Abstract
Coronary artery calcification (CAC) is an established marker of subclinical atherosclerosis and an independent predictor of future coronary heart disease in the asymptomatic primary prevention population, particularly in the intermediate risk cohort. CAC also helps in reclassifying those patients and their risk of cardiovascular events into higher or lower risk categories. MESA (Multi-Ethnic Study of Atherosclerosis) is a NHLBI-sponsored population-based medical research study involving 6,814 men and women from six US communities without a medical history of clinical cardiovascular disease. The evidence from this population cohort revealed that CAC scoring was independently predictive and highly effective at risk stratification of major adverse cardiac events. This article provides available data based on MESA. We focus on the utility of CAC for stratification of individuals and we describe its diagnostic value in identifying patients at risk.
Introduction
Coronary artery calcification (CAC) scanning provides a distinct means of measuring atherosclerosis and is an established predictor for adverse cardiovascular events. [1, 2] CAC can form in the advanced phase of atherosclerosis and reflects a linear estimate of the overall plaque burden of coronary artery atherosclerosis. The presence of a greater CAC score is associated with a higher risk of adverse cardiovascular events and all-cause mortality [3–5]; and thus, guidelines suggest patients with an excessively high CAC score should be treated as high risk patients. MESA (Multi-Ethnic Study of Atherosclerosis) is a NHLBI-sponsored population-based medical research study involving 6,814 men and women without medical history of clinical cardiovascular disease from six US communities including Baltimore, Maryland; Chicago, Illinois; Forsyth, North Carolina; Los Angeles, California; New York, New York; and St. Paul, Minnesota. The purpose of MESA is to investigate the correlations between risk factors including CAC and progression of subclinical cardiovascular disease using Cardiac CT. One cardinal question was whether the CAC score could improve risk prediction beyond the traditional risk factors in an asymptomatic population of the same age, gender and ethnicity. It is important for clinicians to understand the diagnostic value of the CAC score and its implications for long term prognosis in asymptomatic individuals. In this review, we describe the available data supporting the application of CAC.
Which sub-populations have more CAC?
Bild et al. clearly defined the distribution of CAC score among a wide range of patients by age, gender or race/ethnicity and defined their normal values of CAC. [6] They revealed that the relative risks for having CAC compared with Caucasians was 0.78 in African-Americans (95% CI 0.74–0.82), 0.85 in Hispanics (95% CI 0.80–0.91), and 0.92 in Chinese (95% CI 0.85–0.995). [6] McClelland et al. then reported that men had a much greater CAC score compared with females of the same age and, moreover, increasing age showed positive correlation with CAC.[7] Among the different race/ethnic subgroups studied in MESA (Chinese, Hispanics, Caucasians and African-Americans), the CAC score was highest in Caucasian and Hispanic men, with African-Americans having significantly lower prevalence and severity of CAC. Similarly, Caucasian and Hispanic females had the highest CAC score.[7] Incidence and progression of CAC strongly correlated with traditional atherosclerotic factors such as age, gender, race, body mass index (BMI), history of hypertension, diabetes and family history of heart attack. [8–13] DeFlippis et al. reported both a higher Framingham risk score (FRS) calculated with age, gender, blood pressure, total cholesterol, high density cholesterol and smoking history, and a higher Reynolds risk score (RRS), which could be calculated FRS plus high-sensitivity C-reactive protein levels and parental history, could predict the incidence and progression of CAC.[14] Furthermore, Admed et al. reported an interesting relationship between lifestyle and CAC score from the MESA population. Diet, BMI, smoking status and physical activity levels determine the lifestyle score, which is positively correlated with CAC and mortality. [15]
The utility of CAC for predicting CHD/CVD events
All adults are initially required to undergo an office-based assessment to identify those at higher risk for coronary events using quantitative risk predictive estimate systems, such as the FRS or the new American College of Cardiology/American Heart Association (ACC/AHA) Pooled Risk Calculator. FRS is a traditional risk stratification of cardiovascular disease and could predict the 10-year cardiovascular risk of an individual and categorize risk for developing cardiovascular disease (CVD) into low (10 year risk of <10%), intermediate (10 year risk of 10–20%) and high (10 year risk of >20%) risk.[16] Although the FRS is widely used as the primary CVD risk assessment, it has some limitations. The FRS could predict, only modestly, CHD events with a c-statistic value of approximately 0.70 [17, 18] and could not classify younger populations nor females as precisely as high risk cohorts, despite substantial risk factor burden. [19–21]. Thus, additional tests of cardiovascular risk such as CAC scoring have been evaluated as possible ways to improve global CHD risk assessment.
