Abstract
Previous reports have identified an association between cognitive impairment and genetic variation in psychotic disorders. In particular, this association may be related to abnormal regulation of genes responsible for broad cognitive functions such as the oxytocin receptor (OXTR). Within psychotic disorders, it is unknown if OXTR methylation, which can have important implications for gene regulation, is related to cognitive function. The current study examined peripheral blood OXTR methylation and general cognition in people with schizophrenia, schizoaffective disorder, and psychotic disorder not otherwise specified (N = 101). Using hierarchical multiple regression analysis, methylation at the Chr3:8767638 site was significantly associated with composite cognitive performance independent of demographic and medication factors while controlling for multiple testing in this combined diagnostic sample (adjusted p = 0.023).
Key Words: Psychosis, Cognition, Oxytocin receptor, Methylation
Introduction
The neuropeptide oxytocin is associated with broad cognitive processes in humans. Previous findings indicate that both general and social cognitive processes such as working memory and facial emotion recognition, respectively, are related to oxytocin function [1,2,3,4]. Within psychotic disorders such as schizophrenia, broad cognitive deficits have been well documented [5,6,7,8], and oxytocin abnormalities may contribute to these deficits. Further, the link between social cognition and oxytocin in psychotic disorders has garnered attention due to treatment implications (e.g., intranasal oxytocin may improve facial emotion recognition) [9,10,11]. Recent evidence suggests that intranasal oxytocin may also improve general cognition in schizophrenia [12,13,14,15]. In addition, genetic variants of the oxytocin receptor gene (OXTR), which serves as the binding point for oxytocin action through second messenger systems in the brain, have been linked to a diagnosis of schizophrenia [16] and poorer cognitive performance in psychotic disorders [17,18]. Thus, the genetic regulation of oxytocin pathways via deoxyribonucleic acid (DNA) variation, and its relationship to cognition in schizophrenia continues to be an active area of research [for review, see [19]]. While recent reports have identified a relationship between increased OXTR methylation and impaired facial emotion recognition in schizophrenia [20], there have been no studies of OXTR gene regulation through DNA methylation and general cognitive performance in psychotic disorders. It is possible that oxytocin system abnormalities in psychosis may extend to OXTR methylation, and this abnormality may be related to broad cognitive deficits. If true, it would suggest that OXTR gene regulation is a potential treatment target for cognitive deficits in people with psychosis.
Therefore, the current study aimed to investigate the relationship of OXTR DNA methylation and general cognition in a sample of participants with schizophrenia, schizoaffective disorder, or psychotic disorder not otherwise specified. We hypothesized that site-specific OXTR DNA methylation would be associated with cognitive performance across participants.
Methods
Participants
Participants were recruited from the southeastern Michigan area based on the following inclusion criteria for a separate study examining the metabolic side effects of antipsychotic medications in people with a psychotic disorder: (1) Diagnostic and Statistical Manual for Mental Disorders (DSM-IV) [21] Axis I diagnosis of schizophrenia, schizoaffective disorder, schizophreniform disorder, or psychotic disorder not otherwise specified, (2) between the age of 18 and 90, and (3) at least 6 months of stable atypical or typical antipsychotic medication dosage (atypical antipsychotics included risperidone, olanzapine, quetiapine, ziprasidone, aripiprazole, clozapine, paliperidone, iloperidone, asenapine, and lurasidone; typical antipsychotics included haloperidol, fluphenazine, perphenazine, trifluoperazine, chlorpromazine, thioridazine, and thiothixene). Participants were excluded based on the following criteria: (1) diagnosed with type 2 diabetes prior to treatment with antipsychotic medications (criterion required for separate study examining metabolic side effects), and (2) active DSM-IV substance abuse diagnosis. Included participants completed a single visit to undergo a fasting blood draw, comprehensive medication history (relevant to the study of metabolic side effects), diagnostic assessment using the Structured Clinical Interview for DSM-IV (SCID-IV) [22], and cognitive testing. All evaluations were carried out by a single trained research associate. In addition, level of education and smoking history were obtained. Smoking history was assessed by asking the participants if they smoked one or more cigarettes per day. Self-report measures of depression (i.e., Beck Depression Inventory-Revised) [23], psychological stress (i.e., Psychological Stress Index) [24], and state anxiety (i.e., State-Trait Anxiety Inventory) [25] were completed to assess current mood and anxiety. Clinical assessments of current psychotic symptoms were not collected due to time limitations. All participants gave fully informed consent to participate in the protocol, as approved by the University of Michigan Institutional Review Board.
DNA Methylation Analysis
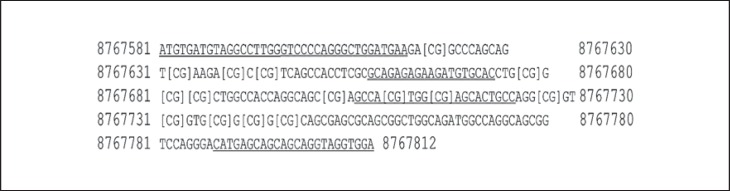
DNA was first extracted using the salt precipitation method [26] and cleaned and concentrated using commercially available kits. Five hundred nanograms of DNA was then bisulfite converted using the EZ DNA Methylation-Gold Kit (Zymo Research, Irvine, Calif., USA). Ten nanograms of bisulfite-converted DNA was placed in a touchdown PCR reaction containing OneTaq Hot Start 2× Master Mix with Standard Buffer (New England BioLabs, Ipswitch, Mass., USA) in order to amplify our chosen OXTR region of interest. Specifically, the 232-bp region is contained within the 3rd exon of the OXTR gene and covered the coordinates Chr3:8767580 - 8767812 (using the GRCh38/hg38 build). Methylation within and immediately adjacent to this region has been investigated in several brain-based disease states [27,28,29,30,31,32]. The studied region is contained within a CpG Island of the OXTR gene that spans from approximately 20 to 2,350 bp downstream of the transcription start site. Differential methylation of this CpG region has been shown to have large functional effects on OXTR expression [30,33]. Within our target amplicon, 15 CpG methylation sites were chosen for analysis by the method of pyrosequencing using three separate pyrosequencing primers for the amplicon [34]. Other CpG methylation sites within the amplicon were not included for the following reasons: (1) the assay design for the region was not included (dictated by the software), and (2) a detectable methylation value was not replicated in ≥66% of the sample. Methylation calls for individual samples were excluded if the replication methylation value was too variable (defined as a coefficient of variation >2.5%) and thus deemed unreliable. The 15 methylation calls that were included for analysis were normalized using the method of Goodrich et al. [35]. Briefly, this method uses methylation standards (0, 20, 40, 60, 80, and 100% methylated) for each analysis in order to construct a standardized curve on which each sample is normalized. Figure 1 shows the amplicon region, primers used, and methylation sites analyzed. All primers were designed using the Pyromark AssayDesgin 2.0 software.
Fig. 1.
