Abstract
Purpose. The purpose of this study was to investigate the expression of cancer-associated fibroblast- (CAF-) related proteins and the implications in breast phyllodes tumor (PT). Methods. Tissue microarrays of 194 PT cases (151 benign PT, 27 borderline PT, and 16 malignant PT) were constructed. We performed immunohistochemical staining for CAF-related proteins (podoplanin, prolyl 4-hydroxylase, FAPα, S100A4, PDGFR α/β, and NG2) and analyzed the results according to clinicopathologic parameters. Results. Expression of PDGFRα and PDGFRβ in the stromal component increased with increasing histologic grade of PT (p = 0.003 and p = 0.034, resp.). Among clinicopathologic parameters, only expression of FAPα in stroma was associated with distant metastasis (p = 0.002). In univariate analysis, stromal expression of PDGFRα was associated with shorter overall survival (p = 0.002). In Cox multivariate analysis, stromal overgrowth and PDGFRα stromal positivity were associated with shorter overall survival (p = 0.006 and p = 0.050, resp.). Furthermore, expression of PDGFRβ in stroma was associated with shorter overall survival in patients with malignant PT (p = 0.041). Conclusion. Stromal expression of PDGFRα and PDGFRβ increased with increasing histologic grade of PT. In addition, PDGFR stromal positivity was associated with shorter overall survival. These results suggest that CAFs are associated with breast PT progression.
1. Introduction
Progress in cancer research has increasingly revealed the clinical significance of the tumor microenvironment. Among various components of the tumor microenvironment, cancer-associated fibroblasts (CAFs), one of the most important elements, have been widely studied [1]. CAFs are located near the cancer cells and have been reported to be involved in tumor initiation, tumor-stimulatory inflammation, metabolism, metastasis, drug response, and immune surveillance [2]. Despite their significant effect on cancer cells, the exact cell origin of CAFs is not completely understood and there is even controversy concerning the definition of CAF [1, 2]. Various proteins have been suggested as markers for CAFs, including α-smooth muscle actin (SMA) [3], tenascin-C [4], chondroitin sulfate proteoglycan (NG2) [5], platelet-derived growth factor receptor (PDGFR)α/β [6], fibroblast activation protein (FAP) [7], podoplanin [8], prolyl 4-hydroxylase [9], and fibroblast-specific protein- (FSP-) 1 [5]. CAFs have been suggested to show various functional subtypes that exhibit different characteristics [10], supporting the hypothesis that CAFs have various phenotypes.
Phyllodes tumor (PT) is a relatively rare biphasic breast tumor that accounts for only 0.3–1.5% of all breast tumors [11]. It is composed of atypical spindle cell stroma and usually benign epithelium [12]. Pathologically, differential diagnosis is difficult because several histologic findings of PT overlap with those of fibroadenoma, which is also a fibroepithelial tumor, and PT shows heterogeneous histologic features within the tumor [11, 13]. In addition, some cases of PT show several clinical features of malignancy such as relapse or distant metastasis [14]. The histologic classification of PT varies according to authors, but PT has been classified as benign, borderline, and malignant according to the World Health Organization classification of tumors of the breast [11]. A higher histologic grade of PT is associated with increased risk of tumor recurrence or distant metastasis, indications of tumor aggressiveness. Furthermore, among malignant PT, 9–36% of cases experience local recurrence, 9–40% of cases progress with metastasis to the lungs, brain, or liver [15], and some cases suffer death due to recurrence and distant metastasis [16, 17]. The fibroblast is an important component of PT [18, 19]; therefore, variations in tumor biology of PT could be accounted for by the phenotype of associated fibroblasts. However, the role of CAF-related proteins in breast PT is poorly understood. The purpose of this study was to investigate the expression of CAF-related proteins and its implications in breast PT.
2. Materials and Methods
2.1. Patient Selection
Tissue samples from patients who were diagnosed with breast PT from 2000 to 2010 in Severance hospital were selected. All tissues were fixed in 10% buffered formalin and embedded in paraffin. Archival hematoxylin and eosin- (H&E-) stained slides for each case were reviewed by a single pathologist (Ja Seung Koo). The PT histologic grade was based on the World Health Organization classification of tumors of the breast [11]. The histologic grade was evaluated with H&E-stained slides and clinical data including patient age, recurrence, distant metastasis, and patient survival were obtained by reviewing the patients' medical records. The study was approved by the Institutional Review Board of Yonsei University Severance Hospital.
2.2. Tissue Microarray
Construction of tissue microarray was performed as previously described. Briefly, a representative area was selected on the H&E-stained slide of the tumor and a corresponding spot was marked on the surface of the paraffin block. Using a biopsy needle, the selected area was punched out and the 5 mm tissue core was placed in a 5 × 6 recipient block. To minimize extraction bias, we extracted two tissue cores for every PT case. Finally, each separate tissue core was assigned a unique tissue microarray location number linked to the database including other clinicopathologic data and was used for immunohistochemical staining.
2.3. Immunohistochemistry
The antibodies used for immunohistochemical staining in this study are shown in Table 1. All immunostaining was performed using the constructed tissue microarray. For immunohistochemistry, 5 μm sections were obtained with a microtome, transferred onto adhesive slides, and dried at 62°C for 30 min. After incubation with primary antibodies, immunodetection was performed with biotinylated antimouse immunoglobulin followed by peroxidase-labeled streptavidin using a labeled streptavidin biotin kit with 3,3′-diaminobenzidine chromogen as substrate. For the negative control, the primary antibody incubation step was omitted. Harris hematoxylin was used for tissue counterstaining. All immunohistochemical markers were assessed using light microscopy and evaluation of staining was performed by calculating the proportion of stained cells and immunostaining intensity. The proportion of stained cells was defined as follows: 0, negative; 1, less than 30% positive; and 2, more than 30% positive. The immunostaining intensity was defined as follows: 0, negative; 1, weak; 2, moderate; and 3, strong. The scores for proportion of stained cells and immunostaining intensity were multiplied, and staining was defined as positive when the final score was >1 [20].