The CAC score itself is a strong predictor of CHD and CVD events. Budoff et al. reported the clinical importance of a CAC score of zero.[22] MESA participants with a CAC score of 1–10 experienced CHD events with a hazard ratio of 3.66 compared to those with a CAC score of zero after adjusting for age, gender, race, and CHD risk factors.[22] A CAC score of zero is considered a stronger negative risk predictor for all CHD/CVD events among negative atherosclerotic risk markers such as carotid intima-media thickness <25th percentile, absence of carotid plaque, brachial flow-mediated dilation >5% change, ankle-brachial index >0.9 and <1.3, high-sensitivity C-reactive protein <2 mg/L, homocysteine <10 μmol/L, N-terminal pro-brain natriuretic peptide <100 pg/mL, no microalbuminuria, no family history of coronary heart disease, absence of metabolic syndrome, and healthy lifestyle. [23] Thus, asymptomatic populations with a CAC score of zero could be considered to have very low risk of CHD. Among 1,850 MESA participants with a CAC score of zero as a baseline, those with a persistent CAC score of zero were significantly more likely to be younger, female, and have fewer traditional risk factors; however, there was no single risk factor or specific low-risk phenotype.[24] A CAC score of zero may be predominantly influenced by the long-term maintenance of low risk factors of cardiovascular disease or genetic factors rather than the absence of any specific risk factors in late adulthood.[24] In contrast, populations with a great CAC burden and serial CAC progression have significant risk of CHD. Detrano et al. reported that the adjusted risk of a coronary event increased by a factor of 7.73 among participants with a CAC score between 101 and 300, and by 9.67 among participants with a CAC score greater than 300, compared to the participants with a CAC score of zero (figure 1). [5] Moreover, Budoff et al. reported the clinical importance of CAC progression for predicting future CHD events.[25] Compared with participants with no increase in CAC score, any increase in CAC score was associated with greater risk for CHD events during the median 7.6 year follow up. Among the participants with a CAC score of zero, CAC progression of 5-units per year was associated with an adjusted HR of 1.4 (95% CI 1.0–1.9) for total CHD and an adjusted HR of 1.5 (95% CI; 1.1–2.1) for hard CHD. Among the participants with a CAC score of more than 0, CAC progression of a 100-unit change per year was associated with an adjusted HR of 1.2 (95% CI; 1.1–1.4) for total CHD and an adjusted HR of 1.3 (95% CI; 1.1–1.5) for hard CHD. [25] Silverman et al. reported CAC having a great impact on prognosis regardless of traditional risk factors including smoking, high low-density lipoprotein cholesterol, low high-density lipoprotein cholesterol, hypertension and diabetes within 7.1 years follow up. [26] Compared to individuals with more than three risk factors and a zero CAC score, those with zero risk factors and a CAC score greater than 300 had 3.5 times higher CHD event rate (3.1 per 1000 per year vs.10.9 per 1000 per year).[26] In terms of coronary artery stenosis, Rosen et al. reported relationships between baseline extent of CAC and the severity of coronary stenosis using coronary angiography.[27] The average CAC scores were 161.3±268.2, 462.7±608.5, 961.7± 986.9, 1351.4±1180.1 and 658.3±607.4 for patients without significant stenosis, 1-, 2-, 3-vessels disease and LMT disease, respectively (p<0.001). [27] Furthermore, a closer relationship was evident between CAC burden and the need for future revascularization. Within 8.5 years median follow up, the revascularization rates per 1000 per years for CAC scores of 1–100, 101–400 and greater than 400 were 4.9, 11.7 and 25.4, respectively.[28] Blaha et al. evaluated whether CAC may further stratify a JUPITER-eligible individuals (LDL cholesterol < 130 mg/dL and hs-CRP ≥ 2.0 mg/dL) in MESA study participants during median 5.8 years follow up.[29] The presence of CAC was associated with a 4.29-fold increased risk of CHD (95% CI 1.99 – 9.25) and a 2.57-fold increased risk of CVD (95% CI 1.48–4.48), while hs-CRP was not associated with either CHD or CVD after multivariate adjustment.[29]
Figure 1.
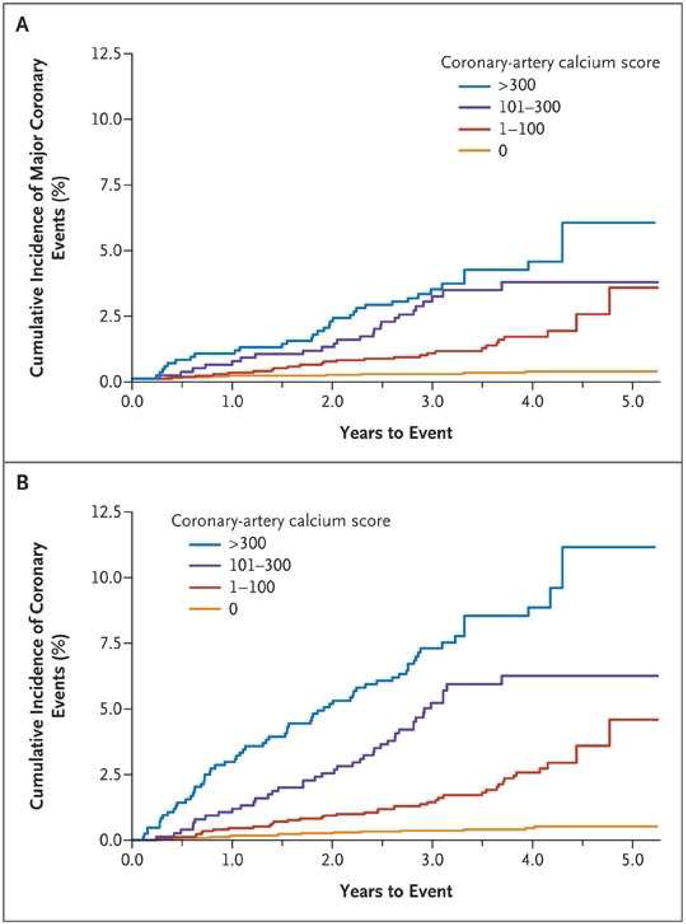
Unadjusted Kaplan–Meier Cumulative-Event Curves for major coronary events and for any coronary event according to coronary calcium score of 0, 1 to 100, 101 to 300, and More Than 300.
