Summary
Intra-venous (IV) burn resuscitation is effective; nevertheless it has its disadvantages. WHO Oral Rehydration Solution (ORS) has shown high effectiveness in treating dehydration. WHO-ORS, with salt supplement, seems to be suitable for burn resuscitation, where IV resuscitation is not available, feasible or possible. The objective of the study was to evaluate acute phase efficacy and safety, as well as limitations and complications of burn resuscitation using WHO-ORS and salt tablets. This randomized controlled clinical trial was conducted in the Burn Unit, Suez Canal University Hospital, Ismailia, Egypt. The study group was given WHO-ORS (15% of body weight/day) with one salt tablet (5gm) per liter according to Sørensen’s formula. The control group was given IV fluids according to the Parkland formula. Patients’ vital signs and urine output were monitored for 72 hours after starting resuscitation. Both groups were comparable regarding age, sex, and percentage, etiology and degree of burns. For all assessed parameters, there were no major significant differences between the study group (10 cases) and control group (20 cases). Even where there was a significant difference, apart from blood pressure in the first hour of the first day, the study group never crossed safe limits for pulse, systolic blood pressure, urine output, respiratory rate and conscious level. WHO-ORS with 5gm salt tablets, given according to Sørenson’s formula, is a safe and efficient alternative for IV resuscitation. It could even be a substitute, particularly in low resource settings and fire disasters.
Keywords: burn resuscitation, oral, WHO-ORS, salt supplement, clinical trial, Sørensen’s formula
Abstract
La réanimation hydro-électrolytique IV initiale des brûlés est efficace mais connaît des effets indésirables. La SRO de l’OMS a montré son efficacité dans le traitement des déshydratations. Cette solution, supplémentée en sel, semble être utilisable pour la réanimation initiale des brûlés lorsque la voie IV n’est pas utilisable. Une étude randomisée prospective a été réalisée dans le CTB du CHU Canal de Suez d’Ismaïlia. Elle avait pour but d’analyser l’efficacité, l’innocuité, les limites et les complications de l’utilisation de la SRO supplémentée en sel dans la réanimation initiale des brûlés. Le groupe à l’étude (10 patients) recevait 15% de son poids de SRO par jour, additionné de 5 g de sel par litre (formule de Sørensen) quand le groupe contrôle (20 patients) était réanimé par voie IV selon la formule de Parkland. Les patients étaient monitorés (paramètres vitaux, diurèse) pendant 72 h. Les groupes étaient comparables en termes de l’âge, du sexe, de la surface, de la profondeur et de la cause de la brûlure. Il n’y avait pas de différence majeure entre les 2 groupes, exceptée une PA plus basse durant la première heure dans le groupe SRO. Il n’a pas été observé, dans ce groupe, d’anomalie dangereuse le la fréquence cardiaque, le la pression artérielle systolique, de la diurèse, de la fréquence respiratoire ni de l’état de conscience. La solution SRO de l’OMS additionnée de 5 g de sel, délivrée selon la formule de Sørensen, est une alternative efficace et sûre à la réanimation IV initiale des brûlés, qu’elle pourrait remplacer dans les pays à IDH bas et en cas de catastrophe.
Introduction
Burn injuries are among the most devastating of all injuries and a major global public health crisis.1,2 They are the fourth most common type of trauma worldwide.3 Burn is a trauma linked to poverty; approximately 90 percent of burns occur in Low and Middle Income Countries (LMICs), and in the poor areas of High Income Countries (HICs).4
All formulas used for burn resuscitation worldwide are through intra-venous (IV) routes: they differ in volume, sodium and colloid content. The disadvantages of IV resuscitation are chemical and mechanical irritation, circulatory overload leading to fluid creep, as well as cannula site infection causing thrombophlebitis/phlebitis, sepsis and even septic shock. Moreover, it is not convenient in mass casualties and disasters.5
Enteral resuscitation has been evaluated in a few articles.6 Although old and with several limitations, these studies appear to have established, to variable degree, the effectiveness and value of enteral resuscitation.
One of the most important references for oral resuscitation is Sørensen.7 In 1966, he sought a simple and fast means to treat mass casualties due to thermal nuclear warfare, namely drinking any beverage with 5gm salt tablets per liter of fluid drunk. Sørensen calculated the amount according to body weight (not including TBSA) and days since burn. Eighty percent of his patients with burns as large as 45% TBSA required no IV support.
WHO Oral Rehydration Solution (WHO-ORS), known to be highly effective in the treatment of dehydration in epidemics of cholera, was effective in treating moderate burn shock in the only study done using it.8
Based on previous studies, it seems that WHO-ORS with salt supplement could be a convenient alternative for burn resuscitation; particularly where IV resuscitation is not available, not feasible or not possible.
Study objective
The objective was to assess efficacy and safety, as well as limitations and complications of oral resuscitation using WHOORS and 5gm salt tablets compared to intravenous Parkland formula in the acute phase, i.e. the first 72 hours after burn injury, in adult patients with burns covering more than 15% TBSA.
Patients and methods
Type of study: Randomized controlled clinical trial.
Study Place: Burn Unit of Suez Canal University Hospital, Ismailia, Egypt.
Study Population: Adult patients with fresh burn, more than 15% TBSA.
Sample size: All eligible patients attending the Burn Unit in a 12-month period (from 1st February 2014 to 1st February 2015).
Inclusion criteria:
Age: 13 years and older (adults according to Lund and Browder chart).
Both genders.
Fresh burn: presenting within 6 hours after the accident.
Physical burns (flame and scald burn).
