Abstract
Background
Social anxiety disorder (SAD) and depression are common among adolescents, frequently comorbid, and resistant to change. Prevention programs for adolescent SAD are scant, and depression prevention programs do not fully address peer-risk factors. One critical peer-risk factor for SAD and depression is peer victimization. We describe the development and initial evaluation of a transdiagnostic school-based preventive intervention for adolescents with elevated symptoms of social anxiety and/or depression and elevated peer victimization. We modified Interpersonal Psychotherapy-Adolescent Skills Training for depression, incorporating strategies for dealing with social anxiety and peer victimization.
Objective
Our open trial assessed the feasibility, acceptability, and preliminary benefit of the modified program (called UTalk) for adolescents at risk for SAD or depression and who also reported peer victimization.
Method
Adolescents (N=14; 13–18 years; 79% girls; 86% Hispanic) were recruited and completed measures of peer victimization, social anxiety, and depression both pre- and post-intervention and provided ratings of treatment satisfaction. Independent evaluators (IEs) rated youths’ clinical severity. The intervention (3 individual and 10 group sessions) was conducted weekly during school.
Results
Regarding feasibility, 86% of the adolescents completed the intervention (M attendance=11.58 sessions). Satisfaction ratings were uniformly positive. Intention-to-treat analyses revealed significant declines in adolescent- and IE-rated social anxiety and depression and in reports of peer victimization. Additional secondary benefits were observed.
Conclusions
Although further evaluation is needed, the UTalk intervention appears feasible to administer in schools, with high satisfaction and preliminary benefit. Implications for research on the prevention of adolescent SAD and depression are discussed.
Keywords: Prevention, Social Anxiety, Depression, Peer Victimization, Adolescents
Social anxiety disorder (SAD) and depression are prevalent among adolescents and often comorbid (Beesdo et al., 2007; Costello, Egger, Copeland, Erkanli, & Angold, 2011; Garber & Weersing, 2010; Stein et al., 2001). Rates of SAD and depression increase across the adolescent years (Costello, Mustillo, Erkanli, Keeler, & Angold, 2003) and are associated with significant impairment (Birmaher et al., 1996; Grant et al., 2005). Moreover, when SAD and depression co-occur, adolescent SAD is associated with a more severe and chronic course of depression than is adult-onset SAD (Dalrymple & Zimmerman, 2011). Despite such alarming findings, only about 20% of youth with anxiety or depressive disorders receive treatment and most treatments are not evidence-based (Kataoka, Zhang, & Wells, 2002; Merikangas et al., 2010).
These findings suggest that a transdiagnostic approach to the prevention of adolescent SAD and depression may be useful. In particular, it may be valuable to develop an accessible, preventive intervention for adolescents with sub-threshold levels of social anxiety or depression to reduce the onset and course of serious emotional disorder in this age group. Accordingly, this paper describes the development of a transdiagnostic approach to the prevention of adolescent SAD and depression, and presents findings from an open trial of the intervention’s feasibility and preliminary benefit.
Prevention of Social Anxiety and Depression
To our knowledge, there are no evidence-based (EB) preventive interventions for adolescent SAD. To date, the bulk of prevention research has universally targeted a broad array of anxiety symptoms in children and early adolescents (e.g., the FRIENDS Program; Barrett, Farrell, Ollendick, & Dadds, 2006; Essau, Conradt, Sasagawa, & Ollendick, 2012), with meta-analytic findings supporting only modest improvements in anxiety-specific symptoms following universal prevention at post-test and follow-up (Ahlen, Lenhard, & Ghaderi, 2015). In contrast, social anxiety-specific research has focused almost exclusively on treating clinical levels of SAD using behavioral and cognitive-behavioral treatment models (e.g., Beidel, Turner, & Morris, 2000; Masia Warner et al., 2005), including treatment studies conducted within school settings (Masia Warner, Colognori, Brice, & Sanchez, 2015). We could find only one study that focused on the prevention of social anxiety in children and early adolescents (ages 11 to 14 years; Aune & Stiles, 2009), and none that addressed SAD prevention among older adolescents (ages 14 to 18 years), our target age group of interest.
EB prevention programs are available for adolescent depression (see Stice et al., 2009 for a review), and primarily have been based on either cognitive-behavioral (CB) approaches (e.g., Coping with Stress; Clarke et al., 1995; Garber et al., 2009), or interpersonal models of psychotherapy (e.g., Young, Mufson, & Davies, 2006; Mufson, Dorta, Moreau, & Weissman, 2004a). However, evidence indicates that these programs are much less effective for adolescents with co-occurring social anxiety (Young, Mufson, & Gallop, 2010). As such, there is a critical need for preventive interventions that address both social anxiety and depressive affect in adolescents, consistent with the perspective of multiple investigators who have emphasized the need for preventing anxiety and depression jointly (e.g., Dozois, Seeds, & Collins, 2009; Weems et al., 2015).
In developing an integrated, transdiagnostic approach to prevention, we targeted adolescents with subclinical levels of social anxiety or depression, as meta-analytic reviews reveal that indicated preventive interventions for adolescent depression are more effective than universal ones (e.g., Stice et al., 2009). Further, we took a selective approach to prevention by also focusing on adolescents who displayed a peer-risk factor for depression, namely that of being victimized by peers. This feature represents a novel contribution to the depression prevention literature in that existing programs often have selected adolescents because of family-risk factors for depression (e.g., parental depression; Garber et al., 2009) but not, as yet, for peer-risk factors. Below we describe the conceptual framework for our integrated preventive intervention as well as the literature on peer victimization as a peer-risk factor for adolescent social anxiety and depression.
Conceptual Framework: Interpersonal Relations As A Pathway for SAD and Depression
Conceptually and empirically, interpersonal difficulties represent a shared pathway in the development of social anxiety and depression in adolescents (La Greca & Lai, 2014; Mufson, La Greca, Young, Ehrenreich-May, 2015). For example, interpersonal stressors are associated with depressive symptoms in adolescents (Blechman et al. 1986; La Greca & Landoll, 2011; La Greca & Lai, 2014; Rudolph et al. 2000), especially for girls (Hankin, 2009), and these associations appear to be reciprocal (McLaughlin et al., 2009; Rudolph et al. 2000). Similarly, interpersonal problems characterize adolescents with high social anxiety, as they have fewer friendships, more negative peer interactions, poorer social skills, and greater conflict avoidance than non-anxious youth (Davila & Beck, 2002; Ginsburg et al., 1998; La Greca & Landoll, 2011; La Greca & Lopez, 1998; Storch & Masia Warner, 2004; Vernberg et al., 1992). The interpersonal difficulties of youth who report high levels of socially anxiety or depression make them vulnerable to negative peer interactions, which can further exacerbate symptoms of social anxiety and depression (McLaughlin et al., 2009; Siegel, La Greca, & Harrison, 2009; Storch et al., 2005).
Thus, in the present study, we used an interpersonal model as the conceptual framework for our preventive intervention. Specifically, we modified Interpersonal Psychotherapy-Adolescent Skills Training (IPT-AST), an indicated school-based preventive intervention for depression in adolescents (13 – 17 years) (Young et al., 2006; Young et al., 2010). IPT-AST is based on Interpersonal Psychotherapy for Adolescents (Mufson et al., 2004a), an EB treatment for adolescent depression (Mufson, Gallagher, Dorta, & Young, 2004b, Mufson et al., 2004c).
IPT-AST emphasizes psychoeducation about depression, identifying connections between interpersonal events and depressive feelings, dealing with interpersonal conflict and change, interpersonal skill building, and enhancing social support (Young & Mufson, 2012). CB programs for depression prevention (e.g., Clarke et al., 1995) also may include attention to social skills, although interpersonal functioning is not the primary focus of intervention. Further, interventions based on CB models often focus on changing cognitions as a first step whereas interpersonal models focus on emotions and interpersonal behavior that may culminate in a change in cognitions, but that is the end point, rather than the starting point. (See Sburlati, Lyneham, Mufson & Schneiring, 2012, for further discussion interpersonal and CB differences.)
We modified IPT-AST to address adolescent SAD by including psychoeducation and exposures relevant to social anxiety (i.e., approaching other peers, conversing with others), as these treatment elements have been widely used for anxiety disorders in youth (e.g., Beidel et al., 2000; Ehrenreich-May et al., in press; Kendall, Furr, & Podell, 2010). We also extended the key interpersonal areas of IPT-AST (i.e., interpersonal conflict, interpersonal role change, and interpersonal skills) to include “interpersonal role insecurity,” which was formulated for treating adults with social anxiety (e.g., Lipsitz et al., 2008). Role insecurity refers to the idea that adolescents with clinically significant anxiety are uncertain of where they fit in with peers and with their changing relationships with parents; these role insecurities can lead to social isolation and social avoidance. IPT-AST was modified to target this uncertainty and avoidance through the practice of graduated approach behaviors with peers and through exposure practice in the group sessions.
