Suzuki et al. show that neural inputs to β2-adrenergic receptors expressed on lymphocytes generate the diurnal variation in the frequency of lymphocyte egress from lymph nodes, which is reflected in the magnitude of the adaptive immune response.
Abstract
Various aspects of the immune system display circadian rhythms. Although lymphocyte trafficking has been suggested to show diurnal variations, the mechanisms and influences on immune responses are unclear. Here, we show in mice that inputs from adrenergic nerves contribute to the diurnal variation of lymphocyte recirculation through lymph nodes (LNs), which is reflected in the magnitude of the adaptive immune response. Neural inputs to β2-adrenergic receptors (β2ARs) expressed on lymphocytes reduced the frequency of lymphocyte egress from LNs at night, which was accompanied by an increase of lymphocyte numbers in LNs. Immunization during the period of lymphocyte accumulation in LNs enhanced antibody responses. The diurnal variation of the humoral immune response was dependent on β2AR-mediated neural signals and was diminished when lymphocyte recirculation through LNs was stopped. This study reveals the physiological role of adrenergic control of lymphocyte trafficking in adaptive immunity and establishes a novel mechanism that generates diurnal rhythmicity in the immune system.
Introduction
Cell trafficking among different anatomical sites is essential for proper functioning of the immune system. Recent studies have demonstrated that the frequency of neutrophil and monocyte migration from blood to tissues shows circadian oscillations that cause variations in the magnitude of inflammatory responses in tissues (Scheiermann et al., 2012; Nguyen et al., 2013). In addition to these innate immune cells, adaptive immune cells, represented by lymphocytes, have been suggested to possess diurnal fluctuations in their trafficking (Suzuki et al., 1997; Haus and Smolensky, 1999). However, the mechanisms and influences on immune responses remain unclear. After surveying a LN for several hours, lymphocytes exit from the LN into lymph, return to blood flow, and travel to other lymphoid organs to continue antigen surveillance in the entire body (Cyster and Schwab, 2012). We recently reported that inputs from adrenergic nerves control lymphocyte egress from, but not entry to, LNs through β2ARs. Activation of lymphocyte β2ARs enhances the responsiveness of CCR7 and CXCR4, chemokine receptors that promote LN retention of lymphocytes, and consequently inhibits their LN egress (Nakai et al., 2014). Because adrenergic nerves release noradrenaline in a circadian manner and directly innervate lymphoid organs (Felten et al., 1985; Elenkov et al., 2000), we hypothesized that the β2AR-mediated control of lymphocyte recirculation through LNs might contribute to the diurnal variation of lymphocyte dynamics.
Results and discussion
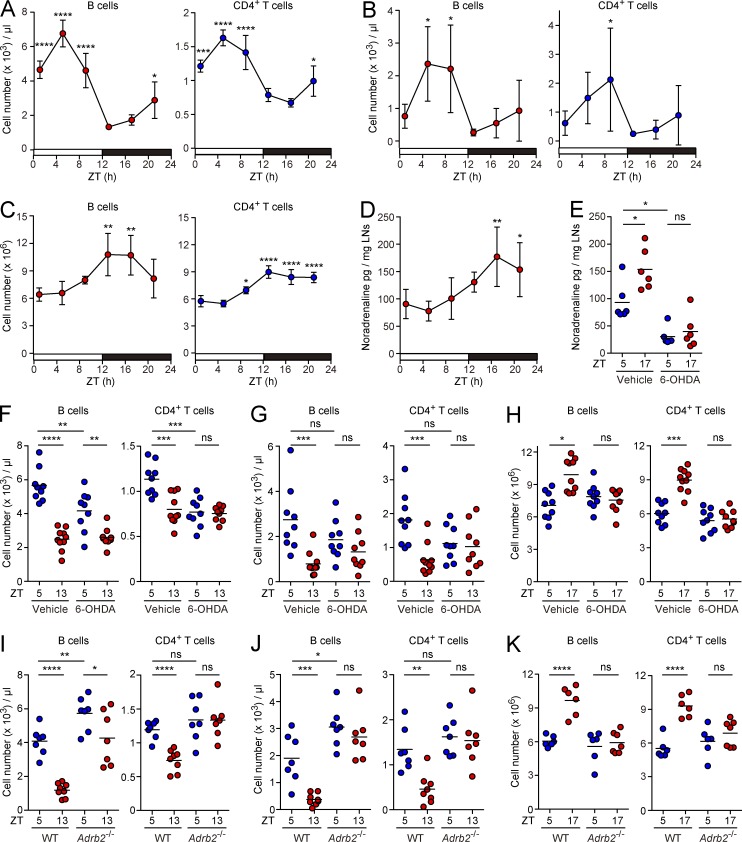
As an initial attempt to test this hypothesis, we assessed daily fluctuations of lymphocyte numbers in blood, lymph, and LNs of WT mice (Fig. S1). Consistent with a previous finding (Scheiermann et al., 2012), the numbers of B cells, CD4+, and CD8+ T cells in blood peaked at 5 h after the onset of light (zeitgeber time 5, ZT5) and decreased toward ZT13, an hour after lights out (Fig. 1 A and not depicted). Notably, we found that lymphocyte numbers in lymph displayed a similar pattern of oscillations (Fig. 1 B). In contrast, lymphocyte numbers in peripheral LNs fluctuated in antiphase to those in blood and lymph, showing a peak from ZT13 to ZT17 and a trough in the daytime (Fig. 1 C). The amount of noradrenaline in peripheral LNs was increased toward night time and peaked at ZT17 (Fig. 1 D). Thus, accumulation of lymphocytes