Highlights
-
•
Various surgical and non-surgical treatment strategies have been identified for humeral shaft fractures.
-
•
Easy application, minimum soft tissue injury, less blood loss and less chances of radial nerve injury are the most important advantages of the inflatable humeral nails.
-
•
Inflatable intramedullary nail is an effective technique for treating humeral AO type A midshaft fractures.
Keywords: Inflatable intramedullary nail, Humeral shaft fractures, Expandable nail, Surgery
Abstract
Background
We assessed the results of humeral shaft fracture fixation using the inflatable intramedullary nail using radiological and clinical findings.
Methods
From 2012 to 2015, we treated 14 patients with humeral shaft fractures using inflatable intramedullary nail after closed reduction.
Results
The mean follow-up time was 14.1 months. The mean time to bone union was 4.5 months. None of the patients had major perioperative mechanical complications or postoperative complications, except for the occurrence of fixation loss and non-union in one patient.
Conclusion
Inflatable intramedullary nails seem to be applicable, safe and effective for humeral AO/OTA type A midshaft fractures.
1. Introduction
Humeral shaft fractures are common injuries, representing 1–3% of all fractures.1, 2 The distribution is bimodal, and they occur more commonly in the third decade of life in males and the seventh decade in females.1, 2, 3 A majority of humeral shaft fractures can be treated successfully using non-operative methods such as hanging cast, functional brace, velpeau dressing, coaptation splint and abduction cast.2, 4, 5, 6 In some cases, conservative methods are not sufficient.2, 4, 7 Some surgeons opt for surgery even for simple humeral shaft fractures to avoid the risk of non-union and allow for early mobilisation and rapid return to work.1, 3, 7, 8, 9, 10, 11, 12
Intramedullary nailing is considered the gold standard treatment for shaft fractures of long bones.1, 5, 13 Although plate and screw fixation has traditionally been the preferred method for humeral shaft fractures, inflatable intramedullary nail is another option for surgical management of humeral shaft fractures, which has the advantages of easy application, minimum soft tissue injury, shortening the surgery time and less exposure to radiation.1, 3, 7, 9, 10, 13, 14, 15, 16, 17
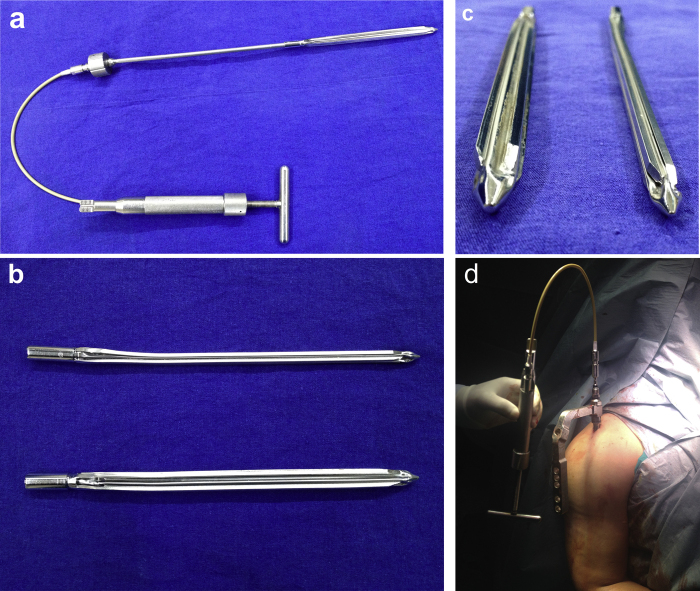
The hydraulically inflatable intramedullary nail consists of an expandable stainless steel tube with four reinforcement bars connected by thin folded stainless steel membranes with a conical distal end.6, 10, 13, 16 Normal saline is injected into the hollow inner core of the nail under pressure through a proximal valve to expand it and increase its effective diameter (Fig. 1).6, 10, 13, 16 Inflatable intramedullary nail methods used for humeral shaft fractures as cited in the literature are shown in Table 1.
Fig. 1.
(a) A manual hydraulical pump is used to inflate the intramedullary nail. (b, c) The nail in its uninflated and inflated state. (d) Intraoperative view of the inflatable intramedullary nail application.
Table 1.