Peer Victimization as a Peer-Risk Factor for Adolescent SAD and Depression
Peer victimization (i.e., being the target/recipient of peers’ aggressive behaviors) represents a common vulnerability factor for symptoms of both SAD and depression in adolescents (De Los Reyes & Prinstein, 2004; La Greca & Harrison, 2005; McLaughlin et al., 2009; Siegel et al., 2009). Although peer victimization (PV) can be overt/physical (e.g., being the target of verbal threats of harm, physical attacks), the most common types of PV are relational (e.g., being rejected or socially excluded) and reputational (e.g., being the target of rumors or efforts to have one’s reputation damaged) (De Los Reyes & Prinstein, 2004; Siegel et al., 2009). We refer to relational and reputational PV as interpersonal forms of PV (or IPV) given their focus on undermining adolescents’ interpersonal relationships.
PV is relatively common, as about 20% to 30% of adolescents report being the recipients of peers’ aggressive behaviors more than once or twice (Dinkes, Cataldi, & Lin-Kelly, 2007). Rates are especially high for IPV (La Greca & Harrison, 2005; Storch, Brassard, & Masia-Warner, 2003), which often goes undetected by others. Further, IPV can occur in the context of technology, such as through texting and social networking sites, and can intensify emotional distress (Cook, Williams, Guerra, Kim, & Sadek, 2010; Landoll, La Greca, Lai, Chan, & Herge, 2015; Lenhart, Purcell, Smith, & Zickuhr, 2010; Williams & Guerra, 2007).
In developing a transdiagnostic preventive intervention for adolescent SAD and depression, we focused on IPV as a shared peer-risk factor for several reasons. First, studies reveal that adolescents with elevated symptoms of both social anxiety and depression have the highest levels of IPV compared with other teens (e.g., Ranta et al., 2009). Second, prospective studies indicate that IPV contributes to significant increases in adolescents’ symptoms of social anxiety and depression over time (e.g., McLaughlin et al., 2009; Siegel et al. 2009; Storch et al., 2005), and that adolescents with internalizing problems, especially those with elevated social anxiety and depression, are more likely targets of IPV (Blote, Miers, Heyne, & Westenberg, 2015). Third, existing school-based interventions for reducing bullying and PV focus mainly on overt peer victimization (e.g., Kärnä et al., 2011; Olweus, 1993), even though high-school-aged youth report high levels of IPV, which are subtle, hard to detect, and rarely reported to adults.
In summary, IPV appears to be a peer-risk factor for significant symptoms of social anxiety and depression, and is an important peer-risk factor to target for adolescents who may already be on a path to clinical disorder. Thus, we focused our preventive intervention on adolescents who reported elevated levels of IPV, and modified the IPT-AST protocol accordingly. Specifically, we incorporated examples of and strategies for dealing with IPV, based on findings from previous research (e.g., De Los Reyes & Prinstein, 2004; La Greca & Harrison, 2005; Siegel et al., 2009). Strategies included psychoeducation about the problem of IPV, disclosing IPV events to adults or friends, problem-solving for ways to deal with uncomfortable or distressing peer interactions when they occur, and knowing the school procedures for bullying and how to seek help if a serious event arises.
Open Trial of the UTalk Version of IPT-AST
We developed the UTalk version of IPT-AST for high-school aged adolescents (14 to 18 years) with elevated symptoms of social anxiety or depression and who also reported elevated levels of IPV. We then tested the intervention in an open trial to determine its feasibility, acceptability, and preliminary benefit. We focused on ethnically-diverse adolescents (predominantly Hispanic) who are less likely to receive mental health services than non-minority youth (Hough, Hazen, & Soriano, 2002: Kataoka et al., 2002). Others have used IPT-AST successfully with adolescents from Hispanic backgrounds (e.g., Young et al., 2006).
We hypothesized that the UTalk intervention would be feasible to conduct with adolescents within the context of the school setting with satisfactory program attendance and program completion. We also hypothesized that the intervention would be acceptable to adolescents as evidenced by positive ratings of treatment satisfaction. In terms of benefit, we hypothesized that youth participating in the intervention would display significant pre- to post-intervention declines in symptoms of social anxiety and depression and in interpersonal peer victimization. Finally, we evaluated intervention-related changes in secondary outcomes and monitored additional variables to evaluate whether any adverse outcomes were apparent.
Method
Participants and Design
Our open trial used a prospective pre-to-post intervention design; all participants received the intervention. To provide a benchmark for functioning pre- and post-intervention, we compared participants’ scores on multiple measures to those obtained from a large community sample of adolescents of high-school age (Herge, La Greca, & Chan, 2016).
Participants were 14 adolescents (78.6% girls), aged 14 to 18 years (M = 15.64, SD = 1.28), who attended the 9th, 10th, or 11th grade in the Southeastern United States (see Table 1). Most (85.7%) were from Hispanic ethnic/cultural backgrounds, similar to the ethnic composition of the broader school district (92.2% Hispanic; exact racial composition not available) (Miami-Dade County Public Schools, 2013). All participants were English-speaking, although 71.4% reported first speaking a language other than English as a child. Specific information was not available on socioeconomic status, although participants attended schools with moderate (48%) to high (75%) levels of eligibility free or reduced price lunch (Miami-Dade County Public Schools, 2013) and likely represented the broad range of middle class backgrounds (low to high).
Table 1.
Participant Demographic and Clinical Characteristics (n = 14)
| Characteristic | Mean (SD) or Frequency (%) |
|---|---|
| Female gender | 11 (78.5%) |
| Age in years | 15.64 (1.28) |
| Grade | |
| 9 | 5 (35.7%) |
| 10 | 2 (14.3%) |
| 11 | 7 (50.0%) |
| Ethnicity | |
| Hispanic | 12 (85.7%) |
| Non-Hispanic White | 1 (7.1%) |
| Non-Hispanic Black | 1 (7.1%) |
| Race | |
| White | 8 (57.1%) |
| Black | 1 (7.1%) |
| Mixed | 5 (35.7%) |
| Screening (Inclusion Criteria) | |
| Social Anxiety (SAS-A) | 52.86 (8.48)* |
| Depression (CES-D) | 20.21 (7.31)* |
| Relational PV (R-PEQ) | 2.55 (0.69)* |
| Reputational PV (R-PEQ) | 2.19 (1.06)* |
| Screening (Exclusion Criteria) | |
| Overt PV (R-PEQ) | 1.31 (0.36) |
| Aggression (YSR) | 9.50 (2.28) |
| Baseline Subclinical Diagnoses on ADIS-C | |
| Social Anxiety | 10 (71%) |
| Major Depression/Dysthymia | 0 (0%) |
Note: CES-D = Center for Epidemiological Studies Depression Scale; SAS-A = Social Anxiety Scale for Adolescents; R-PEQ = Revised Peer Experiences Questionnaire; YSR = Youth Self Report; ADIS-C = Anxiety Disorders Interview Schedule for DSM-IV – Child Version
Significantly elevated compared to a community sample (Herge et al., 2016), p < .05
Procedures
Prior to study initiation, approvals were obtained from the relevant University Internal Review Boards and the participating school district’s research office. Written informed parental consent (in English and Spanish) and written adolescent assent were required for adolescents’ participation in both the screening and the open trial, as described below.
Screening Phase
Adolescents were recruited from two public high schools in November 2012. During recruitment, school flyers were circulated announcing the “UTalk” program, which was described as a program to improve teens’ peer relationships and social life. Research staff also met with teachers and students to describe the UTalk program and the nature of the study, and to circulate parent letters and consent forms to 9th, 10th, or 11th graders who might be interested in participating. Across the two schools, 108 adolescents (M age = 15.45, SD = 1.02; 69.4% girls; 90.7% Hispanic ethnicity) expressed interest in UTalk (i.e., self-selected) and returned parental consent forms; all 108 participated in screening to determine eligibility. No compensation was offered for adolescents who participated in screening.
Adolescents met initial eligibility criteria for eventual participation in UTalk if they reported: a) elevated levels of symptoms of social anxiety or depression, and b) elevated levels of relational or reputational peer victimization (i.e., IPV) on screening measures. As described below, adolescents were excluded if they reported elevated levels of: a) aggressive behavior (to avoid the inclusion of bullies in the intervention groups) or b) overt victimization (to ensure that those who were being physically attacked or threatened would receive immediate help from the school, consistent with school policies for bullying).
Screening occurred December–January, in small groups at the schools. Adolescents completed measures assessing symptoms of social anxiety (Social Anxiety Scale for Adolescents [SAS-A]; La Greca & Lopez, 1998); depression (Center for Epidemiological Studies Depression Scale [CES-D]; Radloff, 1977); peer victimization (overt, relational, reputational; Revised Peer Experiences Questionnaire [R-PEQ]; De Los Reyes & Prinstein, 2004); and aggression (Aggressive Behavior subscale of the Youth Self Report [YSR]; Achenbach & Rescorla, 2001).