Figure 1 shows the OXTR amplicon analyzed in the current study. This amplicon is contained within exon 3 of the OXTR gene downstream to the translation start site. The sequence is displayed using the GRCh38/Hg38 build coordinates Chr3:8767581 - Chr3:87677812. The 19-nucleotide forward primer used for the amplicon is single underlined starting at 8767581 and ending at 8767599, and the 24-nucleotide reverse primer is single underlined from 8767789 to 8767812. The reverse primer was ordered as the reverse complimentary primer and was biotinylated to facilitate pyrosequencing. The three sequencing primers are double underlined and found starting at positions 8767599 (19 nucleotides), 8767656 (19 nucleotides), and 8767704 (20 nucleotides). Analyzed CpG methylation sites are shown bracketed (15 total).
Cognition
Cognitive performance was determined using the Brief Assessment of Cognition in Schizophrenia (BACS), a performance-based battery of cognition with six subscale scores, including Verbal Memory, Digit Sequencing (working memory), Token Motor Task (motor speed), Verbal Fluency, Symbol Coding (attention and speed of information processing), and Tower of London (executive functions) [36,37]. In order to standardize and interpret BACS performance, z-scores were computed with reference to a sample of healthy controls who also lived in Southeastern Michigan (n = 63) and are described in Grove et al. [38]. The BACS provides a composite score to describe overall cognitive performance. This score is analyzed in a ‘whole model’ approach where, in the current study, a significant relationship between BACS composite score and methylation site warrants further analysis of the subscale scores.
Statistical Analyses
Demographic and clinical characteristics are described by means with standard deviation. Differences between the healthy control sample (used to compute BACS z-scores) and participants with a psychotic disorder were determined using independent samples t-tests or χ2 analyses. The healthy controls did not have methylation data available and were not included in methylation analyses. Pearson correlational analyses were used to identify significant associations between BACS z-scores (composite score first and then followed by subscale scores if necessary) and methylation sites. Hierarchical multiple regression models were used to determine if a specific OXTR methylation site (i.e., identified from significant Pearson correlational analyses) would be associated with BACS composite z-scores independent of variables related to cognition and methylation. The regression models contained two steps. The first step included level of education, with a ranking of 1 (grade 6 or less) to 8 (completed graduate/professional school), as educational attainment has been consistently associated with cognition in schizophrenia [39,40]. In addition, considering that epigenetics can be mediated by antipsychotic medication type (i.e., atypical or typical) and cigarette smoking, both of which may play an important role in the pathophysiology of schizophrenia [41,42,43], antipsychotic type and cigarette smoking status (current smoker or nonsmoker) were also included as independent variables in the first step of the models. A methylation site that significantly correlated with BACS composite z-score was entered as an independent variable in the second and final step of the models. Within all models, standardized betas are reported, along with p values for the amount of variance in the BACS z-score explained by the individual methylation site compared with demographic and medication variables. These values were corrected using Benjamini and Hochberg's False Discovery Rate (threshold of 0.05) [44,45,46], which has been recommended as an alternative to the conservative Bonferroni correction for clinical studies. In addition, due to the nonnormal distribution of methylation data, all methylation results were log transformed for statistical analyses. While power analysis was not conducted due to the lack of previous studies examining OXTR methylation and cognition in psychotic disorders needed to estimate the effect size, the current sample size is comparable or larger than previous OXTR methylation studies of clinical populations and psychiatric symptoms [28,29,47,48,49,50]. JMP statistical software (SAS Institute Inc., Cary, N.C., USA) was used for all analyses.
Results
Demographic, Clinical, and Cognitive Characteristics
Demographic, clinical, and cognitive characteristics of the 101 participants with a psychotic disorder are presented in table 1. Compared to the healthy control sample used to compute BACS z-scores [n = 63; average age of 43.5 ± 11.3; age range of 19-66; 65% male (n = 41); Bachelor's degree level of education 6.1 ± 1.8, and 70% Caucasian (n = 46)], participants with a psychotic disorder had a significantly lower level of education [t(151) = 8.71, p < 0.0001] and a significantly higher ratio of non-Caucasian participants (χ2 = 9.47, n = 160, p = 0.002).
Table 1.
Demographic, clinical, cognitive, and physiological characteristics of all clinical participants (i.e., n = 101)
| Age, years | 19 to 71 | 45.4 ± 10.7 |
| Gender | ||
| Male | – | 56 (55) |
| Female | – | 45 (45) |
| Race | ||
| Caucasian | – | 54 (53) |
| African-American | – | 45 (45) |
| Other | – | 5 (5) |
| Level of education (n = 91) | 1 to 8 | 3.9 ± 1.3 |
| DSM-IV Axis I diagnosis | ||
| Schizophrenia | – | 32 (32) |
| Schizoaffective disorder | – | 59 (58) |
| Psychotic disorder NOS | – | 10 (10) |
| Age at diagnosis, years | 16 to 64 | 26.4 ± 9.5 |
| Duration of illness, years | 1 to 44 | 19.0 ± 11.3 |
| Hospitalizations, lifetime | 0 to 44 | 8.9 ± 10.1 |
| Beck Depression Inventory-Revised (n = 94) | 0 to 63 total | 14.95 ± 11.29 |
| Psychological Stress Index (n = 94) | 0 to 4 average | 2.19 ± 0.71 |
| Social Adjustment Scores-Self-Report (n = 95) | 0 to 5 average | 2.24 ± 0.54 |
| BACS composite z-score (n = 94)a | –4.83 to 0.42 | –1.92 ± 1.06 |
| Verbal Memory | –3.85 to 1.44 | –1.35 ± 1.09 |
| Digit Sequencing | –5.95 to 1.66 | –1.41 ± 1.26 |
| Token Motor Task (n = 99) | –5.48 to 1.43 | –1.61 ± 1.24 |
| Verbal Fluency | –4.14 to 1.07 | –1.06 ± 0.91 |
| Symbol Coding (n = 98) | –3.97 to 0.72 | –1.56 ± 0.93 |
| Tower of London (n = 96) | –4.29 to 1.36 | –1.19 ± 1.29 |
| Current cigarette smoker | – | 52 (51.5) |
| Packs of cigarettes per year | 37 to 1,095 | 86.8 ± 123.0 |
| Atypical antipsychotic | – | 91 (90) |
| Typical antipsychotic | – | 19 (18.8) |
| Daily chlorpromazine equivalents, mg | 25 to 3,175 | 530.6 ± 517.9 |
Note: data are presented as range, mean ± SD, or n (%). NOS = Not otherwise specified.
Computation of BACS z-scores utilized a healthy control comparison group.
Relationships between BACS and OXTR Methylation
The average, nontransformed values of the analyzed OXTR methylation sites are listed in table 2. Overall, the investigated sites were ‘lowly’ methylated (average methylation of sites ∼20%), which is in agreement with healthy control studies investigating OXTR methylation within and near this region [29,32].
Table 2.
