Abstract
Asian skin has a higher epidermal melanin content, making it more likely to develop adverse pigmentary reactions following laser surgery. The nanosecond lasers are the gold standard for the treatment of pigmented lesions, but the risk of complications, such as post-inflammatory hyperpigmentation, is increased in dark-skinned patients. Intense Pulsed Light (IPL) or long-pulsed lasers are available for treating superficial pigmented lesions, and fewer complications are seen when using these devices compared to the nanosecond lasers. Nanosecond lasers are essential in the treatment of dermal melanosis. Recently, picosecond lasers have been investigated. Picosecond lasers will also play an important role in the treatment of pigmented lesions.
Keywords: long-pulsed laser, Q-switched laser, nanosecond laser, picosecond laser, pigmented lesions, complications, Asians
Introduction
Since the introduction of selective photothermolysis, short pulse lasers such as Q-switched lasers (nanosecond lasers) have been used for the treatment of pigmented lesions 1). Laser surgery for Asians differs from that for Caucasians in several important aspects 2). Asian patients with photodamage tend to present with dyspigmentation rather than wrinkling. Asian skin, with its higher epidermal melanin content, tends to develop adverse pigmentary reactions following laser surgery 3, 4). The risk of complications such as erythema, blistering, hypopigmentation and post-inflammatory hyperpigmentation are more common in Asian skin. Some conditions, such as Mongolian spots and nevus of Ota, are more commonly seen in Asians.
Superficial pigmented lesions
The use of nanosecond lasers for the treatment of pigmented lesions is based on the principle of selective photothermolysis of melanosomes. In general, the optimal pulse duration for selective photothermolysis is approximately equal to the thermal relaxation time of the intended target structure. For lesions in which pigmented target cells are dispersed singly, such as nevus of Ota, the nanosecond pulse durations appear to be optimal. In common lentigines, abnormal pigmentation exists throughout the basal cell layer of epidermis. Tissue destruction caused by long-pulsed lasers is pure photothermolysis. Nanosecond lasers exhibit both photothermal and photomechanical effects. While very short pulses may cause unwanted mechanical damage, the main concern regarding long-pulsed lasers when treating lentigines is the potential for thermal diffusion from the epidermis to the dermis, which may increase the risk of dermal injury and subsequent scar formation. To prevent this, the pulse duration of the laser should be about equal to or shorter than the thermal relaxation time of the epidermis basal layer. For a basal layer thickness of 20 um, the thermal relaxation time is estimated to be in the range of 1.6–2.8 milliseconds (Figure 1).
Figure 1:
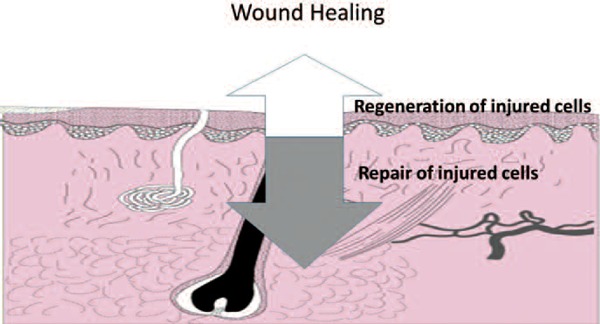
Superficial epidermal injury only involves the epidermis. Wound healing occurs by regeneration of the epidermis from the basal layer. Since the thermal relaxation time of the basal layer is 1.6–2.8 msec, millisecond, microsecond, nanosecond and picosecond lasers are available. On the other hand, dermal wound is repaired with collagen and extracellular matrix. Long-pulsed lasers have a risk of scarring. Short pulse (nanosecond and picosecond) lasers are essential.