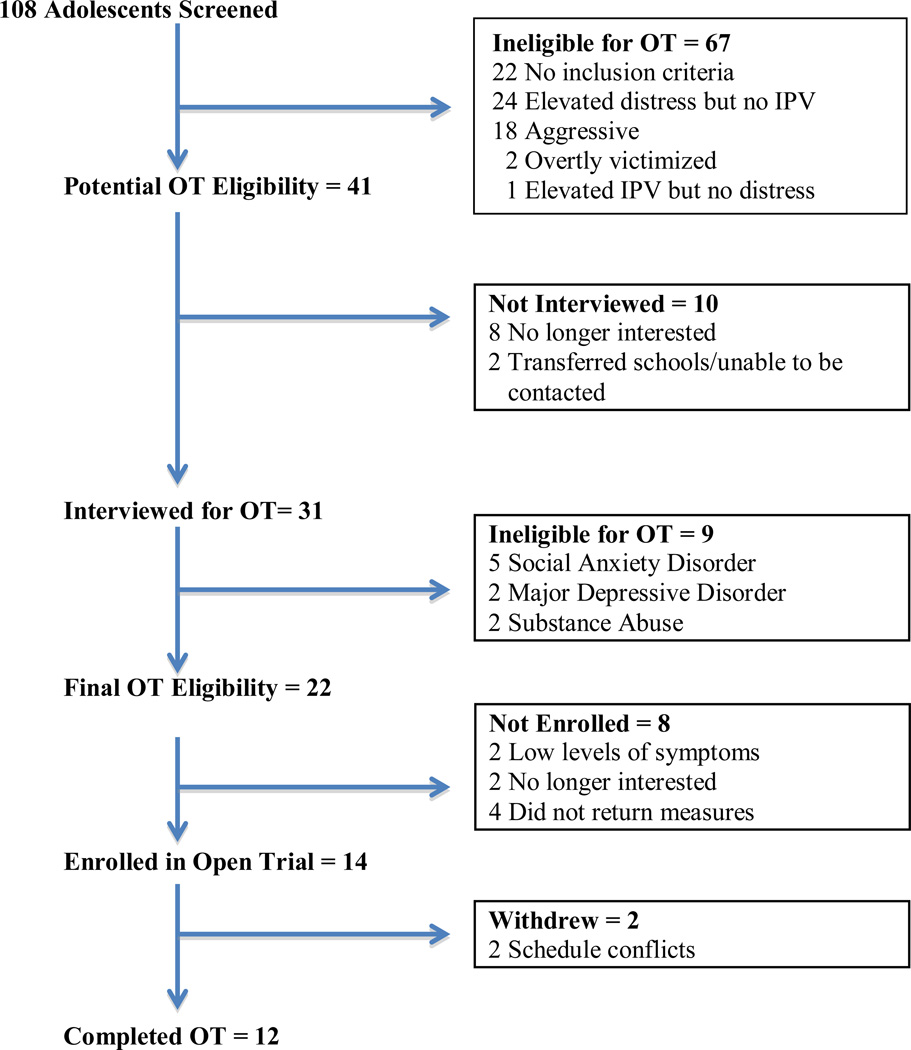
Adolescents met initial screening criteria if their scores were above clinical cutoffs on the SAS-A or CES-D, and also above cutoffs for “being victimized” on the relational or reputational PV subscales of the R-PEQ. Adolescents were excluded after screening if they reported high levels of aggressive behavior on the YSR, or reported being physically victimized on the overt PV subscale of the R-PEQ. In such cases, school counselors were contacted to follow-up with the adolescents. In total, 67 adolescents were ineligible after screening. (See Figure 1 for flow chart.) Of these, 22 (33%) did not meet any of the inclusion criteria, 24 (36%) reported elevated social anxiety or depressive symptoms but did not elevated IPV, 18 (27%) reported high levels of aggressive behavior, 2 (3%) reported elevated levels of overt PV, and 1 reported elevated relational PV but no elevated symptoms of social anxiety or depression. In cases where the adolescents reported elevated symptoms of social anxiety or depression, but not elevated IPV, parents were contacted and provided with clinical referral information for their adolescent.
Figure 1.
Flow Chart Of Participants Through Screening And Open Trial (OT)
All remaining adolescents (n = 41; 38% of those screened) were potentially eligible for the open trial and invited to participate in the baseline evaluation to further assess eligibility (see the next section). The baseline evaluation (mid-January to early-February) occurred immediately after the completion of screening, and was followed by the intervention (mid-February through May). Eligible adolescents did not differ from those ineligible after screening in their demographic or school characteristics. However, on our selection measures, eligible youth reported significantly higher levels of social anxiety (SAS-A M = 53.79 vs. 46.10) and relational and reputational PV (R-PEQ M = 2.73 vs. 1.91, and 2.24 vs. 1.75, respectively; all p’s < .007) compared to ineligible youth. Eligible youth also had higher scores on depressive symptoms (CES-D M = 23.53 vs. 19.98), but this difference was not significant. Of further note, on average, the 108 adolescents who participated in the screening were already significantly more distressed and victimized than adolescents in a community sample (Herge et al., 2016). Compared to community youth, screened adolescents reported higher levels of social anxiety (SAS-A M = 48.93 vs. 37.65), depressive symptoms (CES-D M = 21.32 vs. 13.77), and relational (M = 2.21 vs. 1.63) and reputational PV (M = 1.93 vs. 1.51) on the R-PEQ (all p’s < .001).
Open Trial
Prior to participation in the baseline assessment, written parental informed consent and adolescent assent were obtained for the open trial. Of the 41 adolescents eligible after screening, 31 (76%) consented to be in the open trial and participated in a baseline interview; the others were no longer interested (n = 8) or could not be contacted (n = 2) at the time of enrollment. (See Figure 1.) All participating adolescents received a $25 gift card for completing each of the baseline and post-intervention assessments.
Because this was a prevention trial, at baseline, adolescents participated in a diagnostic interview to rule out the presence of a relevant clinical disorder (i.e., social anxiety disorder, mood or depressive disorder) and/or suicidal risk, which were exclusion criteria for the open trial. Trained independent evaluators (clinical psychology graduate students) administered the Anxiety Disorders Interview Schedule for DSM-IV–Child Version (ADIS-C; Silverman & Albano, 1996) and the Columbia-Suicide Severity Rating Scale (C-SSRS; Posner et al. 2009) for this purpose. (See Measures for details.) After the interview, 9 of the 31 adolescents (29%) were excluded: 5 met criteria for Social Anxiety Disorder, 2 met criteria for Major Depressive Disorder, and 2 met criteria for Substance Abuse. (See Figure 1.) These adolescents’ parents were notified and provided with clinical referral information. The remaining 22 adolescents were eligible for the open trial, and 14 were enrolled (7 at each school). Those not enrolled had very low levels of symptoms during the diagnostic interview (n = 2), were no longer interested in the intervention (n = 2), or did not return study measures (n = 4).
Intervention
UTalk is a group-based preventive intervention based on Interpersonal Psychotherapy – Adolescent Skills Training (IPT-AST; Young & Mufson, 2012) for adolescent depression that was modified and expanded to address social anxiety symptoms and focus on peer relationship issues1. UTalk educates adolescents about the link between their mood, social anxiety, and interpersonal events happening in their lives. It then provides adolescents with communication strategies and interpersonal problem-solving skills to improve their social relationships. The UTalk intervention (February to May) consisted of 3 individual sessions (2 pre-group and 1 mid-intervention; each about 45 minutes), and 10 weekly group sessions (each about 90 minutes) with two group leaders (either postdoctoral or advanced graduate trainees in clinical psychology) who were trained by one of the authors (L.M.). We conducted one group (with 7 adolescents) at each of the two participating high schools.
As a preventive intervention, the UTalk version of IPT-AST is novel in that it addresses ways for adolescents to manage their feelings of both social anxiety and depression and also ways to enhance their friendships and other peer relationships (the predominant focus of the group sessions). This is in contrast to the IPT-AST program (Young & Mufson, 2010), and other depression prevention programs (e.g., Clarke et al., 1995; Garber et al., 2009) that focus on mainly on depressive affect and adolescents’ relationships with parents and other adults in addition to peers. The UTalk intervention also differs from cognitive-behavioral (CB) treatments for adolescent social anxiety, such as Skills for Academic and Social Success (SASS; Masia Warner et al., 2015), in that it emphasizes different interpersonal skills (e.g., more emphasis in UTalk on communication and conflict resolution; more emphasis in SASS on initiating and maintaining conversations, listening and remembering, and assertiveness). Further, consistent with IPT-AST but unlike many CB interventions (Stice et al., 2009), homework assignments are not a routine part of UTalk, although assignments to practice communication skills or peer-approach behaviors occasionally were made during the “middle phase” of the intervention.
Specifically, initial individual sessions involved learning about the adolescents’ key relationships with peers, educating them about four interpersonal problem areas (role disputes, role transitions, interpersonal deficits, and role insecurity), and developing intervention goals. The initial three group sessions included: a) psychoeducation (for depression, social anxiety, friendships, and peer victimization), b) didactics on communication strategies, and c) hypothetical role-plays to practice communication skills.
The next five group sessions (“middle phase”) consisted of didactics on communication skills and problem-solving skills, the use of communication analysis to identify problematic communication patterns, and discussing adolescents’ real-life social scenarios, where they role-played and practiced interpersonal skills inside and outside the group. There were six specific communication strategies (e.g., using “I feel” statements, putting yourself in the other person’s shoes, etc.), uniquely developed as part of IPT-AST (Young & Mufson, 2012) and included in the UTalk adaptation, that are not typically part of other social skills or social anxiety interventions. Session topics also included skills in developing friendships (e.g., approaching other peers, sharing activities), obtaining support from trusted adults, and strategies for coping with peer victimization (e.g., positive ways of confronting others, telling a trusted adult or friend). Interpersonal events that occurred in the adolescents’ lives in the prior week determined the group content that was used to illustrate the impact of relationships on mood and feelings and to provide opportunities to practice communication, problem-solving skills, and social approach behaviors. Attention also was paid to managing adolescents’ threat perceptions (and avoiding self-blame) in the context of interpersonal interactions; these strategies were intended to improve adolescents’ overall social skills and social engagement. Adolescents often discussed family difficulties in regard to lack of support for or conflict surrounding peer activities; sessions were used to problem-solve how to negotiate with parents regarding engagement in peer activities or to gain parental support for peer difficulties. During these “middle” group sessions, adolescents occasionally were asked to practice the communication or approach behaviors they learned in the group session with others during the week (i.e., a “homework-like” request).