Table 1.
Source, clone, and dilution of antibodies used for immunohistochemical staining.
| Antibody | Company | Clone | Dilution |
|---|---|---|---|
| CAF phenotype-related proteins | |||
| Podoplanin | Abcam, Cambridge, UK | 18H5 | 1 : 100 |
| Prolyl 4-hydroxylase | Abcam, Cambridge, UK | Polyclonal | 1 : 200 |
| FAPα | Abcam, Cambridge, UK | Polyclonal | 1 : 100 |
| S100A4 | Abcam, Cambridge, UK | Polyclonal | 1 : 100 |
| PDGFRα | Abcam, Cambridge, UK | Polyclonal | 1 : 100 |
| PDGFRβ | Abcam, Cambridge, UK | Y92 | 1 : 100 |
| NG2 | Abcam, Cambridge, UK | NG2 | 1 : 50 |
2.4. Statistical Analysis
Data were analyzed using SPSS for Windows, Version 21.0 (SPSS Inc., Chicago, IL, USA). Continuous variables were compared using two-tailed Students' t-test and categorical data were compared using the Chi square test. To evaluate the time to tumor recurrence and compare the survivals between groups, Kaplan-Meier survival curves and the log-rank test were used. Multivariate survival analyses using a Cox's proportional hazard model were performed to characterize the prognostic factors in PT. A two-tailed p value < 0.05 was considered statistically significant.
3. Results
3.1. Basal Characteristics of Phyllodes Tumors
This study included 194 cases of breast PT, including 151 cases of benign PT, 27 cases of borderline PT, and 16 cases of malignant PT. The basal characteristics of the patients are shown in Table 2. Greater patient age and larger tumor size were associated with higher PT histologic grade (p = 0.017 and p = 0.001, resp.). Higher rate of tumor recurrence and distant metastasis were also associated with higher PT histologic grade (p < 0.001). Eight cases with distant metastasis showed lung metastasis.
Table 2.
Clinicopathologic characteristics of patients with phyllodes tumor.
| Parameters | Total n = 196 (100%) | PT, benign n = 153 (100%) | PT, borderline n = 27 (100%) | PT, malignant n = 16 (100%) | p value |
|---|---|---|---|---|---|
| Age (years, mean ± SD) | 40.1 ± 12.3 | 38.9 ± 12.2 | 42.3 ± 11.5 | 47.6 ± 12.9 | 0.017 |
| Tumor size (cm, mean ± SD) | 4.0 ± 2.6 | 3.6 ± 2.1 | 4.3 ± 2.5 | 6.7 ± 4.6 | <0.001 |
| Stromal cellularity | <0.001 | ||||
| Mild | 121 (61.7) | 120 (78.4) | 1 (3.7) | 0 (0.0) | |
| Moderate | 63 (32.1) | 33 (21.6) | 23 (85.2) | 7 (43.8) | |
| Marked | 12 (6.1) | 0 (0.0) | 3 (11.1) | 9 (56.2) | |
| Stromal atypia | <0.001 | ||||
| Mild | 156 (79.6) | 151 (98.7) | 5 (18.5) | 0 (0.0) | |
| Moderate | 30 (15.3) | 2 (1.3) | 20 (74.1) | 8 (50.0) | |
| Marked | 10 (5.1) | 0 (0.0) | 2 (7.4) | 8 (50.0) | |
| Stromal mitosis | <0.001 | ||||
| 0–4/10 HPFs | 154 (78.6) | 153 (100.0) | 1 (3.7) | 0 (0.0) | |
| 5–9/10 HPFs | 31 (15.8) | 0 (0.0) | 26 (96.3) | 5 (31.2) | |
| ≥10/10 HPFs | 11 (5.6) | 0 (0.0) | 0 (0.0) | 11 (68.8) | |
| Stromal overgrowth | <0.001 | ||||
| Absent | 179 (91.3) | 153 (100.0) | 24 (88.9) | 2 (12.5) | |
| Present | 17 (8.7) | 0 (0.0) | 3 (11.1) | 14 (87.5) | |
| Tumor margin | <0.001 | ||||
| Circumscribed | 176 (89.8) | 150 (98.0) | 20 (74.1) | 6 (89.7) | |
| Infiltrative | 20 (10.2) | 3 (2.0) | 7 (25.9) | 10 (62.5) | |
| Tumor recurrence | 18 (9.2) | 5 (3.3) | 6 (22.2) | 7 (43.8) | <0.001 |
| Distant metastasis | 8 (4.1) | 0 (0.0) | 1 (3.7) | 7 (43.8) | <0.001 |
PT, phyllodes tumor; HPF, high-power fields.
