Abstract
Objective
The purpose of the present report was to describe the longitudinal trajectories of physical health beginning during preschool and continuing into early adolescence, explore whether these trajectories were predicted by psychosocial adversity, family income-to-needs ratio, and psychiatric disorders occurring during the preschool period, and determine whether psychiatric disorders mediated these relations.
Methods
Participants included 296 children participating in a longitudinal study of early-onset psychopathology spanning ten years. Semi-structured clinical interviews were conducted with caregivers to determine children’s psychiatric diagnoses between ages 3–6. Caregivers also completed annual assessments of their child’s physical health problems (ages 3–13), as well as reported on the family’s income and indicators of psychosocial adversity.
Results
Growth mixture modeling revealed two trajectories of physical health problems: a stable, low group (n = 199) and a high, increasing group (n = 57) indicating linear increases in physical health problems from ages 3–13. Preschool psychiatric diagnoses (Est= 0.05, p<.001), family income-to-needs ratio (Est= −0.01, p=.012), and psychosocial adversity (Est=0.02, p=.015) predicted membership in the high, increasing trajectory of physical health problems. Early-onset psychopathology mediated relations between psychosocial adversity and physical health problems (αβ= 0.31, p=.050) and between income-to-needs ratio and physical health problems (αβ= −0.29, p<.021).
Conclusions
These findings indicate the importance of early indicators of risk: low income-to-needs ratios, high psychosocial adversity, and psychiatric disorders occurring during the preschool period for contributing to increasing physical health problems from preschool through early adolescence. Early-onset psychiatric disorders also mediated relations between psychosocial adversity, income-to-needs ratio, and physical health problems.
Keywords: physical health, adversity, childhood, mental health, growth mixture modeling
Introduction
Numerous longitudinal studies have linked adversity experienced during childhood with poor mental and physical health outcomes in adulthood. Adversity includes experiences involving deprivation and/or threat, such as abuse, neglect, and poverty 1,2. Children raised in poverty3,4, those who are physically and emotionally maltreated5,6, and/or separated from primary caregivers for extended periods of time7 are at an increased risk for poor health outcomes ranging from depression and substance abuse, to heightened levels of inflammation and cancer. In order to link different types of adversity to child outcomes, as well as identify developmental mechanisms explaining multifinality of such outcomes1, it is crucial for longitudinal work to measure multiple domains of adverse environmental experiences. Thus, the purpose of the current paper was to examine whether: financial advantage/disadvantage and psychosocial adversity predicted longitudinal trajectories of physical health beginning during preschool and continuing into early adolescence and whether these relations were mediated by early-onset psychiatric disorder.
In the current paper, adversity is defined as, “ exposure during childhood or adolescence to environmental circumstances that are likely to require significant psychological, social, or neurobiological adaptation by an average child”1. We further distinguish between financial advantage/disadvantage, which includes income and SES-type indicators as a proxy for poverty8 and family resources from psychosocial adversity, which includes specific, measureable instances of child experiences of adversity such as abuse, foster care placement, and caregiver arrest. We also recognize that types of adversity are often intertwined and occur in tandem. Our decision to distinguish financial advantage/disadvantage from psychosocial adversity was guided by recent work highlighting the need for additional research that measures multiple domains of adversity in order to uncover common and specific underlying mechanisms linking adversity to psychopathology1.
While concurrent relations between adversity and physical health problems are well documented in childhood, there have been fewer longitudinal studies linking early childhood adversity (occurring prior to age 6) with physical health difficulties in later childhood and adolescence9,10. This work is crucial because early exposure to financial advantage/disadvantage and psychosocial adversity may begin to shape physical health much earlier than the longitudinal evidence from adulthood indicates11. For example, Vella and colleagues12 used growth mixture modeling to identify trajectories of children’s health-related quality of life from ages 4–13. 15% of children were shown to be at risk for poor health-related quality of life over time, and these children were also more likely to be from homes with lower household incomes. In addition, a recent meta-analysis found only nine studies that investigated the impact of early childhood financial adversity on physical health in later childhood and adolescence9. These nine studies varied broadly in terms of the measures of financial adversity that were used (e.g., income-to-needs, neighborhood income, cumulative disadvantage, low family income) as well as the physical health outcomes that were investigated (e.g., BMI, asthma, maternal reports of health status, hospital inpatient admissions). Despite the varying measures and outcomes used findings appear to be consistent: exposure to financial adversity early in life predicts a range of physical health difficulties later in childhood.
Likewise over the past decade, a growing body of evidence has demonstrated longitudinal relations between psychosocial adversity in childhood and physical health across life. The Consortium for LONGitudinal Studies of Child Abuse and Neglect (LONGSCAN) has prospectively assessed and linked psychosocial adversity with health outcomes during early13 and middle childhood14, as well as adolescence10 and adulthood15. For example, psychosocial adversity occurring by age four was shown to be predictive of child physical health at age 6, such that children with more psychosocial adversity also had greater odds of poor health and physical illnesses requiring professional care16. Furthermore, in the same sample, experiencing psychosocial adversity prior to age six was associated with somatic complaints and complaints of poor health at age 1214. Both sets of findings held even after adjusting for family income/poverty, suggesting that psychosocial adversity is important for health outcomes over and above the influence of poverty.
Many mechanisms have been proposed to explain the relations between early adversity and later physical health, including health problems present from birth17, chronic stress and neuroimmune network dysfunction18, lack of access to healthcare and proper nutrition19, and poor parenting practices20, among others21. For example, using data from the National Longitudinal Survey of Children and Youth, Ferro and colleagues22,23 found that: (1) family functioning was found to mediate the association between maternal depressive symptoms (one type of psychosocial adversity) and adolescent depressive symptoms, particularly among adolescents with a chronic physical health condition22 and (2) the association between maternal depressive symptoms and adolescent psychosocial functioning was moderated by the presence of chronic physical health conditions in the adolescents23. Little work, however, has considered early-onset psychiatric disorders as a potential mechanism that may explain (at least in part) the link between adversity and physical health problems. Early-onset psychiatric disorders are important to consider and have not been accounted for in many studies given that many have only recently been validated and recognized. Given the robust associations between early adversity, both financial and psychosocial, and later psychopathology, accounting for early onset psychopathology is a key area for exploration24–26. The high rates of co-occurrence between mental and physical disorders further underscores the importance of this construct27.