Exclusion criteria:
Patients with co-morbidities (diabetes mellitus, hypertension, renal failure, ischemic heart disease & chronic liver disease).
Inhalation injury.
Associated injuries (multiple trauma, internal hemorrhage ... etc.).
Pregnancy and lactation.
Study methods:
After obtaining approval from the Local Ethics Committee patients were randomly allocated to one of two equal groups on an alternate basis.
Patients were subjected to routine assessments and care including:
history-taking, including mechanism of burn;
clinical examination, including burn wound assessment;
weighing the patient and insertion of silicone urinary catheter;
laboratory investigations: complete blood picture, sodium, potassium, blood urea and serum creatinine.
According to the group the patients were allocated to, the treatment was as follows:
1. Control (IV) group: Resuscitated according to the Parkland formula.
First 24 hours: 4 ml/kg/% burn using Ringer lactate solution.
Second 48 hours;
Crystalloid: 1ml/Kg/% burn Ringer’s lactate solution.
Colloid: 10 – 30ml/Kg/day Dextran 70.
Glucose 5%: 2500 ml/day.
2. Study (oral) group: Resuscitated according to Sørensen’s formula.
First 24 hours: 150-200 ml /kg.
Second 24 hours: 100-150 ml /kg.
Five sachets of WHO-ORS (commercial name in Egypt is Rehydran-n) were added to one liter of water and given, through a nasogastric tube, with a 5gm salt tablet hourly.
Composition of Rehydran – n:
Glucose anhydrous........................4.00 g.
Tri-sodium citrate anhydrous.........0.51 g.
Sodium chloride.............................0.70 g.
Potassium chloride.........................0.30 g.
Patients were encouraged to drink any amount of any type of fluid they wanted per os, in addition to the mentioned basic supply.
We started with the minimum: 150 and 100 for the first and second days respectively. We decided to increase the amount by 10ml/Kg/day if the amount was insufficient. Patients were given their basic hourly requirements as a bolus dose of 1/6 of the amount every 10 minutes. The stomach was aspirated hourly to detect any residuals.
All the patients had been drinking supplementary fluids; therefore we did not increase the amount. Unfortunately, we did not collect any data concerning the nature or amount of supplementary fluids drunk by the patients. Similarly, as our focus was only on safety and effectiveness, no parameters other than basic monitoring were assessed, including patient weight or stool volume output. Due to limited resources, Central Venous Pressure (CVP), arterial blood gases, blood electrolytes and urinary/serum sodium were not measured unless there was a persistent bed-side monitoring anomaly for more than 2 consecutive hours. Invasive monitoring equipment is not available in our unit.
Patient monitoring
Both groups were similarly monitored to assure that each patient’s condition was stable and that resuscitation was sufficient and effective. The monitoring scheme followed in the burn unit, with the critical value for each parameter, is:
Heart rate: less than 100 beats/minute.
Blood pressure: systolic blood pressure more than 100 mmHg.
Urine output: 0.5 - 1 ml/kg/hr.
Level of consciousness: clear (using the AVPU scale).
Respiratory rate: 12 – 20 breaths/minute.
To assure the safety of the study group, patients were monitored hourly for vomiting, distention and gastric residual volume. In addition, an end point for the study was determined: this was persistence of one of the following parameters for more than three consecutive hours, or two of them for more than two consecutive hours. These three parameters were:
pulse rate more than 100/min;
systolic blood pressure less than 100mmHg;.
urine output less than 0.3ml/Kg/h.
None of these parameters was persistent, or even detected after the second hour of starting treatment.
Results
The control group comprised 20 patients versus 10 patients in the study group. This discrepancy was due to a high rate of patients refusing to be allocated to the study group.
Table I shows that patients of both groups were comparable with no significant difference in age, gender or weight. Similarly, Table II demonstrates that both groups were comparable in burn injury parameters regarding percentage, etiology and degree. Regarding degree, all the patients had mixed burns; they were classified either second or third degree according to the prevalent degree.
Table I. Characteristics of the patients of both groups.
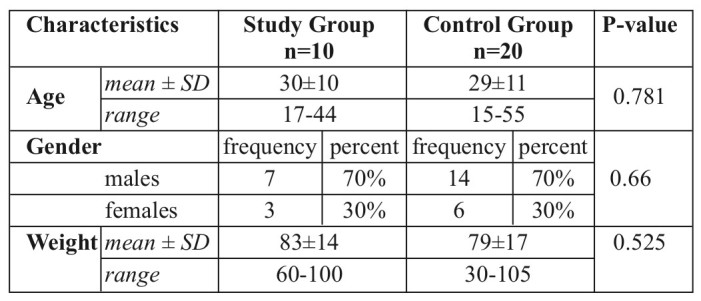
Table II. Comparison of burn details between study and control group.
