
- 11.Hettiaratchy S, Dziewulski P. ABC of burns. Introduction. BMJ, 2004;328:1366–1368. doi: 10.1136/bmj.328.7452.1366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Song C, Chua A. Epidemiology of burn injuries in Singapore from 1997 to 2003. Burns. 2005;31 Suppl 1:S18–S26. doi: 10.1016/j.burns.2004.10.005. [DOI] [PubMed] [Google Scholar]
- 13.World Health Organization. Burns. [Internet] Available from: http://www.who.int/violence_injury_prevention/other_injury/burns/en/ [Google Scholar]
- 14.Wolfson AB, Hendey GW, Ling LJ, Rosen CL et al (eds) A clinicoepidemiologic study of 892 patients with burn injuries at a tertiary care hospital in Punjab, India. J Emerg Trauma Shock. 2011;4(1):7–11. doi: 10.4103/0974-2700.76820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gupta AK, Uppal S, Garg R, Gupta A, Pal R. A clinicoepidemiologic study of 892 patients with burn injuries at a tertiary care hospital in Punjab, India. J Emerg Trauma Shock. 2011;4(1):7–11. doi: 10.4103/0974-2700.76820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shanmugakrishnan RR, Narayanan V, Thirumalaikolundusubramanian P. Epidemiology of burns in a teaching hospital in south India. Indian J Plast Surg. 2008;41(1):34–37. doi: 10.4103/0970-0358.41108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Subrahmanyam M. Epidemiology of burns in a district hospital in western India. Burns. 1996;22(6):439–442. doi: 10.1016/0305-4179(96)00001-0. [DOI] [PubMed] [Google Scholar]
- 18.Lari AR, Alaghehbandan R, Nikui R. Epidemiological study of 3341 burns patients during three years in Tehran, Iran. Burns. 2000;26(1):49–53. doi: 10.1016/s0305-4179(99)00102-3. [DOI] [PubMed] [Google Scholar]
- 19.Soltani K, Zand R, Mirghasemi A. Epidemiology and mortality of burns in Tehran, Iran. Burns. 1998;24(4):325–328. doi: 10.1016/s0305-4179(98)00017-5. [DOI] [PubMed] [Google Scholar]
- 20.Groohi B, Rossignol AM, Barrero SP, Alaghehbandan R. Suicidal behavior by burns among adolescents in Kurdistan, Iran: a social tragedy. Crisis. 2006;27(1):16–21. doi: 10.1027/0227-5910.27.1.16. [DOI] [PubMed] [Google Scholar]
- 21.Anlatici R, Ozerdem OR, Dalay C, Kesiktaş E et al. retrospective analysis of 1083 Turkish patients with serious burns. Part 2: burn care, survival and mortality. Burns. 2002;28(3):239–243. doi: 10.1016/s0305-4179(02)00030-x. [DOI] [PubMed] [Google Scholar]
- 22.Attia AF, Sherif AA, Mandil AM, Massoud MN et al. Epidemiological and sociocultural study of burn patients in Alexandria, Egypt. Eastern Mediterranean Health Journal. 1997;3(3):452–461. [Google Scholar]