In one study, family adversity (e.g., parental education, income, and single-parent-status) during early adolescence had a strong influence on both physical and mental health during the transition to adulthood, approximately 6–8 years later19. Other work in older children and adolescents suggests that chronic physical illnesses present during late childhood predicted increases in symptoms of depression and anxiety over the course of five years28. Two recent meta-analyses show that children and adolescents with physical health problems have higher levels of depressive, internalizing, and externalizing symptoms29,30. However, the authors also note that many of the studies included were cross-sectional and that more longitudinal studies are needed that can analyze the impact of psychological symptoms on the course of physical health problems. Psychiatric disorders may also predict physical health difficulties in children31. For example, a recent meta-analysis found that clinically depressed adolescents have lower resting state heart rate variability than healthy adolescents, an indictor of a poorly functioning anti-inflammatory reflex and physical health problems32. Given that both financial disadvantage and psychosocial adversity have been shown to predict psychiatric disorders, and that psychiatric disorders have been associated with physical health problems, investigations of whether psychiatric disorders may mediate relations between adversity and physical health problems are now needed. These kinds of longitudinal relations between mental and physical health remain to be explored in younger children when both psychiatric disorders and physical health problems can emerge and set the stage for high-risk health trajectories33,34.
The purpose of this study was to investigate the roles of early psychosocial adversity, financial advantage/disadvantage, and early-onset psychopathology on trajectories of physical health from preschool through early adolescence. We applied growth mixture modeling (GMM) to physical health problems endorsed by children and/or their caregivers in a ten-year longitudinal dataset spanning from preschool into early adolescence to create trajectories of physical health over time. GMM offers several advantages when compared to other longitudinal analyses, such as the ability to create unique trajectories of physical health for different groups of children as well as highlight differences in trajectories across time. There have been no studies to our knowledge that have used GMM to establish trajectories of physical health problems in children; therefore we did not hypothesize a specific number of trajectories. Early psychosocial adversity and financial advantage/disadvantage were included in the GMM as predictors of latent class membership. Finally, we explored whether early-onset psychiatric disorders predicted latent class membership and mediated relations between early psychosocial adversity and trajectories of physical health, as well as financial advantage/disadvantage and trajectories of physical health.
Methods
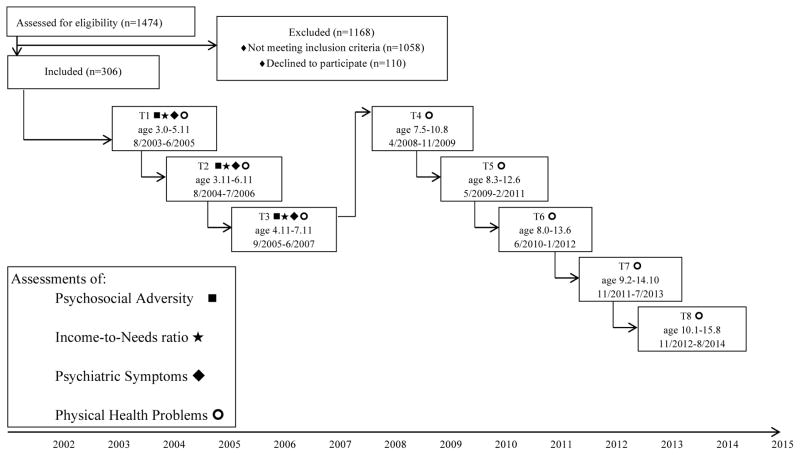
Participants were from the Preschool Depression Study (PDS), a prospective longitudinal investigation of preschoolers and their families conducted at the Washington University School of Medicine (WUSM35). The current study reports on 348 children from the PDS, who across a ten-year period completed at least three behavioral assessments out of a possible eight assessments (Figure 1; due to the grant funding cycle, a larger gap occurred between the third and fourth possible assessment). Parental written consent and child assent were obtained prior to participation and the WUSM Institutional Review Board approved all procedures. Details of recruitment have been previously reported 35,36. In brief, from 2003–2005, 3–6 year olds were recruited from primary care practices and preschools/daycares throughout the Saint Louis metropolitan region using a validated screening checklist (Preschool Feelings Checklist; PFC37) to oversample preschoolers with symptoms of depression and healthy controls. Previous studies have indicated that a PFC score of > 3 maintained high sensitivity and specificity for the diagnosis of depression. Thus, children with scores ≥ 3were invited to participate and those with scores of < 3 were also included to establish an adequate healthy comparison group.
Figure 1.
Preschool Depression Study Assessment Schedule
Materials and Measures
Early Psychosocial Adversity
Seven social risk factors (described below) were assessed during each child’s baseline assessment (e.g. prior to age 6) via caregiver report. Cumulative social adversity/risk scores (occurring prior to age six) were created by summing the dichotomous indicators (0 ‘not present,’ or 1 ‘present’) of each of the seven social risk factors below 38. The cumulative social adversity/risk score ranged from 0–7. This variable was used as a predictor of latent class trajectory membership in later analyses. Psychosocial adversity risk variables included: 1. Living in a single-caregiver household, 2. Maternal psychopathology (Axis I psychiatric disorders excluding eating disorders which were not assessed), 3. Parental arrest, 4. Foster care placement of the child, 5. Physical abuse of the child, 6. Sexual abuse of the child, and 7. Caregiver report of being unable to meet the families financial needs. 32 children did not have complete data on all seven risk factors and were excluded from any analyses that included early adversity. There were no socioeconomic differences between children with and without complete data on this scale. Internal consistency of the psychosocial adversity items was α=0.382, however a confirmatory factor analysis (CFA) supported a single factor and with acceptable model fit (χ2= 24.804, p=0.037; RMSEA=0.051; CFI=0.938). Psychosocial adversity ranged from 0 to 5 in this sample, with a mean (SD) of 0.72 (0.89).
Income-to-Needs ratio
Mothers reported family income at each assessment. The early income-to-needs ratio (e.g., between ages 3–6) was computed as the total family income at baseline divided by the federal poverty level, based on family size, at the time of data collection39. This measure of early financial advantage/disadvantage was used as a predictor of latent class trajectory membership in later analyses. In this sample the mean (SD) was 2.13 (1.19), range 0 – 4.17, indicating relatively low levels of income-to-needs (and high poverty). An income-to-needs ratio of 1 indicates that the family was living at the poverty threshold. 26% of the sample fell below the federal poverty limit.
Physical Health Problems
Mothers completed the MacArthur Health and Behavior Questionnaire40 at each behavioral assessment. The Global Physical Health subscale was used in the current report to create latent class trajectories. This five-item composite score assesses indicators of poor health and difficulties stemming from physical health problems (e.g., missing school) in youth with higher scores indicating worse physical health. Parents are asked to answer questions such as, “in general, would you say your child’s physical health is excellent, good, fair, or poor?” and “how often in an average month does your child stay home or come home from school or childcare because of illness?”. Internal consistency of this scale ranged from adequate to good (α=0.686–0.778) across the waves of data collection.