3.2. Expression of CAF-Related Proteins according to Phyllodes Tumor Histologic Grade
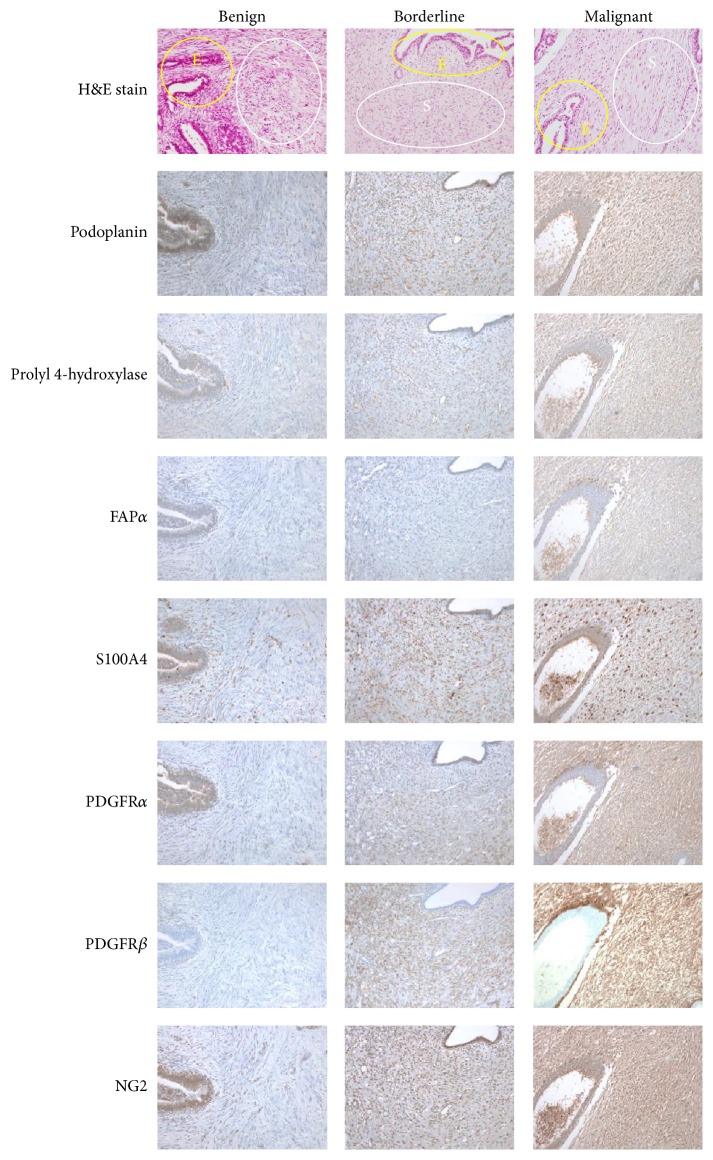
There were no significant differences in immunohistochemical staining in the epithelial component according to PT histologic grade for any of the proteins analyzed (Table 3). For the stromal component, the expression of PDGFRα and PDGFRβ increased with increasing PT histologic grade (p = 0.003 and p = 0.034, resp.) (Table 4 and Figure 1).
Table 3.
Expression of CAF-related proteins in epithelial component of phyllodes tumor according to histologic grade∗.
| Parameters | Total n = 179 (100%) | PT, benign n = 151 (100%) | PT, borderline n = 23 (100%) | PT, malignant n = 5 (100%) | p value |
|---|---|---|---|---|---|
| Podoplanin | 0.329 | ||||
| Negative | 35 (19.6) | 27 (17.9) | 6 (26.1) | 2 (40.0) | |
| Positive | 144 (80.4) | 124 (82.1) | 17 (73.9) | 3 (60.0) | |
| Prolyl 4-hydroxylase | 0.621 | ||||
| Negative | 174 (97.2) | 146 (96.7) | 23 (100.0) | 5 (100.0) | |
| Positive | 5 (2.8) | 5 (3.3) | 0 (0.0) | 0 (0.0) | |
| FAPα | 0.794 | ||||
| Negative | 166 (92.7) | 140 (92.7) | 21 (91.3) | 5 (100.0) | |
| Positive | 13 (7.3) | 11 (7.3) | 2 (8.7) | 0 (0.0) | |
| S100A4 | 0.571 | ||||
| Negative | 93 (52.0) | 81 (53.6) | 10 (43.5) | 2 (40.0) | |
| Positive | 86 (48.0) | 70 (46.4) | 13 (56.5) | 3 (60.0) | |
| PDGFRα | 0.738 | ||||
| Negative | 145 (81.0) | 121 (80.1) | 20 (87.0) | 4 (80.0) | |
| Positive | 34 (19.0) | 30 (19.9) | 3 (13.0) | 1 (20.0) | |
| PDGFRβ | N/A | ||||
| Negative | 179 (100.0) | 151 (100.0) | 23 (100.0) | 5 (100.0) | |
| Positive | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| NG2 | 0.216 | ||||
| Negative | 60 (33.5) | 52 (34.4) | 5 (21.7) | 3 (60.0) | |
| Positive | 119 (66.5) | 99 (65.6) | 18 (78.3) | 2 (40.0) |
∗Seventeen tumors without an epithelial component were excluded.
PT, phyllodes tumor.
Table 4.
Expression of CAF-related proteins in the stromal component of phyllodes tumor according to histologic grade.
| Parameters | Total n = 196 (100%) | PT, benign n = 153 (100%) | PT, borderline n = 27 (100%) | PT, malignant n = 16 (100%) | p value |
|---|---|---|---|---|---|
| Podoplanin | 0.728 | ||||
| Negative | 52 (26.5) | 41 (26.8) | 8 (29.6) | 3 (18.8) | |
| Positive | 144 (73.5) | 112 (73.2) | 19 (70.4) | 13 (81.2) | |
| Prolyl 4-hydroxylase | 0.563 | ||||
| Negative | 192 (98.0) | 149 (97.4) | 27 (100.0) | 16 (100.0) | |
| Positive | 4 (2.0) | 4 (2.6) | 0 (0.0) | 0 (0.0) | |
| FAPα | 0.105 | ||||
| Negative | 188 (95.9) | 149 (97.4) | 25 (92.6) | 14 (87.5) | |
| Positive | 8 (4.1) | 4 (2.6) | 2 (7.4) | 2 (12.5) | |
| S100A4 | 0.104 | ||||
| Negative | 65 (33.2) | 56 (36.6) | 7 (25.9) | 2 (12.5) | |
| Positive | 131 (66.8) | 97 (63.4) | 20 (74.1) | 14 (87.5) | |
| PDGFRα | 0.003 | ||||
| Negative | 179 (91.3) | 142 (92.8) | 26 (96.3) | 11 (68.8) | |
| Positive | 17 (8.7) | 11 (7.2) | 1 (3.7) | 5 (31.2) | |
| PDGFRβ | 0.034 | ||||
| Negative | 80 (40.8) | 69 (45.1) | 5 (18.5) | 6 (37.5) | |
| Positive | 116 (59.2) | 84 (54.9) | 22 (81.5) | 10 (62.5) | |
| NG2 | 0.695 | ||||
| Negative | 93 (47.4) | 75 (49.0) | 11 (40.7) | 7 (43.8) | |
| Positive | 103 (52.6) | 78 (51.0) | 16 (59.3) | 9 (56.2) |
PT, phyllodes tumor.
