Abstract
Aims and Objectives:
Several biological, social, and cultural factors contribute to the poor outcome of tobacco cessation interventions. Inability to engage large number of participants is one of the major identifiable factors. The objective of this study was to compare the outcome of tobacco cessation interventions in the clinical and workplace settings.
Materials and Methods:
In the present study, we recruited 100 participants in tobacco cessation clinic (TCC) group and workplace group (50 participants in each). Both the groups were regularly intervened and were followed up regularly at 2 weeks, 4 weeks, 3 months, and 6 months. Active interventions in the form of awareness lectures, focused group discussions, and if needed, pharmacotherapy (nicotine/non-nicotine replacement therapy) was carried out for all participants. The outcome was assessed as no change, harm reduction (>50% reduction), complete cessation, and drop out. Statistical analysis of the data was done using the Statistical Package for the Social Sciences version 21.0.
Results:
At the end of 1 month, there was higher tobacco cessation rate in the workplace group versus TCC group (n = 22, 44% vs n = 9, 18%; P < 0.0001). The tobacco cessation rate was maintained even after 6 months of intervention (n = 30, 60% vs n = 12, 24%; P = 0.002) and dropout rate was also lower among the workplace group than the TCC group (n = 14, 28% vs n = 27, 54%; P < 0.0001).
Conclusions:
Our study findings suggest that the workplace setting has superior outcome in tobacco cessation and harm reduction than clinical setting. In addition, it is associated with low dropout rate and the cessation effect is maintained over a period of 6 months.
Keywords: Focused group discussion, nicotine dependence, nicotine/non-nicotine replacement therapy, tobacco cessation clinic, workplace
INTRODUCTION
Tobacco use is a major modifiable risk factor for health, which is one of the leading causes of a range of cardiovascular and respiratory disorders in addition to various cancers in the body.[1] India has a huge burden of tobacco-related morbidity, disability, and mortality.[2] The Global Adult Tobacco Survey (GATS) in 2010 revealed that 47.9% of males and 20.3% of females, constituting 34.6% of the adult population, used tobacco in one or the other form in India.[3,4] Social and cultural acceptance among youth is one of the reason for higher prevalence of tobacco consumption in India.
Among the 70% of nicotine dependent participants reporting that they want to quit, annually only 4–6% succeed.[5,6,7,8,9] Unassisted tobacco cessation is very low unlike in the West.[6] To assist the tobacco cessation efforts of tobacco users, tobacco cessation clinics (TCCs) were started across India by the Ministry of Health and Family Welfare, Government of India, with the support of the World Health Organization in 2002.[8,10] A TCC provides interventions such as behavioral counseling with or without medication (nicotine/non-nicotine replacement therapy).
However, long-term outcome of these interventions conducted at TCCs remained poor, but successful than unassisted tobacco cessation. A recently published study showed that only 26% participants improved at 3 months, 21% at 6 months, and 18% at 9 months.[11] Major barriers for long-term tobacco cessation include peer pressure, lack of psychosocial support, attitude towards tobacco cessation, younger age, lack of community awareness, lack of trained professionals, and poor follow-up in subsequent visits.[12,13,14,15,16]
To improve tobacco cessation outcome, it needs to go beyond the health sector to multiple settings such as workplace, educational, and tobacco control policies.[2] In addition, these interventions should be cost-effective and wide reaching. Workplace and educational setting has shown two to three times increase in tobacco cessation rate.[17,18] These results are promising, but limited by uncontrolled study design, non-homogenous study population, and minimal interventions. To overcome the limitations of previously conducted studies, the present study aimed to compare the effectiveness of tobacco cessation services in clinical and workplace settings.
MATERIALS AND METHODS
The present study was a prospective, interventional, cohort study of 6-month duration. The study was conducted with due permission and support from the management, union, and employees of the selected industry as well as hospital. It was approved by the Institutional ethical committee of B.K.L. Walawalkar Rural Medical College.