in peripheral LNs and their reciprocal reduction in blood and lymph were accompanied by the rise of adrenergic tone. Because lymphocyte numbers in mesenteric LNs exhibited a peak at night, as did those in peripheral LNs (unpublished data), lymphocyte numbers in other LNs might also show a similar pattern of diurnal variations. Blood and lymph compartments are too small as reservoirs of lymphocytes to account for the night time increase of lymphocytes in different LNs. Considering the size as a lymphocyte reservoir and antiphase oscillations of lymphocyte numbers to those in LNs (Kawate et al., 1981), the spleen might compensate for the synchronized fluctuation of lymphocyte numbers in LNs.
Figure 1.
Diurnal oscillation of lymphocyte numbers in circulation and LNs. (A–D) Numbers of B cells and CD4+ T cells in blood (A), lymph (B), and peripheral LNs (the sum of inguinal, axillary, and brachial LNs; C), and the noradrenaline content in peripheral LNs (D) of WT mice at the indicated ZTs. Data in A–D are representative of two experiments and shown as the mean ± SD of four mice. (E–H) Noradrenaline levels in peripheral LNs (E) and numbers of B cells and CD4+ T cells in blood (F), lymph (G), and peripheral LNs (H) of vehicle- and 6-OHDA–treated mice at the indicated ZTs. (I–K) Numbers of B cells and CD4+ T cells in blood (I), lymph (J), and peripheral LNs (K) of WT (Adrb2+/+ or Adrb2+/− littermates) and Adrb2−/− mice at the indicated ZTs. Data are pooled from two (E and K) or three (F–J) experiments. Each symbol represents an individual mouse (at least six mice per group) and bars indicate means. *, P < 0.05; **, P < 0.01; ***, P < 0.001; ****, P < 0.0001; ns, not significant. P-values were obtained by one-way ANOVA with Dunnett’s post-hoc test in comparison with the trough (A–D) or two-way ANOVA with Tukey’s post-hoc test (E–K).
To investigate the contribution of adrenergic nerves to the diurnal changes of lymphocyte distribution, we treated mice with 6-hydroxydopamine (6-OHDA) to deplete peripheral adrenergic nerves, and then compared lymphocyte numbers in blood, lymph, and LNs between the daytime and nighttime. The 6-OHDA treatment reduced the level of noradrenaline in peripheral LNs and blunted its diurnal variation (Fig. 1 E). In 6-OHDA–treated mice, the night time reduction of lymphocyte numbers in blood and lymph was not remarkable compared with that in vehicle-treated controls (Fig. 1, F and G). Depletion of adrenergic nerves also abrogated the nocturnal increase of lymphocyte numbers in LNs (Fig. 1 H). The differences of lymphocyte numbers between the two time points were diminished in β2AR-deficient mice (Fig. 1, I, J, and K). These observations suggest that inputs from adrenergic nerves contribute to the diurnal variation of lymphocyte dynamics through β2ARs. Although the daytime lymphocyte numbers in blood and lymph tended to increase in β2AR-deficient mice (Fig. 1, I and J), they were not elevated in 6-OHDA–treated mice (Fig. 1, F and G). This might be caused by another endogenous β2AR agonist, adrenaline, which is produced in adrenal glands and released into the blood stream. The effects of adrenaline could become obvious in 6-OHDA–treated mice because its production is insensitive to 6-OHDA treatment (Clark et al., 1972) and it acts on β2ARs with higher potency than noradrenaline (Liapakis et al., 2004). The reduction of blood B cells at night in 6-OHDA–treated mice (Fig. 1 F) might be caused by the humoral adrenergic inputs from adrenal glands and β3AR-mediated signals that promote B cell recruitment to the BM (Scheiermann et al., 2012). The β3AR-mediated BM recruitment might also account for the incomplete disappearance of diurnal variation of blood B cell numbers in β2AR-deficient mice (Fig. 1 I).