Nontransformed methylation of OXTR sites
| No. | Site | n | Mean ± SD |
|---|---|---|---|
| 1 | Chr 3:8767620 | 91 | 17.3 ± 8.2 |
| 2 | Chr 3:8767632 | 89 | 23.9 ± 10.8 |
| 3 | Chr 3:8767638 | 80 | 17.3 ± 8.8 |
| 4 | Chr 3:8767641 | 77 | 20.4 ± 13.1 |
| 5 | Chr 3:8767678 | 91 | 21.9 ± 7.7 |
| 6 | Chr 3:8767681 | 92 | 17.6 ± 8.1 |
| 7 | Chr 3:8767683 | 88 | 12.3 ± 7.1 |
| 8 | Chr 3:8767701 | 85 | 21.3 ± 8.7 |
| 9 | Chr 3:8767708 | 68 | 11.1 ± 4.8 |
| 10 | Chr 3:8767713 | 67 | 21.4 ± 9.4 |
| 11 | Chr 3:8767727 | 91 | 20.6 ± 9.9 |
| 12 | Chr 3:8767731 | 89 | 14.6 ± 9.5 |
| 13 | Chr 3:8767736 | 90 | 20.6 ± 13.0 |
| 14 | Chr 3:8767739 | 80 | 19.7 ± 13.2 |
| 15 | Chr 3:8767742 | 81 | 13.0 ± 6.8 |
| Overall methylation | – | 92 | 18.2 ± 5.9 |
Note: chromosomal locations using Human Genome build 38.
A significant negative Pearson correlation was observed between Chr 3:8767638 site and BACS composite z-score. Neighboring methylation sites (i.e., Chr 3:8767708, Chr 3:8767681, and Chr 3:8767632), along with the remaining methylation sites, were not significantly correlated with BACS composite z-score except for Chr 3:8767742, which was positively correlated (table 3).
Table 3.
Pearson correlations between BACS and log-transformed OXTR methylation
|
OXTR methylation |
BACS |
|||||||
|---|---|---|---|---|---|---|---|---|
| No. | site | Composite | Verbal Memory | Digit Sequencing | Token Motor Task | Verbal Fluency | Symbol Coding | Tower of London |
| 1 | Chr 3:8767620 | –0.05 | –0.02 | –0.11 | 0.11 | 0.03 | –0.13 | –0.10 |
| 2 | Chr 3:8767632 | –0.13 | –0.12 | –0.21* | 0.11 | –0.10 | –0.23* | –0.03 |
| 3 | Chr 3:8767638 | –0.25* | –0.25* | –0.20 | 0.07 | –0.17 | –0.24* | –0.27* |
| 4 | Chr 3:8767641 | 0.08 | –0.01 | –0.01 | 0.16 | 0.11 | 0.05 | –0.02 |
| 5 | Chr 3:8767678 | –0.06 | –0.12 | –0.12 | 0.09 | –0.02 | –0.16 | 0.04 |
| 6 | Chr 3:8767681 | –0.08 | –0.03 | –0.25** | –0.05 | 0.04 | –0.05 | –0.05 |
| 7 | Chr 3:8767683 | –0.01 | –0.03 | –0.10 | 0.16 | 0.02 | –0.10 | –0.02 |
| 8 | Chr 3:8767701 | 0.12 | 0.05 | 0.02 | 0.27* | 0.00 | 0.03 | 0.08 |
| 9 | Chr 3:8767708 | –0.12 | –0.17 | –0.24 | 0.13 | –0.11 | –0.17 | 0.01 |
| 10 | Chr 3:8767713 | –0.02 | –0.16 | –0.15 | 0.17 | 0.02 | –0.08 | 0.10 |
| 11 | Chr 3:8767727 | –0.05 | –0.02 | –0.11 | 0.11 | 0.03 | –0.13 | –0.10 |
| 12 | Chr 3:8767731 | 0.02 | –0.06 | –0.04 | 0.19 | 0.07 | –0.13 | 0.02 |
| 13 | Chr 3:8767736 | –0.03 | –0.11 | 0.05 | 0.07 | 0.05 | –0.13 | –0.06 |
| 14 | Chr 3:8767739 | 0.04 | –0.04 | 0.09 | 0.13 | 0.05 | –0.07 | –0.03 |
| 15 | Chr 3:8767742 | 0.25* | 0.12 | 0.18 | 0.29** | 0.16 | 0.16 | 0.10 |
| Overall methylation | - | -0.02 | -0.10 | -0.08 | 0.19 | 0.03 | -0.09 | -0.05 |
Note: Pearson correlation coefficients between the log-transformed methylation of the OXTR gene (rows) and BACS z-scores (columns).
p < 0.05,
p < 0.01.
Given the significant findings at Chr3:8767638 and Chr3:8767742, we conducted separate hierarchical regression analyses for each site. The multiple regression analyses showed that only OXTR methylation site Chr3:8767638 explained a significant amount of variance in BACS composite z-score, along with Verbal Memory, Symbol Coding, and Tower of London z-scores, independent of level of education, antipsychotic type, and smoking status, even after correcting for multiple testing (table 4). The association between Chr3:8767742 and BACS composite z-score did not remain significant after accounting for level of education, antipsychotic type, and smoking status (ΔR2 = 0.04, ΔF = 3.19, β = 0.19, p = 0.079). Consequently, Chr3:8767742 and BACS subscale z-scores were not analyzed with hierarchical regression models.
Table 4.
Results from the hierarchical regression models used to predict the effect of Chr3:8767638 OXTR methylation on BACS performance (n = 72)
| BACS | Step 1 |
Step 2 |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| variable statistics, ß |
model statistics |
variable statistics, ß |
model statistics | ||||||
| level of education | antipsychotic type | current smoker | ΔR2 | AF | Chr3:8767638 | ΔR2 | ΔF | FDR- adjusted p value | |
| Composite | 0.30* | –0.18 | 0.17 | 0.15 | 4.03* | –0.31* | 0.09 | 7.89* | 0.023 |
| Verbal Memory | 0.29 | –0.21* | 0.14 | 0.15 | 4.10* | –0.29* | 0.08 | 6.84* | 0.023 |
| Digit Sequencing | 0.30* | –0.20 | 0.10 | 0.15 | 3.83* | –0.20 | 0.04 | 3.20 | 0.062 |
| Token Motor Task | 0.09 | –0.14 | –0.02 | 0.03 | 0.69 | 0.00 | 0.00 | 0.00 | 0.600 |
| Verbal Fluency | –0.07 | –0.01 | 0.16 | 0.03 | 0.75 | –0.21 | 0.04 | 3.00 | 0.062 |
| Symbol Coding | 0.22 | 0.00 | 0.04 | 0.05 | 1.12 | –0.27* | 0.07 | 5.06* | 0.029 |
| Tower of London | 0.29* | –0.09 | 0.25* | 0.14 | 3.72* | –0.27* | 0.07 | 6.04* | 0.024 |
Note: BACS composite and subscale z-scores were included as the dependent variable. Level of education, antipsychotic type (atypical or typical), and cigarette smoking status (Step 1) and methylation value (Step 2) were entered as independent variables for each model. The false discovery rate (FDR)-adjusted p values were calculated for the Step 2 variable (Chr3:8767638 site) only. Standardized betas are reported.
p < 0.05.