The last two group sessions (“termination phase”) focused on reviewing progress and the skills learned and how these skills could generalize to different situations, discussing barriers to implementing the interpersonal skills, identifying when help may be needed, and celebrating adolescents’ successes. In addition, an individual mid-group session with one of the group leaders allowed for discussion of each adolescent’s progress and individualized practice of interpersonal skills using role-plays.
To ensure treatment integrity, a detailed intervention manual was used and weekly supervision meetings were held with clinical experts (X.X. and X.X.X.), who reviewed audiotapes of each session, gave feedback on the session, and helped the group leaders plan the next session. After each session, group leaders completed an adherence checklist regarding their use of the key IPT-AST elements prescribed in the UTalk manual.
Measures
As noted above and below, adolescents completed several measures at screening, and again at baseline (January) and post-intervention (May). At baseline and post-intervention, independent evaluators (IEs) provided ratings for clinical severity using the ADIS-C and the Clinical Global Impressions Scale. Primary outcomes were the IEs’ ratings of clinical severity and adolescents’ reports of relational and reputational PV. Secondary outcomes were adolescents’ reports of social anxiety, depressive symptoms, and peer support. Measures of overt and cyber PV, family support, and peer aggression evaluated the intervention’s generalizability and potential adverse outcomes. Finally, the feasibility of the intervention was assessed by attendance, and acceptability was assessed with a questionnaire regarding program satisfaction.
Adolescent Measures
Peer victimization and peer aggression were assessed with the Revised Peer-Experiences Questionnaire (R-PEQ; De Los Reyes & Prinstein, 2004). Nine items assess the frequency of relational, reputational, and overt PV (3 items per subscale); nine parallel items assess relational, reputational, and overt peer aggression (PA). Items are rated on a 5-point scale (1 = Never, 5 = A few times a week) and averaged for each PV or PA type. The R-PEQ has excellent reliability and validity with multicultural samples of adolescents (De Los Reyes & Prinstein, 2004; Siegel et al., 2009). The PV subscales were administered at screening; both the PV and PA subscales were administered at baseline and post-intervention. Mean scores on relational or reputational PV above 2 (i.e., on average, more than “once or twice”) at screening were required for enrollment in the open trial; also, mean scores greater than 2 on overt PV was an exclusionary criteria. We selected these cutoffs because definitions of victimization and bullying typically refer to events that happen repeatedly, meaning mean more than just once or twice (Solberg & Olweus, 2003; Salmivalli, Sainio, & Hodges, 2013). At screening, internal consistencies for PV were .77 (relational), .85 (reputational), and .75 (overt); for PA they were .68 (relational), .85 (reputational), and .86 (overt).
Social anxiety was assessed with the Social Anxiety Scale for Adolescents (SAS-A; La Greca & Lopez, 1998). Its 18 items assess adolescents’ symptoms of social anxiety with peers (i.e., fear of negative evaluation, social avoidance or distress around new peers or new situations, and generalized social avoidance), and are scored on a 5-point scale (1 = Not at all, 5 = All the time) and summed. The SAS-A has strong support for its measurement model, validity, and reliability (La Greca et al., 2015; La Greca & Lopez, 1998). Based on clinical cutoffs (La Greca, 1999), adolescents with SAS-A scores > 50 at screening were identified as having clinically significant elevations in social anxiety and were potentially eligible for the open trial. In the current sample, internal consistency for this measure was .92 at screening.
Depressive symptoms were assessed with the Center for Epidemiological Studies Depression Scale (CES-D; Radloff, 1977), a well-validated measure that contains 20 items. Items are rated from 0 (Rarely) to 3 (Most or All of the time) and summed. Consistent with prior depression prevention research (Young et al., 2010) and the recommendation of the developer (Radloff, 1977), youth with total scores > 16 at screening were identified as having clinically significant depressive symptoms and were potentially eligible for the open trial. In this sample, internal consistency was .75 at screening.
Aggressive behavior was assessed at screening with the Aggression Subscale of the Youth Self Report (YSR; Achenbach & Rescorla, 2001), a well-validated measure of youth behavior problems. The subscale has 19 items, scored 0 (Not True) to 3 (Very True/Often True). This measure was used at screening to exclude adolescents with high levels of aggression (total scores > 14, representing a T-score of 63 (90th percentile; Achenbach & Rescorla, 2001). Internal consistency for this measure was .79.
Cyber PV and cyber aggression were assessed with the Cyber-Peer Experiences Questionnaire (C-PEQ; Landoll et al., 2015) to monitor adolescents’ cyber experiences. The nine items for cyber PV pertain to aversive peer experiences that occur via electronic media (i.e., cell phones, internet, social networking sites). Items are rated from 1 (Never) to 5 (A few times a week) and averaged across items. Parallel versions of the nine items for cyber PA ask adolescents to indicate whether they perpetrated cyber aggression against peers (0 = No, 1 = Yes). The C-PEQ has demonstrated construct validity and acceptable levels of reliability among adolescents (e.g., a = .78 – .83 for cyber victimization items; Landoll et al., 2015). In the current sample, internal consistency at screening was .83 for cyber PV and .68 for cyber PA.
Intervention acceptability was assessed at post-intervention with the IPT-UTalk Feedback Survey (available from the first author), a 17-item questionnaire modeled on the Treatment Satisfaction Questionnaire that evaluated the IPT-AST intervention (Young & Mufson, 2012). Most of the items asked for informal feedback on the intervention (e.g., likes and dislikes, suggestions for improvement). However, five items on the quality, helpfulness, satisfaction, and effectiveness of the intervention were used to evaluate acceptability and one item was used to evaluate generalizability of the intervention to non-peer relationships (see Results); these items were rated on 4- or 5-point scales, with positive and negative anchors at each end (e.g., very satisfied, mostly satisfied, indifferent, mildly dissatisfied, quite dissatisfied).
Social support was assessed at baseline and post-intervention with the Perceived Social Support Scale (PSS; Procidano & Heller, 1983). The scales for Friends and for Family each have 20 items (0=False, 1=True) that are summed to assess adolescents’ perceived emotional support. The PSS has been used with multicultural samples of adolescents and has demonstrated excellent validity and internal consistency (Procidano & Heller, 1983). In the current sample, internal consistency at baseline (N = 14) was .70 for PSS-Friends and .79 for PSS-Family.
Independent Evaluator Measures
At baseline and post-intervention, independent evaluators (IEs) administered the Anxiety Disorders Interview Schedule for DSM-IV – Child Version (ADIS-C; Silverman & Albano, 1996), a semi-structured interview that assesses the presence and severity of DSM-IV disorders. The ADIS-C has excellent psychometric properties (Wood et al., 2002). The Clinical Severity Ratings (CSRs) can range from 0 (absent) to 8 (very severely disturbing/disabling); scores of 4 or more represent a clinical disorder. IEs used the interview to assess social anxiety disorder, generalized anxiety disorder, posttraumatic stress disorder, major depressive disorder, dysthymia, bipolar disorder, substance abuse, schizophrenia, and eating disorders. The interview was used to determine open trial eligibility (i.e., a CSR less than 4 for social anxiety and depressive disorders) and to evaluate intervention outcome.
The Clinical Global Impressions Scale (CGI; Guy, 1976) is a widely used rating of severity of psychopathology and treatment response consisting of two items, one measuring improvement and one measuring severity of illness. The IEs’ ratings of “severity of illness” (1 = No psychiatric illness, 7 = Extremely severe) were used to evaluate intervention outcome.
The Columbia-Suicide Severity Rating Scale (C-SSRS; Posner et al. 2009) contains 21 items to evaluate the presence of suicidality. Any adolescents with active suicidal ideation, intent, plan, or other self-injurious behavior were excluded and provided referral information.
Ratings of Intervention Fidelity
Fidelity was monitored using the UTalk Clinical Checklist that evaluated clinicians’ adherence to each session’s intervention goals. Depending on the intervention session, clinicians rated 10 to 17 items regarding how well they completed each session goal (Very Well, Well, Could Be Improved, Did Not Complete, and Not Applicable). In addition, the clinical supervisors provided independent weekly ratings of how well the clinicians adhered to the intervention protocol on the UTalk Supervision Checklist to obtain a measure of both completion of specific tasks and use of techniques (Very Well, Well, Could Be Improved, Did Not Complete, and Not Applicable). Clinicians also were given ratings on overall knowledge of the program, rapport with the adolescents, collaborative style, appropriate group content, and individualization of content (Very Well, Well, Could Be Improved, Not Applicable to Session).
