Abstract
Objectives: To identify differences in the diagnosis and treatment of attention deficit/hyperactivity disorder (ADHD) between typically developing children and children with spina bifida. Method: Sixty-eight children with spina bifida and 68 demographically matched, typically developing children participated in a larger, longitudinal study. Rates of maternal, paternal, and teacher reports of attention problems, as well as rates of maternal reports of ADHD diagnosis, diagnosing provider, pharmaceutical treatment, mental health treatment, and academic accommodations were obtained at 5 time points over a period of 8 years and were compared across groups. Results: Children with spina bifida were more likely to have an ADHD diagnosis and attention problems. Attention problems and ADHD diagnoses were first reported at earlier time points for children with spina bifida than typically developing children. Among children with ADHD or attention problems, children with spina bifida were more likely to be treated with medication, but they were just as likely to use mental health services and receive resource services at school. Conclusions: Children with spina bifida were diagnosed with ADHD and identified as having attention problems more frequently and at an earlier age. This finding could be due to earlier symptom development, greater parental awareness, or more contact with providers. Among those with ADHD or attention problems, stimulant medication was more likely to be prescribed to children with spina bifida, despite research that suggests it may not be as beneficial for them. Further research on the effectiveness of ADHD pharmacological treatment for children with spina bifida is recommended.
Keywords: ADHD, attention, longitudinal study, myelomeningocele, spina bifida
Children with spina bifida are often described as having deficits in attention and executive functioning, and thus they have a higher incidence of attention deficit/hyperactivity disorder (ADHD) than typically developing peers.1–5 These deficits appear to have implications for everyday functioning, as attention and executive functioning weaknesses have been found to contribute to difficulties with academic achievement,6 autonomy development,7 and social adjustment.8 It is likely that early identification and intervention for attention and executive functioning concerns would be beneficial for children with spina bifida.
The diagnosis of ADHD may manifest itself differently in children with spina bifida. The profile of attention deficits in children with spina bifida is different from what is typically seen in children with ADHD. Often, children with spina bifida perform less well on measures of selective and divided attention than they do on measures of sustained attention.9–11 For children with spina bifida, this pattern of attention deficits has been associated with posterior brain malformations, such as tectal beaking and smaller posterior brain volume,12 rather than anterior systems (frontal lobes) that are generally associated with ADHD and issues with sustained attention.4 These subtle differences in attentional control may be difficult to detect. Thus, children with spina bifida may be diagnosed with ADHD at a later age. On the other hand, children with spina bifida are in contact with medical care providers more frequently, and thus there may be greater opportunity to identify attention weaknesses. Because it is known that children with spina bifida often show difficulties with attention, care providers may be more sensitive to attention concerns.
The manner in which ADHD is treated may also be different for children with spina bifida. Stimulant medication is often the first line of treatment; yet researchers hypothesize that stimulant medication may not work as well for children with spina bifida,10,13 because of the different brain structures that are likely involved in their attention difficulties.12 Moreover, given that children with spina bifida may receive accommodations at school for mobility concerns or learning disorders, it may be easier to incorporate additional supports for inattention for these children than is the case with children who have ADHD, thus raising the possibility that medication may not need to be the first line of treatment for this population. Alternatively, because ADHD-inattentive type is more common for children with spina bifida than ADHD-hyperactive-impulsive type or ADHD-combined type, its impact on learning in the classroom may not be as overt as the behavioral difficulties associated with hyperactivity.14 Therefore, it is possible that children with spina bifida might receive fewer school accommodations for ADHD.
In the current study, we aimed to examine differences in the identification of attention problems and diagnosis and treatment of ADHD for children with and without spina bifida. Compared to their typically developing peers, we hypothesized that children with spina bifida would have a higher rate of attention problems and ADHD diagnosis. Of those with attention problems or an ADHD diagnosis, we hypothesized that children with spina bifida would be identified as having attention problems/ADHD diagnosis at an earlier time point. Of those with a reported ADHD diagnosis, we believed that children with spina bifida would be more likely to be diagnosed by a medical professional, be less likely to be on stimulant medication, be less likely to receive mental health/behavioral services, and be more likely to receive academic resources at school.