Participants
A total of 100 participants were included in study. Fifty employees working in the selected chemical industrial unit and willing to participate were enrolled in the workplace group. An equal number of age and sex-matched participants visiting TCC of Jagruti De-addiction Centre were recruited in the TCC group. The participants with a previous history of psychiatric illness or neurological illness were excluded from study.
Intervention
The study was conducted from 1st August 2015 to 31st January 2016. All the participants were enrolled in the month of August 2015. The aim and purpose of the study were explained to each participant, and those who are willing to participate were enrolled after signing the written informed consent form which was made available in the local language (Marathi). The first session included an introductory lecture and interviews of the participants to collect preintervention data about various sociodemographic and risk factor variables. The follow-up sessions were offered at 2 weeks and 4 weeks, and then at 3 months and 6 months for both the clinical and TCC groups. During these sessions, professional help in the form of health awareness sessions, focus group discussion, one-on-one counseling, and pharmacotherapy including nicotine (gum, lozenges) and non-nicotine (Bupropion and Varenicline) replacement was provided to the employees by a team of doctors and counselors. During follow-up, abstinence was evaluated by self-report and biochemically confirmed by negative result of a cotinine test performed on saliva (a cotinine level of <15 ng per milliliter)[19] or urine sample (with a level of <2 ng per milliliter).[20] All the pretest measures were repeated in after the test.
Sample size calculation and statistical analysis
Sample size was based on change in the primary outcome variable (qualitative outcome i.e. complete tobacco cessation, more than 50% reduction, no change, and drop out). The PS, Power and Sample Size Calculation version 3.1.2 was used for sample size calculation. Prior studies indicate that the probability of complete tobacco cessation after 6 months of treatment in clinical setting is 0.20 and odds ratio for tobacco cessation in workplace settings is 3.65.[21] The sample size was calculated with a power of 80%, precision rate of 5%, correlation coefficient (φ) of 0.5, and matched in 1:1 ratio. The minimum sample size for this study was calculated to be 47, and therefore, 50 participants were included in each group.
The statistical analysis was carried out by using the Statistical Package for the Social Sciences (SPSS) version 21.0. (IBM Corp. Released 2012. IBM SPSS Statistics for Windows, Armonk, NY). The categorical variables were expressed in percentage and analyzed by independent Chi-square test and Fisher exact test. The quantitative data were expressed in mean ± SD (standard deviation), and compared using independent t-test. Outcome in each group was compared in terms of proportion. Multinominal logistic regression was used to predict the outcome of tobacco cessation in both the settings. For each test, the significance level was set at P < 0.05.
RESULTS
The clinical and sociodemographic characteristics of the workplace and TCC groups are depicted in Table 1. All the participants of the present study were men. There was no statistically significant difference between the two groups in terms of age, socioeconomic status, residence, type of tobacco use, and intervention for tobacco cessation. The age of initiation of tobacco use was significantly lower in case of participants attending tobacco cessation services than the workplace group (P < 0.001). However, the Fagerstrom score was higher and significant among the participants with tobacco cessation group than the workplace group (t = 2.03 df = 98, P = 0.045).
Table 1.