Discussion
Oxytocin Methylation and Cognition
Within the current study, a significant negative association was observed between CpG methylation at Chr 3:8767638 in the OXTR gene and cognitive performance independent of demographic and antipsychotic medication variables in people with schizophrenia, schizoaffective disorder, or psychotic disorder not otherwise specified. Specifically, cognitive deficits in domains such as working memory, attention and speed of information processing, and executive functions may be related to peripheral abnormal OXTR DNA methylation in people with a psychotic disorder.
To our knowledge, this is the first study to investigate OXTR gene methylation and general cognition in people with a psychotic disorder. A previous study has examined facial emotion recognition in people with a psychotic disorder (at site −934 upstream of the OXTR start codon in DNA and the same CpG island as the region in the current study), and found increased OXTR methylation in females, but not males, was associated with greater difficulties identifying angry, sad, and happy faces [20]. In the current study, the association between OXTR methylation and cognition was observed independent of sex. Previous studies have also examined OXTR methylation and social cognition in psychiatrically healthy participants and found that higher degrees of OXTR methylation were associated with greater activation of the superior temporal gyrus/supramarginal gyrus and dorsal anterior cingulate cortex during an animacy task [32]. Further, increased OXTR methylation was associated with higher neural response and decreased functional coupling within brain regions supporting socioemotional processing (i.e., amygdala, fusiform, and insula) [31]. While OXTR methylation in these two studies was assessed in a neighboring region compared to the current study, the methylation regions analyzed in these studies were still contained within the same CpG Island. In conjunction, these findings suggest that decreased OXTR methylation in this CpG Island may contribute to both lower- and higher-level cognitive processing (e.g., working memory and facial emotion recognition, respectively). Yet within psychotic disorders, the relationship between the oxytocin system and cognition is inconsistent. The Psychiatric Genomic Consortium (PGC) did not identify oxytocin (OXT) or OXTR as risk factors for schizophrenia via a genomic-wide association analysis [51]. However, this may be due to oxytocin pathway genes not being implicated in the susceptibility to a psychotic disorder, but rather susceptibility to impaired social behavior (i.e., emotional withdrawal) within the PGC sample [52]. In addition, the role of the oxytocin system in the pathophysiology of positive, negative, and cognitive symptoms continues to be implicated [13,53].
The mechanism by which abnormal oxytocin methylation influences cognition may be explained by biological models that indicate perinatal stress disrupts the oxytocin system in brain areas associated with numerous cognitive processes (e.g., memory retrieval, decision-making, and social cognition) [54,55]. Specifically, increased methylation of OXTR may lead to abnormal gene expression that disrupts hippocampal and/or medial prefrontal cortex function and causes cognitive impairment (e.g., memory deficits and/or impaired emotion recognition) [see [56] for a review]. This disruption may be exacerbated by psychosocial stressors, which can increase OXTR methylation [28]. Considering that OXTR methylation at Chr 3:8767638 was significantly associated with working memory, processing speed, and executive functions, abnormal activation in associated areas (e.g., prefrontal cortex and related substructures) [57,58,59,60,61] may be linked to decreased peripheral OXTR methylation in people with a psychotic disorder. However, future neuroimaging studies with patients and healthy control populations are needed to determine this potential relationship between OXTR methylation and brain function in psychosis. Thus, while further research is needed to confirm these postulations and resolve discrepant findings, abnormal oxytocin methylation in the periphery and the brain may not only contribute to impaired socioemotional processing in psychosis [20], but also general cognitive deficits in psychotic disorders, making OXTR methylation a potential biomarker or treatment target.
Previous reports also indicate that OXTR methylation in overlapping regions of interest is associated with social anxiety disorder [29]. Specifically, elevated Chr3:8767736 methylation and reduced Chr3:8767708 methylation in participants with social anxiety disorder compared with healthy controls was observed [29]. In the current study, no significant correlations were observed between Chr3:8767708 methylation and BACS composite or subscale scores. However, the previous report highlights the importance of OXTR methylation at individual sites, which has apparent variable methylation in association with a given phenotype and may contribute to different disease pathophysiology (i.e., psychotic disorder vs. social anxiety disorder).
Understanding the Influence of Environmental and Lifestyle Factors on Cognition
The potentially positive cognitive effects of nicotine obtained through cigarette smoking in schizophrenia are well documented [62,63], along with the potential role for nicotinic receptors in cognition [64]. The effect of smoking on DNA methylation has been observed in several populations [65,66,67]. Additionally, cigarette smoking has been found to affect OXTR gene regulation and transcription in pregnant women [68]. Yet the current findings suggest smoking may not impact the associations between OXTR methylation and cognition in people with a psychotic disorder, as OXTR methylation explained BACS composite variance independent of smoking status. Further, besides the environmental effect of smoking, cardiovascular function plays an important role in cognition [69,70,71]. Future work may investigate the methylation of known genes that contribute to cardiovascular function in schizophrenia (e.g., methylenetetrahydrofolate reductase) for their role in the relationship between cardiovascular health and cognition in psychotic disorders [72,73,74].
Limitations
The current study was observational in nature, and only associations can be inferred. Considering the critical need for replication of the current findings, future prospective studies could not only replicate but also expand upon the current findings by assessing coincident changes in gene methylation and cognition in psychotic disorders coupled with brain imaging during disease progression and/or treatment to explore casual relationships. While the current study used a candidate epigenetic approach and investigated a single area of a single gene, along with False Discovery Rate correction to reduce the chance of type 1 errors, few correlations were observed between cognition and gene methylation. Associations between cognition and gene methylation of other genes will need to be tested independently in future studies. Further, consequences of gene methylation through RNA studies and downstream protein levels will need to be assessed to understand the molecular effects of differential gene methylation in cognitive processes. However, as described earlier, differential methylation of the CpG Island that contained the current methylation sites has been linked to significant effects in OXTR expression and oxytocin levels [75]. A limitation of the current study is not assessing DNA methylation at the tissue of interest, which in this case would be the brain. A future study using available postmortem human brain samples could have some benefits but would not be without significant limitations of its own. Such limitations may include epigenetic changes that could occur from death to tissue processing, accurate phenotyping of subjects at the time of death (e.g., disease status, medication use, lifestyle factors, cognitive status, etc.), and choosing specific brain regions to analyze OXTR DNA methylation. The current study did not use postmortem brain samples to validate the peripheral blood findings due to a lack of sample access. However, the use of peripheral tissues to study brain genetic regulation is an important initial strategy [76,77,78], and previously reported correlations between OXTR methylation in peripheral blood mononuclear cells and the brain suggest that peripheral methylation may be related to brain function [79]. Additionally, the use of peripheral blood DNA methylation can have significant biomarker value regardless of it not being from the tissue of interest. Nevertheless, preclinical models of cognition in schizophrenia are available [80] and may enable translational studies that can be used to support epigenetic findings in the peripheral blood from humans.