Methods
Participants were a part of a larger, longitudinal study examining psychosocial functioning among youth with spina bifida and typically developing youth (see ref. 15) that was approved by and conducted in accordance with the ethical standards of applicable institutional review boards. Families of children with spina bifida were recruited from 4 hospitals and a statewide spina bifida association in the Midwest. Families received letters inviting them to participate in the study if they had a child with spina bifida between the ages of 8 and 9 years old, lived within 120 miles from the laboratory, and spoke English. This study included a matched comparison sample of typically developing children and their caregivers who were recruited from a select group of schools where participating children with spina bifida were enrolled. Schools were chosen based on location, the average family income of the surrounding community, and the ethnic distribution in the school. About 1,700 letters were sent home with children enrolled at the 12 schools that agreed to participate. The letters requested parental permission for these children to participate in the study. Seventy families with typically developing children and 72 families with children with spina bifida agreed to participate. Families were dropped from each group until the 2 groups were matched on 10 demographic variables including child age, maternal age, paternal age, child birth order, maternal income, paternal income, socioeconomic status, gender, ethnicity, and parent marital status. Groups did not differ significantly on any of these matching variables at Time 1 (p > .05; see ref. 16 for details on the matching process).
The present study examined 5 waves of data that were collected every 2 years (ages 8–9 at Time 1). At Time 1, participants included 68 families of children with spina bifida and 68 typically developing children and their families. Enrollment for subsequent time points was as follows: Time 2, 67 spina bifida and 66 typically developing; Time 3, 64 spina bifida and 66 typically developing; Time 4, 60 spina bifida and 65 typically developing; and Time 5, 52 spina bifida and 61 typically developing (see ref. 15 for more information on attrition rates). At Time 1, 54% of participants were male (n = 37 spina bifida; n = 37 typically developing) and average age was 8.34 years for participants with spina bifida and 8.49 for typically developing peers. Of the participants with spina bifida, 82.4% identified as Caucasian, 5.9% identified as African American, and 11.7% identified as “other” race. Of the typically developing participants, 91.2% identified as Caucasian, 1.5% identified as African American, and 7.3% identified as “other” race.
Information regarding medical status was gathered from maternal report on a questionnaire andareviewofmedicalcharts.Of the 68 participants with spina bifida, 82.4% had myelomeningocele, 11.8% had lipomeningocele, and 5.8% had another spina bifida diagnosis. Additionally, more than half of the participants had spinal lesions located in the lumbar spinal region (54%), 32% had lesions in the sacral region, and 13% had lesions in the thoracic region. Most (71%) of the children with spina bifida had a shunt.
Mothers completed the Parent Demographic Questionnaire (PDQ), which was developed for this study to gather information regarding the child's age and ethnicity. The questionnaire was designed to assess a variety of demographic variables pertaining to the child, caregiver(s), and family.
Mothers also completed a health questionnaire, which gathered information regarding the diagnosis and treatment of ADHD. The following items were asked at all 5 time points: Does your child have an ADHD diagnosis? (yes or no); Who made the diagnosis? (medical provider, mental health professional, or school personnel); Is your child currently taking any medications? (yes or no; if yes, list medications); Have you used mental health services for your child? (yes or no); Does your child receive special accommodations at school? (yes or no). The following medications were considered to relate to medication management of ADHD: Adderall, Dexedrine, methylphenidate, Ritalin, Concerta, Vyvanse, Focalin, or “ADD medication.”
Behavioral rating forms are often used to evaluate attention problems in several environments, for example, at home and at school.17 To obtain such information for the current study, mothers and fathers completed the Child Behavior Checklist (CBCL)18 at every time point and teachers completed the equivalent teacher version – the Teacher Report Form (TRF).18 For each form (CBCL and TRF), reporters rate the child's behavior on a 3-point scale (0 = not true, 1 = somewhat or sometimes true, 2 = very true or often true) for 118 problem behaviors. The CBCL and TRF yield age-based T scores and percentiles for 8 problem subscales. T scores above 70 are considered to fall within the clinical range and indicate significant deviation from the normative sample in the respective problem area. T scores between 65 and 70 are considered to fall within the borderline clinical range. Only the Attention Problems subscale was used in the current study. A cut-off score of 65 was used in the current study, such that children with a T score of 65 or greater were considered to have clinically significant parent- or teacher-reported attention problems.