Sociodemographic and clinical characteristics of workplace and TCC groups
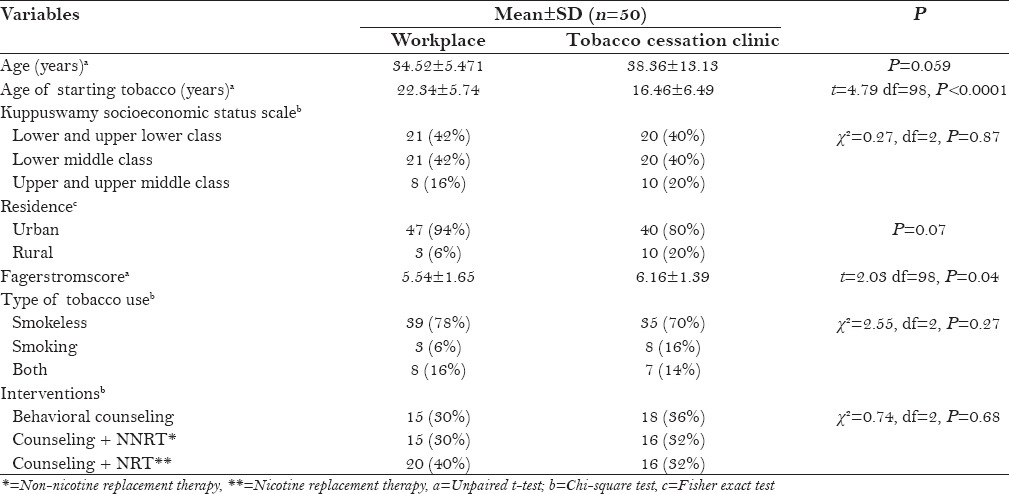
Table 2 and Figure 1 show the outcome of tobacco cessation at the end of 2 weeks, 4 weeks, 3 months, and 6 months after intervention, At the end of 2 weeks, (n = 9, 18%) participants in the TCC group and (n = 22, 44%) participants in the workplace group stopped tobacco consumption completely, whereas (n = 14, 28%) participants in the TCC group and (n = 22, 44%) participants in the workplace group reduced tobacco consumption. Tobacco cessation rate was increased in the subsequent visit in both the groups. However, proportion of tobacco cessation in the workplace group was higher in comparison to the TCC group.
Table 2.
Outcome of tobacco cessation in two groups
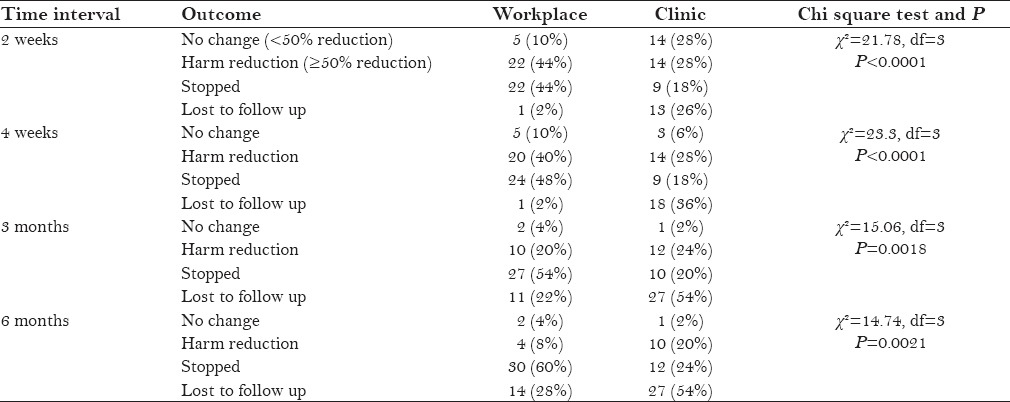
Figure 1.