Preschool-onset Psychiatric Symptoms
Psychiatric diagnoses were assessed at each assessment wave using the Preschool Age Psychiatric Assessment (PAPA41,42) when participants were between the ages of 3–6. Children could have been assessed 1–3 times during this age range, with the mean rating being used in the current paper. The PAPA consists of a series of developmentally appropriate questions assessing the DSM-IV criteria for childhood disorders with information being obtained from parents. For the purpose of the present report, meeting DSM-IV criteria for the following disorders was assessed: depression modified for preschool onset35 (κ = 1.0; ICC = 0.98), externalizing (attention deficit disorder, oppositional defiant, and/or conduct disorder), and internalizing (post traumatic stress disorder, generalized anxiety and separation anxiety). Psychiatric symptoms (combining all disorders listed above) were used as a predictor of latent class membership and as a mediator in later analyses. Consistent with the sampling strategy described above, 50.4% of the sample had an early-onset psychiatric disorder; 29.3% had depression, 35.5% had externalizing disorders, and 28.5% had internalizing disorders.
Statistical Analyses
As recommended by Jung & Wickrama43, prior to beginning the GMM’s, a latent class growth analysis (LCGA) was conducted. The LCGA allows for the identification of distinct classes prior to conducting the GMM. Results from the LCGA of physical health problems indicated 2 distinct classes, which led us to move to a GMM approach to further test our hypotheses and model the unique estimates of variances and covariances. Beginning during the preschool period, participants were classified into subgroups based on physical health problem scores across the longitudinal study using growth mixture modeling 44 in Mplus version 7.3 45. Mplus utilizes full information maximum likelihood (FIML) estimation under the assumption of data missing at random (MAR) with robust standard errors (called the MLR estimator in Mplus). Multiple imputation was not used since the standard FIML estimation used in our analyses corrects for selective attrition46 and recent work suggests that the parameter estimates obtained using FIML approaches are not significantly different than those using multiple imputation47. This GMM model estimated unique variables of intercept and slope for each class (e.g. within-class variance was freely estimated). Specifically, physical health problem scores were calculated at each of the eight annual assessment waves. Quadratic growth mixture models with these scores as the dependent variables were used to determine categorical latent class variables for grouping participants with similar physical health trajectories. In each of these models, the participants’ probability of belonging to each of the latent classes was evaluated, and participants were assigned to the latent class with the greatest probability.
To be included in the quadratic growth mixture models, participants needed to have completed at least three annual assessments (out of a possible eight). Of the N=264 participants included in the growth mixture modeling, 183 (69%) completed at least six, 96 (36%) completed at least 7, and 26 (10%) completed all eight of the possible assessments. When compared to children/families who completed fewer than 6 assessments, children/families who completed 6 or more assessments were equivalent to children/families who completed less than 6 assessments in terms of child sex, ethnicity, maternal education, child psychiatric diagnostic status, maternal history of affective disorder, and family income-to-needs ratio. Several growth mixture models with varying numbers of classes (1–3 classes) for physical health were compared. The model with the best fit according to a combination of the Bayesian Information Criterion (BIC), the Lo-Mendell-Rubin adjusted likelihood ratio test (LRT), and sample size of the resulting classes was selected 43,48–50.
In order to determine whether early-onset psychiatric diagnoses partially explain the relations between income-to-needs and physical health problems, and early psychosocial adversity and physical health problems, mediation analyses were conducted using the PROCESS macro for SAS51,52. When warranted, the Monte Carlo simulator was used to test the statistical significance of the indirect, or mediating effect. The Monte Carlo method is a form of bootstrapping, which simulates random draws from the distributions of each path in the model to estimate a 95% confidence interval around the indirect effect. Bootstrapping is generally preferred over more traditional methods of calculating mediation51.
Results
Fit statistics for the growth mixture models with latent class variables with 1, 2, and 3 classes were compared (Table 1). The 3-class model had the lowest BIC and fit significantly better than the 2-class model according to the Lo-Mendell-Rubin adjusted LRT. However, there were only 8 youth in one of the classes, which would have prevented additional analyses from being conducted with this class. These 8 youth showed initially high levels of physical health problems that declined over time. Therefore, the 8 subjects in this class were excluded from further analyses and the growth mixture models were re-run using the other remaining participants. In these models, the 2-class solution provided the lowest BIC and best fit (Table 1). The probabilities of being included in each latent class were: low 0.98 (0.07) and high 0.95 (0.10).
Table 1.
Fit statistics of growth mixture models with one to three latent classes
| N Latent Classes | N=256
|
|||||
|---|---|---|---|---|---|---|
| AIC | BIC | Log-Likelihood | Entropy | L-M-R ALRT p | Class N’s | |
| 1 | 1311.8 | 1361.5 | −641.9 | -- | -- | 256 |
| 2 | 853.9 | 914.2 | −410.0 | 0.905 | 0.0039 | 57, 199 |
| 3 | 764.0 | 842.0 | −360.0 | 0.830 | 0.1861 | 31, 60, 165 |
AIC = Akaike Information Criterion; BIC = Bayesian Information Criterion; L-M-R ALRT p = Lo-Mendell-Rubin Adjusted Likelihood Ratio Test p-value
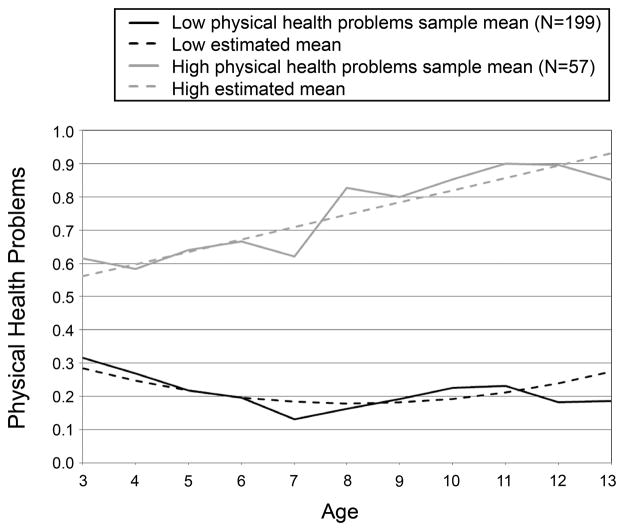
Details of the growth mixture models are shown in Table 2 and the trajectories of latent classes are graphed in Figure 2. The growth mixture model revealed that the latent class with more physical health problems had an intercept significantly different from zero, indicating differences in physical health problems at the first assessment, as well as significant linear slope components, indicating significant changes (increases) in the course of physical health problems across time. The quadratic slope for the class with more physical health problems was not significant. The latent class with few physical health problems evidenced significant linear and quadratic slopes, indicating an initial significant decline in the course of physical health problems, followed by a later increase in physical health problems across time.
Table 2.