Studies available in the literature on the inflatable intramedullary nail method (during 2000–2016).
| Study (years) | Patients (n) | Mean age (years) | Follow-up (months) | Type of fracture (AO classification) | Average operating time (min) | Average union time (months) | Complications | Others |
|---|---|---|---|---|---|---|---|---|
| Lepore et al.13 (2000) | 7 | – | – | A: 5 B: 2 |
– | 3 (consolidation) | Fracture occurred during nail expansion was seen in two patients | One nail was removed without any problem |
| Franck et al.17 (2002) | 22 patients, 23 pathological fractures | 68.2 | – | A2:5 A3:5 B1:2 B2:3 B3:1 C1:2 C2:4 C3:1 |
32 | – | ||
| Blumgerg et al.18 (2002) | 35 | 41 | 4 | – | 52 | – | 7 partial union | Eight nails were removed after complete union was achieved |
| Daglar et al.12 (2002) | 3 | 38 | 16 | A3:2 C2:1 |
35 | 3.6 | – | – |
| Lorich et al.6 (2003) | 11 | 47 | A1:3 A2:2 A3:3 B1:1 B2:1 C3:1 |
90 | 2.1 (Clinical union) 1.9 (Radiographic union) |
– | ||
| Panidis et al.19 (2003) | 6 | 25 | 12.2 | – | 40.5 | – | – | |
| Franck et al.15 (2003) | 25, osteoporotic humerus | 73.5 | – | 4 | – | |||
| Javanovic et al.8 (2004) | 9 | 43 | – | A2: 5 A3: 3 Segmental fracture: 1 |
30 | 6 | – | |
| Smith et al.20 (2004) | 1 | 65 | A3: 1 | – | 4 | Although the nail had deflated, the fracture healed | ||
| Logan et al.21 (2005) | 42 patients: 20 acute fractures, 12 delayed and non-union, 10 pathological fractures | – | 6 | – | 71 | – | 3 non-union | |
| Dall’Oca and Lavini22 (2005) | 19 patients, 20 humerus | 35.6 | – | A1 + A2: 8 A3: 10 B2: 2 |
– | 5 | 2 patients showed delayed union | |
| Daglar et al.9 (2007) | 21 | 39.4 | 31.4 | A1: 2 A2: 1 A3: 7 B1: 4 B2: 4 C1: 1 C2: 2 |
25.3 | 2.9 | 2 non-union | |
| Siegel et al.10 (2008) | 6 pathological fractures | – | 9.3 | – | 22.3 | 4.4 | ||
| Ozturk et al.23 (2008) | 16 | – | – | – | – | – | 2 nails showed non-union, 1 nail was broken | |
| Galasso et al.24 (2008) | 3 non-union | 13 | – | 48 | 5.3 | – | Combined use of inflatable intramedullary nailing and autologous platelet-rich plasma (PRP) |
In the present study, clinical and radiographic outcomes of the inflatable intramedullary nail method were assessed in AO classification type A humeral shaft fractures.
2. Materials and methods
From January 2012 to July 2015, we treated 14 (six males, eight females; five right, nine left side; mean age: 54.8 years, range: 27–88 years) patients with humeral shaft fractures using antegrade inflatable intramedullary nails (Fixion® IM Nail, Dic-O-Tech, St. Herzliya, Israel) after closed reduction. The characteristics of the patients are presented in Table 2.
Table 2.
Patients’ demographic characteristics and clinical outcomes.
| Patients (n) | 14 |
| Follow-up (months) | 14.1 (8–26) |
| Sex, n (%) | |
| Female | 8 (57.2) |
| Male | 6 (42.8) |
| Mean age, years, mean (range) | 54.8 (27–88) |
| Side of involvement, n (%) | |
| Right | 5 (35.7) |
| Left | 9 (64.2) |
| AO classification, n (%) | |
| A1 | 3 (29.4) |
| A2 | 7 (29.4) |
| A3 | 4 (5.8) |
| Operation time, minutes (range) | 42 (30–65) |
| Mean union time, months (range) | 4.5 (3–7) |
2.1. Surgical technique
Patients were placed in a beach chair position and an anterior approach through a small rotator cuff incision (2 cm) was used to place the nails antegrade. The entry hole was established in the humerus using an awl. Reaming was not performed on the humerus. After closed reduction of fractures, the nail (6.7 mm, 7.4 mm or 8.5 mm, with the capacity to expand to 10 mm, 11 mm or 13.5 mm, respectively) was selected and inserted in the humerus.
The patients were administered a long arm plaster splint for seven days postoperatively. Then, the splint was removed and shoulder pendulum exercises were started. After four or five weeks, active exercises were allowed as long as the patients could tolerate.