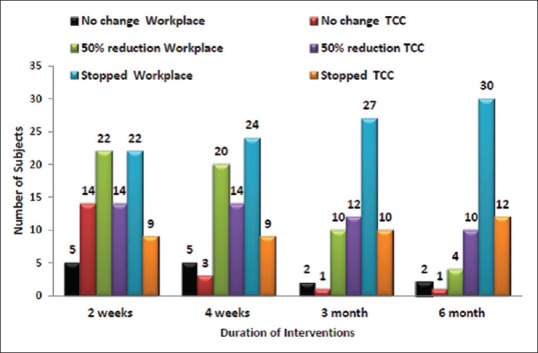
Outcome of tobacco cessation in two groups
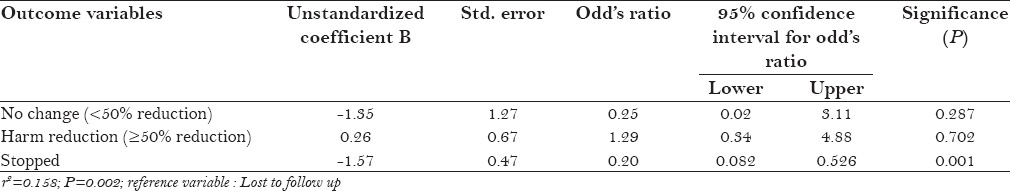
At the end of 6 months, (n = 12, 24%) participants in the TCC group and (n = 30, 60%) participants in the workplace group stopped tobacco consumption completely, whereas (n = 4, 8%) participants in the TCC group and (n = 10, 20%) participants in the workplace group reduced tobacco consumption. The drop out was higher in the TCC group in all follow ups. Only (n = 1, 2%) participant at the end of 2 weeks and (n = 14,28%) participants at the end of 6 months were lost to follow up in the workplace group, while (n = 13,26%) participants at the end of 2 weeks and (n = 27, 54%) participants at the end of 6 months were lost to follow up in the TCC group. On multinominal logistic regression, odds ratio (OR) for complete tobacco cessation was (OR = 0.20, 95% CI = 0.082–0.526, P < 0.001), more than 50% reduction was (OR = 1.29, 95% CI = 0.34–4.88, P = 0.70), and no change was (OR = 0.25, 95% CI = 0.02–3.11, P = 0.28) in clinical group [Table 3].
Table 3.
Multinominal logistic regression analysis of the variables (clinical vs workplace settings)
DISCUSSION
The present study aimed to compare the effectiveness of tobacco cessation services in clinical and workplace settings. We observed that the outcome of tobacco cessation improved in the workplace group than the clinical group. After 6 months of intervention, complete tobacco cessation rate was 2.5 times higher among the workplace group than the clinical group. In addition, the tobacco cessation rate was consistently maintained over period of 6 months, with a lower dropout rate in the workplace group than the clinical group. The literature on tobacco cessation suggests that most relapses occur within the first month of cessation, and that approximately 90% of the relapses occur within the first 6 months.[22] The reasons for this may be that the workplace group was more homogenous and cohesive and peer support in workplace group may be more effective than family support in the TCC group. Peer pressure has a vital role as a predisposing, reinforcing, and enabling factor for tobacco use. Thus, peer support may have a vital role in tobacco cessation. Further studies are warranted to explore the role of peer pressure in tobacco cessation as most of the previous reviews and studies are inconclusive.[23,24]
The primary finding, i.e., improved outcome in workplace setting than that in the clinical group, is in support with almost three-quarters of the previously conducted studies and meta-analysis.[25,26] There are few studies that showed contradictory findings, suggesting the non-effectiveness of workplace interventions.[21,27] However, these studies were uncontrolled, having poor inclusion and exclusion criteria, and other methodological issues. In addition, the recently published Cochrane review showed that there is strong evidence for some interventions (Individual/group counseling, pharmacological treatment) which increases the tobacco cessation rate in the workplace. Self-help group and social support are less effective in tobacco cessation. Out of the 57 reviewed trials, only 5 trials examined outcome with pharmacotherpy, despite having high quality of evidence; most of the trials included one or more intervention at the workplace.[21] In the present study, intensive, comprehensive, and multiple interventions were carried out at both the places, depending on indications in individual case, which may be the reason for higher success rate among the workplace group than the clinical group and previously conducted studies.[17,28,29] These findings supports previously conducted studies involving multiple interventions in the workplace seetings.[30,31]
Another important finding in the present study was that the TCC group participants were highly tobacco dependent than workplace group participants and the age of initiation of tobacco use was also lower among the TCC group participants than the workplace group participants. The early age of initiation of tobacco consumption and higher tobacco dependence may also be responsible for high failure rate and dropout in the TCC group than the workplace group in addition to various individual predictors such as sociodemographic variables (socioeconomic status and residence), number of quit attempts, motivational variables, and nicotine-related variables.[32,33] Tobacco cessation barriers include poor knowledge, lack of advice and support, lack of motivation, as well as intrapersonal, social, cultural, and financial factors.[34] Most of these barriers may be reduced or eliminated by multiple interventions carried out in our study such as pre-awareness session, focus group discussion, one-on-one counseling, and pharmacotherapy resulting in low dropout rate and adherence to the tobacco cessation program. Literature on tobacco cessation in workplace settings is mostly from western countries. Only few studies have been attempted in the Indian context, the second largest tobacco consumer in the world, with variable success.[35] The present study not only represents the success of workplace setting, but also of multiple interventions, as well as an intensive and integrated approach. In addition, workplace-based tobacco cessation interventions are cost effective.