Data Analytic Plan
Analyses were conducted in SPSS Version 22. For feasibility, we calculated the percentage of adolescents who completed the program and the average number of sessions attended. For acceptability, we calculated the frequencies for adolescents’ responses to five key questions on the UTalk Feedback Survey. For program benefit and generalizability, intent-to-treat analyses were conducted with all 14 participants. Means and frequencies were calculated for the primary outcomes (i.e., clinician ratings, adolescent reports of relational and reputational PV), secondary outcomes (i.e., adolescent ratings of social anxiety, depression, and peer support), and other outcomes of interest (i.e., overt and cyber PV, family support, peer aggression). One-tailed paired sample t-tests were conducted to evaluate changes on outcome variables from baseline to post-intervention. Baseline and post-intervention scores were also compared to benchmarks obtained from a community sample of adolescents residing in the same school district (Herge et al., 2016). All adolescents enrolled in UTalk completed post-intervention measures. There was a very small amount of missing data across baseline and post-intervention (3 participants skipped a total of 6 items across all the adolescent-reported measures, representing less than 0.2% of the total data values). Thus, missingness was handled with mean substitution, which is a reasonable method for handling a small percentage of missing data (Downey & King, 1998). Additionally, one adolescent did not complete the peer aggression items of the C-PEQ at post-intervention and thus was not included in the analysis of change from baseline to post-intervention on this measure.
Results
Feasibility
Treatment completers
Of the 14 adolescents enrolled in the open trial, 12 (86%) completed the intervention. Only 2 adolescents, one from each school, withdrew due to schedule conflicts (i.e., the group sessions interfered with an important academic subject or activity).
Attendance
The 12 adolescents who completed the intervention, on average, attended 11.58 of 13 sessions (3 individual and 10 group). All absences occurred for the group sessions, where the median attendance was 9 of 10 sessions. Absences were due to scheduling issues (e.g., having an exam at the time of group), illness, or school absence on the day of group.
Acceptability
Post-intervention ratings of satisfaction
Adolescent ratings for five key items on the UTalk Feedback Survey were used to evaluate intervention acceptability and satisfaction. All responses were positive. First, adolescents rated the quality of the group as “excellent” (75%) or “good” (25%). Second, adolescents indicated they were “very satisfied” (67%) or “mostly satisfied” (33%) with the amount of help they received. Third, all adolescents indicated they received the kind of help they wanted from the program (Yes, definitely = 42%, Yes, generally = 58%). Fourth, all adolescents would recommend the program to a friend who was interested in participating (Yes, definitely = 75%, Yes, generally = 25%). Finally, all adolescents indicated that the program helped them deal more effectively with their peers either “a great deal” (42%) or “somewhat” (58%). None of the responses to the five questions were negative.
As a potential indicator of generalizability for the peer-based intervention, we also asked adolescents whether the program helped them to deal more effectively with other important people in their life. Here, adolescents indicated that the group helped “a great deal” (25%) or “somewhat” (75%) with other important people; none answered that it “really didn’t help” or “seemed to make things worse.”
Open Trial Outcomes
Characteristics of the 14 participating adolescents are presented in Table 1. At screening, the adolescents reported significant elevations in social anxiety, depressive symptoms, and both relational and reputational PV. These means were significantly higher than those for adolescents in a community sample (Herge et al., 2016) residing in the same metropolitan area: SAS-A = 37.66 (± 13.30); CES-D = 13.75 (± 9.72); R-PEQ Scores for relational PV = 1.63 (± .63) and reputational PV = 1.51 (± .70); all p’s < .05.
Primary outcomes
Intention-to-treat analyses of the primary outcome variables (Table 2) revealed significant decreases from baseline to post-intervention (with large effect sizes) for clinician ratings of severity on the ADIS-C (for the primary diagnosis) and on the CGI. Adolescents also reported significant declines in relational PV and reputational PV (medium to large effect sizes), and their post-intervention scores did not differ significantly from those of adolescents in a community sample (Herge et al., 2016).
Table 2.
Baseline to Post-Intervention Changes (Means ± SDs) for Outcome Variables (n = 14)a
| Variable | Baseline | Post- Intervention |
t-valuea | p-value | Cohen’s d |
|---|---|---|---|---|---|
| Primary Outcomes | |||||
| Clinician Ratings | |||||
| CSR from ADIS-C | 2.50 (1.29) | 1.50 (1.16) | 3.89 | .001 | 1.04 |
| CGI-Severity | 2.57 (.85) | 1.71 (.91) | 4.16 | .001 | 1.11 |
| Peer Victimization (R-PEQ) | |||||
| Relational PV | 2.17 (.61) | 1.76 (.68)b | 2.11 | .028 | .56 |
| Reputational PV | 1.81 (.68) | 1.31 (.36)b | 3.50 | .002 | .93 |
| Secondary Outcomes | |||||
| Social Anxiety (SAS-A) | 44.64 (10.08) | 36.00 (13.18)b | 2.92 | .006 | .78 |
| Depression (CES-D) | 16.71 (7.75) | 11.43 (10.80)b | 1.77 | .049 | .47 |
| Social Support - Friends | 12.57 (3.69) | 14.43 (3.88)b | −5.38 | .001 | 1.44 |
| Other Outcomes | |||||
| Peer Victimization | |||||
| Overt (R-PEQ) | 1.14 (.28) | 1.05 (.18)** | 1.47 | .083 | .39 |
| Cyber (C-PEQ) | 1.45 (.35) | 1.17 (.22)b | 2.80 | .008 | .75 |
| Peer Aggression | |||||
| Overt (R-PEQ) | 1.14 (.39) | 1.00 (.00)** | 1.38 | .095 | .37 |
| Relational (R-PEQ) | 1.79 (.72) | 1.36 (.48)b | 2.78 | .008 | .74 |
| Reputational (R-PEQ) | 1.36 (.66) | 1.12 (.36)b | 1.86 | .043 | .50 |
| Cyber (C-PEQ) | .21 (.18) | .16 (.15)b | 1.20 | .130 | .33 |
| Social Support - Family | 9.86 (4.45) | 11.79 (6.57)b | −1.62 | .065 | .43 |
Note: CSR = Clinical Severity Rating (for primary diagnosis); ADIS-C = Anxiety Disorders Interview Schedule for DSM-IV – Child Version; CGI = Clinical Global Impressions Scale; SAS-A = Social Anxiety Scale for Adolescents; CES-D = Center for Epidemiological Studies Depression Scale; R-PEQ = Revised Peer Experiences Questionnaire
Based on Intention-to-Treat analyses using paired-sample t-tests; n = 13 for C-PEQ Aggression
Scores are not significantly different from a community sample (Herge et al., 2016)
Scores are significantly lower than for adolescents in a community sample (Herge et al., 2016)
Secondary outcomes
Intention-to-treat analyses of the secondary outcomes (Table 2) revealed significant declines in adolescent-reported symptoms of social anxiety and depression (medium effect sizes), which, at post-intervention, did not differ significantly from adolescents in a community sample (Herge et al., 2016). Increases were observed in perceived social support from friends (large effect size).
Generalization and Potential Adverse Outcomes
Because this was an intervention development project, we examined several additional variables to determine whether the intervention: a) generalized to other aspects of adolescents’ interpersonal functioning that were not directly targeted in the intervention (i.e., overt and cyber PV, family support), and b) did not lead to problems with peer aggression. As seen in Table 2, over the course of the intervention, significant declines were observed for adolescents’ reports of cyber PV. No significant changes were observed for overt PV or for social support from family members. Further, no increases in adolescent-reported peer aggression were observed; in fact, peer aggression levels declined significantly for interpersonal forms of peer aggression (i.e., relational aggression and reputational aggression).
In addition to the above, at post-intervention, one of the 14 adolescents (7%) met diagnostic criteria for social phobia on the ADIS-C, with a clinical severity rating of 4 (i.e., clinically significant, just above threshold). This adolescent had received a diagnosis of Anxiety Disorder, Not Otherwise Specified (with sub-clinical Social Phobia symptoms noted) at baseline and had been given a clinical severity rating of 6 for this diagnosis (i.e., frequently interfering, more than moderately disabling), but had not been excluded from the intervention due to failure to meet full Social Phobia criteria. No other adolescents met criteria for an anxiety or depressive disorder at post-intervention and no adolescents were terminated from the intervention due clinical deterioration or the need for immediate clinical referral (e.g., suicidal intent or plan).
Treatment Fidelity
Clinicians’ weekly ratings of the UTalk sessions were positive, indicating that they met the intervention goals well or very well. Specifically, across all the sessions, clinicians at School 1 rated 87.7% of the items (regarding how well they met intervention goals) as Well or Very Well, and clinicians at School 2 rated 92.5% of items as Well or Very Well. All the clinicians received ratings of Well or Very Well on supervisor ratings for the UTalk Supervision Checklist.
Discussion
This study is the first to evaluate a transdiagnostic approach to the prevention of adolescent SAD and depression and to target a peer-risk factor for these disorders. UTalk builds on and extends IPT-AST (Young et al., 2006), a preventive intervention for adolescent depression, by directly addressing adolescents’ symptoms of social anxiety and by incorporating a focus on peer victimization issues. In particular, interpersonal peer victimization (IPV) is common among adolescents and directly contributes to social anxiety and/or depression (e.g., Dinkes et al., 2007; La Greca & Harrison, 2005; Siegel et al., 2009; Storch et al., 2005), yet strategies for dealing with IPV have not been incorporated into existing prevention programs for internalizing disorders. Our findings suggest that the UTalk version of IPT-AST may be beneficial for adolescents who report IPV and subclinical levels of SAD and/or depression.