For the study parameters, in an attempt to overcome the relatively small sample size, we used Mann Whitney U value for significance as it is non-parametric and has more statistical power than the classic student t-test. It was also more appropriate as it ignores any empty or non-numeric cells and allows comparison without making the assumption that values are normally distributed - which might be the case in our study
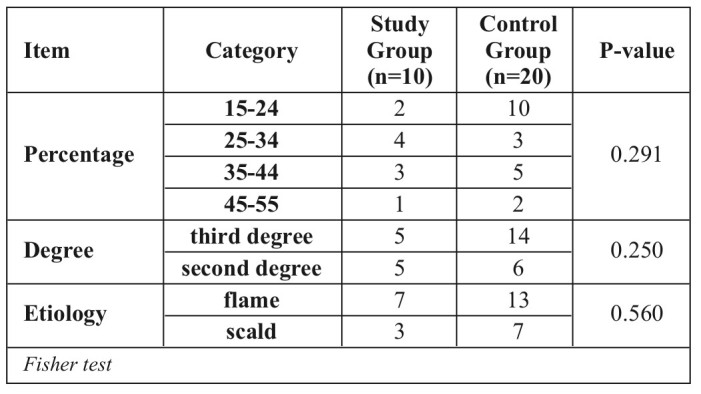
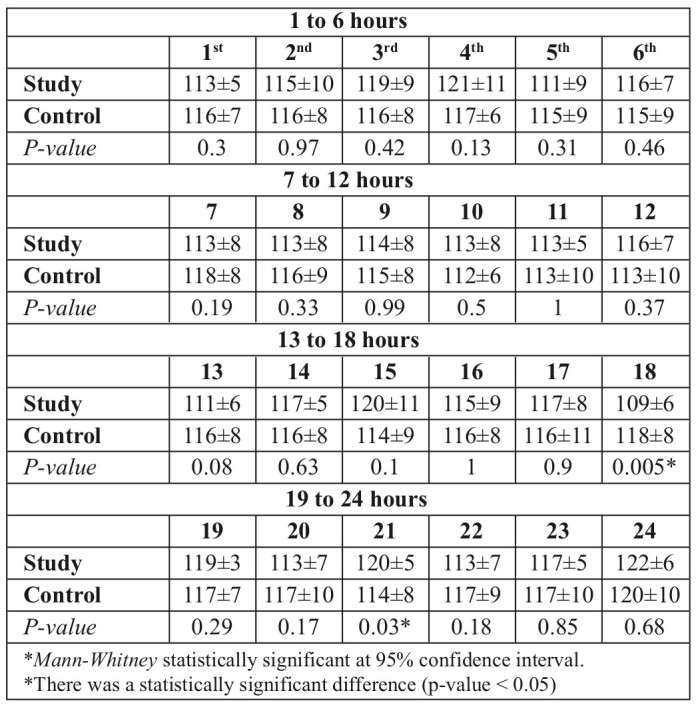
Tables III, IV and V compare mean systolic blood pressure (SBP) in both groups throughout the study period (72 hours after starting treatment). In Table III, significant lower values were evident in the study group in the 1st, 7th and 19th hour. The first hour was the only period when SBP passed the critical limit of below 100mmHg. On the second and third day, although there was a significantly lower value of mean SBP in one reading each in the study group, the value did not fall below the critical limit
Table III. Mean systolic blood pressure in both groups on the first day.
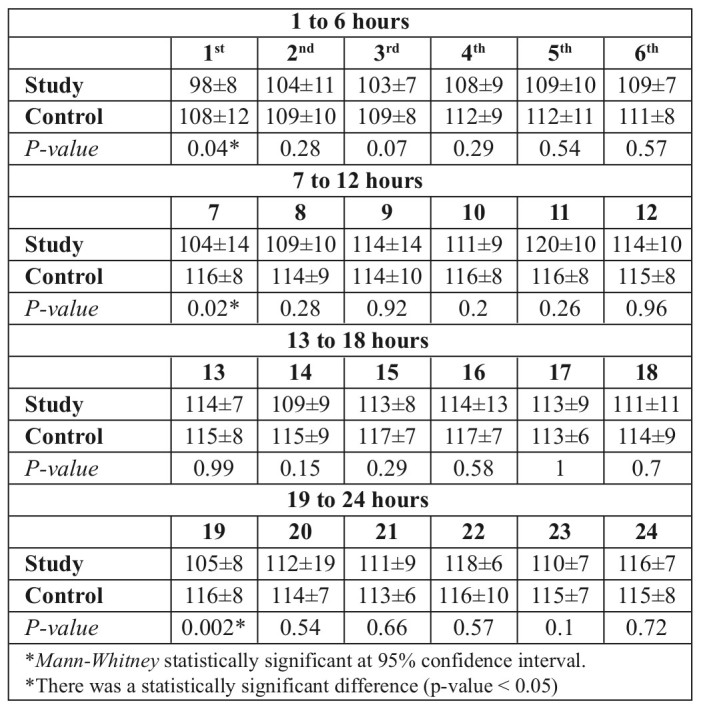
Table IV. Mean systolic blood pressure in both groups on the second day.
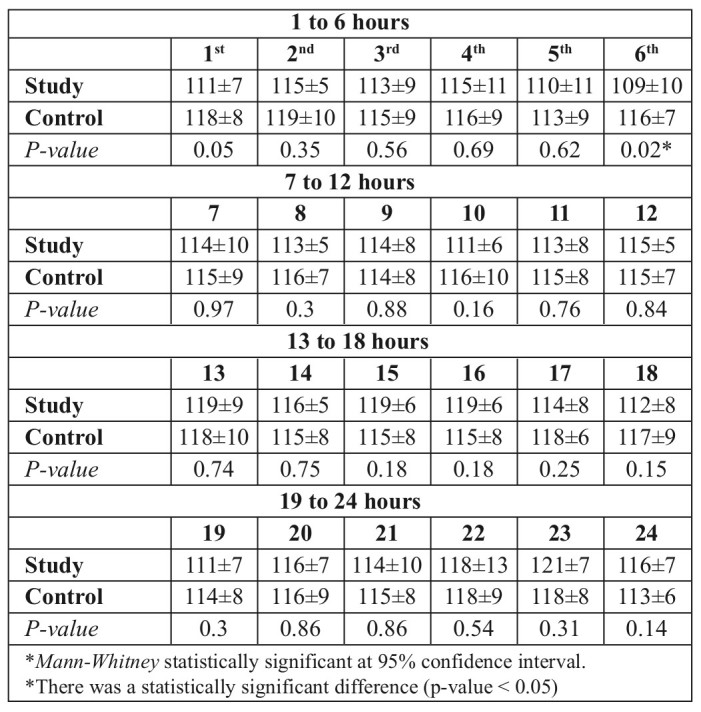
Table V. Mean systolic blood pressure in both groups on the third day.