A study looking at the use of a Q-switched ruby (QS ruby) laser for the treatment of cutaneous pigmented lesions in Chinese patients reported a rate of post inflammatory hyperpigmentation (PIH) of about 25% 3). We compared the use of different types of 532 nm neodymium: yttrium-aluminum-garnet (Nd:YAG) lasers in the treatment of lentigines in Asians. This study showed the same efficacy between the long-pulsed 532 nm lasers and the nanosecond lasers, but the study also showed a significantly higher risk of hyperpigmentation when patients were treated with the nanosecond 532 nm lasers 5). To balance cost-effectiveness and clinical outcomes, one approach is to treat several test areas with different laser devices. For nanosecond lasers, the clinical endpoint is defined as the lowest fluence that can achieve immediate whitening. For long pulsed lasers, the clinical endpoint is defined as slate grey appearance. If the outcome is satisfactory, the patient is advised to continue treatment with the same laser, which can achieve excellent results after 1 to 2 full treatments. If, on the other hand, PIH develops at the test sites, intense pulsed light treatment may be substituted for the laser. In our experience, although IPL requires more sessions to achieve a desirable result, it is associated with a lower risk of post-inflammatory hyperpigmentation. Ho et.al reported a comparison study of Q-switched and long-pulsed alexandrite laser for the treatment of freckles and lentigines in Oriental Patients 6). In this study, there was statistically significant improvement in pigmentation in both groups, with no statistical difference in efficacy found between the groups. PIH was more frequently found after nanosecond laser treatment (22%), compared to long-pulsed laser treatment (6%). The author's concluded that long-pulsed alexandrite laser is quick and effective, and carries a lower risk of adverse effects when compared to the nanosecond alexandrite laser for the removal of freckles and lentigines in darker skin types (Figure 2).
Figure 2:

A: 70 year old female patient with solar lentigines. Left: Before treatment (Antera 3D TM Miravex : color image mode) Right: After 755 nm Alexandrite laser (TriVantage TM by Syneron/Candela Corporation) using the 100 microsecond (Antera 3D TM Miravex: color image mode).
B: Left: Before treatment (Antera 3D TM Miravex: melanin mode) Right: After treatment (Antera 3D TM Miravex: melanin mode)
Frequency doubled Nd:YAG (532 nm) and pulsed dye lasers (577–600 nm, PDL) are well known as vascular lasers. Their wavelengths are absorbed not only by hemoglobin, but also by melanin. It is well known that pressure “diascopy” eliminates blood from cutaneous vessels by coapting the vessel lumen. Removal of blood removes laser absorption by hemoglobin, making it possible to use the pulsed dye laser for treating lentigines without purpura. Purpura is indicative of vascular injury. Using the compression method, Nd:YAG (532 nm) and PDL (577–600 nm) may be used for treating pigmented lesions. We used pressure applied by a flat glass window on the PDL handpiece to remove cutaneous blood during laser exposure 8). This study showed that long (millisecond) pulses can provide effective and safe treatment of lentigines. Furthermore, it shows that the PDL, commonly used for treating vascular lesions, is easily modified for the treatment of lentigines by using our compression technique.
The end-point of long-pulsed lasers is ashen grey appearance (Figure 3). The undesirable photomechanical effects of nanosecond laser-tissue interactions lead to damage of surrounding tissue, resulting in post-inflammatory hyperpigmentation. In the treatment of superficial pigmented lesions in Asians, long-pulsed lasers and IPLs are the best treatment options, as they have less side effects and complications when compared to the nanosecond lasers.
Figure 3:

Laser-tissue interaction: the irradiance and exposure durations.