The correlation of DNA methylation across tissues continues to be an active area of research, and correlations between OXTR peripheral blood methylation and the temporal cortex have been reported, suggesting that there may be some degree of similarity [50]. Although likely gene dependent, work in animals and humans continues to support translatability between peripheral blood and brain DNA methylation [81,82,83,84]. Nevertheless, correlating site-specific peripheral methylation findings to the brain may be required. As studies continue to assess DNA methylation in the periphery, it is important that similar extraction and assessment methodologies are used in order to test replication of any findings put forth. Finally, although limited in sample size, significant associations remained after correction for multiple testing. However, larger sample sizes with better demographically matched controls than the current study (along with cognition and methylation data for both cases and controls) may allow for replication of these analyses within and across DSM-IV diagnostic groups. Between-group analyses within the current sample are limited by the small number of participants diagnosed with psychotic disorder not otherwise specified (i.e., 10 participants). In addition, the current study did not assess psychotic symptoms, and future studies should explore the relationship between OXTR methylation and the severity of psychosis, as previous reports indicate a relationship between OXTR variants and a diagnosis of schizophrenia [16].
Conclusion
Methylation levels of the OXTR gene at the Chr 3:8767638 site are negatively associated with general cognitive performance in people with a psychotic disorder (i.e., schizophrenia, schizoaffective disorder, or psychotic disorder not otherwise specified). This association is independent of demographic and antipsychotic medication type, and remains after adjusting for multiple testing, suggesting that abnormal OXTR methylation may contribute to the cognitive deficits and pathophysiology of psychotic disorders.
Statement of Ethics
The authors have no ethical conflicts to disclose.
Disclosure Statement
Stephan F. Taylor has a research contract with St. Jude Medical and receives research support from Neuronetics. All other authors declare that they have no conflicts of interest.
Acknowledgement
The authors thank the staff and consumers at the Washtenaw County Health Organization, Ann Arbor Veterans Affairs Medical Center, and the Detroit-Wayne County Community Mental Health Agency for their assistance and participation, respectively, in the current study. In addition, this study was supported by grants from The National Institute of Mental Health (R01MH082784, DK020572, and 2UL1TR000433), the National Center for Advancing Translational Sciences of the National Institutes of Health (2UL1TR000433-06), and the Chemistry Core of the Michigan Diabetes Research and Training Center (DK020572) from the National Institute of Diabetes and Digestive and Kidney Diseases. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
References
- 1.Kirsch P, Esslinger C, Chen Q, Mier D, Lis S, Siddhanti S, Gruppe H, Mattay VS, Gallhofer B, Meyer-Lindenberg A. Oxytocin modulates neural circuitry for social cognition and fear in humans. J Neurosci. 2005;25:11489–11493. doi: 10.1523/JNEUROSCI.3984-05.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Meyer-Lindenberg A, Domes G, Kirsch P, Heinrichs M. Oxytocin and vasopressin in the human brain: social neuropeptides for translational medicine. Nat Rev Neurosci. 2011;12:524–538. doi: 10.1038/nrn3044. [DOI] [PubMed] [Google Scholar]
- 3.Cochran DM, Fallon D, Hill M, Frazier JA. The role of oxytocin in psychiatric disorders: a review of biological and therapeutic research findings. Harv Rev Psychiatry. 2013;21:219–247. doi: 10.1097/HRP.0b013e3182a75b7d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chini B, Leonzino M, Braida D, Sala M. Learning about oxytocin: pharmacologic and behavioral issues. Biol Psychiatry. 2014;76:360–366. doi: 10.1016/j.biopsych.2013.08.029. [DOI] [PubMed] [Google Scholar]
- 5.Keefe RS. The longitudinal course of cognitive impairment in schizophrenia: an examination of data from premorbid through posttreatment phases of illness. J Clin Psychiatry. 2014;75(suppl 2):8–13. doi: 10.4088/JCP.13065su1.02. [DOI] [PubMed] [Google Scholar]
- 6.Nuechterlein KH, Ventura J, Subotnik KL, Bartzokis G. The early longitudinal course of cognitive deficits in schizophrenia. J Clin Psychiatry. 2014;75(suppl 2):25–29. doi: 10.4088/JCP.13065.su1.06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kurtz MM. Neurocognitive impairment across the lifespan in schizophrenia: an update. Schizophr Res. 2005;74:15–26. doi: 10.1016/j.schres.2004.07.005. [DOI] [PubMed] [Google Scholar]
- 8.Stirling J. Neurocognitive function and outcome in first-episode schizophrenia: a 10-year follow-up of an epidemiological cohort. Schizophr Res. 2003;65:75–86. doi: 10.1016/s0920-9964(03)00014-8. [DOI] [PubMed] [Google Scholar]
- 9.Woolley JD, Chuang B, Lam O, Lai W, O'Donovan A, Rankin KP, Mathalon DH, Vinogradov S. Oxytocin administration enhances controlled social cognition in patients with schizophrenia. Psychoneuroendocrinology. 2014;47:116–125. doi: 10.1016/j.psyneuen.2014.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Averbeck BB, Bobin T, Evans S, Shergill SS. Emotion recognition and oxytocin in patients with schizophrenia. Psychol Med. 2011:1–8. doi: 10.1017/S0033291711001413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Davis MC, Lee J, Horan WP, Clarke AD, McGee MR, Green MF, Marder SR. Effects of single dose intranasal oxytocin on social cognition in schizophrenia. Schizophr Res. 2013;147:393–397. doi: 10.1016/j.schres.2013.04.023. [DOI] [PubMed] [Google Scholar]
- 12.Feifel D, Macdonald K, Cobb P, Minassian A. Adjunctive intranasal oxytocin improves verbal memory in people with schizophrenia. Schizophr Res. 2012;139:207–210. doi: 10.1016/j.schres.2012.05.018. [DOI] [PubMed] [Google Scholar]