Figure 1.
Expression of CAF-related proteins according to the histologic grade of phyllodes tumor. The stromal expression of PDGFRα and β increased with increasing phyllodes tumor histologic grade. The yellow circle indicates epithelium and the white circle indicates the stroma. CAF, cancer-associated fibroblast; H&E, hematoxylin and eosin stain; FAP, fibroblast activation protein; PDGFR, platelet-derived growth factor receptor; NG2, chondroitin sulfate proteoglycan.
3.3. Correlation between the Expression of CAF-Related Proteins in Phyllodes Tumor and Clinicopathologic Parameters
We investigated the correlation between the expression of CAF-related proteins in PT and clinicopathologic parameters. Only expression of FAPα in the stromal cells was associated with distant metastasis (p = 0.002) (Figure 2). Other clinicopathologic parameters, including age, tumor size, stromal cellularity, stromal atypia, stromal mitosis, stromal overgrowth, tumor margin, and tumor recurrence, were not associated with the expression of CAF-related proteins in PT.
Figure 2.
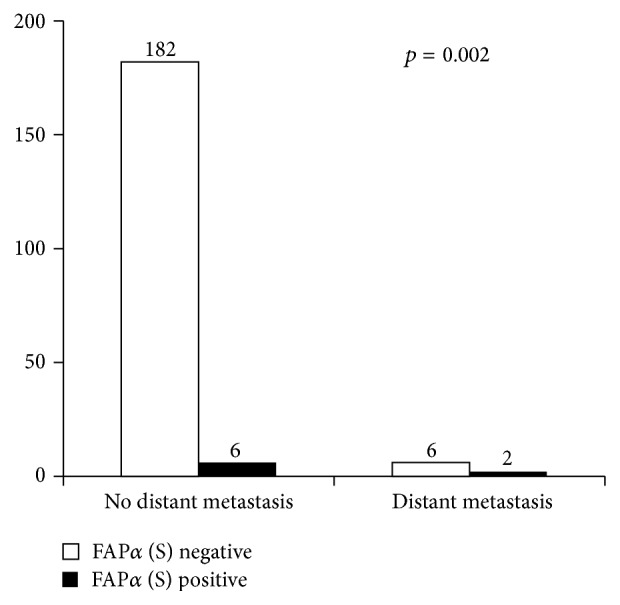
Correlation between stromal expression of fibroblast activation protein (FAP)α in phyllodes tumor and distant metastasis.
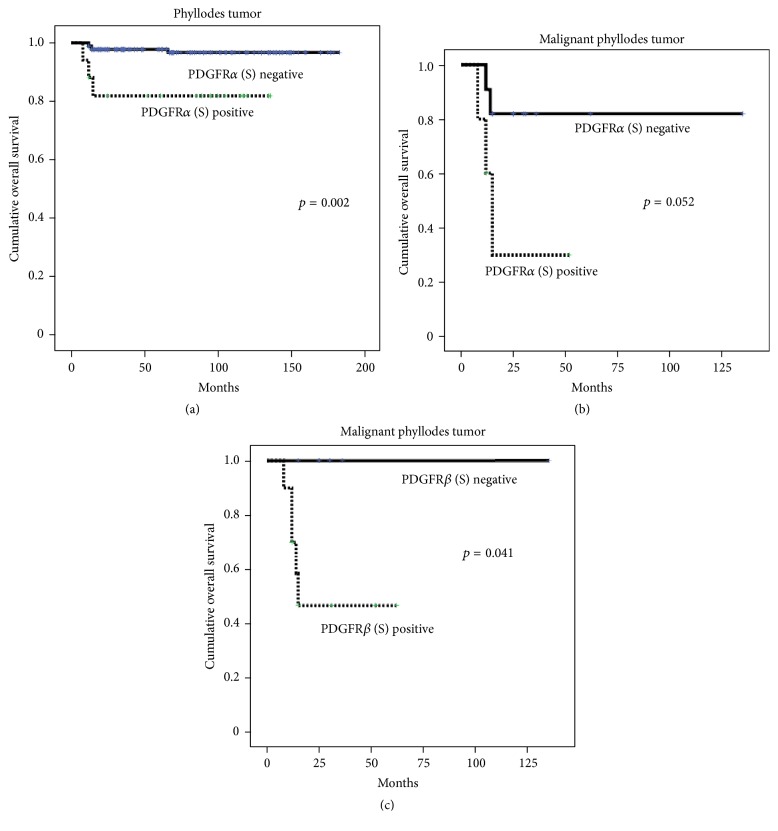
3.4. Impact of Expression of CAF-Related Proteins on Patient Prognosis
Univariate analysis showed that stromal expression of PDGFRα was associated with shorter overall survival (p = 0.002) (Table 5 and Figure 3(a)). Furthermore, in Cox multivariate analysis, higher PT histologic grade (hazard ratio: 7.990, 95% CI: 2.196–29.07, and p = 0.002) and stromal overgrowth (hazard ratio: 7.288, 95% CI: 1.225–43.35, and p = 0.029) were associated with shorter disease-free survival. Regarding overall survival, stromal overgrowth (hazard ratio: 58.10, 95% CI: 3.116–1083, and p = 0.006) and PDGFRα positivity (hazard ratio: 5.486, 95% CI: 1.003–30.01, and p = 0.050) were associated with shorter overall survival (Table 6). Furthermore, stromal expression of PDGFRα (p = 0.052) (Figure 3(b)) and PDGFRβ (p = 0.041) (Figure 3(c)) was associated with shorter overall survival in malignant PT, although statistical significance was not reached regarding PDGFRα expression.