Chi-square and t tests were used to determine group differences in ADHD diagnosis/reported attention problems, timing of diagnosis/attention problems, diagnosing provider, and treatment. Analyses were run separately for ADHD diagnosis and parent/teacher-reported attention problems. A child was rated as having attention problems if any score on the mother, father, or teacher CBCL/TRF Attention Problems subscale was elevated (T score ≥ 65). Due to the small sample size, Fisher's exact test was used to determine statistical significance.
Results
For ADHD diagnosis, chi-square analyses revealed that the rate of ADHD diagnosis was higher for children with spina bifida than typically developing children (χ2 = 11.12, p < .01; see Table 1). Twenty-six (38%) children with spina bifida and 9 (13%) typically developing children had a diagnosis of ADHD at some point from age 8 to 17 years. Mothers of children with spina bifida first reported a diagnosis of ADHD at an earlier time point than mothers of typically developing children, t(33) = −3.99, p < .01 (spina bifida mean time point = 1.62 [SD = .80]; typically developing mean time point = 3.11 [SD = 1.36]). Among children with ADHD, children with spina bifida were more likely to be treated with medication (χ2 = 18.17, p < .01), but were just as likely to be diagnosed by a medical professional (χ2 = .64, p = .73), use mental health services (χ2 = .783, p = .45), and receive resource services at school as typically developing children (χ2 = 2.23, p = .19). Of note, not a single typically developing child with ADHD was being treated with medication, whereas 80% of the children with spina bifida and ADHD were being treated with ADHD medication.
Table 1.
Comparisons between children with and without spina bifida
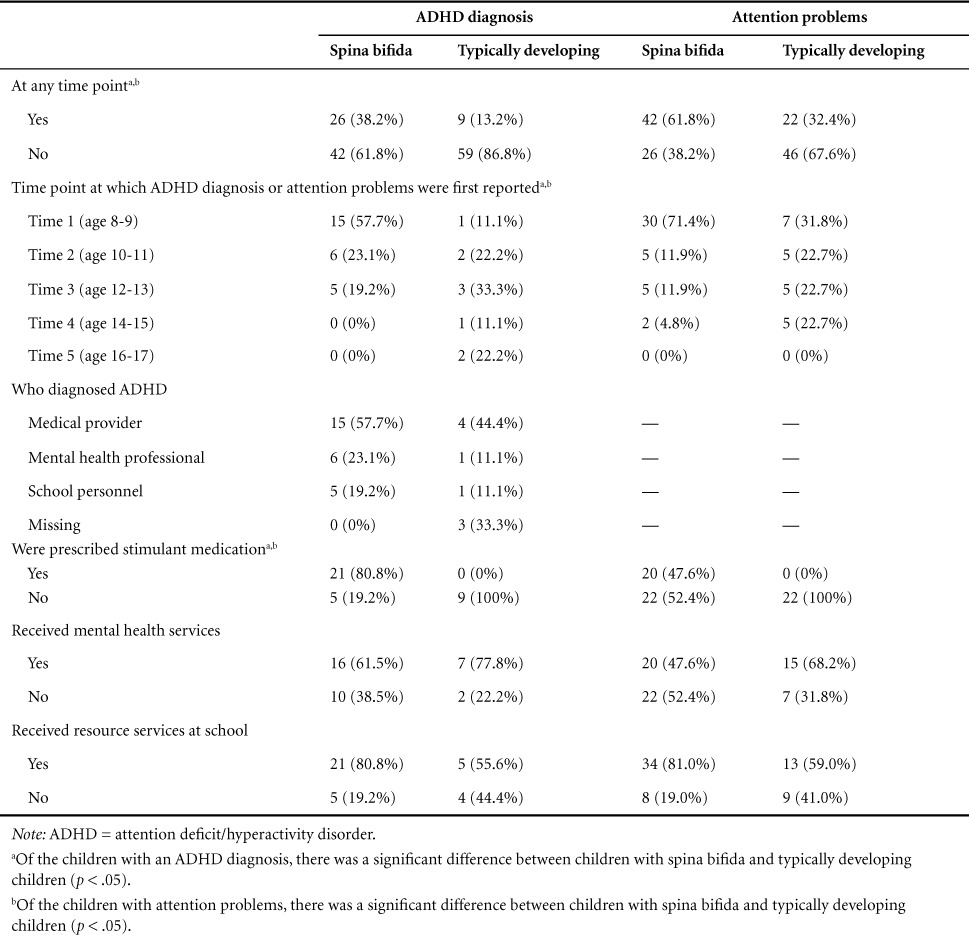
In regard to attention problems, chi-square analyses indicated that the rate of attention problems was higher for children with spina bifida than typically developing children (χ2 = 11.12, p < .01; see Table 1). Twenty-six (38%) children with spina bifida and 9 (13%) typically developing children had a diagnosis of ADHD at some point from age 8 to 17 years. Mothers of children with spina bifida first reported a diagnosis of ADHD at an earlier time point than mothers of typically developing children, t(33) = −3.99, p < .01 (spina bifida mean time point = 1.62 [SD = .80]; typically developing mean time point = 3.11 [SD = 1.36]). Among children with ADHD, children with spina bifida were more likely to be treated with medication (χ2 = 18.17, p < .01), but were just as likely to be diagnosed by a medical professional (χ2 = .64, p = .73), use mental health services (χ2 = .783, p = .45), and receive resource services at school as typically developing children (χ2 = 2.23, p = .19). Of note, not a single typically developing child with ADHD was being treated with medication, whereas 80% of the children with spina bifida and ADHD were being treated with ADHD medication.