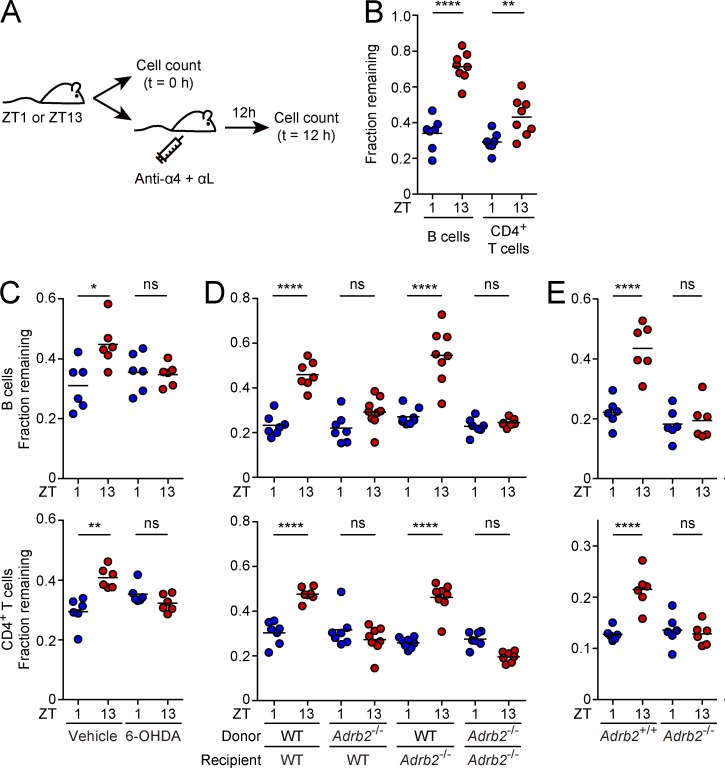
The increase of lymphocyte numbers in LNs and their concomitant decrease in circulation, especially lymph, strongly suggest inhibition of lymphocyte egress from LNs at night. To test this possibility, we blocked lymphocyte entry to LNs at ZT1 or ZT13 by treatment with neutralizing antibodies against α4 and αL integrins for 12 h (Lo et al., 2005; Fig. 2 A). The numbers of B cells, CD4+, and CD8+ T cells remaining in peripheral LNs were higher when the entry blockade was performed at ZT13 (Fig. 2 B and not depicted), indicating restriction of lymphocyte egress at night. The diurnal variation of LN egress was diminished by depletion of adrenergic nerves (Fig. 2 C) and in WT mice that were reconstituted with β2AR-deficient BM cells, but not in β2AR-deficient mice that were reconstituted with WT BM cells (Fig. 2 D). Moreover, β2AR-deficient lymphocytes transferred into WT mice did not exhibit diurnal variations of LN egress (Fig. 2 E and Fig. S2). These observations suggest that the diurnal variation of lymphocyte egress from LNs largely depends on adrenergic inputs to β2ARs expressed on lymphocytes. Although direct demonstration of diurnal alterations in CCR7 and CXCR4 signaling has not been achieved, we speculate that the retention-promoting signals mediated by these chemokine receptors might oscillate during a day in response to the inputs to lymphocyte β2ARs and generate a rhythm of LN egress.
Figure 2.