Panel A shows the rates for major coronary events (myocardial infarction and death from coronary heart disease), and Panel B shows the rates for any coronary event. The differences among all curves are statistically significant (P<0.001). (Reprinted with permission from Detrano [5])
Different CAC score cutoffs have been examined to distinguish the high risk population in MESA. Currently, CAC scores of 1–100, 101–300 and >300 are the most common used cutoffs points for increasing CHD risk. [5, 30] Moreover, some studies from MESA have revealed the significant association between CAC score and cerebrovascular diseases.[31, 32] Gibson et al. reported that CAC score was an independent risk factor of cerebrovascular disease and improves the ability of prediction for it by the Framingham stroke risk score. Log transformed CAC score was associated with the increased risk for cerebrovascular disease after adjusting for traditional risk factors (HR 1.13: 95% CI 1.07–1.20, p<0.0001).[32] MESA has established that the CAC score itself is a strong risk marker for future cerebrovascular events.
The utility of a CAC score in combination with other risk factors
CAC score assessment in combination with the FRS is useful compared with just FRS. Detrano et al. reported the clinical value of CAC score in combination with the traditional risk factors.[5] The areas under the receiver-operating-characteristic curves (AUC) analysis for the predictive value of major adverse coronary events and any coronary events increased from 0.79 to 0.83 (p=0.006) and from 0.77 to 0.82 (p<0.001), respectively.[5] Lakski, et al. stated the significant role of CAC score in subsequent risk for CHD and CVD events among 3,601 asymptomatic women classified as low risk based on FRS in MESA population. Compared to women with zero CAC score in low risk category with FRS, those with a CAC score greater than 0 in low risk category with FRS showed significant risk of CHD events (HR, 6.5; 95% CI 2.6–16.4) and CVD events (HR, 5.2; 95% CI, 2.5–10.8).[33] This result showed the possibility of a CAC score improving risk prediction obtained from FRS, especially in the female population, which was considered as a limitation. Polonsky et al. also reported the clinical significance of the CAC score for risk stratification in addition to traditional risk factors in each category.[3] Compared with factors alone, calculated by including models of FRS and race/ethnicity, the risk prediction of CHD events showed a significant improvement after including CAC scores. (NRI=0.25, 95% confidence interval 0.16–0.34, P<0.001). The AUC analysis for the prediction of CHD events was 0.76 (95% CI 0.72–0.79) using only traditional risk factors, which increased to 0.81 (95% CI 0.78 – 0.84) (P<0.001) with the model after the addition to CAC score. [3] Pletcher et al. reported CAC score could be used to improve the pretest CHD risk estimate in each individual clinical scenario.[34] The most interesting clinical scenario was the interpretation of the intermediate CAC score groups (1–100). In scenarios in which a high CAC score was expected, a moderately elevated CAC score of 1–100 was reassuring (reducing the risk from a pre-test CHD risk estimate of 10% to post-test risk estimate of 6% in a healthy older Caucasian man). However, when a low or zero CAC score was expected, even with identical pre-test CHD risk, the same CAC score of 1–100 may be alarmingly high (increasing the risk from a pre-test CHD risk estimate of 10% to a post-test risk estimate of 20% in a middle-aged African American women with multiple risk factors).[34] Moreover, a CAC score could have a superior diagnostic value for CHD and CVD compared with risk markers such as CIMT (Carotid intima-media thickness) [35, 36], brachial flow-mediated dilation (FMD), hsCRP, a family history of CHD and ABI (Ankle-brachial index) in non-diabetic population with intermediate-risk MESA participants. The CAC score could highly improve the area under the operating curve for incident CHD after combining it with FRS and race/ethnicity among the 6 risk markers (figure 2).[37] CAC screening can also improve CHD and CVD risk stratification in diabetic individuals.[38] Malik et al. reported that even when diabetes was present, if the CAC score was not significant, CHD or CVD event rates were as low as in those without diabetes; 0.1% of annual rate for CHD and 0.2% for CVD. They also showed a 10-fold variation in CHD event rates in those with diabetes or metabolic syndrome ranging from a zero CAC score to CAC score greater than 400. From AUC analysis, the CAC score addition to the adjusted models including traditional risk factors showed strong incremental predictive value for CHD compared with the adjusted models alone (0.78 vs. 0.72, p<0.0001) in diabetic populations. [38] Martin et al. reported the possibility of CAC in reclassification of population by the addition of a number of traditional lipid abnormalities including low-density lipoprotein cholesterol ≥ 130 mg/dL, high-density lipoprotein cholesterol <40 mg/dL for men or <50 mg/dL for women, and triglycerides ≥ 150 mg/dL.[39] Participants with a CAC score greater than 100 and no lipid abnormalities, showed higher event rates of CVD compared with the patients who had no CAC and three lipid abnormalities (22.7 versus 5.9 per 1000 person per years). Individuals without any lipid abnormalities by traditional definitions could be evaluated more accurately by adding a CAC score.[39] Recently, a report which focused on each component of the CAC score, including volume and density of CAC, was published.[40] Compared with base model containing the FRS, race/ethnicity and statin use, adding the CAC volume score and CAC density score to this base model significantly improved the predictive ability of CHD in the AUC analyses from 0.668 to 0.771, p=0.006. Similarly, the AUC for CVD increased from 0.669 to 0.704, p<0.001. Furthermore, the CAC density score showed a significantly stronger predictive value compared with the CAC volume score for CHD and CVD. [40] 2010 American College of Cardiology (ACC) and American Heart Association (AHA) guidelines have incorporated CAC for cardiovascular risk assessment in asymptomatic adults at intermediate risk (10–20% 10-years FRS risk: Class II a indication), for persons with diabetes (Class II a indication) and at low-intermediate risk (6–10% 10-years FRS risk: Class II b indication).