In regard to attention problems, chi-square analyses indicated that the rate of attention problems was higher for children with spina bifida than typically developing children (χ2 = 11.81, p < .01; see Table 1). When collapsed across all time points, 42 (62%) children with spina bifida and 22 (32%) typically developing children had attention problems at some point across the 5 time points. Attention problems were reported at an earlier time point for children with spina bifida than typically developing children, t(62) = −3.29, p < .01 (spina bifida mean time point = 1.50 [SD = .89]; typically developing mean time point = 2.36 [SD = 1.18]). Of the children with attention problems, children with spina bifida were more likely to be treated with medication (χ2 = 15.24, p < .01), but they were just as likely to use mental health services (χ2 = 2.46, p = .19) and receive resources services at school (χ2 = 3.54, p = .08) as typically developing children.
We also examined the concordance between reported ADHD diagnosis and attention problems at any time point. Twenty-nine participants (20 with spina bifida and 9 typically developing) had both an ADHD diagnosis and reported attention problems at some time point. Six participants (6 with spina bifida and 0 typically developing) had an ADHD diagnosis without attention problems. Finally, 35 participants (22 spina bifida and 13 typically developing) had attention problems without a reported ADHD diagnosis.
Discussion
The purpose of the current study was to examine differences in the reporting of attention problems and the diagnosis and treatment of ADHD in children with and without spina bifida. Several findings were as expected and hypothesized. The rate of reported ADHD diagnosis was higher for children with spina bifida than their typically developing peers and was similar to previous reports in the literature (ie, 31% to 34%).1,4,5 Moreover, attention problems were reported at a higher rate for children with spina bifida than typically developing peers. Additionally, attention concerns were identified earlier and ADHD diagnoses were made at an earlier age for children with spina bifida. This finding is encouraging in that earlier diagnosis may lead to earlier intervention. It also suggests that attentional concerns in children with spina bifida are present and noticed by caregivers at an earlier age.
However, contrary to our hypotheses, findings indicated that children with spina bifida were more likely to be on stimulant medication for ADHD treatment. One possible explanation is that parents of children with spina bifida are more accepting of stimulants, because youth with spina bifida are likely to already be taking other medications, whereas parents of typically developing children may be hesitant to start a stimulant if their children have not been taking other medications. Alternatively, it is possible that parents of children with spina bifida may be more concerned about the possible impact of their child's attention difficulties on academic achievement, as children with spina bifida are also at increased risk for learning difficulties.19 Still, as previously mentioned, stimulant medication may not be as beneficial for treating ADHD and attention problems in children with spina bifida.10,13 Thus, given the finding that stimulant medication is used more often in this population, further research is necessary to determine its effectiveness for children with spina bifida.