Intradermal pigmented lesions
The diameter of tattoo particles (20–200 nm) is smaller than that of melanosomes. Ideally the pulse width should be shorter than the thermal relaxation time of the intended target. Nanosecond lasers have pulse durations which are not short enough to accomplish the most efficient tattoo removal. With nanosecond lasers, complications are common, such as hyper- or hypopigmentation, textural changes, and even scarring 11, 12). Patients with darker skin types are at a higher risk of complications in tattoo removal using nanosecond lasers. In 1998, Ross et al. reported the use of nanosecond and picosecond lasers for the treatment of tattoos, and he found that the picosecond laser was more effective than the nanosecond laser 13). This is the first report using a picosecond laser to treat tattoos in human. The paper compares 35ps and 10ns laser pulses from two Nd:YAG laser systems. Other than the difference in pulse duration, sixteen tattoos were treated with identical treatment parameters. The study reported that 12 of the 16 tattoos were significantly lighter when treated once with the picosecond laser, when compared to the nanosecond laser. This paper showed that shorter pulses are more effective in clearing tattoos if all other parameters are kept constant. Brauer reported ten subjects with multi-color decorative tattoos that were treated with sub-nanosecond laser pulses (0.75 – 0.9 ns) operating at 755 nm 14). Spot sizes ranged from 3.0 to 3.6 mm producing fluences between 2.0 and 2.83 J/cm2. The laser operated at a fixed energy of 0.2 J per pulse. Of particular note in this study is a rapid clearance of blue and green inks, typically taking one or two treatments to clear. Purple inks had greater than 75% clearance after one or two treatments. The remaining colors, including the most prevalent black ink, showed 25% clearance or less after one or two treatments. Alabdulrazzaq reported the first commercially available 532 nm picosecond laser for tattoo removal. In this study, six subjects with multi-color decorative tattoos were treated with sub-nanosecond laser pulses (0.75 – 0.9 ns) operating at 532 nm 15). Energy densities ranged from 1.1 to 1.4 J/cm2 with a range of spot sized from 2.6 to 3.3 mm. The treatments were safe, with the most common side effects being edema, erythema, crusting, and pain. Of particular note in this study is a consistent reduction in yellow inks with all six subjects having greater than 75% clearance after 1 to 5 treatments. Milli-second and micro-second lasers induce a photo-thermal effect. Nano-second lasers induce both a photo-thermal and a photo-mechanical effect. Pico-second lasers mainly rely on a photo-mechanical effect. Although, the thermal relaxation time of tattoo particle is less than 1 nanosecond, selective photothermolysis is not the main mechanism used by picosecond lasers. Photomechanical (or Photoacoustic) fragmentation is responsible for destruction of tattoo ink. Picolasers have demonstrated better results than nanosecond lasers in many aspects (Figure 4 and 5). When treating tattoos, the wavelength is selected to maximize absorption by the tattoo chromophore. Multi-wavelength picolasers are essential for the successful treatment of multi-color tattoos. To date, no severe complications have been reported when using picosecond lasers.
Figure 4:

70 year old female patient with solar lentigines. Immediately after 755 nm Alexandrite laser (TriVantage TM by Syneron/Candela Corporation) treatment using the 100 microsecond. The end-point of long-pulsed laser is ashen grey appearance. The epidermis is easily peeled off using wet cotton stick (right half of the lesion).
Figure 5:

28 year old male patient with black tattoo.
A: The upper left was treated with the 532 nm picosecond, lower left with the 1064nm picosecond laser, upper right with the 532 nm nanosecond laser, lower right with the 1064 nm nanosecond laser: 532/1064 nm Nd:YAG laser (TriVantage TM by Candela Corporation) using the 50 ns and 532/1064 nm Nd:YAG laser (Picoway TM by Candela Corporation) using the 375/450 psec
B: Clearance of pigment after one treatment. Most significant reduction in areas treated with 1064 nm picosecond laser.