Table 5.
Univariate analysis of the impact of CAF-related proteins in the stromal component of phyllodes tumor on patient prognosis using the log-rank test.
| Parameters | Number of patients Total/recurrence/metastasis | Disease-free survival | Overall survival | ||
|---|---|---|---|---|---|
| Median survival (95% CI) months | p value | Median survival (95% CI) months | p value | ||
| Podoplanin | 0.936 | 0.494 | |||
| Negative | 52/5/3 | 160 (146–174) | 166 (155–178) | ||
| Positive | 144/13/5 | 166 (158–175) | 177 (171–182) | ||
| Prolyl 4-hydroxylase | n/a | n/a | |||
| Negative | 192/18/8 | n/a | n/a | ||
| Positive | 4/0/0 | n/a | n/a | ||
| FAPα | 0.099 | 0.233 | |||
| Negative | 188/16/7 | 164 (157–171) | 172 (167–177) | ||
| Positive | 8/2/1 | 131 (71–191) | 162 (123–200) | ||
| S100A4 | 0.607 | 0.792 | |||
| Negative | 65/5/3 | 163 (152–174) | 168 (159–177) | ||
| Positive | 131/13/5 | 165 (155–174) | 176 (170–182) | ||
| PDGFRα | 0.698 | 0.002 | |||
| Negative | 179/16/5 | 167 (159–174) | 177 (173–182) | ||
| Positive | 17/2/3 | 121 (102–140) | 113 (90–136) | ||
| PDGFRβ | 0.394 | 0.087 | |||
| Negative | 80/6/1 | 164 (154–174) | 174 (170–178) | ||
| Positive | 116/12/7 | 163 (153–173) | 172 (164–179) | ||
| NG2 | 0.830 | 0.216 | |||
| Negative | 93/8/2 | 145 (136–154) | 155 (151–160) | ||
| Positive | 103/10/6 | 165 (155–175) | 172 (164–180) | ||
Figure 3.
Overall survival curves according to the status of CAF-related proteins in stromal component of phyllodes tumor. (a) Univariate analysis showed that stromal expression of PDGFRα was associated with shorter overall survival in phyllodes tumor. (b) Stromal expression of PDGFRα was associated with shorter overall survival in malignant phyllodes tumor, although statistical significance was not reached regarding PDGFRα expression. (c) Stromal expression of PDGFRβ was associated with shorter overall survival in malignant phyllodes tumor. CAF, cancer-associated fibroblast; PDGFR, platelet-derived growth factor receptor.
Table 6.
Multivariate analysis of disease-free and overall survival in patients with phyllodes tumors.
| Included factor | Disease-free survival | Overall survival | ||||
|---|---|---|---|---|---|---|
| Hazard ratio | 95% CI | p value | Hazard ratio | 95% CI | p value | |
| Histologic grade | 0.002 | N/A | ||||
| Benign versus borderline/malignant | 7.990 | 2.196–29.07 | N/A | N/A | ||
| Stromal cellularity | 0.597 | 0.467 | ||||
| Mild versus moderate/marked | 0.625 | 0.109–3.569 | 2.862 | 0.169–48.60 | ||
| Stromal atypia | 0.886 | 0.708 | ||||
| Mild versus moderate/marked | 0.881 | 0.158–4.925 | 0.630 | 0.056–7.049 | ||
| Stromal mitosis | 0.854 | 0.437 | ||||
| 0–4/10 HPF versus >4/10 HPF | 0.782 | 0.057–10.81 | 0.210 | 0.004–10.70 | ||
| Stromal overgrowth | 0.029 | 0.006 | ||||
| Absent versus present | 7.288 | 1.225–43.35 | 58.10 | 3.116–1083 | ||
| Tumor margin | 0.275 | 0.187 | ||||
| Circumscribed versus infiltrative | 0.468 | 0.120–1.830 | 0.321 | 0.060–1.732 | ||
| PDGFRα (stromal) | 0.867 | 0.050 | ||||
| Negative versus positive | 0.879 | 0.193–4.008 | 5.486 | 1.003–30.01 | ||
HPF, high-power field.
4. Discussion
In this study, we investigated the expression of CAF-related proteins in breast PT according to histologic grade with the aim of identifying a new therapeutic target for PT.
Recently, there have been many studies on the tumor microenvironment as a novel therapeutic target. The tumor microenvironment includes nontumor cells with nontransformed elements, including immune system elements (such as macrophages and lymphocytes), blood vessel cells, fibroblasts, myofibroblasts, mesenchymal stem cells, adipocytes, and extracellular matrix, in close proximity to tumor cells. PT is a representative fibroepithelial tumor characterized by fibrous stroma composed of fibroblasts surrounding the epithelium. Previous studies reported that CD34-expressing fibroblasts exist in mammary stroma. Because CD34-expressing fibroblasts were observed in both fibroadenoma and PT [19], efficient treatment for fibroepithelial tumors might be achieved by targeting the fibrous stroma. However, there are no studies on the expression of CAF-related proteins in PT, and as PT shows heterogeneous tumor stromal features, the expression of CAF-related proteins is predicted to vary in each type.