Estimates from growth mixture model of physical health problems
| Model: | Estimate | SE | Z | Two-tailed p |
|---|---|---|---|---|
| Low physical health problems | ||||
| Intercept | 0.284 | 0.027 | 10.404 | <0.001 |
| Linear Slope | −0.041 | 0.014 | −2.942 | 0.003 |
| Quadratic | 0.004 | 0.002 | 2.256 | 0.024 |
| High physical health problems | ||||
| Intercept | 0.561 | 0.081 | 6.953 | <0.001 |
| Linear Slope | 0.037 | 0.017 | 2.113 | 0.035 |
| Quadratic | * | * | * | * |
quadratic term non-significant, so removed from model
Figure 2.
Latent class trajectories of global physical health problems from preschool through early adolescence
Correlations between baseline predictors and global physical health scores across time are presented in Table S1 (Supplemental Digital Content 1). Additional descriptive statistics for participants are presented in Table 3 as well as χ2 and t-tests that examined group differences between the low and high latent classes.
Table 3.
Demographic characteristics of participants
| Low GPH (N=199)
|
High GPH (N=57)
|
Low vs. High
|
||||
|---|---|---|---|---|---|---|
| % | N | % | N | χ2 | p | |
| Sex | ||||||
| Male | 51.8 | 103 | 54.4 | 31 | 0.12 | 0.7268 |
| Female | 48.2 | 96 | 45.6 | 26 | ||
| Race | ||||||
| White | 60.3 | 120 | 47.4 | 27 | 3.00 | 0.0833 |
| Non-White | 39.7 | 79 | 52.6 | 30 | ||
| Psychiatric Diagnosis at Age 3–6 | 45.2 | 90 | 68.4 | 39 | 9.17 | 0.0025 |
| Mean | SD | Mean | SD | t | p | |
|
|
||||||
| Income-to-needs ratio | 2.23 | 1.14 | 1.79 | 1.28 | 2.51 | 0.0127 |
| Early psychosocial adversity | 0.66 | 0.86 | 0.93 | 0.98 | −2.03 | 0.0429 |
Influence of Early Psychosocial Adversity, Income-to-Needs, and Psychiatric Disorders on Latent Class Membership
Family income-to-needs ratio and early psychosocial adversity were included as predictor variables in the GMM’s53. Family income-to-needs ratio during the preschool period differentiated the high, increasing trajectory class of physical health problems from the low class of physical health problems (χ2(1) = 4.391, p=.036), such that children in the low latent class had families with greater incomes relative to needs (M= 2.226; SE= 0.083) compared to children in the high latent class (M=1.809; SE= 0.176). In addition, early psychosocial adversity, experienced before age 6 was a significant predictor of latent class membership (χ2(1) = 4.246, p=.039). Children in the high, increasing trajectory of physical health problems were more likely to experience adversity prior to age 6 (M= 0.956; SE= 0.133) compared to children in the low latent class (M= 0.649; SE= 0.062).
The presence of psychiatric disorders during the preschool period significantly predicted membership in the high, increasing trajectory of physical health problems (χ2(1) = 9.17, p=.003).
Influence of the Predictors on Individual Intercepts and Slopes from Growth Mixture Models of Physical Health Problems
As noted above, the individuals in the high, increasing trajectory both started with higher physical health problems (higher intercept) and showed a steeper increase over time (steeper slope). Thus, we wished to determine whether early psychosocial adversity, income-to-needs, and psychiatric disorders were related to both the intercepts and slopes of the growth mixture models. Early psychosocial adversity, income-to-needs, and psychiatric disorders each predicted the individual intercepts of the growth mixture models (Table 4). Individual slopes were not significantly predicted by early psychosocial adversity, income-to-needs, or psychiatric disorders after adjusting for individual intercepts.
Table 4.
Potential Predictors of Individual Intercepts from GMM of Physical Health in Univariate Linear Regression Models
| Estimate | SE | t | p | |
|---|---|---|---|---|
| Income-to-needs ratio | −0.014 | 0.006 | −2.53 | 0.0120 |
| Early psychosocial adversity | 0.019 | 0.008 | 2.45 | 0.0151 |
| Psychiatric Diagnoses at Age 3–6 | 0.049 | 0.013 | 3.64 | <0.001 |
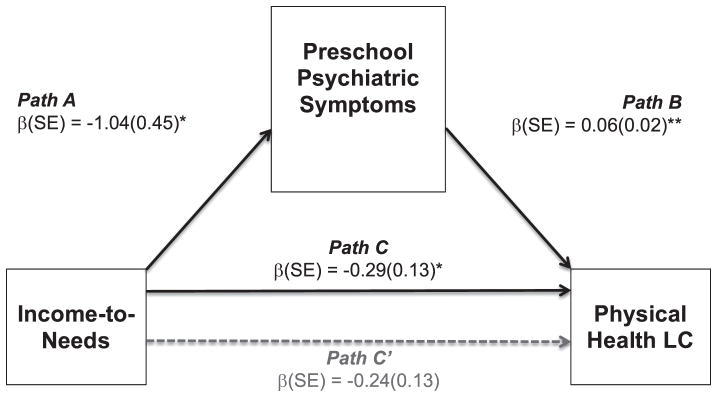
Mediation Analyses
As shown in Figure 3, income-to-needs ratio significantly predicted more psychiatric symptoms during preschool (path a). In turn, psychiatric symptoms predicted membership in the high, increasing latent class of physical health problems (path b). The relation between income-to-needs and latent class membership (path c) was also significant, with lower income-to-needs predicting membership in the high, increasing latent class. Path c’ was non-significant and there was a significant effect for the meditational path via calculation of the indirect effect, a*b (Figure 2; β= −0.29, p<.021).
Figure 3.
Indirect effect of total preschool depression, externalizing, and internalizing symptoms in the relation between income-to-needs and latent class of physical health problems
LC = latent class
Indirect effect of adversity on high LC = 95% CI: −0.142 to −0.011
Direct effect of adversity on high LC = 95% CI: −0.493 to 0.018
Total effect of adversity on high LC = 95% CI: −0.543 to −0.044
*p<.05, **p<.001
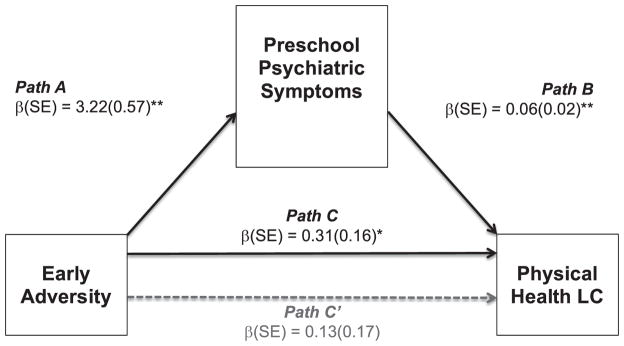
The mediation model for early psychosocial adversity was also significant (Figure 4). Greater psychosocial adversity predicted more psychiatric symptoms during preschool (path a). In turn, psychiatric symptoms predicted membership in the high, increasing latent class of physical health problems (path b). The relation between early psychosocial adversity and latent class membership (path c) was also significant, with greater psychosocial adversity predicting membership in the high, increasing latent class. The c’ prime path was non-significant. The indirect effect (a*b) was significant (Figure 3; β= 0.31, p=.050), indicative of mediation.