Figure 2.
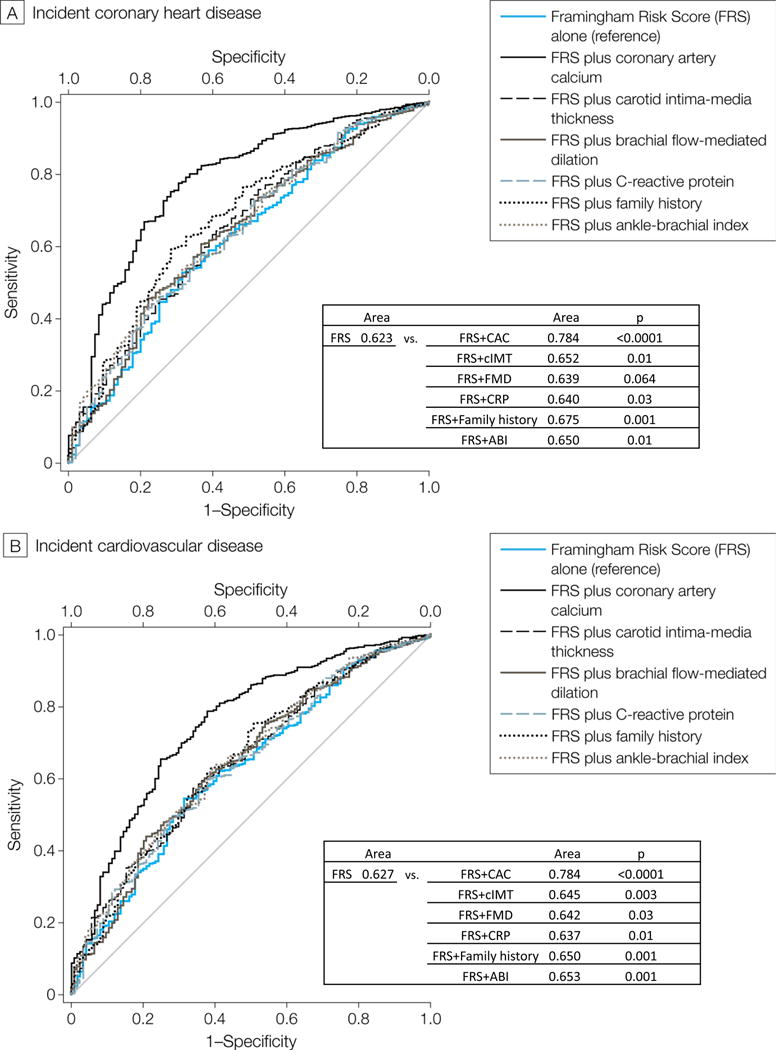
Receiver operator characteristic curves showing area under the curve for FRS alone vs. FRS plus CAC (coronary artery calcification), FRS plus IMT (intima-media thickness), FRS plus FMD (flow-mediated dilation), FRS plus CRP (high-sensitivity C- reactive protein), FRS plus family history and FRS plus ABI (ankle-brachial index) for incident CAD (A) and CVD (B) in MESA intermediate risk participants. (Reprinted with permission from Yeboah [37])
The utility of CAC score for patient’s treatment
In 2013, the ACC/AHA released the updated CVD prevention guidelines [41, 42]. Of note, the 2013 guidelines changed the outcome (atherosclerosis cardiovascular disease: ASCVD) to include stroke. Moreover, the guidelines moved away from LDL cholesterol level and instead, recommended the use of a statin for individuals with a 10-year ASCVD risk of greater than 7.5 %, which lowered from former threshold and the numbers of eligible individuals for statin therapy increased greatly. With the new guidelines, many future ASCVD events could be decreased; however, it could lead to potential overestimation in patients with lower ASCVD risk. [18, 43, 44] DeFilippis et al. showed the discriminative capability of the new 2013 guidelines in the 4,227 MESA participants.[18] They revealed an overestimation of the new guidelines in cardiovascular events (predicted events; 9.16% vs. observed events; 5.16%) and 78% of discordance. Discordance between observed and expected risk was found throughout the risk continuum, including those at moderate risk.[18] It is easy to imagine that risk overestimation could lead to increased use of preventive medications such as statin therapy, potentially exposing some patients to the unnecessary risks of these drugs and resulting in more health care cost. The CAC score could be suggested for evaluating individuals at intermediate risk when there is uncertainty about the role for lipid lowering agents.[44–46] Nasir et al. evaluated the utility of CAC score in reclassifying populations in ASCVD by each risk stratum in which statins were recommended according to the guidelines in 4,758 MESA population.[44] According to these guidelines, 2,377 participants were recommended for moderate to high intensity statin therapy. However, 41 % of the 2,377 participants had a CAC score of zero with only 5.2 events per 1000 persons per years. Among 589 participants considered for moderate intensity statin, 338 (57%) had a CAC score of zero, with an ASCVD event rate of only 1.5 per 1000 persons per year. From these results, almost 50% of the patients assigned statin treatment had low event rates and were actually low risk (<7.5% 10 year risk). Thus, a CAC score of zero could reclassify approximately one-half of candidates as not eligible for statin therapy. [44]
In contrast, in the 2013 guidelines, CAC scores of either ≥ 75th percentile for age and gender or ≥300 Agatston units were considered as high risk and warrant high dose statins. Based on studies from MESA, a CAC score of >100 was more predictive of events than >75th percentile, and achieve high cardiovascular risk, so we recommend use of a CAC score >100 as the cutpoint for aggressive statin therapy[30]. Kim et al. reported significant risk reduction of atorvastatin in individuals with a CAC score >400.[47] They demonstrated that atorvastatin reduced cardiovascular events by 42% in those with CAC score > 400, with a needed to treat (NNT) to reduce one myocardial infarction or death of only 16.[47]
The CAC score can robustly identify individuals who could benefit from anti-atherosclerotic therapies and also identify those who may not need any treatment.