- 13.Feifel D, Shilling PD, MacDonald K. A review of oxytocin's effects on the positive, negative, and cognitive domains of schizophrenia. Biol Psychiatry. 2016;79:222–233. doi: 10.1016/j.biopsych.2015.07.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bakermans-Kranenburg MJ, van I Jzendoorn MH. Sniffing around oxytocin: review and meta-analyses of trials in healthy and clinical groups with implications for pharmacotherapy. Transl Psychiatry. 2013;3:e258. doi: 10.1038/tp.2013.34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Michalopoulou PG, Averbeck BB, Kalpakidou AK, Evans S, Bobin T, Kapur S, Shergill SS. The effects of a single dose of oxytocin on working memory in schizophrenia. Schizophr Res. 2015;162:62–63. doi: 10.1016/j.schres.2014.12.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Montag C, Brockmann EM, Bayerl M, Rujescu D, Muller DJ, Gallinat J. Oxytocin and oxytocin receptor gene polymorphisms and risk for schizophrenia: a case-control study. World J Biol Psychiatry. 2013;14:500–508. doi: 10.3109/15622975.2012.677547. [DOI] [PubMed] [Google Scholar]
- 17.Davis MC, Horan WP, Nurmi EL, Rizzo S, Li W, Sugar CA, Green MF. Associations between oxytocin receptor genotypes and social cognitive performance in individuals with schizophrenia. Schizophr Res. 2014;159:353–357. doi: 10.1016/j.schres.2014.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schmidt SJ, Mueller DR, Roder V. Social cognition as a mediator variable between neurocognition and functional outcome in schizophrenia: empirical review and new results by structural equation modeling. Schizophr Bull. 2011;37(suppl 2):S41–S54. doi: 10.1093/schbul/sbr079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bartholomeusz CF, Ganella EP, Labuschagne I, Bousman C, Pantelis C. Effects of oxytocin and genetic variants on brain and behaviour: implications for treatment in schizophrenia. Schizophr Res. 2015;168:614–627. doi: 10.1016/j.schres.2015.06.007. [DOI] [PubMed] [Google Scholar]
- 20.Rubin LH, Connelly JJ, Reilly JL, Carter CS, Drogos LL, Pournajafi-Nazarloo H, Ruocco AC, Keedy SK, Matthew I, Tandon N, Pearlson GD, Clementz BA, Tamminga CA, Gershon ES, Keshavan MS, Bishop JR, Sweeney JA. Sex and diagnosis specific associations between DNA methylation of the oxytocin receptor gene with emotion processing and temporal-limbic and prefrontal brain volumes in psychotic disorders. Biol Psychiatry. 2016;1:141–151. doi: 10.1016/j.bpsc.2015.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. ed 4. Washington: American Psychiatric Association; 2000. [Google Scholar]
- 22.First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders SCID-I: Clinician Version, Administration Booklet. Washington: American Psychiatric Press; 1997. [Google Scholar]
- 23.Beck AT, Steer RA. Manual for the Beck Depression Inventory. 1993 edition. San Antonio: The Psychological Corporation; 1987. [Google Scholar]
- 24.Tso IF, Grove TB, Taylor SF. Self-assessment of psychological stress in schizophrenia: preliminary evidence of reliability and validity. Psychiatry Res. 2012;195:39–44. doi: 10.1016/j.psychres.2011.07.009. [DOI] [PubMed] [Google Scholar]
- 25.Spielberger CD, Gorsuch RL, Lushene R, Vagg PR, Jacobs GA. Manual for the State-Trait Anxiety Inventory. Palo Alto: Consulting Psychologists Press; 1983. [Google Scholar]
- 26.Lahiri DK, Nurnberger JI., Jr A rapid non-enzymatic method for the preparation of HMW DNA from blood for RFLP studies. Nucleic Acids Res. 1991;19:5444. doi: 10.1093/nar/19.19.5444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mamrut S, Harony H, Sood R, Shahar-Gold H, Gainer H, Shi YJ, Barki-Harrington L, Wagner S. DNA methylation of specific CpG sites in the promoter region regulates the transcription of the mouse oxytocin receptor. PLoS One. 2013;8:e56869. doi: 10.1371/journal.pone.0056869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Unternaehrer E, Luers P, Mill J, Dempster E, Meyer AH, Staehli S, Lieb R, Hellhammer DH, Meinlschmidt G. Dynamic changes in DNA methylation of stress-associated genes (OXTR, BDNF) after acute psychosocial stress. Transl Psychiatry. 2012;2:e150. doi: 10.1038/tp.2012.77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ziegler C, Dannlowski U, Brauer D, Stevens S, Laeger I, Wittmann H, Kugel H, Dobel C, Hurlemann R, Reif A, Lesch KP, Heindel W, Kirschbaum C, Arolt V, Gerlach AL, Hoyer J, Deckert J, Zwanzger P, Domschke K. Oxytocin receptor gene methylation: converging multilevel evidence for a role in social anxiety. Neuropsychopharmacology. 2015;40:1528–1538. doi: 10.1038/npp.2015.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kumsta R, Hummel E, Chen FS, Heinrichs M. Epigenetic regulation of the oxytocin receptor gene: implications for behavioral neuroscience. Front Neurosci. 2013;7:83. doi: 10.3389/fnins.2013.00083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Puglia MH, Lillard TS, Morris JP, Connelly JJ. Epigenetic modification of the oxytocin receptor gene influences the perception of anger and fear in the human brain. Proc Natl Acad Sci USA. 2015;112:3308–3313. doi: 10.1073/pnas.1422096112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jack A, Connelly JJ, Morris JP. DNA methylation of the oxytocin receptor gene predicts neural response to ambiguous social stimuli. Front Hum Neurosci. 2012;6:280. doi: 10.3389/fnhum.2012.00280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kusui C, Kimura T, Ogita K, Nakamura H, Matsumura Y, Koyama M, Azuma C, Murata Y. DNA methylation of the human oxytocin receptor gene promoter regulates tissue-specific gene suppression. Biochem Biophys Res Commun. 2001;289:681–686. doi: 10.1006/bbrc.2001.6024. [DOI] [PubMed] [Google Scholar]
- 34.Tost J, Dunker J, Gut IG. Analysis and quantification of multiple methylation variable positions in CpG islands by pyrosequencing. Biotechniques. 2003;35:152–156. doi: 10.2144/03351md02. [DOI] [PubMed] [Google Scholar]
- 35.Goodrich JM, Sanchez BN, Dolinoy DC, Zhang Z, Hernandez-Avila M, Hu H, Peterson KE, Tellez-Rojo MM. Quality control and statistical modeling for environmental epigenetics: a study on in utero lead exposure and DNA methylation at birth. Epigenetics. 2015;10:19–30. doi: 10.4161/15592294.2014.989077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Keefe R. Brief Assessment of Cognition in Schizophrenia (BACS) Durham: Duke University Medical Center; 1999. [Google Scholar]
- 37.Keefe RS, Goldberg TE, Harvey PD, Gold JM, Poe MP, Coughenour L. The Brief Assessment of Cognition in Schizophrenia: reliability, sensitivity, and comparison with a standard neurocognitive battery. Schizophr Res. 2004;68:283–297. doi: 10.1016/j.schres.2003.09.011. [DOI] [PubMed] [Google Scholar]