Finally, there were no differences in the current study between children with and without spina bifida in terms of who made the ADHD diagnosis or whether the child received mental health/behavioral services or accommodations at school. Children both with and without spina bifida were more likely to be diagnosed by a medical provider than a mental health professional or school personnel. Although it is encouraging that medical providers are able to identify and diagnose attention problems in these children, it is possible that the nuanced profile of attention problems in children with spina bifida may be better identified with a neuropsychological assessment than through observation and/or behavioral ratings/parent interviews. These findings also indicate that children with an ADHD diagnosis receive the same amount of behavioral supports and school accommodations whether or not they have spina bifida. This finding is encouraging, suggesting that children with special needs (either ADHD or spina bifida) are receiving supportive services, but it is still important for future research to determine the quality and effectiveness of such services.
This study has several strengths, including a longitudinal design and a matched comparison sample, but it is not without limitations. First, the study relied solely on mother report for information about ADHD diagnosis and treatment. Although reported attention problems resulted in similar findings, the overlap between children who had an ADHD diagnosis and those with attention problems was not perfect. It is understandable that many participants had attention problems without an ADHD diagnosis, as an ADHD diagnosis requires documented attention problems in at least 2 environments (eg, home and school), whereas a child was determined to have “attention problems” based on a single report (mother, father, or teacher). However, it is less likely that participants would have an ADHD diagnosis without attention problems. Despite this, it is possible that these participants were being treated for ADHD and thus did not display concurrent attention problems. To resolve some of these inconsistencies, future research may want to include objective evaluations or provider report to verify an ADHD diagnosis. Second, we did not assess duration of treatment or the level of satisfaction or reduction of symptoms with the treatment regimen. It is recommended that future studies evaluate which medications are used and when (as well as level of adherence to medication). Similarly, to evaluate the potential impact of behavioral strategies, it is recommended that more information be obtained to determine the kinds of accommodations that are being provided in the home or school settings and the effectiveness of these strategies.
Conclusions
Findings from the current study indicated that children with spina bifida are at an increased risk for attention problems and ADHD, are more likely to have these attention problems identified and ADHD diagnosed at an earlier age, and are more likely to be treated with medication to address attention problems. Thus, more research and greater clinical focus on attention problems in children with spina bifida are warranted. Given that symptoms of inattention are often different in children with spina bifida than other children with ADHD (eg, greater difficulty shifting than focusing), it will be especially important for researchers and clinicians to use appropriate assessments and evaluate the effectiveness of interventions (eg, medication) in this population. Future research is needed to examine the ways in which attention problems are effectively identified and supported to promote healthy academic and social development for children with spina bifida.
Acknowledgments
The authors declare no conflicts of interest. This work was supported by the National Institute of Child Health and Human Development (R01-HD048629) and the March of Dimes Birth Defects Foundation (12-FY13-0271). This study is part of an ongoing, longitudinal study.