Feasibility, Acceptability, and Preliminary Benefit
Specifically, the UTalk intervention appeared feasible to conduct in a school setting and was acceptable to the adolescents who participated. Most of the adolescents who were eligible after screening elected to participate in the intervention (76%), and most who enrolled in the prevention trial completed the program (86%); these rates are comparable to those of other school-based depression prevention programs (e.g., Young et al., 2006, 2010). The intervention completion rate also is comparable to that of clinical interventions for adolescent social anxiety disorder or depressive disorder (e.g., Masia Warner et al., 2007; Mufson et al., 2004c). Further, all adolescents reported high levels of satisfaction with the UTalk intervention; none reported negative ratings for any of the feedback items. Our anecdotal observations are consistent with these data, as adolescents often expressed high interest in and enthusiasm for “UTalk.” Adolescent engagement in the group intervention was especially remarkable given the high levels of social anxiety that adolescents reported pre-intervention. Our findings also suggest that the UTalk intervention can be implemented with good fidelity and integrity.
Importantly, findings regarding the potential benefit of the UTalk intervention were encouraging and support the need for continued evaluation of the intervention’s effectiveness. Participating adolescents displayed significant declines in symptoms of social anxiety and depression (as rated by adolescents and independent evaluators) and in relational and reputational peer victimization. Their self-reported functioning at post-intervention was comparable to adolescents in a large community sample. Further, adolescents reported positive gains for secondary outcomes, including increased social support from friends and reductions in cyber PV (which were not directly targeted in the intervention).
Also noteworthy was the fact that we did not observe clinical deterioration or other adverse outcomes for participating adolescents; in fact, adolescents’ post-intervention levels of overt peer victimization and overt peer aggression were significantly below the levels reported by adolescents in a community sample. Together the findings suggest that the UTalk intervention was successful in reducing adolescents’ symptoms of social anxiety and depression and their interpersonal PV, and also may have had some positive “spillover effects” by reducing peer aggression and enhancing peer-based social support.
Further evaluation of the UTalk intervention in a randomized controlled trial and with a follow-up assessment is essential before more definitive statements can be made about its effects. Nevertheless, the current findings are promising and raise the possibility of the program serving as an effective intervention for reducing the negative effects of bullying and cyberbullying. Despite high levels of “traditional” and cyber PV among older adolescents (Dinkes et al., 2007; Lenhart et al., 2010; Landoll et al., 2015), a recent review of school-based interventions for bullying and cyberbullying (Cantone et al., 2015) revealed a dearth of effective programs, especially for adolescents. Our findings suggest that an intervention like the UTalk version of IPT-AST may be useful for reducing the adverse impact of peer and cyber victimization.
Limitations and Future Directions
This study represents an important preliminary evaluation of the UTalk intervention, and studies that extend the current findings are critical. Future studies need to address several potential biases that could have affected the results of our open trial, such as the lack of random assignment to a control condition, the small sample size, and use of multiple analyses of outcome measures. In the future, a randomized controlled trial with a larger sample of youth is needed to address these limitations and also allow for the examination of potential mediators and moderators of intervention outcome.
From a practical standpoint, although our data suggest that UTalk can be implemented successfully in schools, we recognize that school-based interventions can be challenging. This was particularly true for scheduling group sessions during the school day, as adolescents’ class schedules differed substantially, and the two adolescents who dropped out of the intervention cited schedule conflicts. Scheduling issues are common in school-based interventions (Chu, Colognori, Weissman, & Bannon, 2009; Masia Warner et al., 2015), where time limitations and irregular schedules may require flexibility in implementation. Scheduling sessions after school or conducting sessions on different weekdays or during time-periods dedicated to elective programming might help to minimize this issue in future studies.
Furthermore, an important direction for future research is to examine the sustainability of school-based interventions, such as UTalk, and explore potential cost-effective models for intervention delivery. We designed UTalk (i.e., group format; weekly sessions over an academic semester; detailed manual with multiple examples) so that it would be feasible for school counselors or school psychologists to administer. Other school-based programs (e.g., SASS, Masia Warner et al., 2015) have used similar strategies to enable school personnel to deliver interventions effectively. Exploring alternative and low-cost delivery models, such as teacher-led elective classes or peer-led coaching, will be important and desirable. Despite potential implementation challenges, school-based interventions are appealing as they facilitate access to evidence-based interventions for youth in need, especially for minority and economically disadvantaged youth who otherwise may not receive mental health attention (Kataoka et al., 2002; Masia Warner et al., 2015).
There are several notable strengths to the current study. In our assessment strategy, we compared the functioning of participating adolescents to those in a community setting (i.e., community benchmarks), which revealed that our participants were significantly more distressed at pre-intervention, but no longer differed from community youth at post-intervention on key outcome variables. We also incorporated independent evaluations of adolescents’ symptomatology rather than relying on self-reported symptoms, which has been commonly done in depression prevention studies (see Stice et al., 2009). Importantly, we focused on diverse youth who came from predominantly Hispanic backgrounds, which is an underserved population for mental heath needs (Kataoka et al., 2002).
In summary, the UTalk version of IPT-AST, which takes an integrated, transdiagnostic approach to preventing adolescent SAD and depression and targets peer victimization issues, has the potential to be feasible and acceptable in high school settings. An interpersonal model appears to be well suited to the prevention of both social anxiety and depression. Our preliminary results suggest that adolescents who experience significant symptoms of social anxiety or depression as well as elevated levels of interpersonal peer victimization may benefit from the intervention. Future studies that incorporate randomized designs, credible control conditions, and follow-up assessments will be important to verify our findings.
Acknowledgments
Funding
This study was funded by a grant from the National Institute of Mental Health (R34 MH095959) to the first author (PI) and the next two co-authors (Co-Is). The effort of the last author was supported in part by funding from the Canadian Institutes of Health Research Doctoral Foreign Study Award (#201210DFS-303899-191868).
Author C has received book royalties from Guilford Publications, Inc. and Oxford University Press for publications on Interpersonal Psychotherapy for Depressed Adolescents and Interpersonal Psychotherapy - Adolescent Skills Training, respectively.
Footnotes
Conflict of Interest:
Authors A, B, and D declare that they have no conflict of interest.
A copy of the Manual is available from the first author.
Compliance with Ethical Standards
Research Involving Human Participants
All procedures performed in the study were in accordance with national and institutional ethical standards for research with human subjects and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained for all participants. In general, written informed parental consent and written adolescent assent were required for all adolescents prior to participating in the screening phase of the open trial. Separate written parental consent and written adolescent assent were required for all adolescents participating in the open trial intervention.
Access to Data
The first author and fourth authors take responsibility for the integrity of the data and the accuracy of the data analyses.