- 38.Grove T, Taylor S, Dalack G, Ellingrod V. Endothelial function, folate pharmacogenomics, and neurocognition in psychotic disorders. Schizophr Res. 2015;164:115–121. doi: 10.1016/j.schres.2015.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Vreeker A, Boks MP, Abramovic L, Verkooijen S, et al. High educational performance is a distinctive feature of bipolar disorder: a study on cognition in bipolar disorder, schizophrenia patients, relatives and controls. Psychol Med. 2016;46:807–818. doi: 10.1017/S0033291715002299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Vargas G, Strassnig M, Sabbag S, Gould F, Durand D, Stone L, Patterson TL, Harvey PD. The course of vocational functioning in patients with schizophrenia: re-examining social drift. Schizophr Res Cogn. 2014;1:e41–e46. doi: 10.1016/j.scog.2014.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Roth TL, Lubin FD, Sodhi M, Kleinman JE. Epigenetic mechanisms in schizophrenia. Biochim Biophys Acta. 2009;1790:869–877. doi: 10.1016/j.bbagen.2009.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Grayson DR, Guidotti A. The dynamics of DNA methylation in schizophrenia and related psychiatric disorders. Neuropsychopharmacology. 2013;38:138–166. doi: 10.1038/npp.2012.125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Boyadjieva N, Varadinova M. Epigenetics of psychoactive drugs. J Pharm Pharmacol. 2012;64:1349–1358. doi: 10.1111/j.2042-7158.2012.01475.x. [DOI] [PubMed] [Google Scholar]
- 44.Benjamini Y, Hochberg Y. On the adaptive control of the False Discovery Rate in multiple testing with independent statistics. J Educ Behav Stat. 2000;25:60–83. [Google Scholar]
- 45.Pike N. Using false discovery rates for multiple comparisons in ecology and evolution. Methods Ecol Evol. 2011;2:278–282. [Google Scholar]
- 46.Glickman ME, Rao SR, Schultz MR. False discovery rate control is a recommended alternative to Bonferroni-type adjustments in health studies. J Clin Epidemiol. 2014;67:850–857. doi: 10.1016/j.jclinepi.2014.03.012. [DOI] [PubMed] [Google Scholar]
- 47.Chagnon YC, Potvin O, Hudon C, Preville M. DNA methylation and single nucleotide variants in the brain-derived neurotrophic factor (BDNF) and oxytocin receptor (OXTR) genes are associated with anxiety/depression in older women. Front Genet. 2015;6:230. doi: 10.3389/fgene.2015.00230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Reiner I, Van IMH, Bakermans-Kranenburg MJ, Bleich S, Beutel M, Frieling H. Methylation of the oxytocin receptor gene in clinically depressed patients compared to controls: the role of OXTR rs53576 genotype. J Psychiatr Res. 2015;65:9–15. doi: 10.1016/j.jpsychires.2015.03.012. [DOI] [PubMed] [Google Scholar]
- 49.Kim YR, Kim JH, Kim MJ, Treasure J. Differential methylation of the oxytocin receptor gene in patients with anorexia nervosa: a pilot study. PLoS One. 2014;9:e88673. doi: 10.1371/journal.pone.0088673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Gregory SG, Connelly JJ, Towers AJ, Johnson J, Biscocho D, Markunas CA, Lintas C, Abramson RK, Wright HH, Ellis P, Langford CF, Worley G, Delong GR, Murphy SK, Cuccaro ML, Persico A, Pericak-Vance MA. Genomic and epigenetic evidence for oxytocin receptor deficiency in autism. BMC Med. 2009;7:62. doi: 10.1186/1741-7015-7-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Schizophrenia Working Group of the Psychiatric Genomics Consortium Biological insights from 108 schizophrenia-associated genetic loci. Nature. 2014;511:421–427. doi: 10.1038/nature13595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Haram M, Tesli M, Bettella F, Djurovic S, Andreassen OA, Melle I. Association between genetic variation in the oxytocin receptor gene and emotional withdrawal, but not between oxytocin pathway genes and diagnosis in psychotic disorders. Front Hum Neurosci. 2015;9:9. doi: 10.3389/fnhum.2015.00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Feifel D. Oxytocin as a potential therapeutic target for schizophrenia and other neuropsychiatric conditions. Neuropsychopharmacol Rev. 2012;37:304–305. doi: 10.1038/npp.2011.184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ridderinkhof KR, Nieuwenhuis S, Braver TS. Medial frontal cortex function: an introduction and overview. Cogn Affect Behav Neurosci. 2007;7:261–265. doi: 10.3758/cabn.7.4.261. [DOI] [PubMed] [Google Scholar]
- 55.Leuner B, Gould E. Structural plasticity and hippocampal function. Annu Rev Psychol. 2010;61:111–140. doi: 10.1146/annurev.psych.093008.100359. C111-C113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Rich ME, Caldwell HK. A role for oxytocin in the etiology and treatment of schizophrenia. Front Endocrinol (Lausanne) 2015;6:90. doi: 10.3389/fendo.2015.00090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Owen AM. The functional organization of working memory processes within human lateral frontal cortex: the contribution of functional neuroimaging. Eur J Neurosci. 1997;9:1329–1339. doi: 10.1111/j.1460-9568.1997.tb01487.x. [DOI] [PubMed] [Google Scholar]
- 58.Honey GD, Fu CHY, Kim J, Brammer MJ, Croudace TJ, Suckling J, Pich EM, Williams SCR, Bullmore ET. Effects of verbal working memory load on corticocortical connectivity modeled by path analysis of functional magnetic resonance imaging data. Neuroimage. 2002;17:573–582. [PubMed] [Google Scholar]
- 59.Kondo H, Osaka N, Osaka M. Cooperation of the anterior cingulate cortex and dorsolateral prefrontal cortex for attention shifting. Neuroimage. 2004;23:670–679. doi: 10.1016/j.neuroimage.2004.06.014. [DOI] [PubMed] [Google Scholar]
- 60.Osaka N, Osaka M, Kondo H, Morishita M, Fukuyama H, Shibasaki H. The neural basis of executive function in working memory: an fMRI study based on individual differences. Neuroimage. 2004;21:623–631. doi: 10.1016/j.neuroimage.2003.09.069. [DOI] [PubMed] [Google Scholar]
- 61.Alvarez JA, Emory E. Executive function and the frontal lobes: a meta-analytic review. Neuropsychol Rev. 2006;16:17–42. doi: 10.1007/s11065-006-9002-x. [DOI] [PubMed] [Google Scholar]
- 62.Depp CA, Bowie CR, Mausbach BT, Wolyniec P, Thornquist MH, Luke JR, McGrath JA, Pulver AE, Patterson TL, Harvey PD. Current smoking is associated with worse cognitive and adaptive functioning in serious mental illness. Acta Psychiatr Scand. 2015;131:333–341. doi: 10.1111/acps.12380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Smith RC, Singh A, Infante M, Khandat A, Kloos A. Effects of cigarette smoking and nicotine nasal spray on psychiatric symptoms and cognition in schizophrenia. Neuropsychopharmacology. 2002;27:479–497. doi: 10.1016/S0893-133X(02)00324-X. [DOI] [PubMed] [Google Scholar]