Diurnal variation of lymphocyte egress from LNs. (A) Experimental design. Mice were treated with neutralizing antibodies against α4 and αL integrins at ZT1 or ZT13. Fractions of lymphocytes remaining in peripheral LNs at 12 h after the integrin blockade were determined as ratios relative to those at 0 h. (B–D) Fractions of B cells and CD4+ T cells remaining in peripheral LNs of WT mice (B), vehicle- and 6-OHDA–treated mice (C), and BM chimeras generated with WT (Adrb2+/+ or Adrb2+/−) or Adrb2−/− mice as donors and/or recipients (D). (E) B cells or CD4+ T cells from Adrb2+/+ or Adrb2−/− mice were labeled with CFSE and transferred into WT mice. Fractions of transferred cells remaining in peripheral LNs were determined at 12 h after the integrin blockade. Data are pooled from two (B and C) or eight (D) experiments, or two experiments for each cell type (E). Each symbol represents an individual mouse (at least six mice per group) and bars indicate means. *, P < 0.05; **, P < 0.01; ****, P < 0.0001; ns, not significant. P-values were obtained by unpaired Student’s t test (B) or two-way ANOVA with Tukey’s post-hoc test (C, D, and E).
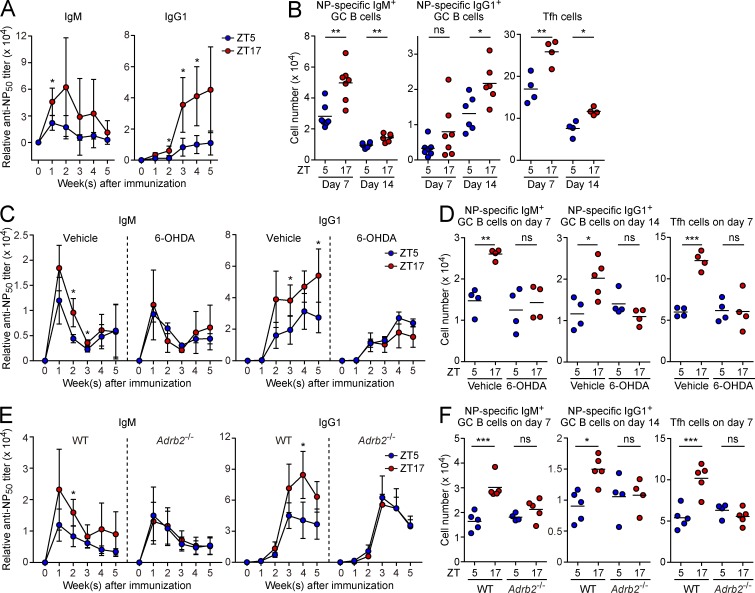
Our findings demonstrated sequestration of lymphocytes in LNs from circulation during the period of activity and high adrenergic tone. Lymphocytes specific for a given antigen are very rare (estimated to be <10 cells per LN), and the population size dictates the magnitude of responses (Moon et al., 2007). Therefore, we hypothesized that the sequestration of lymphocytes in LNs during the active phase may increase the chance of antigen encounter and potentiate adaptive immune responses. As an approach to favor the likelihood that an antigen is directly delivered to the draining LN with a minimal time lag after injection and supplied to the LN for a limited period of time (Pape et al., 2007), we immunized mice in the ear by intradermal injection of a soluble antigen, (4-hydroxy-3-nitrophenyl) acetyl (NP) hapten conjugated with chicken γ-globulin (NP-CGG), in the form of a nonviscous emulsion containing monophosphoryl lipid A as an adjuvant. Immunization was performed at ZT5 or ZT17 when lymphocyte numbers in LNs exhibited a trough and peak in a day, respectively. We found that the elevation of NP-specific antibody titers of IgM and IgG1 classes was more evident when mice were immunized at ZT17 (Fig. 3 A). Consistently, in the ear-draining LN, the generation of germinal center (GC) B cells, which recognized the hapten, and follicular helper T (Tfh) cells was enhanced by immunizing mice at night (Fig. 3 B and Fig. S3). These results indicate that induction of the humoral immune response in LNs is promoted during the period of high adrenergic activity.
Figure 3.
Diurnal variation of the humoral immune response. (A and B) WT mice were immunized in the ear with NP-CGG at ZT5 or ZT17. Serum titers of NP-specific IgM and IgG1 at the indicated times after immunization were measured by ELISA (A). The numbers of IgM+ and IgG1+ NP-specific GC B cells, and total Tfh cells generated in the ear-draining cervical LN were measured by flow cytometry at 7 and 14 d after immunization (B). (C–F) Serum antibody titers (C and E) and the generation of GC B cells and Tfh cells (D and F) were measured at the indicted time after immunization in mice treated with the vehicle or 6-OHDA (C and D), and in WT (Adrb2+/+ or Adrb2+/− littermates) and Adrb2−/− mice (E and F). Data are representative of three (A) or two (C and E) experiments, or pooled from two experiments (B, D, and F). Antibody titers are shown as the mean ± SD of at least four mice (A, C, and E). Cell numbers are shown as the mean of at least four mice with symbols representing individual mice (B, D, and F). *, P < 0.05; **, P < 0.01; ***, P < 0.001; ns, not significant. P-values were obtained by unpaired Student’s t test (A–C and E) or two-way ANOVA with Tukey’s post-hoc test (D and F).