Figure 4.
Indirect effect of total preschool depression, externalizing, and internalizing symptoms in the relation between early adversity and latent class of physical health problems
LC = latent class
Indirect effect of adversity on high LC = 95% CI: 0.061 to 0.336
Direct effect of adversity on high LC = 95% CI: −0.208 to 0.470
Total effect of adversity on high LC = 95% CI: 0.001 to 0.620
*p<.05, **p<.001
Discussion
There has been little research examining early-onset psychiatric disorders as a mechanism associated with physical health problems throughout childhood29,54–56. By extending the literature on relationship of early adversity to the trajectories of physical health problems assessed from preschool to early adolescence, these findings indicate the importance and predictive power of early financial advantage/disadvantage, psychosocial adversity, and psychiatric disorders occurring during the preschool period for contributing to increasing physical health problems from preschool through early adolescence. The analyses distinguished between financial advantage/disadvantage, which includes income and SES-type indicators as a proxy for poverty8 from psychosocial adversity, which includes specific, measureable instances of how a child experiences adversity such as abuse, foster care placement, and caregiver arrest, yet findings were similar across types of adversity. The findings from this study suggest that the co-occurrence between early physical and mental health problems, as well as early adversity may be of significant public health importance, particularly given the rise in prevalence rates for chronic health problems in children57. Further, the results highlight the key role of early mental health problems in predicting later physical health, a finding that has not yet been reported in the literature and has yet to be emphasized by public policy.
Using growth mixture modeling to create latent class trajectories of physical health problems, a two-class solution provided the best balance between statistical indices of fit and the number of children in each trajectory class. A low latent class was comprised of youth whose physical health problems were minimal and remained stable and low throughout the duration of the study. On the other hand, during the preschool period, children in the high latent class were reporting almost twice the number of physical health concerns as children in the low latent class. Thus, differences in physical health problems were evident even among the youngest ages assessed in the sample, suggesting that physical health concerns may begin at a very young age for some children. The youth in the low physical health problems latent class evidenced a significant quadratic slope over time, indicating that these youth initially showed a decline in physical health problems, followed by a rise in later years. Further, the youth in the high latent class showed a significant positive linear slope, signifying a faster rate of increase in physical health problems from preschool through early adolescence. These trajectories offer unique insights into the course of physical health concerns beginning during preschool and the continuation of these early-onset problems into adolescence, in a sample of youth who were not recruited on the basis of physical health problems.
Both high financial disadvantage and high levels of early psychosocial adversity predicted membership in the increasing class of physical health problems from preschool through early adolescence. While at first glance these concepts may seem similar, and they are indeed related, they actually refer to two different processes: family financial strain versus the experience of specific psychosocial stressors. In this study, both appear to be influencing physical health problems in children. These findings replicate work with adults showing that childhood socioeconomic status and poverty predicts adult physical health problems58–60. However, our findings focus specifically on the childhood period, suggesting that the relationship between early adversity and physical health problems often seen in the adult literature may begin much earlier than previously recognized. Furthermore, our measures of family income-to-needs ratios and psychosocial adversity were only assessed between the ages of 3–6, and it is striking that these early measures of risk exerted such a strong influence on latent class trajectory membership through age 13. These empirical findings are consistent with a model proposed by Miller and Chen suggesting that early adversity affects behaviors that then affect health trajectories34,61.
These findings link work from two existing areas in the literature, studies that have focused on the impact of poverty on physical health9 as well as studies that have focused on the impact of adverse child experiences on physical health14. This represents an advance from prior studies, as most have not assessed or examined the role of co-morbid, early-occurring mental health problems. Of greater interest is that early-onset psychiatric disorders mediated relations between psychosocial adversity and physical health problems, as well as between financial advantage/disadvantage and physical health problems. Thus, early-onset psychiatric disorders accounted for much of the relation between early psychosocial adversity and later physical health problems and financial advantage/disadvantage and later physical health problems. The similar impact of early financial advantage/disadvantage and psychosocial adversity on physical health may have great public health significance. In this study, both financial advantage/disadvantage and psychosocial adversity occurred early in the child’s life (between ages 3–6), when children depend on caregivers to respond and tend to their physical and mental health complaints. Caregivers experiencing high levels of adversity may fail to recognize early indicators of poor physical and mental health, increasing the likelihood for more serious, chronic conditions to emerge.
In fact, the number of children with chronic health conditions has increased dramatically over the past four decades and increased health care utilization and costs57. In addition, increasing evidence supports a close relationship between physical and mental health problems, as well as the development of new models of care to address both in tandem62,63. By assessing both mental and physical health problems in the same sample, across time, researchers can begin to uncover the complex interplay between mental and physical health as well as determine any underlying physiological processes that may promote risk for both types of conditions18,64. Further, the recognition and treatment of mental health problems in early childhood remains a highly neglected area and these findings suggest that greater attention to treatment of these disorders may have broader health effects downstream.
While this study has strength in the use of a relatively large sample of youth followed longitudinally across a span of ten years, the sample is on the smaller side for conducting more complex GMM’s and therefore has reduced power to detect additional distinctions (e.g., sex) between trajectory classes. Detailed clinical interviews were conducted with all youth during the preschool period, however our measurement of physical health problems was limited by the use of a parent-report questionnaire. Additionally given that maternal/caregiver report was used for assessment of psychiatric symptoms, physical health, and adversity, social desirability bias may need to be considered when evaluating the validity of these reports. In particular, it is likely that caregivers may underreport their children’s exposure to adversity. Future work may wish to include more detailed and objective measurements of physical health problems. We are currently collecting follow-up assessments of this sample through later adolescence and including more objective and specific assessments of physical health (e.g. use of accelerometers/sedentary behavior) that will be important to investigate fluctuations in physical health trajectories over time. Rather than including a single predictor of psychosocial risk, such as parental education or income, this study is also strengthened from creating a cumulative variable encompassing seven indicators of psychosocial risk. However, the levels of exposure to psychosocial adversity in this sample were slightly lower than the rates of exposure seen in past work that has specifically recruited children at high-risk for child abuse and neglect. This composite variable also had low internal consistency reliability in the current study, limiting the interpretations that can be drawn from these findings. The inclusion of additional predictive and mediating variables, such as familial and/or biological indices could further elucidate trajectories of physical health problems throughout childhood.