- 64.Mackowick KM, Barr MS, Wing VC, Rabin RA, Ouellet-Plamondon C, George TP. Neurocognitive endophenotypes in schizophrenia: modulation by nicotinic receptor systems. Prog Neuropsychopharmacol Biol Psychiatry. 2014;52:79–85. doi: 10.1016/j.pnpbp.2013.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Burghardt KJ, Goodrich JM, Dolinoy DC, Ellingrod VL. DNA methylation, insulin resistance and second-generation antipsychotics in bipolar disorder. Epigenomics. 2015;7:343–352. doi: 10.2217/epi.15.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Maccani JZ, Maccani MA. Altered placental DNA methylation patterns associated with maternal smoking: current perspectives. Adv Genomics Genet. 2015;2015:205–214. doi: 10.2147/AGG.S61518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Zhang Y, Schottker B, Florath I, Stock C, Butterbach K, Holleczek B, Mons U, Brenner H. Smoking-associated DNA methylation biomarkers and their predictive value for all-cause and cardiovascular mortality. Environ Health Perspect. 2016;124:67–74. doi: 10.1289/ehp.1409020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Kanamori C, Yasuda K, Sumi G, Kimura Y, Tsuzuki T, Cho H, Okada H, Kanzaki H. Effect of cigarette smoking on mRNA and protein levels of oxytocin receptor and on contractile sensitivity of uterine myometrium to oxytocin in pregnant women. Eur J Obstet Gynecol Reprod Biol. 2014;178:142–147. doi: 10.1016/j.ejogrb.2014.03.037. [DOI] [PubMed] [Google Scholar]
- 69.Novak V, Hajjar I. The relationship between blood pressure and cognitive function. Nat Rev Cardiol. 2010;7:686–698. doi: 10.1038/nrcardio.2010.161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Wadley VG, McClure LA, Howard VJ, Unverzagt FW, Go RC, Moy CS, Crowther MR, Gomez CR, Howard G. Cognitive status, stroke symptom reports, and modifiable risk factors among individuals with no diagnosis of stroke or transient ischemic attack in the REasons for Geographic and Racial Differences in Stroke (REGARDS) Study. Stroke. 2007;38:1143–1147. doi: 10.1161/01.STR.0000259676.75552.38. [DOI] [PubMed] [Google Scholar]
- 71.Crichton GE, Elias MF, Davey A, Alkerwi A. Cardiovascular health and cognitive function: the Maine-Syracuse Longitudinal Study. PLoS One. 2014;9:e89317. doi: 10.1371/journal.pone.0089317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Imamura A, Takahashi R, Murakami R, Kataoka H, Cheng XW, Numaguchi Y, Murohara T, Okumura K. The effects of endothelial nitric oxide synthase gene polymorphisms on endothelial function and metabolic risk factors in healthy subjects: the significance of plasma adiponectin levels. Eur J Endocrinol. 2008;158:189–195. doi: 10.1530/EJE-07-0632. [DOI] [PubMed] [Google Scholar]
- 73.Ellingrod VL, Taylor SF, Brook RD, Evans SJ, Zollner SK, Grove TB, Gardner KM, Bly MJ, Pop-Busui R, Dalack G. Dietary, lifestyle and pharmacogenetic factors associated with arteriole endothelial-dependent vasodilatation in schizophrenia patients treated with atypical antipsychotics (AAPs) Schizophr Res. 2011;130:20–26. doi: 10.1016/j.schres.2011.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Burghardt K, Grove T, Ellingrod V. Endothelial nitric oxide synthetase genetic variants, metabolic syndrome and endothelial function in schizophrenia. J Psychopharmacol. 2014;28:349–356. doi: 10.1177/0269881113516200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Dadds MR, Moul C, Cauchi A, Dobson-Stone C, Hawes DJ, Brennan J, Ebstein RE. Methylation of the oxytocin receptor gene and oxytocin blood levels in the development of psychopathy. Dev Psychopathol. 2014;26:33–40. doi: 10.1017/S0954579413000497. [DOI] [PubMed] [Google Scholar]
- 76.Horvath S, Zhang Y, Langfelder P, Kahn RS, Boks MP, van Eijk K, van den Berg LH, Ophoff RA. Aging effects on DNA methylation modules in human brain and blood tissue. Genome Biol. 2012;13:R97. doi: 10.1186/gb-2012-13-10-r97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Thompson TM, Sharfi D, Lee M, Yrigollen CM, Naumova OY, Grigorenko EL. Comparison of whole-genome DNA methylation patterns in whole blood, saliva, and lymphoblastoid cell lines. Behav Genet. 2013;43:168–176. doi: 10.1007/s10519-012-9579-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Beery AK, McEwen LM, MacIsaac JL, Francis DD, Kobor MS. Natural variation in maternal care and cross-tissue patterns of oxytocin receptor gene methylation in rats. Horm Behav. 2016;77:42–52. doi: 10.1016/j.yhbeh.2015.05.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Ebstein RP, Knafo A, Mankuta D, Chew SH, Lai PS. The contributions of oxytocin and vasopressin pathway genes to human behavior. Horm Behav. 2012;61:359–379. doi: 10.1016/j.yhbeh.2011.12.014. [DOI] [PubMed] [Google Scholar]
- 80.Rajagopal L, Massey BW, Huang M, Oyamada Y, Meltzer HY. The novel object recognition test in rodents in relation to cognitive impairment in schizophrenia. Curr Pharm Des. 2014;20:5104–5114. doi: 10.2174/1381612819666131216114240. [DOI] [PubMed] [Google Scholar]
- 81.Davies MN, Volta M, Pidsley R, Lunnon K, Dixit A, Lovestone S, Coarfa C, Harris RA, Milosavljevic A, Troakes C, Al-Sarraj S, Dobson R, Schalkwyk LC, Mill J. Functional annotation of the human brain methylome identifies tissue-specific epigenetic variation across brain and blood. Genome Biol. 2012;13:R43. doi: 10.1186/gb-2012-13-6-r43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Provencal N, Suderman MJ, Guillemin C, Massart R, Ruggiero A, Wang D, Bennett AJ, Pierre PJ, Friedman DP, Cote SM, Hallett M, Tremblay RE, Suomi SJ, Szyf M. The signature of maternal rearing in the methylome in rhesus macaque prefrontal cortex and T cells. J Neurosci. 2012;32:15626–15642. doi: 10.1523/JNEUROSCI.1470-12.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Ursini G, Bollati V, Fazio L, Porcelli A, Iacovelli L, Catalani A, Sinibaldi L, Gelao B, Romano R, Rampino A, Taurisano P, Mancini M, Di Giorgio A, Popolizio T, Baccarelli A, De Blasi A, Blasi G, Bertolino A. Stress-related methylation of the catechol-O-methyltransferase Val158 allele predicts human prefrontal cognition and activity. J Neurosci. 2011;31:6692–6698. doi: 10.1523/JNEUROSCI.6631-10.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Domschke K, Tidow N, Kuithan H, Schwarte K, Klauke B, Ambree O, Reif A, Schmidt H, Arolt V, Kersting A, Zwanzger P, Deckert J. Monoamine oxidase A gene DNA hypomethylation - a risk factor for panic disorder? Int J Neuropsychopharmacol. 2012;15:1217–1228. doi: 10.1017/S146114571200020X. [DOI] [PubMed] [Google Scholar]