Conclusion
In this review, we described the usefulness of the CAC as the strongest predictor of incident coronary events and its ability to reevaluate risk from MESA. The prevalence and progression of CAC is different between race/ethnic categories and associated with traditional atherosclerotic factors such as an advanced age, male gender, hypertension, dyslipidemia, diabetes, smoking status, adiposities such as BMI, family history of premature CHD. The CAC score itself is a reliable independent predictor of CHD compared with other traditional coronary artery risk factors including FRS components and could improve the area under the operating curve for incident CHD after combining it with traditional risk factors. A CAC score of zero is a promising marker of very low risk of CHD. The most commonly used cutoff numbers of CAC for distinguishing the high risk population of CHD are CAC score of 1–100, 101–300 and greater than 300. Furthermore, the density of CAC obtained simultaneously with a CAC score could be a new risk predictive marker and show a promising future of risk evaluation for CHD and CVD. CAC, in MESA, has been strongly associated with the development of stroke and combined endpoints of CHD/CVD. In MESA the CAC score is able to reclassify low-to-intermediate risk groups and certain subgroups, especially women and young adults, most of whom may classify as low risk by FRS risk stratification. The clinical role of the CAC score has been solidified as a part of our 2013 cholesterol guidelines, and is now under discussion as a universally covered service by the US Preventive Services Task Force. The CAC score will likely play an increasingly important role in health care management.
Area under the ROC curve for risk factors alone and risk factors alone plus CAC
| First Author (Ref. #) | N | specific subjects | Follow-up years | event | AUC for risk factors alone | AUC for risk factors plus CAC | p value |
|---|---|---|---|---|---|---|---|
| Detrano et al (5) | 6722 | 3.9 | Major coronary event Any coronary event |
0.79 0.77 |
0.83 0.82 |
0.006 <0.001 |
|
| Polonsky et al (3) | 5931 | non diabetic | 5.8 | CHD event | 0.76 | 0.81 | <0.001 |
| Gepner et al (36) | 6779 | 9.5 | CVD event CHD event |
0.756 0.752 |
0.776 0.784 |
<0.001 <0.001 |
|
| Yeboah et al (37) | 6814 | 7.6 | CHD event CVD event |
0.623 0.627 |
0.784 0.752 |
<0.001 <0.001 |
|
| Malik et al (38) | 6603 | neither metabolic nor diabetic Metabolic diabetic |
6.4 | CHD/CVD event CHD/CVD event CHD/CVD event |
0.73 0.73 0.72 |
0.80 0.79 0.78 |
<0.001 <0.001 <0.001 |
| Criqui et al (40) | 3398 | greater than zero CAC score at baseline | 7.6 | CHD event CVD event |
0.668 0.669 |
0.696 0.688 |
0.02 0.02 |
| Yeboah et al (46) | 5185 | 10 | ASCVD event | 0.74 | 0.78 | 0.001 |
CAC; coronary artery calcification
CHD; coronary heart disease
CVD; cardiovascular disease
ASCVD; atherosclerosis cardiovascular disease
Highlights.
This article reviews the role of CAC in the assessment of coronary risk in the Multi-Ethnic Study of Atherosclerosis (MESA) which is a population based, multicenter longitudinal study of 6814 participants undergoing demographic, risk factor, and subclinical disease evaluations.
The prevalence and progression of CAC is different among the subgroups defined by race, ethnicity, age, gender, smoking status, BMI, life style, a history of hypertension, dyslipidemia, diabetes or a family history of premature CHD.
The CAC score itself is a reliable independent predictor of CHD compared with other traditional risk factors and could improve the area under the operating curve for incident CHD after combination with traditional risk factors.
A CAC score of zero is a promising marker of very low risk for CHD. In contrast, a CAC score >0 equals increased risk of atherosclerosis. The most commonly used cutoffs number of CAC for distinguishing the high risk population of CHD is CAC score 1–100, 101–300 and more over than 300.