References
- Achenbach TM, Rescorla LA. Manual for the ASEBA School-Age Forms & Profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth, & Families; 2001. [Google Scholar]
- Ahlen J, Lenhard F, Ghaderi A. Universal prevention for anxiety and depressive symptoms in children: A meta-analysis of randomized and cluster-randomized trials. Journal of Primary Prevention. 2015;36(6):387–403. doi: 10.1007/s10935-015-0405-4. [DOI] [PubMed] [Google Scholar]
- Aune T, Stiles TC. Universal-based prevention of syndromal and subsyndromal social anxiety: A randomized controlled study. Journal of Consulting and Clinical Psychology. 2009;77(5):867–879. doi: 10.1037/a0015813. [DOI] [PubMed] [Google Scholar]
- Barrett PM, Farrell LJ, Ollendick TH, Dadds M. Long-term outcomes of an Australian universal prevention trial of anxiety and depression symptoms in children and youth: An evaluation of the FRIENDS program. Journal of Clinical Child and Adolescent Psychology. 2006;35(3):403–411. doi: 10.1207/s15374424jccp3503_5. [DOI] [PubMed] [Google Scholar]
- Beesdo K, Bittner A, Pine DS, Stein MB, Hölfer M, Lieb DR, Wittchen H. Incidence of social anxiety disorder and the consistent risk for secondary depression in the first three decades of life. Archives of General Psychiatry. 2007;64:903–912. doi: 10.1001/archpsyc.64.8.903. [DOI] [PubMed] [Google Scholar]
- Beidel DC, Turner SM, Morris TL. Behavioral treatment of childhood social phobia. Journal of Consulting and Clinical Psychology. 2000;68:1072–1080. [PubMed] [Google Scholar]
- Birmaher B, Ryan ND, Williamson DE, Brent DA, Kaufman J. Childhood and adolescent depression: A review of the past 10 years. Journal of the American Academy of Child and Adolescent Psychiatry. 1996;35(12):1575. doi: 10.1097/00004583-199612000-00008. [DOI] [PubMed] [Google Scholar]
- Blechman EA, McEnroe MJ, Carella ET, Audette DP. Childhood competence and depression. Journal of Abnormal Psychology. 1986;95:223–227. doi: 10.1037//0021-843x.95.3.223. [DOI] [PubMed] [Google Scholar]
- Blöte AW, Miers AC, Heyne DA, Westenberg PM. Social anxiety and the school environment of adolescents. In: Ranta K, La Greca AM, García-Lopez LJ, Marttunen M, editors. Social anxiety and phobia in adolescents: Development, manifestation and intervention strategies. Springer International Publishing; 2015. pp. 151–181. [Google Scholar]
- Cantone E, Piras AP, Vellante M, Preti A, Danielsdottir S, D’Aloja E, Lesinskiene S, Angermeyes MC, Carta MG, Bhugra D. Interventions on bullying and cyberbullying in schools: A systematic review. Clinical Practice and Epidemiology in Mental Health. 2015;11(Suppl 1: M4):58–76. doi: 10.2174/1745017901511010058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chu BC, Colognori D, Weissman AS, Bannon K. An initial description and pilot of group behavioral activation therapy for anxious and depressed youth. Cognitive and Behavioral Practice. 2009;11:408–419. [Google Scholar]
- Clarke GN, Hawkins W, Murphy M, Sheeber LB, Lewinsohn PM, Seeley JR. Targeted prevention of unipolar depressive disorder in an at-risk sample of high school adolescents: A randomized trial of a group cognitive intervention. Journal of the American Academy of Child and Adolescent Psychiatry. 1995;34(3):312–321. doi: 10.1097/00004583-199503000-00016. [DOI] [PubMed] [Google Scholar]
- Cook CR, Williams KR, Guerra NG, Kim TE, Sadek S. Predictors of bullying and victimization in childhood and adolescence: A meta-analytic investigation. School Psychology Quarterly. 2010;25(2):65–83. [Google Scholar]
- Costello EJ, Egger H, Copeland W, Erkanli A, Angold A. The developmental epidemiology of anxiety disorders: Phenomenology, prevalence, and comorbidity. In: Silverman WK, Field A, editors. Anxiety disorders in children and adolescents. 2nd. New York, NY: Cambridge University Press; 2011. [Google Scholar]
- Costello EJ, Mustillo S, Erkanli A, Keeler G, Angold A. Prevalence and development of psychiatric disorders in childhood and adolescence. Archives of General Psychiatry. 2003;60(8):837–844. doi: 10.1001/archpsyc.60.8.837. [DOI] [PubMed] [Google Scholar]
- Dalrymple KL, Zimmerman M. Age of onset of social anxiety disorder in depressed outpatients. Journal of Anxiety Disorders. 2011;25:131–137. doi: 10.1016/j.janxdis.2010.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davila J, Beck JG. Is social anxiety associated with impairment in close relationships? A preliminary investigation. Behavior Therapy. 2002;33:427–446. [Google Scholar]
- De Los Reyes A, Prinstein MJ. Applying depression-distortion hypotheses to the assessment of peer victimization in adolescents. Journal of Clinical Child Adolescent Psychology. 2004;33(2):325–335. doi: 10.1207/s15374424jccp3302_14. [DOI] [PubMed] [Google Scholar]
- Dinkes R, Cataldi EF, Lin-Kelly W. Indicators of school crime and safety: 2007 (NCES 2008-021/NCJ 219553) Washington, DC: National Center for Education Statistics, Institute of Education Sciences, U.S. Department of Education, and Bureau of Justice Statistics, Office of Justice Programs, U.S. Department of Justice; 2007. [Google Scholar]
- Dozois DJA, Seeds PM, Collins KA. Transdiagnostic approaches to the prevention of depression and anxiety. Journal of Cognitive Psychotherapy. 2009;23:44–59. [Google Scholar]
- Downey RG, King CV. Missing data in Likert ratings: A comparison of replacement methods. Journal of General Psychology. 1998;125:175–191. doi: 10.1080/00221309809595542. 1998. [DOI] [PubMed] [Google Scholar]
- Ehrenreich-May J, Bilek EL, Buzzella BA, Kennedy SM, Mash JA, Bennett SM. The unified protocols for the transdiagnostic treatment of emotional disorders in children and adolescents: Therapist guide. New York: Oxford University Press; (in press) [Google Scholar]
- Essau CA, Conradt J, Sasagawa S, Ollendick TM. Prevention of anxiety symptoms in children: A universal school-based trial. Behavior Therapy. 2012;43:450–464. doi: 10.1016/j.beth.2011.08.003. [DOI] [PubMed] [Google Scholar]
- Garber J, Clarke GN, Weersing VR, Beardslee WR, et al. Prevention of depression in at-risk adolescents. Journal of the American Medical Association. 2009;301(21):2215–2224. doi: 10.1001/jama.2009.788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garber J, Weersing VR. Comorbidity of anxiety and depression in youth: Implications for treatment and prevention. Clinical Psychology: Science and Practice. 2010;17:293–306. doi: 10.1111/j.1468-2850.2010.01221.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ginsburg GS, La Greca AM, Silverman WK. Social anxiety in children with anxiety disorders: Relation with social and emotional functioning. Journal of Abnormal Child Psychology. 1998;26(3):75–185. doi: 10.1023/a:1022668101048. [DOI] [PubMed] [Google Scholar]
- Grant BF, Hasin D, Blanco C, Stinson FS, Huang B. The epidemiology of social anxiety disorder in the United States: Results from the national epidemiologic survey on alcohol and related conditions. Journal of Clinical Psychiatry. 2005;66(11):1351–1361. doi: 10.4088/jcp.v66n1102. [DOI] [PubMed] [Google Scholar]
- Guy W. Clinical Global Impression Scale. The ECDEU Assessment Manual for Psychopharmacology-Revised. Volume DHEW Publ No ADM 76. 1976;338:218–222. [Google Scholar]
- Hankin BL. Development of sex differences in depressive and co-occurring anxious symptoms during adolescence: Descriptive trajectories and potential explanations in a multiwave prospective study. Journal of Clinical Child and Adolescent Psychology. 2009;38:460–472. doi: 10.1080/15374410902976288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herge WM, La Greca AM, Chan SR. Adolescent peer victimization and physical health problems. Journal of Pediatric Psychology. 2016;41(1):15–27. doi: 10.1093/jpepsy/jsv050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hough RL, Hazen A, Soriano F. Mental health care for Latinos: Mental health services for Latino adolescents with psychiatric disorders. Psychiatry Service. 2002;53:1556–1562. doi: 10.1176/appi.ps.53.12.1556. [DOI] [PubMed] [Google Scholar]
- Kärnä A, Voeten M, Little TD, Poskiparta E, Alanen E, Salmivalli C. Going to scale: A nonrandomized nationwide trial of the KiVa antibullying program for grades 1–9. Journal of Consulting and Clinical Psychology. 2011;79(6):796–805. doi: 10.1037/a0025740. [DOI] [PubMed] [Google Scholar]
- Kataoka SH, Zhang L, Wells KB. Unmet need for mental health care among U.S. children: Variation by ethnicity and insurance status. American Journal of Psychiatry. 2002;159(9):1548–1555. doi: 10.1176/appi.ajp.159.9.1548. [DOI] [PubMed] [Google Scholar]
- Kendall PC, Furr JM, Podell JL. Child-focused treatment of anxiety. In: Weisz J, Kazdin A, editors. Evidence-based psychotherapies for children and adolescents. 2nd. New York, NY: Guildford Press; 2010. pp. 45–60. [Google Scholar]
- La Greca AM. Manual for the Social Anxiety Scales for Children and Adolescents - Revised. Miami, FL: Author; 1999. (Available from the author.) [Google Scholar]
- La Greca AM, Harrison HM. Adolescent peer relations, friendships, and romantic relationships: Do they predict social anxiety and depression? Journal of Clinical Child and Adolescent Psychology. 2005;34(1):49–61. doi: 10.1207/s15374424jccp3401_5. [DOI] [PubMed] [Google Scholar]
- La Greca AM, Lai B. The role of peer relationships in youth psychopathology. In: Chu B, Ehrenreich-May J, editors. Transdiagnostic mechanisms and treatment of youth psychopathology. New York: Guilford Press; 2014. pp. 111–137. [Google Scholar]