Depletion of adrenergic nerves reduced the diurnal variations in antibody responses and the generation of GC B cells and Tfh cells (Fig. 3, C and D). Additionally, the fluctuations of the humoral immune response were abrogated in β2AR-deficient mice (Fig. 3, E and F). These observations suggest that inputs from adrenergic nerves contribute to the nocturnal enhancement of adaptive immunity through β2ARs. There were no significant diurnal variations in the surface expression of B cell receptors, CD40, CD86, and MHC class II on naive B cells, and TCRs and CD28 on naive CD4+ T cells (unpublished data). However, we cannot exclude the possibility that antigen priming of B cells and CD4+ T cells, and their respective differentiation to GC B cells and Tfh cells are under the control of lymphocyte-intrinsic circadian clocks as demonstrated in the differentiation of IL-17–producing helper T cells (Yu et al., 2013). Although previous studies showed that signals though β2ARs had some impacts on B cell responses in vitro and in vivo (Sanders, 2012), the baseline level of the humoral immune response was not affected by the deficiency of β2AR-mediated signals in our experimental system.
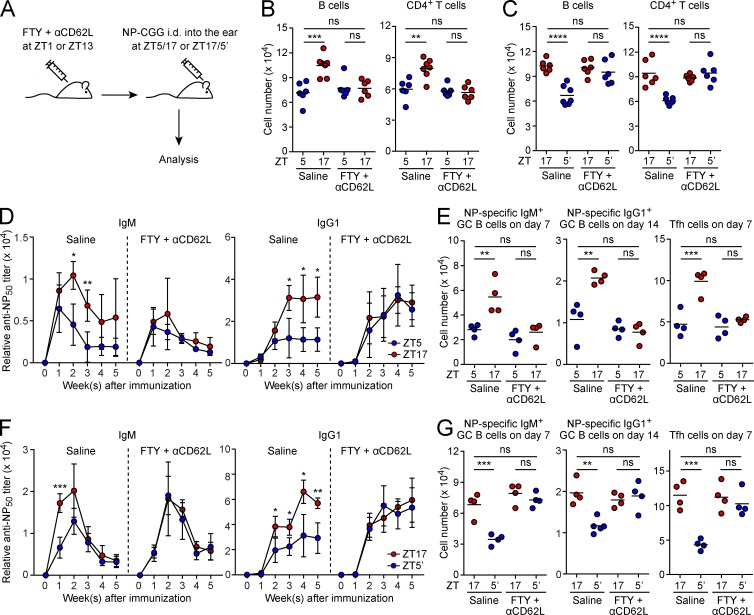
To directly assess whether lymphocyte recirculation through LNs contributes to the diurnal variation of the humoral immune response, we set up an experimental system to block both LN egress and entry of lymphocytes (Fig. 4 A). Because lymphocyte egress from LNs is strongly dependent on sphingosine-1-phosphate receptor-1, its functional antagonist, FTY720, was used to block LN egress (Rosen and Goetzl, 2005; Schwab and Cyster, 2007). To block LN entry, a neutralizing antibody against CD62L, an adhesion molecule that mediates LN entry together with α4 and αL integrins (von Andrian and Mempel, 2003), was used; unlike these integrins, CD62L is not involved in cognate interactions between B cells and T cells, and its blockade might not affect the magnitude of the humoral immune response (Xu et al., 1996). Combined treatment with FTY720 and the anti-CD62L antibody at ZT1 or ZT13 fixed lymphocyte numbers of LNs in the low and high state, respectively (Fig. 4, B and C), suggesting that lymphocyte recirculation through LNs was stopped by this treatment. We found that the fluctuations of the humoral immune response between ZT5 and ZT17 were diminished by treatment with FTY720 and the anti-CD62L antibody, and the magnitude of the response largely reflected lymphocyte numbers in LNs at the time of immunization (Fig. 4, D–G). These results suggest that lymphocyte recirculation through LNs contributes to the diurnal variation of the adaptive immune response induced in LNs. However, because FTY720 and the anti-CD62L antibody could act on many cell types, we cannot exclude a possibility that these reagents might affect other biological events besides lymphocyte trafficking through LNs. The serum titer of NP-specific IgG1 was clamped at high levels, even when lymphocyte numbers in LNs were fixed in the low state at the time of immunization (Fig. 4 D), which might be a result of the nontrafficking effects of the reagents.