The CAC score is useful to reclassify low-to-intermediate risk groups and certain subgroups, especially women and young adults most of whom may be classified as low risk by FRS risk stratification. The clinical role of CAC score has been solidified as a part of our 2013 cholesterol guidelines, and now under discussion as a universally covered service by the US Preventive Services Task Force. The CAC score will likely play an increasingly important role in health care management.
Acknowledgments
Matthew Budoff MD: NIH, General electric healthcare
Abbreviations
- CAC
coronary artery calcification
- CT
computed tomography
- FRS
Framingham risk score
- RRS
Reynolds risk score
- CHD
coronary heart disease
- CVD
cardiovascular disease
- ASCVD
atherosclerosis cardiovascular disease
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of interest statement
15 January 2016
Professor J. Narula, Editor-in-Chief Global Heart
Dear Professor, Narula
K.O and R.N declare that they have no conflicts of interest.
Dr. Matthew Budoff has a disclosure about supported by NIH and General electric.
Kazuhiro Osawa, MD
Los Angeles Biomedical Research Institute at Harbor, University of California-Los Angeles, Los Angeles, California.
Address: 1124 West Carson Street Torrance, CA 90502 the United States of America
Phone: +1-877-452-2674 E-mail: kosawa@labiomed.org
References
- 1.Budoff MJ, Achenbach S, Blumenthal RS, et al. Assessment of coronary artery disease by cardiac computed tomography: a scientific statement from the American Heart Association Committee on Cardiovascular Imaging and Intervention, Council on Cardiovascular Radiology and Intervention, and Committee on Cardiac Imaging, Council on Clinical Cardiology. Circulation. 2006;114:1761–1791. doi: 10.1161/CIRCULATIONAHA.106.178458. [DOI] [PubMed] [Google Scholar]
- 2.Wayhs R, Zelinger A, Raggi P. High coronary artery calcium scores pose an extremely elevated risk for hard events. J Am Coll Cardiol. 2002;39:225–230. doi: 10.1016/s0735-1097(01)01737-5. [DOI] [PubMed] [Google Scholar]
- 3.Polonsky TS, McClelland RL, Jorgensen NW, et al. Coronary artery calcium score and risk classification for coronary heart disease prediction. JAMA. 2010;303:1610–1616. doi: 10.1001/jama.2010.461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Greenland P, LaBree L, Azen SP, Doherty TM, Detrano RC. Coronary artery calcium score combined with Framingham score for risk prediction in asymptomatic individuals. JAMA. 2004;291:210–215. doi: 10.1001/jama.291.2.210. [DOI] [PubMed] [Google Scholar]
- 5.Detrano R, Guerci AD, Carr JJ, et al. Coronary calcium as a predictor of coronary events in four racial or ethnic groups. N Engl J Med. 2008;358:1336–1345. doi: 10.1056/NEJMoa072100. [DOI] [PubMed] [Google Scholar]
- 6.Bild DE, Detrano R, Peterson D, et al. Ethnic differences in coronary calcification: the Multi-Ethnic Study of Atherosclerosis (MESA) Circulation. 2005;111:1313–1320. doi: 10.1161/01.CIR.0000157730.94423.4B. [DOI] [PubMed] [Google Scholar]
- 7.McClelland RL, Chung H, Detrano R, Post W, Kronmal RA. Distribution of coronary artery calcium by race, gender, and age: results from the Multi-Ethnic Study of Atherosclerosis (MESA) Circulation. 2006;113:30–37. doi: 10.1161/CIRCULATIONAHA.105.580696. [DOI] [PubMed] [Google Scholar]
- 8.Kronmal RA, McClelland RL, Detrano R, et al. Risk factors for the progression of coronary artery calcification in asymptomatic subjects: results from the Multi-Ethnic Study of Atherosclerosis (MESA) Circulation. 2007;115:2722–2730. doi: 10.1161/CIRCULATIONAHA.106.674143. [DOI] [PubMed] [Google Scholar]
- 9.Paramsothy P, Knopp RH, Bertoni AG, et al. Association of combinations of lipid parameters with carotid intima-media thickness and coronary artery calcium in the MESA (Multi-Ethnic Study of Atherosclerosis) J Am Coll Cardiol. 2010;56:1034–1041. doi: 10.1016/j.jacc.2010.01.073. [DOI] [PubMed] [Google Scholar]
- 10.McEvoy JW, Nasir K, DeFilippis AP, et al. Relationship of cigarette smoking with inflammation and subclinical vascular disease: the Multi-Ethnic Study of Atherosclerosis. Arterioscler Thromb Vasc Biol. 2015;35:1002–1010. doi: 10.1161/ATVBAHA.114.304960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wong ND, Nelson JC, Granston T, et al. Metabolic syndrome, diabetes, and incidence and progression of coronary calcium: the Multiethnic Study of Atherosclerosis study. JACC Cardiovasc Imaging. 2012;5:358–366. doi: 10.1016/j.jcmg.2011.12.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nasir K, Budoff MJ, Wong ND, et al. Family history of premature coronary heart disease and coronary artery calcification: Multi-Ethnic Study of Atherosclerosis (MESA) Circulation. 2007;116:619–626. doi: 10.1161/CIRCULATIONAHA.107.688739. [DOI] [PubMed] [Google Scholar]