- La Greca AM, Landoll RR. Peer influences in the development and maintenance of anxiety disorders. In: Silverman WK, Field A, editors. Anxiety disorders in children and adolescents: Research, assessment, and intervention. 2nd. London: Cambridge University Press; 2011. [Google Scholar]
- La Greca AM, Lopez N. Social anxiety among adolescents: Linkages with peer relations and friendships. Journal of Abnormal Child Psychology. 1998;26(2):83–94. doi: 10.1023/a:1022684520514. [DOI] [PubMed] [Google Scholar]
- La Greca AM, Young JE, Mufson L, Ehrenreich-May J, Girio-Herrera E. Manual for the PEERS/UTalk version of Interpersonal Psychotherapy-Adolescent Skills Training. University of Miami, Coral Gables, FL: Authors; 2015. (Available from first author.) [Google Scholar]
- Landoll RL, La Greca AM, Lai BS, Chan S, Herge W. Cyber victimization by peers: Prospective associations with adolescent social anxiety and depressive symptoms. Journal of Adolescence. 2015;42:77–86. doi: 10.1016/j.adolescence.2015.04.002. [DOI] [PubMed] [Google Scholar]
- Lenhart A, Purcell K, Smith A, Zickuhr K. Social media and young adults. [Retrieved on May 24, 2016];Pew Research Internet Project. 2010 from http://pewresearch.org/pubs/1484/social-media-mobile-internet-use-teens-millennials-fewer-blog. [Google Scholar]
- Lipsitz JD, Gur M, Vermes D, Petkova E, Cheng J, Miller N, Laino J, Fyer AJ. A randomized trial of interpersonal therapy versus supportive therapy for social anxiety disorder. Depression and Anxiety. 2008;25(6):542–553. doi: 10.1002/da.20364. [DOI] [PubMed] [Google Scholar]
- Masia Warner C, Colognori D, Brice C, Sanchez A. A school-based intervention for adolescents with Social Anxiety Disorder. In: Ranta K, La Greca KAM, Marttunen M, Garcia-Lopez LJ, editors. Social anxiety and social phobia in adolescents: Development, manifestation, and treatment strategies. New York, NY: Springer; 2015. pp. 271–288. [Google Scholar]
- Masia Warner C, Fisher PH, Shrout PE, Rathor S, Klein RG. Treating adolescents with social anxiety disorder in school: An attention control trial. Journal of Child Psychology and Psychiatry. 2007;48:676–686. doi: 10.1111/j.1469-7610.2007.01737.x. [DOI] [PubMed] [Google Scholar]
- McLaughlin KA, Hatzenbuehler ML, Hilt LM. Emotion dysregulation as a mechanism linking peer victimization to internalizing symptoms in adolescents. Journal of Consulting Clinical Psychology. 2009;77(5):894–904. doi: 10.1037/a0015760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merikangas KR, He JP, Brody D, Fisher PW, Bourdon K, Koretz DS. Prevalence and treatment of mental disorders among US children in the 2001–2004 NHANES. Pediatrics. 2010;125(1):75–81. doi: 10.1542/peds.2008-2598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miami-Dade County Public Schools. [Retrieved on May 19, 2016];Statistical Highlights, 2012–13. 2013 from http://drs.dadeschools.net/StatisticalHighlights/SH1213_Final.pdf. [Google Scholar]
- Mufson L, Dorta KP, Moreau D, Weissman MM. Interpersonal psychotherapy for depressed adolescents. second. New York: Guilford Publications, Inc; 2004a. [Google Scholar]
- Mufson L, Gallagher T, Dorta KP, Young JF. Interpersonal psychotherapy for adolescent depression: Adaptation for group therapy. American Journal of Psychotherapy. 2004b;58:220–237. doi: 10.1176/appi.psychotherapy.2004.58.2.220. [DOI] [PubMed] [Google Scholar]
- Mufson L, Dorta KP, Wickramaratne P, Nomura Y, Olfson M, Weissman MM. A randomized effectiveness trial of Interpersonal Psychotherapy for depressed adolescents. Archives of General Psychiatry. 2004c;61:577–584. doi: 10.1001/archpsyc.61.6.577. [DOI] [PubMed] [Google Scholar]
- Mufson L, La Greca AM, Young J, Ehrenreich-May J. Interpersonal approaches to intervention: Implications for preventing and treating social anxiety in adolescents. In: Ranta K, La Greca KAB, Marttunen M, Garcia-Lopez LJ, editors. Social anxiety and social phobia in adolescents: Development, manifestation, and treatment strategies. New York, NY: Springer; 2015. pp. 251–270. [Google Scholar]
- Olweus D. Bullying at school: What we know and what we can do. Oxford, England: Blackwell Publishers; 1993. [Google Scholar]
- Posner K, Brent D, Lucas C, Gould M, Stanley B, Brown G, Mann J. Columbia-Suicide Severity Rating Scale. Manual for the Columbia Suicide Severity Rating Scale. New York, NY: New York State Psychiatric Institute; 2009. [Google Scholar]
- Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Ranta K, Kaltiala-Heino R, Pelkonen M, Marttunen M. Associations between peer victimization, self-reported depression and social phobia among adolescents: The role of comorbidity. Journal of Adolescence. 2009;32(1):77–93. doi: 10.1016/j.adolescence.2007.11.005. [DOI] [PubMed] [Google Scholar]
- Rudolph KD, Hammen C, Burge D, Lindberg N, Herzberg D, Daley SE. Toward an interpersonal life-stress model of depression: The developmental context of stress generation. Development and Psychopathology. 2000;12:215–234. doi: 10.1017/s0954579400002066. [DOI] [PubMed] [Google Scholar]
- Salmivalli C, Sainio M, Hodges E. Electronic victimization: Correlates, antecedents, and consequences among elementary and middle school students. Journal of Clinical Child and Adolescent Psychology. 2013;42(4):442–453. doi: 10.1080/15374416.2012.759228. [DOI] [PubMed] [Google Scholar]
- Sburlati ES, Lyneham HJ, Mufson L, Schneiring CA. A model of therapist competencies for the empirically supported Interpersonal Psychotherapy for Adolescent Depression. Clinical Child and Family Psychology Review. 2012;15:93–112. doi: 10.1007/s10567-012-0111-1. [DOI] [PubMed] [Google Scholar]
- Siegel RS, La Greca AM, Harrison HM. Peer victimization and social anxiety in adolescents: Prospective and reciprocal relationships. Journal of Youth and Adolescence. 2009;38(8):1096–1109. doi: 10.1007/s10964-009-9392-1. [DOI] [PubMed] [Google Scholar]
- Silverman WK, Albano AM. The Anxiety Disorders Interview Schedule for DSM-IV-Child and Parent Versions. London: Oxford University Press; 1996. [Google Scholar]
- Solberg ME, Olweus D. Prevalence estimation of school bullying with the Olweus Bully/Victim Questionnaire. Aggressive Behavior. 2003;29:239–268. [Google Scholar]
- Stein MB, Fuetsch M, Muller N, Hölfer M, Lieb DR, Wittchen H. Social anxiety disorder and the risk of depression: A prospective community study of adolescents and young adults. Archives of General Psychiatry. 2001;58(3):251–256. doi: 10.1001/archpsyc.58.3.251. [DOI] [PubMed] [Google Scholar]
- Stice E, Shaw H, Bohon C, Marti CN, Rohde P. A meta-analytic review of depression prevention programs for children and adolescents: Factors that predict magnitude of intervention effects. Journal of Consulting and Clinical Psychology. 2009;77:486–503. doi: 10.1037/a0015168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Storch EA, Brassard MR, Masia-Warner C. The relationship of peer victimization to social anxiety and loneliness in adolescence. Child Study Journal. 2003;33(1):1–18. doi: 10.1016/j.adolescence.2004.03.003. [DOI] [PubMed] [Google Scholar]
- Storch EA, Masia-Warner C, Dent HC, Roberti JW, Fisher PH. Psychometric evaluation of the Social Anxiety Scale For Adolescents and the Social Phobia And Anxiety Inventory For Children: Construct validity and normative data. Journal of Anxiety Disorders. 2004;18:665–679. doi: 10.1016/j.janxdis.2003.09.002. [DOI] [PubMed] [Google Scholar]
- Storch EA, Masia-Warner C, Crisp H, Klein RG. Peer victimization and social anxiety in adolescence: A prospective study. Aggressive Behavior. 2005;31(5):437–452. [Google Scholar]
- Vernberg EM, Abwender DA, Ewell KK, Beery SH. Social anxiety and peer relationships in early adolescence: A prospective analysis. Journal of Clinical Child and Adolescent Psychology. 1992;21(2):189–196. [Google Scholar]
- Weems CF, Scott BG, Graham RA, Banks DM, Russell JD, Taylor LK, Cannon M, Varela RE, Scheeringa MS, Perry AM, Marino RC. Fitting anxious emotion focused intervention into the ecology of schools: Results from a test anxiety program evaluation. Prevention Science. 2015;16:200–210. doi: 10.1007/s11121-014-0491-1. [DOI] [PubMed] [Google Scholar]
- Williams KR, Guerra NG. Prevalence and predictors of Internet bullying. Journal of Adolescent Health. 2007;41(6):S14. doi: 10.1016/j.jadohealth.2007.08.018. [DOI] [PubMed] [Google Scholar]
- Wood JJ, Piacentini JC, Bergman RL, McCracken J, Barrios V. Concurrent validity of the anxiety disorders section of the Anxiety Disorders Interview Schedule for DSM-IV: Child and parent versions. Journal of Clinical Child and Adolescent Psychology. 2002;31:335–342. doi: 10.1207/S15374424JCCP3103_05. [DOI] [PubMed] [Google Scholar]
- Young JF, Mufson L. Manual for Interpersonal Psychotherapy: Adolescent Skills Training (IPT-AST) Authors; 2012. [Google Scholar]
- Young JF, Mufson L, Davies M. Efficacy of interpersonal psychotherapy-adolescent skills training: An indicated preventive intervention for depression. Journal of Child Psychology and Psychiatry. 2006;47(12):1254–1262. doi: 10.1111/j.1469-7610.2006.01667.x. [DOI] [PubMed] [Google Scholar]
- Young JF, Mufson L, Gallop R. Preventing depression: A randomized trial of interpersonal psychotherapy-adolescent skills training. Depression and Anxiety. 2010;27(5):426–433. doi: 10.1002/da.20664. [DOI] [PMC free article] [PubMed] [Google Scholar]