The findings from this study suggest that early-onset psychiatric disorders may alter the course of physical health problems since children with early onset disorders were more likely to have increasing physical health problems over time. Children presenting with early-onset psychopathology and early psychosocial adversity may need to be more carefully screened for physical health difficulties, as these results suggest that this co-occurrence may increase the likelihood and severity of physical health problems later in childhood and adolescence. These results indicate that the regular screening of physical health problems for children presenting with mental health problems, and screening for mental health problems among children presenting with physical health problems may be needed and decrease the likelihood for negative health trajectories and high rates of co-morbidity. From a public health standpoint, these findings raise concern about the nature and course of both physical and mental health problems in very young children, as physical health problems are most often assessed as an outcome later in life and not as a phenomenon that may be altered earlier in development. Earlier intervention addressing psychosocial and physiological indices in children facing both early adversity and preschool psychopathology may be warranted. For example, children whose families have lower income-to-need ratios and early-onset psychiatric disorders are at greater risk for increasing physical health problems and may benefit from earlier interventions aimed at decreasing the influence their symptoms may have on their physical health during early childhood.
Supplementary Material
Acknowledgments
All phases of this study were supported by an NIH grant, R01 MH064769-06A1. Dr. Whalen’s work was supported by NIH grants: T32 MH100019 (PI’s: Barch and Luby) and L30 MH108015 (PI: Whalen). The authors wish to thank the children, caregivers, and staff of the Preschool Depression Study for their time and dedication to this project.
List of Abbreviations used in Text
- SES
socioeconomic status
- BMI
body mass index
- GMM
growth mixture modeling
- PDS
preschool depression study
- WUSM
Washington University School of Medicine
- PFC
Preschool Feelings Checklist
- CFA
confirmatory factor analysis
- PAPA
Preschool Age Psychiatric Assessment
- FIML
full information maximum likelihood
- MAR
missing at random
- BIC
Bayesian Information Criterion (BIC)
- LRT
likelihood ratio test
Footnotes
Conflict of Interest: Dr. Luby reports receiving royalties from Guilford Press for a book on preschool mental health. Dr. Barch consults for Pfizer, Amgen, Takeda, and Roche on psychosis related work.
References
- 1.McLaughlin KA. Future Directions in Childhood Adversity and Youth Psychopathology. J Clin Child Adolesc Psychol. 2016;45(3):361–382. doi: 10.1080/15374416.2015.1110823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.McLaughlin KA, Sheridan MA, Lambert HK. Childhood adversity and neural development: deprivation and threat as distinct dimensions of early experience. Neurosci Biobehav Rev. 2014;47:578–591. doi: 10.1016/j.neubiorev.2014.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Melchior M, Moffitt TE, Milne BJ, Poulton R, Caspi A. Why Do Children from Socioeconomically Disadvantaged Families Suffer from Poor Health When They Reach Adulthood? A Life-Course Study. Am J Epidemiol. 2007;166(8):966–974. doi: 10.1093/aje/kwm155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chen E, Martin AD, Matthews KA. Trajectories of Socioeconomic Status Across Children’s Lifetime Predict Health. Pediatrics. 2007;120(2):e297–e303. doi: 10.1542/peds.2006-3098. [DOI] [PubMed] [Google Scholar]
- 5.Lanier P, Jonson-Reid M, Stahlschmidt MJ, Drake B, Constantino J. Child Maltreatment and Pediatric Health Outcomes: A Longitudinal Study of Low-income Children. J Pediatr Psychol. 2010;35(5):511–522. doi: 10.1093/jpepsy/jsp086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hussey JM, Chang JJ, Kotch JB. Child Maltreatment in the United States: Prevalence, Risk Factors, and Adolescent Health Consequences. Pediatrics. 2006;118(3):933–942. doi: 10.1542/peds.2005-2452. [DOI] [PubMed] [Google Scholar]
- 7.Luecken LJ, Lemery KS. Early caregiving and physiological stress responses. Clin Psychol Rev. 2004;24(2):171–191. doi: 10.1016/j.cpr.2004.01.003. [DOI] [PubMed] [Google Scholar]
- 8.Johnson SB, Riis JL, Noble KG. State of the Art Review: Poverty and the Developing Brain. Pediatrics. 2016;137(4) doi: 10.1542/peds.2015-3075. peds.2015–3075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Spencer N, Thanh TM, Louise S. Low Income/Socio-Economic Status in Early Childhood and Physical Health in Later Childhood/Adolescence: A Systematic Review. Matern Child Health J. 2012;17(3):424–431. doi: 10.1007/s10995-012-1010-2. [DOI] [PubMed] [Google Scholar]
- 10.Flaherty EG, Thompson R, Dubowitz H, et al. Adverse childhood experiences and child health in early adolescence. JAMA Pediatr. 2013;167(7):622–629. doi: 10.1001/jamapediatrics.2013.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Power C, Kuh D, Morton S. From Developmental Origins of Adult Disease to Life Course Research on Adult Disease and Aging: Insights from Birth Cohort Studies. Annu Rev Public Health. 2013;34(1):7–28. doi: 10.1146/annurev-publhealth-031912-114423. [DOI] [PubMed] [Google Scholar]
- 12.Vella SA, Magee CA, Cliff DP. Trajectories and Predictors of Health-Related Quality of Life during Childhood. J Pediatr. 2015;167(2):422–427. doi: 10.1016/j.jpeds.2015.04.079. [DOI] [PubMed] [Google Scholar]
- 13.Flaherty EG, Thompson R, Litrownik AJ, et al. Effect of early childhood adversity on child health. Arch Pediatr Adolesc Med. 2006;160(12):1232–1238. doi: 10.1001/archpedi.160.12.1232. [DOI] [PubMed] [Google Scholar]
- 14.Flaherty EG, Thompson R, Litrownik AJ, et al. Adverse Childhood Exposures and Reported Child Health at Age 12. Acad Pediatr. 2009;9(3):150–156. doi: 10.1016/j.acap.2008.11.003. [DOI] [PubMed] [Google Scholar]