- 13.Pandey AK, Blaha MJ, Sharma K, et al. Family history of coronary heart disease and the incidence and progression of coronary artery calcification: Multi-Ethnic Study of Atherosclerosis (MESA) Atherosclerosis. 2014;232:369–376. doi: 10.1016/j.atherosclerosis.2013.11.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.DeFilippis AP, Blaha MJ, Ndumele CE, et al. The association of Framingham and Reynolds risk scores with incidence and progression of coronary artery calcification in MESA (Multi-Ethnic Study of Atherosclerosis) J Am Coll Cardiol. 2011;58:2076–2083. doi: 10.1016/j.jacc.2011.08.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ahmed HM, Blaha MJ, Nasir K, et al. Low-risk lifestyle, coronary calcium, cardiovascular events, and mortality: results from MESA. Am J Epidemiol. 2013;178:12–21. doi: 10.1093/aje/kws453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Grundy SM, Pasternak R, Greenland P, Smith S, Jr, Fuster V. Assessment of cardiovascular risk by use of multiple-risk-factor assessment equations: a statement for healthcare professionals from the American Heart Association and the American College of Cardiology. Circulation. 1999;100:1481–1492. doi: 10.1161/01.cir.100.13.1481. [DOI] [PubMed] [Google Scholar]
- 17.Cook NR, Paynter NP, Eaton CB, et al. Comparison of the Framingham and Reynolds Risk scores for global cardiovascular risk prediction in the multiethnic Women’s Health Initiative. Circulation. 2012;125:1748–1756. S1741–1711. doi: 10.1161/CIRCULATIONAHA.111.075929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.DeFilippis AP, Young R, Carrubba CJ, et al. An analysis of calibration and discrimination among multiple cardiovascular risk scores in a modern multiethnic cohort. Ann Intern Med. 2015;162:266–275. doi: 10.7326/M14-1281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Akosah KO, Schaper A, Cogbill C, Schoenfeld P. Preventing myocardial infarction in the young adult in the first place: how do the National Cholesterol Education Panel III guidelines perform? J Am Coll Cardiol. 2003;41:1475–1479. doi: 10.1016/s0735-1097(03)00187-6. [DOI] [PubMed] [Google Scholar]
- 20.Michos ED, Nasir K, Braunstein JB, et al. Framingham risk equation underestimates subclinical atherosclerosis risk in asymptomatic women. Atherosclerosis. 2006;184:201–206. doi: 10.1016/j.atherosclerosis.2005.04.004. [DOI] [PubMed] [Google Scholar]
- 21.Berry JD, Lloyd-Jones DM, Garside DB, Greenland P. Framingham risk score and prediction of coronary heart disease death in young men. Am Heart J. 2007;154:80–86. doi: 10.1016/j.ahj.2007.03.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Budoff MJ, McClelland RL, Nasir K, et al. Cardiovascular events with absent or minimal coronary calcification: the Multi-Ethnic Study of Atherosclerosis (MESA) Am Heart J. 2009;158:554–561. doi: 10.1016/j.ahj.2009.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Blaha MJ, Cainzos-Achirica M, Greenland P, et al. Role of Coronary Artery Calcium Score of Zero and Other Negative Risk Markers for Cardiovascular Disease: The Multi-Ethnic Study of Atherosclerosis (MESA) Circulation. 2016;133:849–858. doi: 10.1161/CIRCULATIONAHA.115.018524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Whelton SP, Silverman MG, McEvoy JW, et al. Predictors of Long-Term Healthy Arterial Aging: Coronary Artery Calcium Nondevelopment in the MESA Study. JACC Cardiovasc Imaging. 2015;8:1393–1400. doi: 10.1016/j.jcmg.2015.06.019. [DOI] [PubMed] [Google Scholar]
- 25.Budoff MJ, Young R, Lopez VA, et al. Progression of coronary calcium and incident coronary heart disease events: MESA (Multi-Ethnic Study of Atherosclerosis) J Am Coll Cardiol. 2013;61:1231–1239. doi: 10.1016/j.jacc.2012.12.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Silverman MG, Blaha MJ, Krumholz HM, et al. Impact of coronary artery calcium on coronary heart disease events in individuals at the extremes of traditional risk factor burden: the Multi-Ethnic Study of Atherosclerosis. Eur Heart J. 2014;35:2232–2241. doi: 10.1093/eurheartj/eht508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rosen BD, Fernandes V, McClelland RL, et al. Relationship between baseline coronary calcium score and demonstration of coronary artery stenoses during follow-up MESA (Multi-Ethnic Study of Atherosclerosis) JACC Cardiovasc Imaging. 2009;2:1175–1183. doi: 10.1016/j.jcmg.2009.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Silverman MG, Harkness JR, Blankstein R, et al. Baseline subclinical atherosclerosis burden and distribution are associated with frequency and mode of future coronary revascularization: multi-ethnic study of atherosclerosis. JACC Cardiovasc Imaging. 2014;7:476–486. doi: 10.1016/j.jcmg.2014.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Blaha MJ, Budoff MJ, DeFilippis AP, et al. Associations between C-reactive protein, coronary artery calcium, and cardiovascular events: implications for the JUPITER population from MESA, a population-based cohort study. Lancet. 2011;378:684–692. doi: 10.1016/S0140-6736(11)60784-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Budoff MJ, Nasir K, McClelland RL, et al. Coronary calcium predicts events better with absolute calcium scores than age-sex-race/ethnicity percentiles: MESA (Multi-Ethnic Study of Atherosclerosis) J Am Coll Cardiol. 2009;53:345–352. doi: 10.1016/j.jacc.2008.07.072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lee KB, Budoff MJ, Zavodni A, et al. Coronary artery calcium is associated with degree of stenosis and surface irregularity of carotid artery. Atherosclerosis. 2012;223:160–165. doi: 10.1016/j.atherosclerosis.2012.05.012. [DOI] [PubMed] [Google Scholar]