At the last follow-up, all the patients were evaluated radiologically for bone union. Fracture healing was assessed by an independent observer. Radiographic healing was defined as callus bridging of three of four cortices on anteroposterior and lateral radiographs,25 as well as being painless on the affected extremity. In addition, the patients were investigated for the presence of infection, neurovascular disorders and deformities (varus/valgus, rotation and shortening) and clinical evaluation was performed using the Constant shoulder score.26 The study was approved by our Institutional Review Board, and all patients provided informed consent.
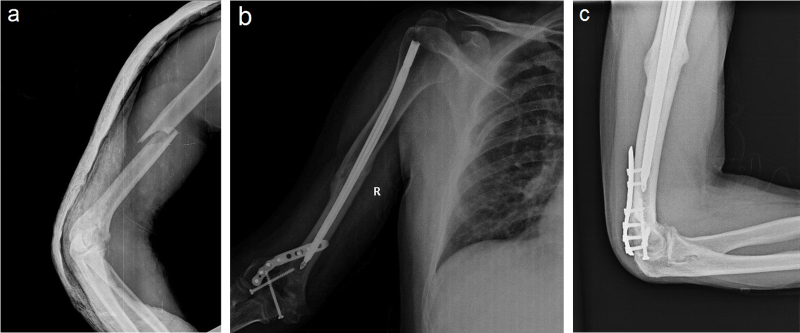
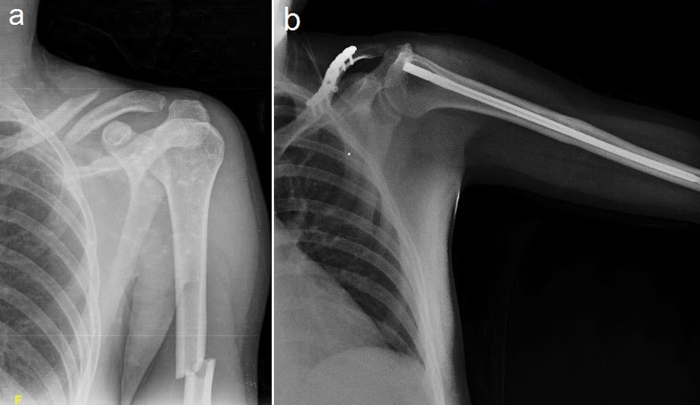
3. Results
Patient fractures were classified according to the AO classification as follows: A1 in three (21.5%) patients, A2 in seven (50%) patients and A3 in four (28.5%) patients. The most common cause of injury was fall related in nine cases (64.2%), while five (35.8%) of the fractures were related to a traffic accident. Four (36.3%) patients also had fractures in other extremities. The mean follow-up time was 14.1 months (range: 8–26 months). The mean operation time was 42 min (range: 30–65 min). The mean length of hospitalisation was 5.8 days (range: 2–14 days). The mean time to bone union was 4.5 months (range: 3–7 months). None of the patients had major perioperative mechanical complications or postoperative complications such as infections and neurovascular complications, except for the occurrence of fixation loss and non-union in one patient. All the other patients had complete union at the last follow-up (Fig. 2, Fig. 3). There were no sagittal or rotatory deformities upon clinical examination. Any limb shortening was also not observed. One patient had shoulder pain and range of motion restriction (Fig. 4). Constant scores were excellent (>90) for nine (64.2%) patients, well (80–89) for four (28.5%) patients and worse (<70) for one (7.1%) patient.
Fig. 2.
Radiographic images of humeral fracture of a 39-year-old male patient with multiple fractures. (a) Pre-operative radiograph. (b) Radiograph at postoperative month 7.
Fig. 3.
Radiographic images of humeral fracture of a 28-year-old male patient with multiple fractures. (a) Pre-operative radiograph. (b) Radiograph at postoperative month 26.
Fig. 4.

Radiographic image of proximal migration of the inflatable nail with non-union in the humeral fracture of a 60-year-old female patient.