- 15.Thompson R, Flaherty EG, English DJ, et al. Trajectories of Adverse Childhood Experiences and Self-Reported Health at Age 18. Acad Pediatr. 2015;15(5):503–509. doi: 10.1016/j.acap.2014.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Flaherty EG, Thompson R, Litrownik AJ, et al. Effect of early childhood adversity on child health. Arch Pediatr Adolesc Med. 2006;160(12):1232–1238. doi: 10.1001/archpedi.160.12.1232. [DOI] [PubMed] [Google Scholar]
- 17.Braveman P, Barclay C. Health Disparities Beginning in Childhood: A Life-Course Perspective. Pediatrics. 2009;124(Supplement 3):S163–S175. doi: 10.1542/peds.2009-1100D. [DOI] [PubMed] [Google Scholar]
- 18.Nusslock R, Miller GE. Early-Life Adversity and Physical and Emotional Health Across the Lifespan: A Neuroimmune Network Hypothesis. Biol Psychiatry. doi: 10.1016/j.biopsych.2015.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wickrama KaS, Conger RD, Abraham WT. Early Adversity and later health: The intergenerational transmission of adversity through mental disorder and physical illness. J Gerontol B Psychol Sci Soc Sci. 2005;60(Special Issue 2):S125–S129. doi: 10.1093/geronb/60.Special_Issue_2.S125. [DOI] [PubMed] [Google Scholar]
- 20.Belsky J, Bell B, Bradley RH, Stallard N, Stewart-Brown SL. Socioeconomic risk, parenting during the preschool years and child health age 6 years. Eur J Public Health. 2007;17(5):508–513. doi: 10.1093/eurpub/ckl261. [DOI] [PubMed] [Google Scholar]
- 21.Adler N, Bush NR, Pantell MS. Rigor, vigor, and the study of health disparities. Proc Natl Acad Sci. 2012;109(Supplement 2):17154–17159. doi: 10.1073/pnas.1121399109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ferro MA. Mediated moderation of the relation between maternal and adolescent depressive symptoms: role of adolescent physical health. Soc Psychiatry Psychiatr Epidemiol. 2015;50(11):1743–1751. doi: 10.1007/s00127-015-1103-5. [DOI] [PubMed] [Google Scholar]
- 23.Ferro MA, Boyle MH, Avison WR. Association between trajectories of maternal depression and subsequent psychological functioning in youth with and without chronic physical illness. Health Psychol. 2015;34(8):820–828. doi: 10.1037/hea0000226. [DOI] [PubMed] [Google Scholar]
- 24.Kessler RC, McLaughlin KA, Green JG, et al. Childhood adversities and adult psychopathology in the WHO World Mental Health Surveys. Br J Psychiatry. 2010;197(5):378–385. doi: 10.1192/bjp.bp.110.080499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McLaughlin KA, Greif Green J, Gruber MJ, Sampson NA, Zaslavsky AM, Kessler RC. CHildhood adversities and first onset of psychiatric disorders in a national sample of us adolescents. Arch Gen Psychiatry. 2012;69(11):1151–1160. doi: 10.1001/archgenpsychiatry.2011.2277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ferro MA, Gorter JW, Boyle MH. Trajectories of Depressive Symptoms in Canadian Emerging Adults. Am J Public Health. 2015;105(11):2322–2327. doi: 10.2105/AJPH.2015.302817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jones DR, Macias C, Barreira PJ, Fisher WH, Hargreaves WA, Harding CM. Prevalence, Severity, and Co-occurrence of Chronic Physical Health Problems of Persons With Serious Mental Illness. Psychiatr Serv. 2004;55(11):1250–1257. doi: 10.1176/appi.ps.55.11.1250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ferro MA, Boyle MH. The Impact of Chronic Physical Illness, Maternal Depressive Symptoms, Family Functioning, and Self-esteem on Symptoms of Anxiety and Depression in Children. J Abnorm Child Psychol. 2014;43(1):177–187. doi: 10.1007/s10802-014-9893-6. [DOI] [PubMed] [Google Scholar]
- 29.Pinquart M, Shen Y. Depressive Symptoms in Children and Adolescents with Chronic Physical Illness: An Updated Meta-Analysis. J Pediatr Psychol. 2011;36(4):375–384. doi: 10.1093/jpepsy/jsq104. [DOI] [PubMed] [Google Scholar]
- 30.Pinquart M, Shen Y. Behavior Problems in Children and Adolescents With Chronic Physical Illness: A Meta-Analysis. J Pediatr Psychol. 2011;36(9):1003–1016. doi: 10.1093/jpepsy/jsr042. [DOI] [PubMed] [Google Scholar]
- 31.Crowell SE, Puzia ME, Yaptangco M. The ontogeny of chronic distress: emotion dysregulation across the life span and its implications for psychological and physical health. Curr Opin Psychol. 2015;3:91–99. [Google Scholar]
- 32.Koenig J, Kemp AH, Beauchaine TP, Thayer JF, Kaess M. Depression and resting state heart rate variability in children and adolescents — A systematic review and meta-analysis. Clin Psychol Rev. 2016;46:136–150. doi: 10.1016/j.cpr.2016.04.013. [DOI] [PubMed] [Google Scholar]
- 33.Miller G, Chen E, Cole SW. Health Psychology: Developing Biologically Plausible Models Linking the Social World and Physical Health. Annu Rev Psychol. 2009;60(1):501–524. doi: 10.1146/annurev.psych.60.110707.163551. [DOI] [PubMed] [Google Scholar]
- 34.Miller GE, Chen E. The Biological Residue of Childhood Poverty. Child Dev Perspect. 2013;7(2):67–73. doi: 10.1111/cdep.12021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Luby JL, Si X, Belden AC, Tandon M, Spitznagel E. Preschool depression: Homotypic continuity and course over 24 months. Arch Gen Psychiatry. 2009;66(8):897–905. doi: 10.1001/archgenpsychiatry.2009.97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Luby JL, Gaffrey MS, Tillman R, April LM, Belden AC. Trajectories of preschool disorders to full DSM depression at school age and early adolescence: Continuity of preschool depression. Am J Psychiatry. 2014;171(7):768–776. doi: 10.1176/appi.ajp.2014.13091198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Luby JL, Heffelfinger A, Koenig-McNaught AL, Brown K, Spitznagel E. The Preschool Feelings Checklist: A Brief and Sensitive Screening Measure for Depression in Young Children. J Am Acad Child Adolesc Psychiatry. 2004;43(6):708–717. doi: 10.1097/01.chi.0000121066.29744.08. [DOI] [PubMed] [Google Scholar]
- 38.Slopen N, Koenen KC, Kubzansky LD. Cumulative Adversity in Childhood and Emergent Risk Factors for Long-Term Health. J Pediatr. 2014;164(3):631–638. e2. doi: 10.1016/j.jpeds.2013.11.003. [DOI] [PubMed] [Google Scholar]
- 39.McLoyd VC. Socioeconomic disadvantage and child development. Am Psychol. 1998;53(2):185–204. doi: 10.1037/0003-066X.53.2.185. [DOI] [PubMed] [Google Scholar]