Nevus of Ota or nevus fuscocaeruleus opthalmomaxillaris is a dermal melanocytic hamartoma that presents as grey or bluish hyperpigmentation along the first and/or second branches of the trigeminal nerve. It affects between 0.014 to 0.034% of the Asian population. In contrast to superficial pigmented lesions, long-pulsed lasers are not a good option for treatment of intradermal pigmented lesions, such as nevus of Ota. Using this type of laser to treat an intradermal lesion can induce scar formation (Figure 1). The thermal relaxation time of a melanosome is 50 nanoseconds, therefore nanosecond lasers are essential. Goldberg and Nychayand Geronemus were among the first to report the use of nanosecond ruby lasers to treat nevus of Ota 16). Watanabe et al. reported a study of 114 nevus of Ota patients treated with a nanosecond ruby laser 17). They found that a good to excellent degree of lightening was achieved after three or more treatment sessions. Side effects were few, with transient hyperpigmentation seen in some patients. Nanosecond alexandrite lasers and nanosecond 1064 nm Nd:YAG lasers have also been used successfully for the removal of nevus of Ota. In terms of complications when treating with nanosecond lasers, hypopigmentation was common, especially among those treated with the nanosecond ruby 18–20). The alternating use of a nanosecond alexandrite and a nanosecond 1064 Nd:YAG in different treatment sessions was also associated with a higher risk of complications 21, 22). Nevus of Ota can recur in patients with experienced complete clearing after laser treatment. The risk of such recurrence is estimated to be between 0.6% and 1.2%. This is particularly important for children with nevus of Ota, as early treatment has been the standard practice. Early treatment, leading to complete clearance before school, can mean avoiding the childhood psychological trauma associated with the cosmetic disfigurement of the nevus. This advantage must now be weighed against the risk of recurrence and the stress associated with multiple sessions of laser surgery. Chesnut reported three subjects with recalcitrant Nevus of Ota that were treated successfully with a sub-nanosecond 755 nm laser having a pulse duration of 750 picosecond 23). All three subjects were skin type IV and had previous treatments with other laser systems with little response. Topical 7% lidocaine and 7% tetracaine was applied topically prior to treatment. One subject was treated twice at 2.08 J/cm2 with 8 weeks between treatments, and another patient had three treatments over a 6 month period, using a fluence of 2.8 J/cm2. The last subject had two treatments 6 weeks apart with a fluence of 2.1 J/cm2. Following treatment, all subjects showed significant lightening of their lesions with no significant adverse events reported. These results suggest that although the nanosecond lasers have pulse durations that are shorter than the thermal relaxation time of a dermal melanosome, further shortening of the laser pulse duration may improve the treatment response. Large prospective studies of non-treated Ota nevi patients are warranted.
Conclusions
Long-pulsed lasers can reduce the risk of complications in the treatment of superficial pigmented lesions in darker skin types. Nanosecond lasers are still the gold standard treatment in dermal pigmented lesions in Asians. Pico-lasers will play an important role not only tattoo removal, but also in the treatment of pigmented lesions in Asians.
Acknowledgements
Conflict of interest: Dr.T. Kono has received equipment from Syneron-Candela and Cynosure. Dr. H.H.L. Chan has conducted research, received grants and free equipment from Syneron-Candela and Cynosure.
References
- 1: Anderson RR, Margolis RJ, Watenabe S. Selective photothermolysis of cutaneous pigmentation by Q-switched Nd:YAG laser pulses at 1064, 532 and 355 nm. J Invest Dermatol 1989; 93: 28-32. [DOI] [PubMed] [Google Scholar]
- 2: Chan HH, Alam M, Kono T, Dover JS. Clinical applications of lasers in Asians. Derm Surg. 2008;28(7):556-563. [DOI] [PubMed] [Google Scholar]
- 3: Murphy MJ, Huang MY. Q-switched ruby laser treatment of benign pigmented lesions in Chinese skin. Am Acad Med Singapore 1994; 23: 60-66. [PubMed] [Google Scholar]