Similarly, Tables VI, VII and VIII show only a few sporadic significant lower values for mean pulse in the study group. On the contrary, no value exceeded the critical value of 100/min.
Table VI. Mean pulse in both groups on the first day.
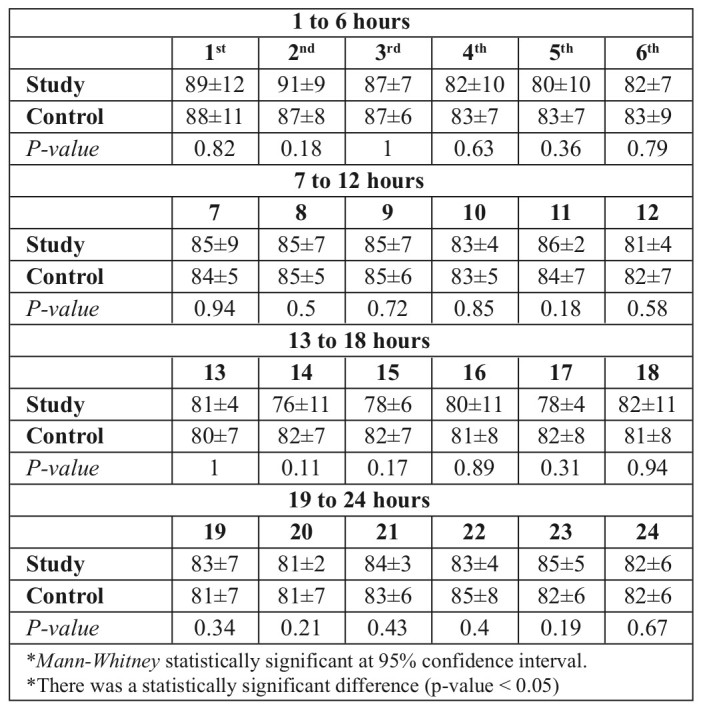
Table VII. Mean pulse in both groups on the second day.
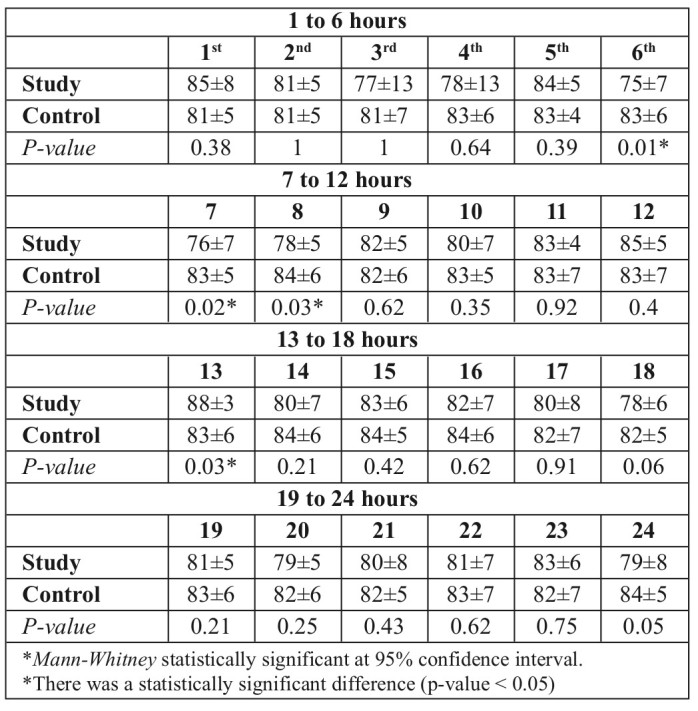
Table VIII. Mean pulse in both groups on the third day.