Figure 4.
Contribution of lymphocyte recirculation through LNs to the diurnal variation of humoral immunity. (A) Experimental design. WT mice were treated with FTY720 (FTY) and a neutralizing antibody against CD62L (αCD62L) at ZT1, and then immunized with NP-CGG in the ear at ZT5 or ZT17. Or mice were treated with FTY and αCD62L at ZT13, and then immunized at ZT17 or ZT5 on the next day (ZT5′). (B and C) Numbers of B cells and CD4+ T cells in peripheral LNs of unimmunized mice were measured at the indicated ZTs after treatment with saline or FTY plus αCD62L at ZT1 (B) or ZT13 (C). (D–G) Serum titers of NP-specific antibodies (D and F) and the generation of NP-specific GC B cells and total Tfh cells in the ear-draining cervical LN (E and G) were analyzed in mice immunized at the indicated ZTs after treatment with FTY and αCD62L at ZT1 (D and E) or ZT13 (F and G). Data are representative of two experiments (D and F) or pooled from two experiments (B, C, E, and G). Antibody titers are shown as the mean ± SD of four mice (D and F). Cell numbers are shown as the mean of at least four mice with symbols representing individual mice (B, C, E, and G). *, P < 0.05; **, P < 0.01; ***, P < 0.001; ****, P < 0.0001; ns, not significant. P-values were obtained by two-way ANOVA with Tukey’s post-hoc test (B, C, E, and G) or unpaired Student’s t test (D and F).
The aforementioned findings demonstrate that neural inputs mediated by β2ARs generate the diurnal variation of lymphocyte egress from LNs, which is translated into significant changes in the adaptive immune response. In this regard, this study reveals the physiological relevance of the mechanism by which adrenergic nerves control lymphocyte recirculation through LNs. In humans, blood lymphocyte numbers exhibit an opposing diurnal fluctuation to those in mice (Suzuki et al., 1997; Haus and Smolensky, 1999). However, considering the fact that adrenergic nerve activity in humans and mice oscillates in antiphase during a day (Suzuki et al., 1997), the same mechanism might operate to generate diurnal variations of lymphocyte trafficking in both humans and mice.
Our study is in line with a recent study implying that the adaptive immune system is influenced by external diurnal signals (Hemmers and Rudensky, 2015). However, it is still possible that cell-intrinsic circadian clocks are also involved in the control of lymphocyte recirculation through LNs as shown in monocyte trafficking (Nguyen et al., 2013). Because local autonomic innervation is an important factor for entrainment of peripheral clocks (Dibner et al., 2010), adrenergic nerves may contribute to diurnal lymphocyte trafficking directly through β2AR-mediated enhancement of chemokine receptor signals (Nakai et al., 2014) and by synchronizing the molecular clocks in lymphocytes and their microenvironments.
Previous studies have suggested that the innate immune system is prepared to sense pathogens more efficiently during periods of activity (Scheiermann et al., 2012; Silver et al., 2012; Curtis et al., 2015). Our study demonstrates that the adaptive immune system is also poised to mount higher responses in LNs during the active phase. The synchronization of both arms of the immune system may have evolved to maximize the efficiency of host defense when encounters with pathogens are more likely to occur. The time-dependent differences in immune responses can be exploited in clinical settings, such that vaccination during the immunologically active phase might ensure potent protection against infectious diseases.
Materials and methods
Mice
C57BL/6 mice were purchased from Clea. Adrb2−/− mice on a C57BL/6 background were generated as described previously (Hanyu et al., 2012). 8–12-wk-old mice were used for experiments. BM chimeras were generated by irradiating recipient mice with a single dose of 8 Gy, followed by i.v. transfer of 5–10 × 106 BM cells per mouse. Chimeras were analyzed at least 8 wk after BM reconstitution. Mice were housed in a 12-h light/12-h dark cycle (light period from 8 a.m. to 8 p.m.) with ad libitum feeding in a specific pathogen–free facility maintained at 22°C. All experiments were performed in accordance with protocols approved by the Osaka University Animal Care Committee.