Strengths and limitations
In the present study, there was no difference among the two groups for confounding factors such as sociodemographic variables and pharmacological intervention reflecting well-controlled and planned study design than previous studies. Still, the index study findings should be interpreted considering few limitations. The present study population represents a small sample size, open-label design, and only male employees from low socioeconomic status. Further large scale, multicentric, controlled studies are required to better understand the role of gender, peer pressure, and sociocultural factors in tobacco cessation outcome in the workplace settings among the Indian population.
CONCLUSION
Our study shows that multiple, intensive tobacco cessation interventions are more effective in workplace setting than the clinical setting (TCC). Peer support and regular follow-up in the workplace setting may be responsible to increase the success rate. Our study findings suggest that there is a need of expansion of existing clinic-based tobacco cessation services to workplace tobacco cessation services.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We are thankful to the Management of Industrial unit and employees for their active participation and support to the study.
REFERENCES
- 1.Bernstein SL. Tobacco-Related Illnesses and Management. Oncol Emer Med. 2016:97–105. [Google Scholar]
- 2.Thankappan KR. Tobacco cessation in India: A priority health intervention. Indian J Med Res. 2014;1394:484–6. [PMC free article] [PubMed] [Google Scholar]
- 3.Global Adult Tobacco Survey (GATS) India report 2009–2010 (Tobacco Free Initiative) Geneva: World Health Organization; 2011. [Last accessed on 2016 Sep 24]. Available from: http://www.searo.who.int/tobacco/documents/2010.pub2.pdf . [Google Scholar]
- 4.Jena PK, Kishore J, Sarkar BK. Global Adult Tobacco Survey (GATS): A case for change in definition, analysis and interpretation of “cigarettes” and “cigarettes per day” in completed and future surveys. Asian Pac J Cancer Prev. 2013;145:3299–304. doi: 10.7314/apjcp.2013.14.5.3299. [DOI] [PubMed] [Google Scholar]
- 5.Kumar MS, Sarma PS, Thankappan KR. Community-based group intervention for tobacco cessation in rural Tamil Nadu, India: A cluster randomized trial. J Subst Abuse Treat. 2012;431:53–60. doi: 10.1016/j.jsat.2011.10.026. [DOI] [PubMed] [Google Scholar]
- 6.Chapman S, MacKenzie R. The Global Research Neglect of Unassisted Smoking Cessation: Causes and Consequences. PLoS Med. 2010;72:e1000216. doi: 10.1371/journal.pmed.1000216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hu SS, Neff L, Agaku IT, Cox S, Day HR, Holder-Hayes E, et al. Tobacco Product Use Among Adults - United States, 2013-2014. MMWR Morb Mortal Wkly Rep. 2016;6527:685–91. doi: 10.15585/mmwr.mm6527a1. [DOI] [PubMed] [Google Scholar]
- 8.Jayakrishnan R, Mathew A, Uutela A, Auvinen A, Sebastian P. Multiple approaches and participation rate for a community based smoking cessation intervention trial in rural Kerala, India. Asian Pac J Cancer Prev. 2013;145:2891–6. doi: 10.7314/apjcp.2013.14.5.2891. [DOI] [PubMed] [Google Scholar]
- 9.Elshatarat RA, Yacoub MI, Khraim FM, Saleh ZT, Afaneh TR. Self-efficacy in treating tobacco use: A review article. Proc Singapore Healthcare. 2016;254:243–8. [Google Scholar]