In this study, we performed immunohistochemical staining for CAF-related proteins focusing on the stromal component. Our results showed that the expression of PDGFRα and PDGFRβ increased with increasing PT histologic grade. Platelet-derived growth factor is a major mitogen for several cell types, including connective tissue cells, that is activated by binding to two protein tyrosine kinase receptors (PDGFRα and PDGFRβ). PDGF signaling in tumor cells induces point mutations, amplification, and translocations, which stimulate autocrine stimulatory loops [6, 21]. For example, PDGFRα and β are two well-known receptors that participate in breast cancer progression [22]. In addition, in breast cancer, the desmoplastic response appears to be mediated by PDGF-AA signaling in PDGFRα type CAFs [23]. Desmoplasia refers to the growth of fibrous or connective tissue near the tumor and is increased in tumors with aggressive properties. The results from our study revealed that higher grade PT with more active fibroblasts showed higher expression of PDGFRα and β, suggesting that fibroblasts with a CAF phenotype are associated with PT progression.
Stromal PDGFRα expression was related to the prognosis of patients with PT. Furthermore, subgroup analysis in malignant PT showed that stromal PDGFRβ expression was associated with shorter overall survival and, although statistical significance was not noted, there was also a trend for increased stromal PDGFRα expression. In previous studies of glioma [24], squamous cell carcinoma of the head and neck [25], colorectal cancer [26], pancreatic cancer [27], and T cell lymphoma [28], PDGFR activation induced the intracellular signaling pathway and promoted cell migration, invasion, survival, and proliferation [29]. Similarly, PDGFR activation is related to lymphatic metastasis in pancreatic cancer [30] and gastric cancer [31], suggesting that PDGFR might be used as a prognostic marker in malignant PT. This should be validated in future studies.
We found that expression of FAPα in stroma was associated with distant metastasis. Fibroblast activation protein is expressed by reactive CAFs in tumor stroma or granulation tissue and is known to be involved in wound healing. The expression of FAP in CAFs is reported in various carcinomas and is used as an important marker of CAF [32, 33]. In a meta-analysis that analyzed the clinical implication of FAP overexpression in solid tumors of colorectal cancer, pancreatic adenocarcinoma, non-small cell lung cancer, breast cancer, medullary thyroid carcinoma, and oral squamous cell carcinoma, high FAP expression was related to the risk of distant metastasis (OR: 2.56) [34], showing similar results to our study. FAP regulates proteolysis of the extracellular cell matrix in tumor stroma, causing stromal cell proliferation and invasiveness. Therefore, it could be speculated that tumors with high expression of FAPα are prone to metastasis to distant organs [35, 36].
The clinical significance of this study is the role of CAFs as a potential therapeutic target. Sunitinib, a US Food and Drug Administration- (FDA-) approved PDGFR inhibitor, is currently used in the treatment of advanced renal cell carcinoma [37], advanced progressive pancreatic neuroendocrine tumor [38], and advanced radioiodine refractory thyroid carcinoma [39]. Furthermore, ongoing preclinical trials are testing the therapeutic effect of another PDGFR inhibitor, imatinib mesylate, in gastrointestinal stromal tumor [40, 41] and in vitro and in vivo studies of malignant peripheral nerve sheath tumors have shown promising results [42]. Therefore, inhibition of PDGFR in PT might be a potential therapeutic strategy. However, further investigation regarding the effect of these inhibitors in PT is required.
Taken together, our data show that expression of PDGFRα and PDGFRβ in the stromal component increased with increased PT histologic grade. Also, stromal expression of PDGFR was associated with shorter overall survival. Overall, the expression of CAF-related proteins is related to the histologic grade of breast PT and PDGFR inhibitors in particular have potential as novel treatments for PT.
Acknowledgments
This study was supported by a grant from the National R&D Program for Cancer Control, Ministry of Health & Welfare, Republic of Korea (1420080). Additionally, it was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Science, ICT and Future Planning (2015R1A1A1A05001209).
Competing Interests
The authors declare that there is no conflict of interests regarding the publication of this paper.