- 4: Wang CC, Sue YM, Yang CH, Chen CK. A comparison of Q-switched alexandrite laser and intense pulsed light for the treatment of freckles and lentigines in Asian persons: A randomized, physician-blinded, split-face comparative trial. J Am Acad Dermatol. 2006;54(5):804-810. [DOI] [PubMed] [Google Scholar]
- 5: Chan HH, Fung WK, Ying SY, Kono T. An in vivo trial comparing the use of different types of 532 nm Nd:YAG lasers in the treatment of facial lentigines in Oriental patients. Dermatol Surg. 2000;26(8):743-749. [DOI] [PubMed] [Google Scholar]
- 6: Ho SG, Yeung CK, Chan NP, Shek SY, Chan HH. A comparison of Q-switched and long-pulsed alexandrite laser for the treatment of freckles and lentigines in oriental patients. Lasers Surg Med. 2011;43(2):108-113. [DOI] [PubMed] [Google Scholar]
- 7: Kono T, Manstein D, Chan HH, Nozaki M, Anderson RR. Q-switched ruby versus long-pulsed dye laser delivered with compression for treatment of facial lentigines in Asians. Lasers Surg Med. 2006. February;38(2):94-7. [DOI] [PubMed] [Google Scholar]
- 8: Negishi K, Tezuka Y, Kushikata N, Wakamatsu S. Photorejuvenation for Asian skin by intense pulsed light. Dermatol Surg 2001; 27: 627-632. [DOI] [PubMed] [Google Scholar]
- 9: Rosenbach A, Lee SJ, Johr RH. Treatment of medium-brown solar lentigines using an alexandrite laser designed for hair reduction. Arch Dermatol 2002; 138: 547-548. [DOI] [PubMed] [Google Scholar]
- 10: Trafeli JP, Kwan JM, Meehan KJ, et al. Use of a long-pulse alexandrite laser in the treatment of superficial pigmented lesions. Dermatol Surg 2007; 33: 1477-1482. [DOI] [PubMed] [Google Scholar]
- 11: Ho SG, Goh CL. Laser tattoo removal: a clinical update. J Cutan Aesthet Surg. 2015;8(1):9-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12: Khunger N, Molpariya A, Khunger A. Complications of Tattoos and Tattoo Removal: Stop and Think Before you ink. J Cutan Aesthet Surg. 2015. Jan-Mar;8(1):30-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13: Ross V, Naseef G, Lin G, Kelly M, Michaud N, Flotte TJ, Raythen J, Anderson RR. Comparison of responses of tattoos to picosecond and nanosecond Q-switched neodymium: YAG lasers. Arch Dermatol. 1998;134(2):167-71. [DOI] [PubMed] [Google Scholar]
- 14: Brauer JA, Reddy KK, Anolik R, et al. Successful and rapid treatment of blue and green tattoo pigment with a novel picosecond laser. Arch Dermatol. 2012;148(7):820-3. [DOI] [PubMed] [Google Scholar]
- 15: Alabdulrazzaq H, Brauer JA, Bae YS, Geronemus RG. Clearance of yellow tattoo ink with a novel 532-nm picosecond laser. Lasers Surg Med. 2015. April;47(4):285-8. [DOI] [PubMed] [Google Scholar]
- 16: Goldberg D.J., Nychay S.G.: Q-switched ruby laser treatment of nevus of Ota. J Dermatol Surg. 1992, 18 (9): 817-821. [DOI] [PubMed] [Google Scholar]
- 17: Watanabe S, Takahashi H. Treatment of nevus of Ota with the Q-switched ruby laser. N Engl J Med. 1994. December 29;331(26):1745-50. [DOI] [PubMed] [Google Scholar]
- 18: Kono T., Nozaki M., Chan H.H., Mikashima Y.: A retrospective study looking at the long-term complications of Q-switched ruby laser in the treatment of nevus of Ota. Lasers Surg Med, 29(2): 156-159, 2001. [DOI] [PubMed] [Google Scholar]
- 19: Chang C.J., Kou C.S.: Comparing the effectiveness of Q-switched Ruby laser treatment with that of Qswitched Nd:YAG laser for oculodermal melanosis (Nevus of Ota). J Plast Reconstr Aesthet Surg, 64(3): 339-345, 2011. [DOI] [PubMed] [Google Scholar]
- 20: Kono T., Chan H.H., Erçöçen A.R., Kikuchi Y., Uezono S., Iwasaka S., Isago T., Nozaki M.: Use of Qswitched ruby laser in the treatment of nevus of ota in different age groups. Lasers Surg Med, 32(5): 391-395, 2003. [DOI] [PubMed] [Google Scholar]
- 21: Chan HH, Ying SY, Ho WS, et al. : An in vivo trial comparing the clinical efficacy and complications of Q-switched 755 nm alexandrite and Q-switched 1064 nm Nd:YAG lasers in the treatment of nevus of Ota. Dermatol Surg 26(10):919-922.2000. [DOI] [PubMed] [Google Scholar]
- 22: Chan H.H., Leung P.S., Ying S.Y., Lai C.F., Kono T., Chua J.K., Ho W.S.: A retrospective analysis of complications in the treatment of nevus of Ota with the Q-switched alexandrite and Q-switched Nd:YAG lasers. J Dermatol Surg, 26 (11): 1000-1006, 2000. [DOI] [PubMed] [Google Scholar]
- 23: Chesnut C, Diehl J, Lask G. Treatment of nevus of ota with a picosecond 755-nm alexandrite laser. Dermatol Surg. 2015. April;41(4):508-10. [DOI] [PubMed] [Google Scholar]