- 10.Mony PK, Vishwanath N, Krishnan S. Tobacco use, attitudes and cessation practices among healthcare workers of a city health department in Southern India. J Family Med Prim Care. 2015;42:261. doi: 10.4103/2249-4863.154670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Varghese C, Kaur J, Desai NG, Murthy P, Malhotra S, Subbakrishna D, et al. Initiating tobacco cessation services in India: Challenges and opportunities. 2012. WHO South-East Asia J Pub Health. 2012;1:159–68. doi: 10.4103/2224-3151.206929. [DOI] [PubMed] [Google Scholar]
- 12.Murthy P, Saddichha S. Tobacco cessation services in India: recent developments and the need for expansion. Indian J Cancer. 2010;47(Suppl 1):69–74. doi: 10.4103/0019-509X.63873. [DOI] [PubMed] [Google Scholar]
- 13.Thankappan K. Tobacco cessation in India: A priority health intervention. Indian J Med Res. 2014;1394:484. [PMC free article] [PubMed] [Google Scholar]
- 14.Rigotti NA. Overview of smoking cessation management in adults 2016. [Last accessed on 2016 Sep 10]. Available from: http://www.uptodate.com/contents/overview-of-smoking-cessation-management-in-adults .
- 15.Abdullah AS, Driezen P, Quah AC, Nargis N, Fong GT. Predictors of smoking cessation behavior among Bangladeshi adults: Findings from ITC Bangladesh survey. Tob Induc Dis. 2015;131:1. doi: 10.1186/s12971-015-0050-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Patnode CD, Henderson JT, Thompson JH, Senger CA, Fortmann SP, Whitlock EP. Behavioral counseling and pharmacotherapy interventions for tobacco cessation in adults, including pregnant women: A review of reviews for the US Preventive Services Task Force. Ann Intern Med. 2015;1638:608–21. doi: 10.7326/M15-0171. [DOI] [PubMed] [Google Scholar]
- 17.Mishra GA, Majmudar PV, Gupta SD, Rane PS, Uplap PA, Shastri SS. Workplace tobacco cessation program in India: A success story. Indian J Occup Environ Med. 2009;133:146–53. doi: 10.4103/0019-5278.58919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mishra GA, Kulkarni SV, Majmudar PV, Gupta SD, Shastri SS. Community-based tobacco cessation program among women in Mumbai, India. Indian J Cancer. 2014;51(Suppl 1):S54–9. doi: 10.4103/0019-509X.147474. [DOI] [PubMed] [Google Scholar]
- 19.SRNT subcommittee on biological markers. Biochemical verification of tobacco use and cessation. Nicotine Tob Res. 2002;42:149–59. doi: 10.1080/14622200210123581. [DOI] [PubMed] [Google Scholar]
- 20.McGuffey JE, Wei B, Bernert JT, Morrow JC, Xia B, Wang L, et al. Validation of a LC-MS/MS method for quantifying urinary nicotine, six nicotine metabolites and the minor tobacco alkaloids-anatabine and anabasine-in smokers’ urine. PloS One. 2014;97:e101816. doi: 10.1371/journal.pone.0101816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cahill K, Lancaster T. Workplace interventions for smoking cessation. Cochrane Database Syst Rev. 2014;2:Cd003440. doi: 10.1002/14651858.CD003440.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hughes JR, Keely J, Naud S. Shape of the relapse curve and long-term abstinence among untreated smokers. Addiction. 2004;991:29–38. doi: 10.1111/j.1360-0443.2004.00540.x. [DOI] [PubMed] [Google Scholar]