4. Discussion
Humeral shaft fractures have a high tolerance less than anatomical reduction compared with other long bone fractures and are considered acceptable with angulation of up to 20° and shortening up to 3 cm.1, 2, 3, 4, 7 Various surgical and non-surgical treatment strategies have been identified for humeral shaft fractures. Each method has its own advantages and disadvantages.1, 2, 3, 4, 5, 7 A majorities of the humeral shaft fractures can be treated using non-operative methods such as hanging cast, functional brace, velpeau dressing, coaptation splint and abduction cast with good functional outcomes.1, 3, 4, 5, 7
Although closed techniques have successful results, they may not be suitable for all situations.1, 3, 4, 5 In particular, the application of plaster splint may not be easily tolerated by some patients.4, 15, 17 Indications for surgical treatment of humeral shaft fractures can be classified as malalignment, open fractures, vascular injuries, polytraumatised patients, ipsilateral fractures and pathological fractures.3, 4, 6, 7 In addition, there is a growing interest in treating even simple humeral shaft fractures using surgery, to allow for earlier mobilisation and rapid return to work.1, 3, 7, 8, 10, 11
Inflatable intramedullary nails due to their small diameter permit easy advance through the medullary canal and allow closed fixation.7, 10, 16 After the application when the nail is inflated using serum saline infusion, the medullary canal fills with the nail and the fracture can be stablised.7, 8, 9, 10, 15, 16, 17 Easy application, minimum soft tissue injury, less blood loss and less chances of radial nerve injury are the most important advantages of the inflatable humeral nails.7, 8, 9, 10, 15, 16, 17 In addition, other important advantages of the inflatable intramedullary nails include shortening of surgery time and reducing the exposure to fluoroscopy dose.10, 14, 16 In our study, we determined the mean operation time as 47.5 min. In similar studies on humeral fractures, Lorich et al.6 reported the mean operation time as 90 min, Javanovic et al.8 reported the mean operation time as 30 min, Daglar et al.9 reported it as 25.3 min, Siegel et al.10 reported it as 22.3 min, Blumgerg et al.18 observed the mean operation time as 52 min and Panidis et al.19 reported an average operation time of 40.5 min.
Compared to locked intramedullary nails, inflatable intramedullary nails do not provide sufficient stability for complex-multipart unstable fractures and also have less resistance against rotational forces.10, 14, 27, 28 Therefore, it must be considered that inflatable intramedullary nails may fail to provide sufficient stability for metaphyseal and complex-multipart fractures.27, 28 Blomquist et al.27 in their biomechanical study on cadavers found that inflatable intramedullary nails had high bending stiffness and low torsional strength as compared with locked intramedullary nails. They also reported that inflatable intramedullary nails made slippage movement during torsional tests.27
In some studies, it was observed that the bars surrounding the inflatable intramedullary nails, which make contact with the medulla, achieve multiplanar stability. The surface area of the nail was increased in the axial section after the expansion of the nails.14, 27, 28 In addition, inflatable intramedullary nails are superior to interlocking intramedullary nails in terms of the frequency of bending but are insufficient in terms of rotational stiffness.14, 27 However, some authors prefer inflatable intramedullary nails, particularly in osteoporotic patients, because they support the idea that drilling the cortex several times while inserting the distal screws weakens the cortex and may cause the cut out of the screw.6, 15
Open reduction and plating is considered to be the gold standard for surgical intervention of humeral shaft fractures. However, conventional plating technique involves an extensive surgical approach for open reduction of the fracture and is theoretically associated with increased risk of radial nerve injury and more blood loss.1, 3, 4 Intramedullary nailing in humeral fractures is a less invasive procedure.1, 4 A meta-analysis of 10 studies comparing the results of plating versus classic locked intramedullary nailing concluded that both achieve similar results in humeral fractures, but plating was associated with reduced shoulder problems.3
On the other hand, the smaller diameter of the inflatable humeral nail offers easier insertion into the humeral canal.6, 7 This also allows for a more lateral starting point of proximal humerus, thereby decreasing the likelihood of injuring the rotator cuff structures in antegrade insertion.6, 7 In our study, we did not encounter any serious shoulder problems, except in one patient in the follow-up period. We could manage good upper limb function recovery with early rehabilitation and stable fixation with minimal trauma in surgery.
Expandable nail has a 7.8% rate of non-union, which is similar to the reported rate of non-union following locked humeral nailing (0–8%).7 Franck et al.15, 17 showed almost 100% union rate and no complications in two separate studies using Fixion® nails to stabilise pathological and osteoporotic humeral fractures with 6 months of follow-up. Lorich et al.,6 Javanovic et al.,8 Lepore et al.,13 Siegel et al.10 and Panidis et al.20 have shown 100% union rates, while Daglar et al.9 reported 90% union rate and Logan et al.21 reported 85% union rate for the primary fracture fixation. In our series, we managed nearly 93% union rate using inflatable humeral nails. The non-union rate of the inflatable intramedullary nails that either migrated proximally or failed to maintain reduction has been reported to be 2.8%.10, 11, 23 The most common reason for this is that the nail spontaneously deflated following implantation, leading to instability at the fracture site.7 In our study, occurrence of fixation loss and non-union was seen in one patient due to proximal migration of the nail.