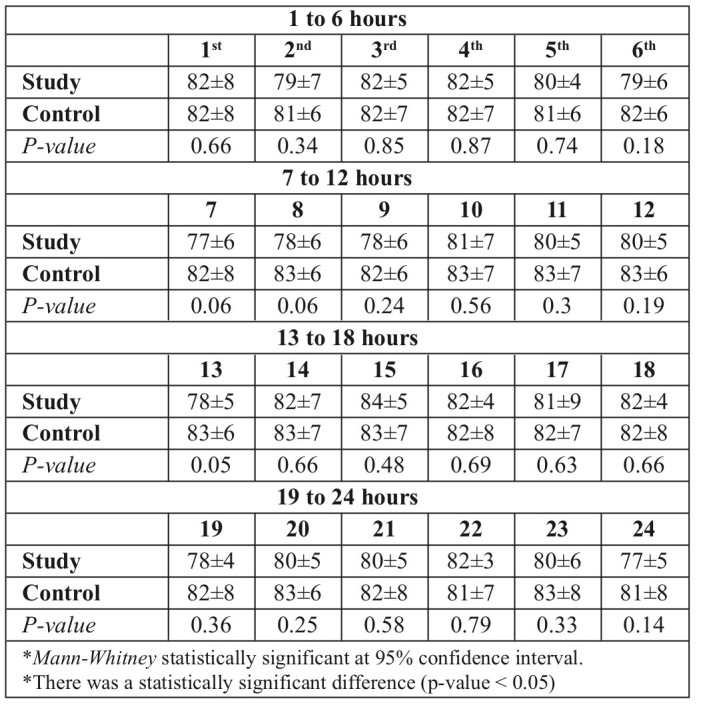
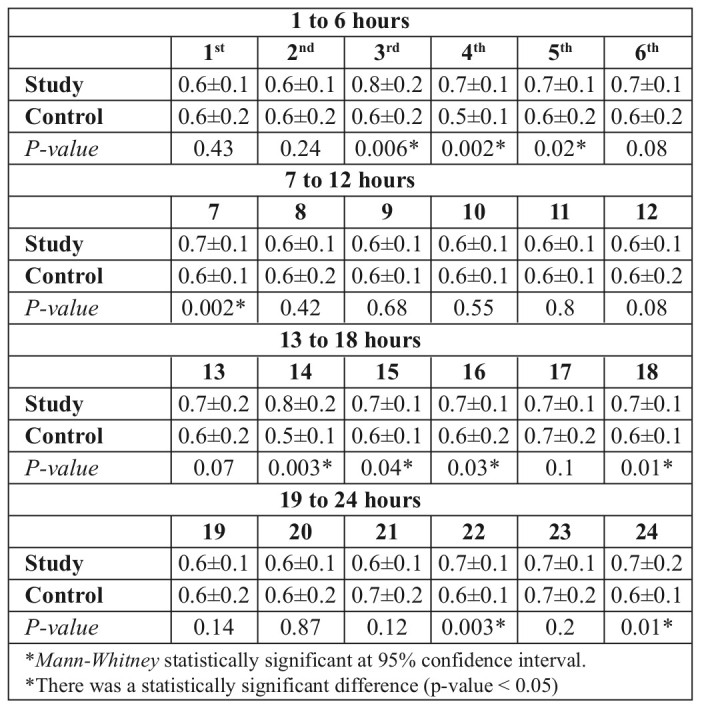
Urine output (Tables IX, X and XI) was significantly lower in the study group on the first day in 2 readings only (3rd and 9th hour), with values above the critical value. On the second day, the study group showed 3 significantly higher and 2 significantly lower values than the control group (Table X); both lower values in both groups were above the critical value. On the third day, the study group showed significantly higher values on 10 occasions, with control group values above the critical value.
Table IX. Mean urine output in both groups on the first day.
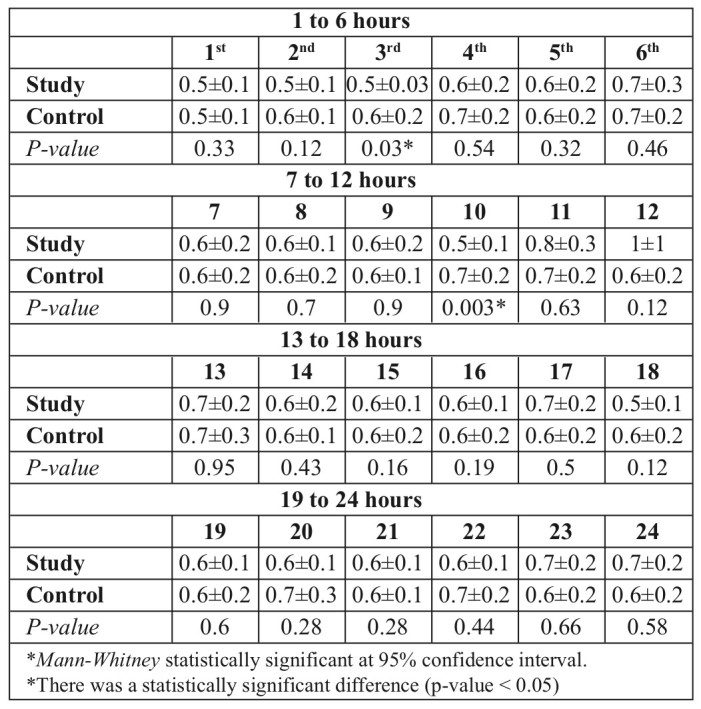
Table X. Mean urine output in both groups on the second day.
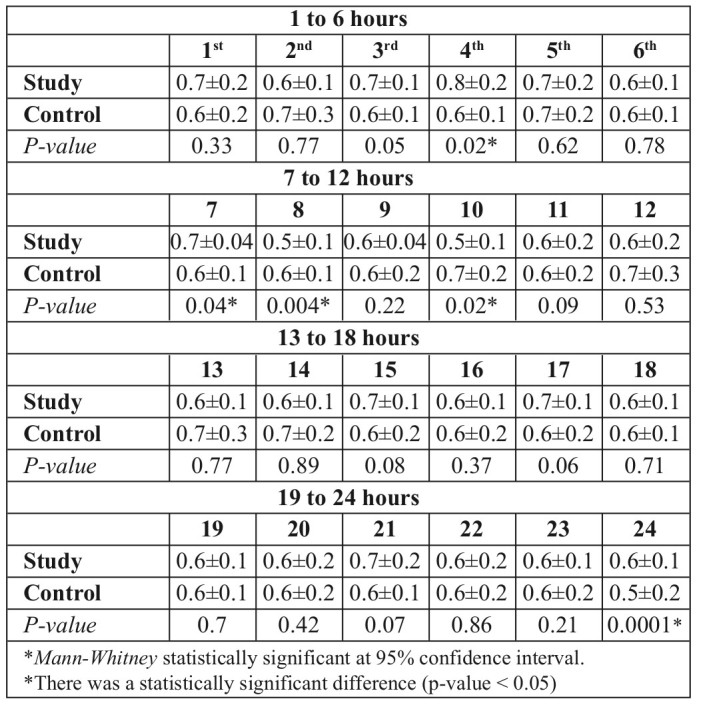
Table XI. Mean urine output in both groups on the third day.