References
- 1.Franco O. E., Shaw A. K., Strand D. W., Hayward S. W. Cancer associated fibroblasts in cancer pathogenesis. Seminars in Cell and Developmental Biology. 2010;21(1):33–39. doi: 10.1016/j.semcdb.2009.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Östman A. Cancer-associated fibroblasts: recent developments and emerging challenges. Seminars in Cancer Biology. 2014;25:1–2. doi: 10.1016/j.semcancer.2014.02.004. [DOI] [PubMed] [Google Scholar]
- 3.Desmoulière A., Guyot C., Gabbiani G. The stroma reaction myofibroblast: a key player in the control of tumor cell behavior. International Journal of Developmental Biology. 2004;48(5-6):509–517. doi: 10.1387/ijdb.041802ad. [DOI] [PubMed] [Google Scholar]
- 4.De Wever O., Nguyen Q.-D., Van Hoorde L., et al. Tenascin-C and SF/HGF produced by myofibroblasts in vitro provide convergent pro-invasive signals to human colon cancer cells through RhoA and Rac. FASEB Journal. 2004;18(9):1016–1018. doi: 10.1096/fj.03-1110fje. [DOI] [PubMed] [Google Scholar]
- 5.Sugimoto H., Mundel T. M., Kieran M. W., Kalluri R. Identification of fibroblast heterogeneity in the tumor microenvironment. Cancer Biology and Therapy. 2006;5(12):1640–1646. doi: 10.4161/cbt.5.12.3354. [DOI] [PubMed] [Google Scholar]
- 6.Pietras K., Sjöblom T., Rubin K., Heldin C.-H., Östman A. PDGF receptors as cancer drug targets. Cancer Cell. 2003;3(5):439–443. doi: 10.1016/S1535-6108(03)00089-8. [DOI] [PubMed] [Google Scholar]
- 7.Kraman M., Bambrough P. J., Arnold J. N., et al. Suppression of antitumor immunity by stromal cells expressing fibroblast activation protein-α . Science. 2010;330(6005):827–830. doi: 10.1126/science.1195300. [DOI] [PubMed] [Google Scholar]
- 8.Kawase A., Ishii G., Nagai K., et al. Podoplanin expression by cancer associated fibroblasts predicts poor prognosis of lung adenocarcinoma. International Journal of Cancer. 2008;123(5):1053–1059. doi: 10.1002/ijc.23611. [DOI] [PubMed] [Google Scholar]
- 9.Kojima Y., Acar A., Eaton E. N., et al. Autocrine TGF-β and stromal cell-derived factor-1 (SDF-1) signaling drives the evolution of tumor-promoting mammary stromal myofibroblasts. Proceedings of the National Academy of Sciences of the United States of America. 2010;107(46):20009–20014. doi: 10.1073/pnas.1013805107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cortez E., Roswall P., Pietras K. Functional subsets of mesenchymal cell types in the tumor microenvironment. Seminars in Cancer Biology. 2014;25:3–9. doi: 10.1016/j.semcancer.2013.12.010. [DOI] [PubMed] [Google Scholar]
- 11.Tavassoli F. A., Devilee P. World Heath Organization Classification of Tumors. Lyon, France: IARC Press; 2003. [Google Scholar]
- 12.Dacic S., Kounelis S., Kouri E., Jones M. W. Immunohistochemical profile of cystosarcoma phyllodes of the breast: a study of 23 cases. Breast Journal. 2002;8(6):376–381. doi: 10.1046/j.1524-4741.2002.08608.x. [DOI] [PubMed] [Google Scholar]
- 13.Anderson B., Lawton T., Lehman C., Moe R. Phyllodes tumor. In: Morrow M., Osborne C., editors. Disease of the Breast. Philadelphia: Lippincott Williams & Wilkins; 2004. pp. 991–1006. [Google Scholar]
- 14.Ben hassouna J., Damak T., Gamoudi A., et al. Phyllodes tumors of the breast: a case series of 106 patients. American Journal of Surgery. 2006;192(2):141–147. doi: 10.1016/j.amjsurg.2006.04.007. [DOI] [PubMed] [Google Scholar]
- 15.Mitus J., Reinfuss M., Mitus J. W., et al. Malignant phyllodes tumor of the breast: treatment and prognosis. Breast Journal. 2014;20(6):639–644. doi: 10.1111/tbj.12333. [DOI] [PubMed] [Google Scholar]
- 16.Tan P.-H., Jayabaskar T., Chuah K.-L., et al. Phyllodes tumors of the breast: the role of pathologic parameters. American Journal of Clinical Pathology. 2005;123(4):529–540. doi: 10.1309/u6dv-bfm8-1mlj-c1fn. [DOI] [PubMed] [Google Scholar]
- 17.Barrio A. V., Clark B. D., Goldberg J. I., et al. Clinicopathologic features and long-term outcomes of 293 phyllodes tumors of the breast. Annals of Surgical Oncology. 2007;14(10):2961–2970. doi: 10.1245/s10434-007-9439-z. [DOI] [PubMed] [Google Scholar]
- 18.Aranda F. I., Laforga J. B., Lopez J. I. Phyllodes tumor of the breast. An immunohistochemical study of 28 cases with special attention to the role of myofibroblasts. Pathology Research and Practice. 1994;190(5):474–481. doi: 10.1016/S0344-0338(11)80210-4. [DOI] [PubMed] [Google Scholar]
- 19.Silverman J. S., Tamsen A. Mammary fibroadenoma and some phyllodes tumour stroma are composed of CD34+ fibroblasts and factor XIIIa+ dendrophages. Histopathology. 1996;29(5):411–419. doi: 10.1046/j.1365-2559.1996.d01-510.x. [DOI] [PubMed] [Google Scholar]
- 20.Won K. Y., Kim G. Y., Kim Y. W., Song J. Y., Lim S.-J. Clinicopathologic correlation of beclin-1 and bcl-2 expression in human breast cancer. Human Pathology. 2010;41(1):107–112. doi: 10.1016/j.humpath.2009.07.006. [DOI] [PubMed] [Google Scholar]
- 21.Andrae J., Gallini R., Betsholtz C. Role of platelet-derived growth factors in physiology and medicine. Genes and Development. 2008;22(10):1276–1312. doi: 10.1101/gad.1653708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Meng F., Speyer C. L., Zhang B., et al. PDGFRα and β play critical roles in mediating Foxq1-driven breast cancer stemness and chemoresistance. Cancer Research. 2015;75(3):584–593. doi: 10.1158/0008-5472.can-13-3029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shao Z.-M., Nguyen M., Barsky S. H. Human breast carcinoma desmoplasia is PDGF initiated. Oncogene. 2000;19(38):4337–4345. doi: 10.1038/sj.onc.1203785. [DOI] [PubMed] [Google Scholar]