In summary, inflatable intramedullary nails seem to be easily applicable, safe and effective for humeral AO type A midshaft fractures. Inflatable intramedullary nails have some advantages in the treatment of humeral midshaft fractures, such as easy insertion, reduced operating time and reducing the exposure to fluoroscopy dose. In cases of multiple injuries that require rapid intervention, use of inflatable intramedullary nails may be appropriate.
Conflicts of interest
The authors have none to declare.
References
- 1.Li Y., Wang C., Wang M., Huang L., Huang Q. Postoperative malrotation of humeral shaft fracture after plating compared with intramedullary nailing. J Shoulder Elbow Surg. 2011;20:947–954. doi: 10.1016/j.jse.2010.12.016. [DOI] [PubMed] [Google Scholar]
- 2.Sarmiento A., Zagorski J.B., Zych G.A., Latta L.L., Capps C.A. Functional bracing for the treatment of fractures of the humeral diaphysis. J Bone Joint Surg Am. 2000;82:478–486. doi: 10.2106/00004623-200004000-00003. [DOI] [PubMed] [Google Scholar]
- 3.Ouyang H., Xiong J., Xiang P., Cui Z., Chen L., Yu B. Plate versus intramedullary nail fixation in the treatment of humeral shaft fractures: an updated meta-analysis. J Shoulder Elbow Surg. 2013;22:387–395. doi: 10.1016/j.jse.2012.06.007. [DOI] [PubMed] [Google Scholar]
- 4.Walker M., Palumbo B., Badman B., Brooks J., Van Gelderen J., Mighell M. Humeral shaft fractures: a review. J Shoulder Elbow Surg. 2011;20:833–844. doi: 10.1016/j.jse.2010.11.030. [DOI] [PubMed] [Google Scholar]
- 5.Pehlivan O., Arpacioglu M.O., Kiral A., Akmaz I., Mahirogullari M., Kaplan H. Comparison between functional bracing and locked intramedullary nailing in isolated and closed humeral shaft fractures. Eklem Hastalik Cerrahisi. 2005;16:175–180. [Google Scholar]
- 6.Lorich D.G., Geller D.S., Yacoubian S.V., Leo A.J., Helfet D.L. Intramedullary fixation of humeral shaft fractures using an inflatable nail. Orthopedics. 2003;26:1011–1014. doi: 10.3928/0147-7447-20031001-10. [DOI] [PubMed] [Google Scholar]
- 7.Rose D.M., Smith T.O., Nielsen D., Hing C.B. Expandable intramedullary nails for humeral fractures: a systematic review of clinical and radiological outcomes. Eur J Orthop Surg Traumatol. 2013;23:1–11. doi: 10.1007/s00590-011-0908-5. [DOI] [PubMed] [Google Scholar]
- 8.Jovanovic A., Pirpiris M., Semirli H., Doig S.G. Fixion nails for humeral fractures. Injury. 2004;35:1140–1142. doi: 10.1016/j.injury.2004.01.020. [DOI] [PubMed] [Google Scholar]
- 9.Dağlar B., Delialioğlu O.M., Taşbaş B.A., Bayrakçi K., Ağar M., Günel U. Comparison of plate-screw fixation and intramedullary fixation with inflatable nails in the treatment of acute humeral shaft fractures. Acta Orthop Traumatol Turc. 2007;41:7–14. [Article in Turkish] [PubMed] [Google Scholar]
- 10.Siegel H.J., Sessions W., Casillas M.A., Jr. Stabilization of pathologic long bone fractures with the Fixion expandable nail. Orthopedics. 2008;31:143–148. doi: 10.3928/01477447-20080201-31. [DOI] [PubMed] [Google Scholar]
- 11.Mallick E., Hazarika S., Assad S., Scott M. The Fixion® nailing system for stabilising diaphyseal fractures of the humerus: a two-year clinical experience. Acta Orthop Belg. 2008;74:308–316. [PubMed] [Google Scholar]
- 12.Daglar B., Bayrakci K., Tasbas B.A., Gürkan I., Agar M., Günel U. Short-term results of treatment of humeral and tibial fractures with new inflatable intramedullary nails. Acta Orthop Traumatol Turc. 2002;36:322–327. [Article in Turkish] [PubMed] [Google Scholar]