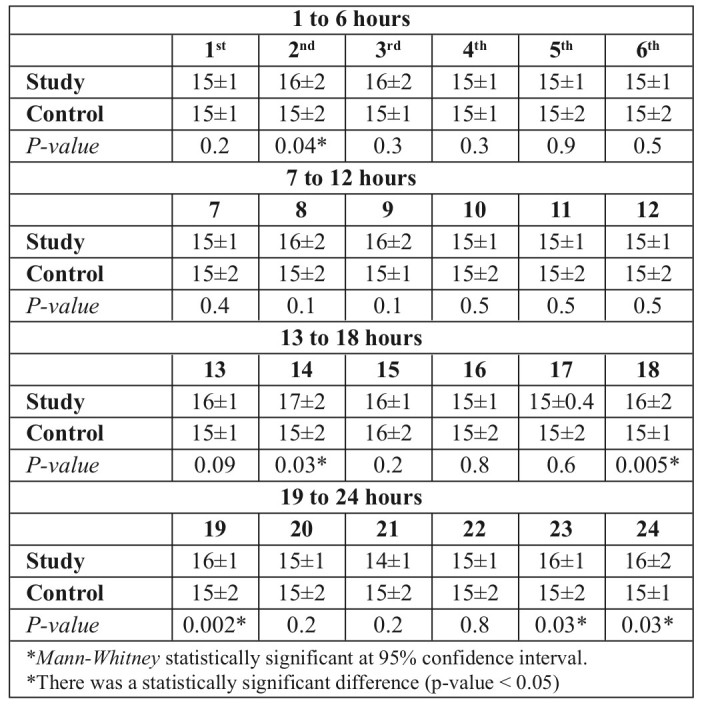
Respiratory rate (Tables XII, XIII and XIV) followed the same rule: although it was significantly higher on some sporadic occasions in the study group, it did not exceed the limit of 20/min (the maximum was 18/min, and this occurred in the first 12 hours only). All patients were alert in both groups (all A).
Table XII. Mean respiratory rate in both groups on the first day.
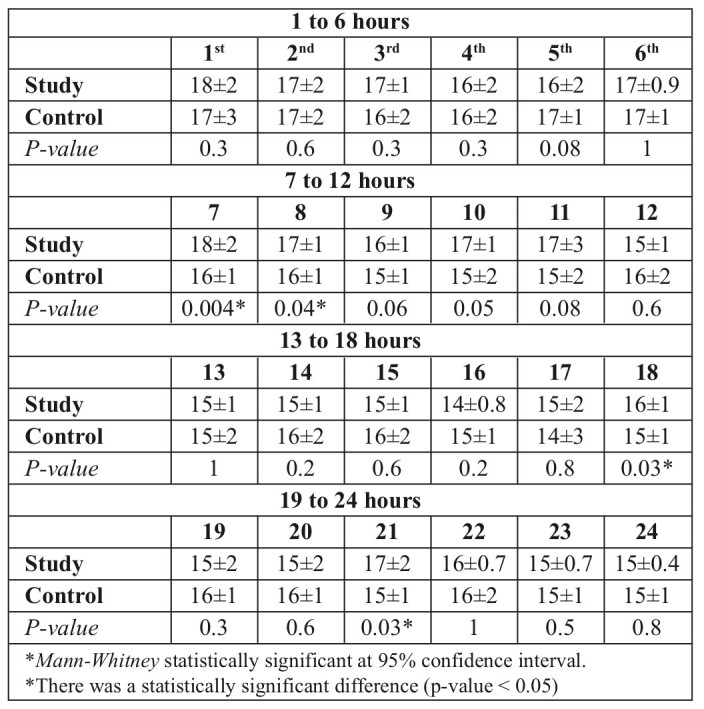
Table XIII. Mean respiratory rate in both groups on the second day.
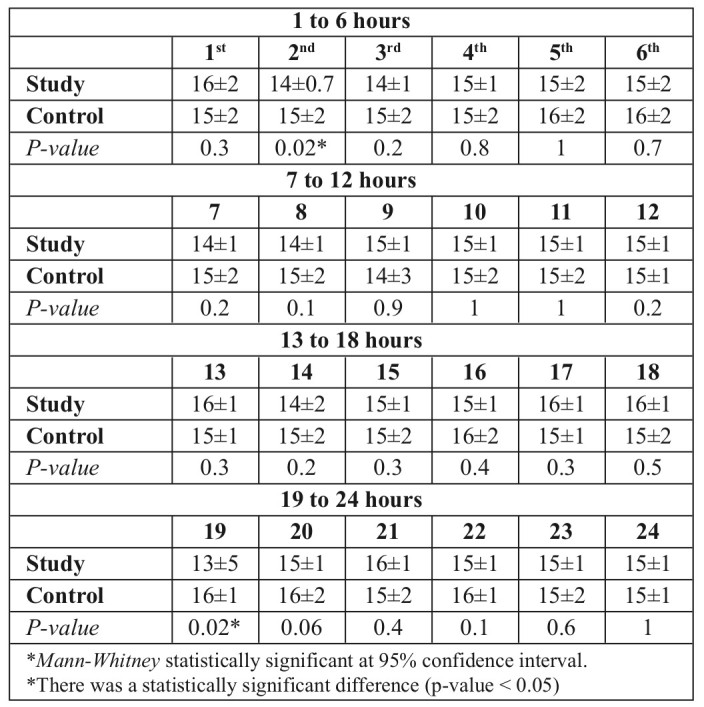
Table XIV. Mean respiratory rate in both groups on the third day.