- 40.Essex MJ, Boyce WT, Goldstein L, Armstrong J, Kraemer HC, Kupfer DJ. The Confluence of Mental, Physical, Social, and Academic Difficulties in Middle Childhood. II: Developing the MacArthur Health and Behavior Questionnaire. J Am Acad Child Adolesc Psychiatry. 2002;41(5):588–603. doi: 10.1097/00004583-200205000-00017. [DOI] [PubMed] [Google Scholar]
- 41.Egger HL, Ascher B, Angold A. The Preschool Age Psychiatric Assessment: Version 1.4. Center for Developmental Epidemiology, Department of Psychiatry and Behavioral Sciences. Duke Univ Med Cent Durh NC. 2003 [Google Scholar]
- 42.Egger HL, Erkanli A, Keeler G, Potts E, Waltr BK, Angold A. Test-Retest Reliability of the Preschool Age Psychiatric Assessment (PAPA) J Am Acad Child Adolesc Psychiatry. 2006;45(5):538–549. doi: 10.1097/01.chi.0000205705.71194.b8. [DOI] [PubMed] [Google Scholar]
- 43.Jung T, Wickrama KaS. An Introduction to Latent Class Growth Analysis and Growth Mixture Modeling. Soc Personal Psychol Compass. 2008;2(1):302–317. doi: 10.1111/j.1751-9004.2007.00054.x. [DOI] [Google Scholar]
- 44.Muthén B, Muthén LK. Integrating Person-Centered and Variable-Centered Analyses: Growth Mixture Modeling With Latent Trajectory Classes. Alcohol Clin Exp Res. 2000;24(6):882–891. doi: 10.1111/j.1530-0277.2000.tb02070.x. [DOI] [PubMed] [Google Scholar]
- 45.Muthén B, Muthén LK. Mplus Version 7: User’s guide. Los Angel CA: Muthén Muthén; 2012. [Google Scholar]
- 46.Asendorpf JB, Schoot R, van de Denissen JJA, Hutteman R. Reducing bias due to systematic attrition in longitudinal studies: The benefits of multiple imputation. Int J Behav Dev. 2014;38(5):453–460. doi: 10.1177/0165025414542713. [DOI] [Google Scholar]
- 47.Ferro MA. Missing data in longitudinal studies: cross-sectional multiple imputation provides similar estimates to full-information maximum likelihood. Ann Epidemiol. 2014;24(1):75–77. doi: 10.1016/j.annepidem.2013.10.007. [DOI] [PubMed] [Google Scholar]
- 48.Nylund KL, Asparouhov T, Muthén BO. Deciding on the Number of Classes in Latent Class Analysis and Growth Mixture Modeling: A Monte Carlo Simulation Study. Struct Equ Model Multidiscip J. 2007;14(4):535–569. doi: 10.1080/10705510701575396. [DOI] [Google Scholar]
- 49.Berlin KS, Parra GR, Williams NA. An Introduction to Latent Variable Mixture Modeling (Part 2): Longitudinal Latent Class Growth Analysis and Growth Mixture Models. J Pediatr Psychol. 2014;39(2):188–203. doi: 10.1093/jpepsy/jst085. [DOI] [PubMed] [Google Scholar]
- 50.Berlin KS, Williams NA, Parra GR. An Introduction to Latent Variable Mixture Modeling (Part 1): Overview and Cross-Sectional Latent Class and Latent Profile Analyses. J Pediatr Psychol. 2014;39(2):174–187. doi: 10.1093/jpepsy/jst084. [DOI] [PubMed] [Google Scholar]
- 51.Hayes AF. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach. Guilford Press; 2013. [Google Scholar]
- 52.Hayes AF. PROCESS: A versatile computational tool for observed variable mediation, moderation, and conditional process modeling. 2012. [Google Scholar]
- 53.Asparouhov T, Muthén B. Auxiliary Variables in Mixture Modeling: Three-Step Approaches Using Mplus. Struct Equ Model Multidiscip J. 2014;21(3):329–341. doi: 10.1080/10705511.2014.915181. [DOI] [Google Scholar]
- 54.Goodwin RD, Sourander A, Duarte CS, et al. Do mental health problems in childhood predict chronic physical conditions among males in early adulthood? Evidence from a community-based prospective study. Psychol Med. 2009;39(02):301–311. doi: 10.1017/S0033291708003504. [DOI] [PubMed] [Google Scholar]
- 55.Gonzalez A, Boyle MH, Kyu HH, Georgiades K, Duncan L, MacMillan HL. Childhood and family influences on depression, chronic physical conditions, and their comorbidity: Findings from the Ontario Child Health Study. J Psychiatr Res. 2012;46(11):1475–1482. doi: 10.1016/j.jpsychires.2012.08.004. [DOI] [PubMed] [Google Scholar]
- 56.McCloughen A, Foster K, Huws-Thomas M, Delgado C. Physical health and wellbeing of emerging and young adults with mental illness: An integrative review of international literature. Int J Ment Health Nurs. 2012;21(3):274–288. doi: 10.1111/j.1447-0349.2011.00796.x. [DOI] [PubMed] [Google Scholar]
- 57.Perrin JM, Bloom SR, Gortmaker SL. THe increase of childhood chronic conditions in the united states. JAMA. 2007;297(24):2755–2759. doi: 10.1001/jama.297.24.2755. [DOI] [PubMed] [Google Scholar]
- 58.Cohen S, Janicki-Deverts D, Chen E, Matthews KA. Childhood socioeconomic status and adult health. Ann N Y Acad Sci. 2010;1186(1):37–55. doi: 10.1111/j.1749-6632.2009.05334.x. [DOI] [PubMed] [Google Scholar]
- 59.Luo Y, Waite LJ. The Impact of Childhood and Adult SES on Physical, Mental, and Cognitive Well-Being in Later Life. J Gerontol B Psychol Sci Soc Sci. 2005;60(2):S93–S101. doi: 10.1093/geronb/60.2.S93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.McEwen BS. Early life influences on life-long patterns of behavior and health. Ment Retard Dev Disabil Res Rev. 2003;9(3):149–154. doi: 10.1002/mrdd.10074. [DOI] [PubMed] [Google Scholar]
- 61.Miller GE, Chen E, Fok AK, et al. Low early-life social class leaves a biological residue manifested by decreased glucocorticoid and increased proinflammatory signaling. Proc Natl Acad Sci. 2009;106(34):14716–14721. doi: 10.1073/pnas.0902971106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Care AD, Siegel BS, Shonkoff JP, Garner AS, et al. Pediatrics AS on D and B, Health TC on PA of C and F, Childhood C on E, Adoption. The Lifelong Effects of Early Childhood Adversity and Toxic Stress. Pediatrics. 2012;129(1):e232–e246. doi: 10.1542/peds.2011-2663. [DOI] [PubMed] [Google Scholar]
- 63.Shonkoff JP, Boyce W, McEwen BS. Neuroscience, molecular biology, and the childhood roots of health disparities: Building a new framework for health promotion and disease prevention. JAMA. 2009;301(21):2252–2259. doi: 10.1001/jama.2009.754. [DOI] [PubMed] [Google Scholar]
- 64.Chiang JJ, Taylor SE, Bower JE. Early adversity, neural development, and inflammation. Dev Psychobiol. 2015 Sep; doi: 10.1002/dev.21329. n/a - n/a. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.