- 13.Lepore S., Capuano N., Lepore L., Romano G. Preliminary clinical and radiographic results with the Fixion intramedullary nail: an inflatable self-locking system for long bone fractures. J Orthopaed Traumatol. 2000;1:135–140. [Google Scholar]
- 14.Bekmezci T., Baca E., Kocabas R., Kaynak H., Tonbul M. Early results of treatment with expandable intramedullary nails in tibia shaft fractures. Acta Orthop Traumatol Turc. 2005;39:421–424. [PubMed] [Google Scholar]
- 15.Franck W.M., Olivieri M., Jannasch O., Hennig F.F. Expandable nail system for osteoporotic humeral shaft fractures: preliminary results. J Trauma. 2003;54:1152–1158. doi: 10.1097/01.TA.0000066146.13247.CA. [DOI] [PubMed] [Google Scholar]
- 16.Kapoor S.K., Kataria H., Boruah T., Patra S.R., Chaudhry A., Kapoor S. Expandable self-locking nail in the management of closed diaphyseal fractures of femur and tibia. Indian J Orthop. 2009;43:264–270. doi: 10.4103/0019-5413.53457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Franck W.M., Olivieri M., Jannasch O., Hennig F.F. An expandable nailing system for the management of pathological humerus fractures. Arch Orthop Trauma Surg. 2002;122:400–405. doi: 10.1007/s00402-002-0428-1. [DOI] [PubMed] [Google Scholar]
- 18.Blumgerg N., Tauber M., Dekel S., Steinberg E. A preliminary clinical experience with the expandable intramedullary nail in traumatic humerus, tibia and femur fractures. Orthopaedic Proc. 2002;84:304. [Google Scholar]
- 19.Panidis G., Sayegh F.E., Beletsiotis A., Natsis K., Hatzemmanuil D., Antosidis K. Treating-stabilizing long bone fractures using inflatable self-locking intramedullary nail technique-preliminary results. Orthopaedic Proc. 2003;85:229. [Google Scholar]
- 20.Smith M.G., Canty S.J., Khan S.A. Fixion – an inflatable or deflatable nail? Injury. 2004;35:329–331. doi: 10.1016/s0020-1383(03)00260-2. [DOI] [PubMed] [Google Scholar]
- 21.Logan K.J., Costa M., Patel A.D. The fixion humeral nail: the Norwich experience of 42 cases. Orthopaedic Proc. 2005;87:336–337. [Google Scholar]
- 22.Dall’Oca C., Lavini F. “Fixion” intramedullary nailing: an inflatable system in humeral diaphyseal fractures. J Bone Joint Surg Br. 2005;87:179. [Google Scholar]
- 23.Ozturk H., Unsaldi T., Oztemur Z., Bulut O., Korkmaz M., Demirel H. Extreme complications of Fixion nail in treatment of long bone fractures. Arch Orthop Trauma Surg. 2008;128:301–306. doi: 10.1007/s00402-007-0458-9. [DOI] [PubMed] [Google Scholar]
- 24.Galasso O., Mariconda M., Romano G. Expandable intramedullary nailing and platelet rich plasma to treat long bone non-unions. J Orthop Traumatol. 2008;9:129–134. doi: 10.1007/s10195-008-0021-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Whelan D.B., Bhandari M., McKee M.D. Interobserver and intraobserver variation in the assessment of the healing of tibial fractures after intramedullary fixation. J Bone Joint Surg Br. 2002;84:15–18. doi: 10.1302/0301-620x.84b1.11347. [DOI] [PubMed] [Google Scholar]
- 26.Constant C.R., Murley A.H. A clinical method of functional assessment of the shoulder. Clin Orthop Rel Res. 1987;214:160–164. [PubMed] [Google Scholar]
- 27.Blomquist J., Lundberg O.J., Gjerdet N.R., Molster A. Are inflatable nails an alternative to interlocked nails in tibial fractures? Clin Orthop Relat Res. 2008;466:1225–1231. doi: 10.1007/s11999-008-0169-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Maher S.A., Meyers K., Borens O. Biomechanical evaluation of an expandable nail for the fixation of midshaft fractures. J Trauma. 2007;63:103–107. doi: 10.1097/01.TA.0000243205.24809.3f. [DOI] [PubMed] [Google Scholar]