Discussion
Burn and trauma patients in underdeveloped countries often have delayed, limited, or even no access to IV fluid therapy. Even in HICs, access to delivery of IV fluids might be limited in large fire disasters.9
The aim of the present work was to create a new philosophy through reviving and merging two old abandoned philosophies to produce a synergy. Sørensen’s formula7 was effective in most but not all cases. Monafo10 found that adding high salt supplements to IV resuscitation formula significantly and dramatically reduced the amount of fluid needed and increased its effectiveness. Therefore we believed that replacing water by WHO-ORS and adding supplementary salt to Sørensen’s formula would largely increase its effectiveness.
WHO-ORS (containing a considerable amount of salt) was chosen instead of water, as mentioned by Sørensen, as it has proved to be effective, even alone, in treating moderate dehydration and burns.8
Our study was conceived to compare two groups: patients receiving intravenous resuscitation using the Parkland formula (control group) and those given oral resuscitations using Oral Rehydration Solution and 5gm salt tablets according to Sørensen’s formula (study group). There was no significant difference in all the demographic data or burn percentage, depth as well as etiology, between the two groups.
There was great concern about the safety of this study. According to Kramer et al.6, the few studies encouraging enteral resuscitation on humans are old and/or with several limitations. Nevertheless, these studies have established variable effectiveness and value of enteral resuscitation.
All available studies, except El Sonbaty,8 used solutions that are not available in LMICs or in most non-specialized centers in HICs. Based on the results of the use of ORS and Sørensen’s formula separately, we believed that combining the two would not turn out to be inferior to IV resuscitation. As far as we know, this combination has not been used before.
Our results showed that the mean values of all parameters in both groups were comparable. Even where there was a significant difference, in some sporadic instances, the values never reached critical values throughout the whole study period The only exception was mean systolic blood pressure in the study group after the first hour of resuscitation, which was 98 mmHg. These results show concordance with the results of the studies that exclusively used oral, or even mixed, resuscitation.
In 1941, Charles Fox successfully resuscitated 4 children (TBSA 23%–80%) and 5 adults (19%–41%) with full thickness burns using chilled isotonic sodium lactate at a rate of 100-150 mL/kg/24 hours to obtain 1–2 liters of urine per day. Nasogastric tubes were used only when vomiting occurred.11
In 1949, Carl Moyer started oral resuscitation after initial IV resuscitation with lactated Ringer’s or plasma until the peripheral collapse was corrected. He noted that citrated formula led to a lot less acidosis, nausea and vomiting than oral lactated Ringer’s solution.12
The first clinical trial comparing oral with IV resuscitation was carried out in 1956 by Markley et al.13 This extensive NIH sponsored trial (55 children and 56 adults), conducted in Peru, compared oral isotonic bicarbonated saline and IV therapy using plasma and saline (Evans formula) in the first 48 hours for severe burns (from 30% to 40% TBSA). The volume of oral saline was 110 ml/kg, regardless of TBSA, in the first 24 hours. Although Markley reported similar mortality rates in both groups, this amount seemed unable to fully resuscitate burns >50% TBSA.
Davies made the same ‘mistake’ in 1964. He resuscitated burn patients, 10-95% TBSA, with oral water and oral Moyer solution administered at double the normal oral fluid input, regardless of injury size. Clearly, this was inadequate for several patients, making the study of very limited value.14
In 1960, Wilson and Stirman used blood to resuscitate the IV group. Therefore, results of the oral group were much better as far as mortality and morbidity were concerned. The only relevant part we can rely upon in this study is that 81 of Wilson’s patients were treated exclusively with oral intake of isotonic saline, including some patients with 60% TBSA injury who survived with no hemodynamic problems; although he mentioned using IV initially in patients with peripheral circulatory collapse.15
In 1962, Sørensen similarly didn’t titrate the fluid intake to burn size; his modification was only limited to using higher volumes: 150 to 200 ml/kg and 100 to 150 ml/kg in the first and second 24 hours. He didn’t use any ‘particular’ fluid; he only insisted on introducing 5gm salt tablets per each liter of fluid drunk. He succeeded in resuscitating 26 consecutive patients with burns up to 45% TBSA where 80% of them required no IV support.7
In 1966, Jackson and Chen treated 162 burn cases (113 children and 49 adults) with 10% to 35% TBSA injuries with enterally administered Meyer’s solution; 75% were exclusively and successfully treated with oral resuscitation. Nevertheless, mean urine output was reported to be less than normal within the first 48 hours post-burn. Vomiting, although frequent, was not necessarily a criterion to start IV therapy.16
Monafo created a mixed resuscitation formula in 1970. He reported successful resuscitation of 4 burn adults (up to 95% TBSA) and 3 children (up to 58% TBSA). Patients received 10-60% and 60-90% of their fluid needs in the first and second 24 hours respectively through oral route. Hypertonic lactated saline was the IV solution used.10
In 1975, Ahnefeld reported on the use of Liquidsorb for treating 68 burn patients with 12 to 34% TBSA. Liquidsorb contained 4 g of glucose, 100 mg ascorbic acid, and 12 mg nicotinamide per liter of bicarbonated saline. He demonstrated the superiority of nasogastric infusion of this fluid, except for patients with severe shock, evidenced by delayed capillary refill.17
Maksimov reported that the use of oral alkaline solution was sufficient for mild burn shocks only.18
The study conducted by El-Sonbaty, despite focusing exclusively on children, reveals the value of WHO-ORS in treating moderate burns. He reported that oral and intravenous resuscitations were similar; urine output was 0.8 to 2.5 ml/h and 1 to 2.5 ml/h in the1st and 2nd groups in the first 24 h.8
Limitations of the study
The limited number of patients in both groups was due to the renovation work being carried out to expand our burn unit. The smaller number in the study group was due to patients’ refusal to be allocated to the study group (10 patients) as they were skeptical, and we did not have any good evidence to support this practice.