- 24.Nazarenko I., Hede S.-M., He X., et al. PDGF and PDGF receptors in glioma. Upsala Journal of Medical Sciences. 2012;117(2):99–112. doi: 10.3109/03009734.2012.665097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schultz J. D., Rotunno S., Riedel F., et al. Synergistic effects of imatinib and carboplatin on VEGF, PDGF and PDGF-Rα/β expression in squamous cell carcinoma of the head and neck in vitro. International Journal of Oncology. 2011;38(4):1001–1012. doi: 10.3892/ijo.2011.912. [DOI] [PubMed] [Google Scholar]
- 26.Steller E. J. A., Raats D. A., Koster J., et al. PDGFRB promotes liver metastasis formation of mesenchymal-like colorectal tumor cells. Neoplasia (United States) 2013;15(2):204–217. doi: 10.1593/neo.121726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kurahara H., Maemura K., Mataki Y., Sakoda M., Shinchi H., Natsugoe S. Impact of p53 and PDGFR-β expression on metastasis and prognosis of patients with pancreatic cancer. World Journal of Surgery. 2016;40(8):1977–1984. doi: 10.1007/s00268-016-3477-2. [DOI] [PubMed] [Google Scholar]
- 28.Piccaluga P. P., Rossi M., Agostinelli C., et al. Platelet-derived growth factor alpha mediates the proliferation of peripheral T-cell lymphoma cells via an autocrine regulatory pathway. Leukemia. 2014;28(8):1687–1697. doi: 10.1038/leu.2014.50. [DOI] [PubMed] [Google Scholar]
- 29.Heldin C.-H., Westermark B. Mechanism of action and in vivo role of platelet-derived growth factor. Physiological Reviews. 1999;79(4):1283–1316. doi: 10.1152/physrev.1999.79.4.1283. [DOI] [PubMed] [Google Scholar]
- 30.Weissmueller S., Manchado E., Saborowski M., et al. Mutant p53 drives pancreatic cancer metastasis through cell-autonomous PDGF receptor β signaling. Cell. 2014;157(2):382–394. doi: 10.1016/j.cell.2014.01.066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kodama M., Kitadai Y., Sumida T., et al. Expression of platelet-derived growth factor (PDGF)-B and PDGF-receptor β is associated with lymphatic metastasis in human gastric carcinoma. Cancer Science. 2010;101(9):1984–1989. doi: 10.1111/j.1349-7006.2010.01639.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Meng M., Wang W., Yan J., et al. Immunization of stromal cell targeting fibroblast activation protein providing immunotherapy to breast cancer mouse model. Tumor Biology. 2016;37(8):10317–10327. doi: 10.1007/s13277-016-4825-4. [DOI] [PubMed] [Google Scholar]
- 33.Wang H., Wu Q., Liu Z., et al. Downregulation of FAP suppresses cell proliferation and metastasis through PTEN/PI3K/AKT and Ras-ERK signaling in oral squamous cell carcinoma. Cell Death and Disease. 2014;5(4) doi: 10.1038/cddis.2014.122.e1155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Liu F., Qi L., Liu B., et al. Fibroblast activation protein overexpression and clinical implications in solid tumors: a meta-analysis. PLoS ONE. 2015;10(3) doi: 10.1371/journal.pone.0116683.e0116683 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Yuan D., Liu B., Liu K., Zhu G., Dai Z., Xie Y. Overexpression of fibroblast activation protein and its clinical implications in patients with osteosarcoma. Journal of Surgical Oncology. 2013;108(3):157–162. doi: 10.1002/jso.23368. [DOI] [PubMed] [Google Scholar]
- 36.Goscinski M. A., Suo Z., Flørenes V. A., Vlatkovic L., Nesland J. M., Giercksky K.-E. FAP-α and uPA show different expression patterns in premalignant and malignant esophageal lesions. Ultrastructural Pathology. 2008;32(3):89–96. doi: 10.1080/01913120802034934. [DOI] [PubMed] [Google Scholar]
- 37.Coelho R. C., Reinert T., Campos F., et al. Sunitinib treatment in patients with advanced renal cell cancer: the Brazilian National Cancer Institute (INCA) experience. International Brazilian Journal of Urology. 2016;42(4):694–703. doi: 10.1590/s1677-5538.ibju.2015.0226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Efficiency of sunitinib in Chinese patients with advanced progressive pancreatic neuroendocrine tumor. Zhongguo Yi Xue Ke Xue Yuan Xue Bao. 2016;38(3):300–304. doi: 10.3881/j.issn.1000-503X.2016.03.010. [DOI] [PubMed] [Google Scholar]
- 39.Atallah V., Hocquelet A., Do Cao C., et al. Activity and safety of sunitinib in patients with advanced radioiodine refractory thyroid carcinoma: a retrospective analysis of 57 patients. Thyroid. 2016;26(8):1085–1092. doi: 10.1089/thy.2015.0648. [DOI] [PubMed] [Google Scholar]
- 40.Moawad E. Y. Predicting effectiveness of imatinib mesylate in tumors expressing platelet-derived growth factors (PDGF-AA, PDGF-BB), stem cell factor ligands and their respective receptors (PDGFR-α, PDGFR-β, and c-kit) Journal of Gastrointestinal Cancer. 2015;46(3):272–283. doi: 10.1007/s12029-015-9721-4. [DOI] [PubMed] [Google Scholar]
- 41.Hayashi Y., Bardsley M. R., Toyomasu Y., et al. Platelet-derived growth factor receptor-α regulates proliferation of gastrointestinal stromal tumor cells with mutations in KIT by stabilizing ETV1. Gastroenterology. 2015;149(2):420–432.e16. doi: 10.1053/j.gastro.2015.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ohishi J., Aoki M., Nabeshima K., et al. Imatinib mesylate inhibits cell growth of malignant peripheral nerve sheath tumors in vitro and in vivo through suppression of PDGFR-β . BMC Cancer. 2013;13, article 224 doi: 10.1186/1471-2407-13-224. [DOI] [PMC free article] [PubMed] [Google Scholar]