REFERENCES
- 1. Ammerman RT, Kane VR, Slomka GT, Reigel DH, Franzen MD, Gadow KD.. Psychiatric symptomatology and family functioning in children and adolescents with spina bifida. J Clin Psychol Med Settings. 1998; 5( 4): 449– 465. [Google Scholar]
- 2. Argento AG, Warschausky SA, Shank L, Hornyak JE.. Spina bifida myelomemingocele. : Goldstein S, Reynolds CR, . Handbook of Neurodevelopmental and Genetic Disorders in Children. 2nd ed. New York: Guilford Press; 2011. [Google Scholar]
- 3. Brown TM, Ris MD, Beebe D, . et al. Factors of biological risk and reserve associated with executive behaviors in children and adolescents with spina bifida myelomeningocele. Child Neuropsychol. 2008; 14( 2): 118– 134. [DOI] [PubMed] [Google Scholar]
- 4. Burmeister R, Hannay HJ, Copeland K, Fletcher JM, Boudousquie A, Dennis M.. Attention problems and executive functions in children with spina bifida and hydrocephalus. Child Neuropsychol. 2005; 11( 3): 265– 283. [DOI] [PubMed] [Google Scholar]
- 5. Fletcher JM, Copeland K, Frederick JA, . et al. Spinal lesion level in spina bifida: A source of neural and cognitive heterogeneity. J Neurosurg Pediatr. 2005; 102( 3): 268– 279. [DOI] [PubMed] [Google Scholar]
- 6. Loss N, OwenYeates K, Enrile BG.. Attention in children with myelomeningocele. Child Neuropsychol. 1998; 4( 1): 7– 20. [Google Scholar]
- 7. Tuminello ER, Holmbeck GN, Olson R.. Executive functions inadolescents with spina bifida: Relations with autonomy development and parental intrusiveness. Child Neuropsychol. 2012. March; 18( 2): 105– 124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Rose BM, Holmbeck GN.. Attention and executive functions in adolescents with spina bifida. J Pediatr Psychol. 2007; 32( 8): 983– 994. [DOI] [PubMed] [Google Scholar]
- 9. Brewer VR, Fletcher JM, Hiscock M, Davidson KC.. Attention processes in children with shunted hydrocephalus versus attention deficit-hyperactivity disorder. Neuropsychology. 2001; 15( 2): 185. [DOI] [PubMed] [Google Scholar]
- 10. Dennis M, Sinopoli KJ, Fletcher JM, Schachar R.. Puppets, robots, critics, and actors within a taxonomy of attention for developmental disorders. J Int Neuropsychol Soc. 2008; 14( 05): 673– 690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Erickson K, Baron IS, Fantie BD.. Neuropsychological functioning in early hydrocephalus: Review from a developmental perspective. Child Neuropsychol. 2001; 7( 4): 199– 229. [DOI] [PubMed] [Google Scholar]
- 12. Dennis M, Edelstein K, Copeland K, . et al. Covert orienting to exogenous and endogenous cues in children with spina bifida. Neuropsychologia. 2005; 43( 6): 976– 987. [DOI] [PubMed] [Google Scholar]
- 13. Davidovitch M, Manning-Courtney PA, Linda AH, Watson J, Lutkenhoff M, Oppenheimer S.. The prevalence of attentional problems and the effect of methylphenidate in children with myelomenigocele. Pediatr Rehabil. 1999; 3( 1): 29– 35. [DOI] [PubMed] [Google Scholar]
- 14. Quinn PO. Treating adolescent girls and women with ADHD: Gender-specific issues. J Clin Psychol. 2005; 61( 5): 579– 587. [DOI] [PubMed] [Google Scholar]
- 15. Holmbeck GN, DeLucia C, Essner B, . et al. Trajectories of psychosocial adjustment in adolescents with spina bifida: A 6-year, four-wave longitudinal follow-up. J Consult Clin Psychol. 2010; 78( 4): 511. [DOI] [PubMed] [Google Scholar]
- 16. Holmbeck GN, Westhoven VC, Phillips WS, . et al. A multimethod, multi-informant, and multidimensional perspective on psychosocial adjustment in preadolescents with spina bifida. J Consult Clin Psychol. 2003; 71( 4): 782. [DOI] [PubMed] [Google Scholar]
- 17. Subcommittee on Attention-Deficit/Hyperactivity Disorder, Steering Committee on Quality Improvement and Management. . ADHD: Clinical practice guideline for the diagnosis, evaluation, and treatment of attention-deficit/hyperactivity disorder in children and adolescents. Pediatrics. http://pediatrics.aappublications.org/content/pediatrics/early/2011/10/14/peds.2011-2654.full.pdf. [DOI] [PMC free article] [PubMed]
- 18. Achenbach TM, Rescorla LA.. Manual for the ASEBA School-Age Forms & Profiles: An Integrated System of Multi-Informant Assessment. Burlington, VT: University of Vermont, Research Center for Children, Youth, & Families; 2001. [Google Scholar]
- 19. Wills KE, Holmbeck GN, Dillon K, McLone DG.. Intelligence and achievement in children with myelomeningocele. J Pediatr Psychol. 1990; 15( 2): 161– 176. [DOI] [PubMed] [Google Scholar]