Lack of laboratory investigations, as well as invasive investigations, which would have allowed better comparison of biological parameters in both groups.
Recommendations
A multi-center study, which includes ultra-major burns, should be performed to allow better evaluation of the efficacy and limitation of this combination, with eventual modification of its use, composition and amount.
Level of confidence in the trial should be increased by conducting a non-inferiority study, and a higher power level of statistical analysis.
The electrolyte profile of burned patients treated with both modalities should be measured, hourly if possible, to give more sophisticated and detailed results on safety and efficacy.
Oral intake, through the formula and the supplement, should be correlated to possible factors allowing better calculation of requirements, such as sex, age, TBSA burned, degree of burn and type of beverage.
There should be long term follow-up for complications, as well as other physiological parameters such as weight gain and stool volume output in both groups.
References
- 1.Forjouh SN. Burns in low- and middle-income countries: a review of available literature on descriptive epidemiology, risk factors, treatment, and prevention. Burns. 2006;32(5):529–537. doi: 10.1016/j.burns.2006.04.002. [DOI] [PubMed] [Google Scholar]
- 2.Peck MD, Kruger GF, van der Merwe AE, Godakumbura W, Ahuja RB. Burns and fires from non-electric domestic appliances in low and middle income countries. Part I. The scope of the problem. Burns. 2008;34(3):303–311. doi: 10.1016/j.burns.2007.08.014. [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization. The Global Burden of Disease: 2004 Update. World Health Organization, Geneva. 2008 Available from: www.who.int/healthinfo/global_burden_disease/GBD_report_2004update_full.pdf .
- 4.Murray CJL, Lopez, AD. The global burden of disease: a comprehensive assessment of mortality and disability from diseases, injuries, and risk factors in 1990 and projected to 2020. World Health Organization, Switzerland. 2006 [Google Scholar]
- 5.Jordan MH, Hollowed KA, Turner DG, Wang DS, Jeng JC. The Pentagon attack of September 11, 2001: a burn center’s experience. J Burn Care Rehabil. 2005;26:109–116. doi: 10.1097/01.bcr.0000155539.82870.64. [DOI] [PubMed] [Google Scholar]
- 6.Kramer GC, Michell MW, Oliveira H, Brown TL et al. Oral and enteral resuscitation of burn shock: the historical record and implications for mass casualty care. Eplasty. 2010;10:458–474. [PMC free article] [PubMed] [Google Scholar]
- 7.Sørensen B. Management of burns occurring as mass casualties after nuclear explosion. Burns. 1960;6:33–36. [Google Scholar]
- 8.El Sonbaty MA. Oral rehydration therapy in moderately burned children. Ann Burn Fire Disaster. 1960;4:29–32. [Google Scholar]
- 9.Cancio LC, Pruitt B. Management of mass casualty burn disasters. Int J Disaster Med. 2004;2:114–129. [Google Scholar]
- 10.Monafo WW. The treatment of burn shock by the intravenous and oral administration of hypertonic lactated saline solution. J Trauma. 1970;10(7):575–586. doi: 10.1097/00005373-197007000-00006. [DOI] [PubMed] [Google Scholar]
- 11.Fox CLJ. Oral sodium lactates in treatment of burns and shock. JAMA. 1944;124:207–212. [Google Scholar]
- 12.Moyer CA. Recent advances in the chemical supportive therapy of thermal injuries. Tex State J Med. 1949;45:635–639. [PubMed] [Google Scholar]
- 13.Markley K, Bocanegra M, Bazan A, Temple R et al. evaluation of saline solution therapy in burn shock. JAMA. 1956;161(15):1465–1473. doi: 10.1001/jama.1956.02970150033008. [DOI] [PubMed] [Google Scholar]
- 14.Davies JWL. Blood volume changes in patients with burns treated with either colloid or saline solutions. Clin Sci. 1964;26:429–443. [PubMed] [Google Scholar]
- 15.Wilson BJ, Stirman JA. Initial treatment of burns. JAMA. 1960;173(5):509–516. doi: 10.1001/jama.1960.73020230008008. [DOI] [PubMed] [Google Scholar]
- 16.Jackson D, Cason JS. The treatment of burns shock with oral hypotonic saline-bicarbonate solution. Wallace AB, Wilkinson AW (eds) London: E. Livingstone Ltd; 1966. pp. 61–70. [Google Scholar]
- 17.Ahnefeld FW, Borst RH, Bardua R. Oral ingestion of an electrolyte solution as shock prophylaxis in burn patients. Vrabec ZK, Moserova J (eds): ‘Basic Problems in Burns: Proceedings of the Symposium for Treatment of Burns’. Prague: Heidelberg New York, Springer-Verlag Berlin; 1975. pp. 74–79. [Google Scholar]
- 18.Maksimov PI. Comparative effectiveness of various methods of fluid therapy in the treatment of moderate and severe burn shock. Khirurgiia (Mosk) 1989;3 (English abstract):87–90. [PubMed] [Google Scholar]