- 23.Ford P, Clifford A, Gussy K, Gartner C. A Systematic Review of Peer-Support Programs for Smoking Cessation in Disadvantaged Groups. Int J Environ Res Publ. 2013;1011:5507–22. doi: 10.3390/ijerph10115507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.May S, West R. Do social support interventions (“buddy systems”) aid smoking cessation? A review. Tob Control. 2000;94:415–22. doi: 10.1136/tc.9.4.415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cahill K, Moher M, Lancaster T. Workplace interventions for smoking cessation. Cochrane Database Syst Rev. 2008;4:Cd003440. doi: 10.1002/14651858.CD003440.pub3. [DOI] [PubMed] [Google Scholar]
- 26.Curry SJ, McBride CM. Relapse prevention for smoking cessation: Review and evaluation of concepts and interventions. Ann Rev Publ Health. 1994;15:345–66. doi: 10.1146/annurev.pu.15.050194.002021. [DOI] [PubMed] [Google Scholar]
- 27.Wada K, Higuchi Y, Smith DR. Assessing the Impact of Nationwide Smoking Cessation Interventions among Employed, Middle-Aged Japanese Men, 2005-2010. PloS One. 2016;115:e0155151. doi: 10.1371/journal.pone.0155151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cruse S, Forster N, Thurgood G, Sys L. Smoking cessation in the workplace: Results of an intervention programme using nicotine patches. Occup Med. 2001;518:501–6. doi: 10.1093/occmed/51.8.501. [DOI] [PubMed] [Google Scholar]
- 29.Koffman DM, Lee JW, Hopp JW, Emont SL. The impact of including incentives and competition in a workplace smoking cessation program on quit rates. Am J Health Promot. 1998;132:105–11. doi: 10.4278/0890-1171-13.2.105. [DOI] [PubMed] [Google Scholar]
- 30.Naito M, Nakayama T, Okamura T, Miura K, Yanagita M, Fujieda Y, et al. Effect of a 4-year workplace-based physical activity intervention program on the blood lipid profiles of participating employees: The high-risk and population strategy for occupational health promotion (HIPOP-OHP) study. Atherosclerosis. 2008;1972:784–90. doi: 10.1016/j.atherosclerosis.2007.07.026. [DOI] [PubMed] [Google Scholar]
- 31.Chin DL, Hong O, Gillen M, Bates MN, Okechukwu CA. Heavy and Light/Moderate Smoking Among Building Trades Construction Workers. Publ Health Nurs. 2013;302:128–39. doi: 10.1111/j.1525-1446.2012.01041.x. [DOI] [PubMed] [Google Scholar]
- 32.Persai D, Panda R, Gupta A. Examining Implementation of Tobacco Control Policy at the District Level: A Case Study Analysis from a High Burden State in India. Adv Prev Med 2016. 2016:8. doi: 10.1155/2016/4018023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Shmulewitz D, Stohl M, Keyes KM, Brown Q, Saha TD, Hasin D. Effects of state-level tobacco environment on cigarette smoking are stronger among those with individual-level risk factors. Nicotine Tob Res. 2016;10:2020–30. doi: 10.1093/ntr/ntw114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pagano A, Tajima B, Guydish J. Barriers and facilitators to tobacco cessation in a nationwide sample of addiction treatment programs. J Subst Abuse Treat. 2016;67:22–9. doi: 10.1016/j.jsat.2016.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mishra GA, Pimple SA, Shastri SS. An overview of the tobacco problem in India. Indian J Med Paediatr Oncol. 2012;333:139–45. doi: 10.4103/0971-5851.103139. [DOI] [PMC free article] [PubMed] [Google Scholar]