- 32.Gibson AO, Blaha MJ, Arnan MK, et al. Coronary artery calcium and incident cerebrovascular events in an asymptomatic cohort. JACC Cardiovasc Imaging. 2014;7:1108–1115. doi: 10.1016/j.jcmg.2014.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lakoski SG, Greenland P, Wong ND, et al. Coronary artery calcium scores and risk for cardiovascular events in women classified as “low risk” based on Framingham risk score: the multi-ethnic study of atherosclerosis (MESA) Arch Intern Med. 2007;167:2437–2442. doi: 10.1001/archinte.167.22.2437. [DOI] [PubMed] [Google Scholar]
- 34.Pletcher MJ, Sibley CT, Pignone M, Vittinghoff E, Greenland P. Interpretation of the coronary artery calcium score in combination with conventional cardiovascular risk factors: the Multi-Ethnic Study of Atherosclerosis (MESA) Circulation. 2013;128:1076–1084. doi: 10.1161/CIRCULATIONAHA.113.002598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Folsom AR, Kronmal RA, Detrano RC, et al. Coronary artery calcification compared with carotid intima-media thickness in the prediction of cardiovascular disease incidence: the Multi-Ethnic Study of Atherosclerosis (MESA) Arch Intern Med. 2008;168:1333–1339. doi: 10.1001/archinte.168.12.1333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gepner AD, Young R, Delaney JA, et al. Comparison of coronary artery calcium presence, carotid plaque presence, and carotid intima-media thickness for cardiovascular disease prediction in the Multi-Ethnic Study of Atherosclerosis. Circ Cardiovasc Imaging. 2015;8 doi: 10.1161/CIRCIMAGING.114.002262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yeboah J, McClelland RL, Polonsky TS, et al. Comparison of novel risk markers for improvement in cardiovascular risk assessment in intermediate-risk individuals. JAMA. 2012;308:788–795. doi: 10.1001/jama.2012.9624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Malik S, Budoff MJ, Katz R, et al. Impact of subclinical atherosclerosis on cardiovascular disease events in individuals with metabolic syndrome and diabetes: the multi-ethnic study of atherosclerosis. Diabetes Care. 2011;34:2285–2290. doi: 10.2337/dc11-0816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Martin SS, Blaha MJ, Blankstein R, et al. Dyslipidemia, coronary artery calcium, and incident atherosclerotic cardiovascular disease: implications for statin therapy from the multi-ethnic study of atherosclerosis. Circulation. 2014;129:77–86. doi: 10.1161/CIRCULATIONAHA.113.003625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Criqui MH, Denenberg JO, Ix JH, et al. Calcium density of coronary artery plaque and risk of incident cardiovascular events. JAMA. 2014;311:271–278. doi: 10.1001/jama.2013.282535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Goff DC, Jr, Lloyd-Jones DM, Bennett G, et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63:2935–2959. doi: 10.1016/j.jacc.2013.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Stone NJ, Robinson JG, Lichtenstein AH, et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63:2889–2934. doi: 10.1016/j.jacc.2013.11.002. [DOI] [PubMed] [Google Scholar]
- 43.Kavousi M, Leening MJ, Nanchen D, et al. Comparison of application of the ACC/AHA guidelines, Adult Treatment Panel III guidelines, and European Society of Cardiology guidelines for cardiovascular disease prevention in a European cohort. JAMA. 2014;311:1416–1423. doi: 10.1001/jama.2014.2632. [DOI] [PubMed] [Google Scholar]
- 44.Nasir K, Bittencourt MS, Blaha MJ, et al. Implications of Coronary Artery Calcium Testing Among Statin Candidates According to American College of Cardiology/American Heart Association Cholesterol Management Guidelines: MESA (Multi-Ethnic Study of Atherosclerosis) J Am Coll Cardiol. 2015;66:1657–1668. doi: 10.1016/j.jacc.2015.07.066. [DOI] [PubMed] [Google Scholar]
- 45.Yeboah J, Polonsky TS, Young R, et al. Utility of Nontraditional Risk Markers in Individuals Ineligible for Statin Therapy According to the 2013 American College of Cardiology/American Heart Association Cholesterol Guidelines. Circulation. 2015;132:916–922. doi: 10.1161/CIRCULATIONAHA.115.016846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Yeboah J, Young R, McClelland RL, et al. Utility of Nontraditional Risk Markers in Atherosclerotic Cardiovascular Disease Risk Assessment. J Am Coll Cardiol. 2016;67:139–147. doi: 10.1016/j.jacc.2015.10.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kim J, McEvoy JW, Nasir K, et al. Critical review of high-sensitivity C-reactive protein and coronary artery calcium for the guidance of statin allocation: head-to-head comparison of the JUPITER and St. Francis Heart Trials. Circ Cardiovasc Qual Outcomes. 2014;7:315–322. doi: 10.1161/CIRCOUTCOMES.113.000519. [DOI] [PubMed] [Google Scholar]