Collection of blood, lymph, and LNs
After mice were euthanized by CO2 asphyxiation, lymph was drawn from the cysterna chyli using a fine microcapillary pipette (Matloubian et al., 2004). Blood was collected from the inferior vena cava using a syringe with a 26-G needle, and red blood cells were lysed with ammonium chloride potassium buffer. Peripheral LNs (inguinal, axillary, and brachial LNs; total 6 LNs) were collected, and disrupted by passing through a 40-µm cell strainer (BD). Cell numbers in blood and LNs were measured with a Z2 Coulter counter (Beckman Coulter). To determine the cell concentration in lymph, cell numbers were counted by flow cytometry and divided by the volume of the collected lymph.
Flow cytometry
Single cells were stained with fluorophore-labeled antibodies recognizing the following molecules (BioLegend): B220 (RA3-6B2), CD4 (RM4-5), CD8α (53–6.7), CD19 (6D5), IgD (11-26c.2a), IgG1 (RMG1-1), IgM (RMM-1), Ly-6G (1A8), PD-1 (29F.1A12), and TCRβ (H57-597). Antibodies against CD95 (Jo2) and CXCR5 (2G8) were purchased from BD. Data were acquired on a FACSVerse cytometer (BD) and analyzed with FlowJo software (Tree Star) to detect the following populations: B cells in blood and lymph (CD19+) or LNs (CD19+IgDhiCD95−) of unimmunized mice; CD4+ or CD8+ T cells (CD4+ or CD8+) in blood, lymph, and LNs of unimmunized mice; and GC B cells (B220+IgDloCD95+IgM+ or IgG1+) and Tfh cells (CD4+TCRβ+CXCR5+PD-1+) in LNs of immunized mice. NP-specific GC B cells were labeled with NP23-PE (Biosearch Technologies) at 7 and 14 d after immunization.
Assessment of lymphocyte egress from LNs
Lymphocyte entry to LNs was blocked by i.v. injection of neutralizing antibodies against α4 (PS/2) and αL (M17/4) integrins (both purchased from Bio X Cell) at 100 µg each per mouse. After 12 h, lymphocytes remaining in peripheral LNs were enumerated (Lo et al., 2005). For transfer experiments, B cells or CD4+ T cells were isolated with 90–95% purity from spleens of Adrb2+/+ or Adrb2−/− mice by negative selection with AutoMACS (Miltenyi Biotec) using anti-CD43 magnetic beads or a CD4+ T cell isolation kit (both purchased from Miltenyi Biotec), respectively. The cells were labeled with 0.5 µM CFSE in DMEM containing 1% FBS for 10 min at 37°C, and 2 × 107 cells were transferred i.v. into each recipient mouse. Entry blockade was performed at 20–24 h after the cell transfer.
Depletion of adrenergic nerves
Mice were injected i.p. with 100 mg/kg 6-OHDA (Sigma-Aldrich) dissolved in saline containing 0.01% antioxidant ascorbate on days −7 and −5, and 200 mg/kg 6-OHDA in the ascorbate-containing salineon day −3 (Grebe et al., 2010).
Immunization
Mice received i.d. injection of 20 µg NP31-CGG (Biosearch Technologies) in Sigma Adjuvant System (Sigma-Aldrich) into the ear pinna under isoflurane anesthesia. Sera were collected every week after immunization to measure anti-NP antibody titers by ELISA. The ear-draining cervical LN was collected at 7 or 14 d after immunization and subjected to flow cytometry of GC B cells and Tfh cells. To block both LN entry and egress of lymphocytes, a neutralizing antibody against CD62L (Mel-14; Bio X Cell) at 200 µg per mouse and FTY720 (Sigma-Aldrich) at 1 mg/kg were administered i.v. and i.p., respectively.
ELISA
To measure anti-NP antibody titers, Maxisorp immunoplates (Thermo Fisher Scientific) were coated with NP50-BSA (Biosearch Technologies), followed by blocking with 0.5% BSA in PBS containing 0.05% Tween-20 (PBST). Serially diluted sera were added to the wells, followed by incubation for 5–6 h at room temperature. After washing with PBST, HRP-conjugated goat anti–mouse IgM or IgG1 (Southern Biotech) was added to the wells, followed by overnight incubation at 4°C. The HRP activity was detected with tetramethylbenzidine substrate (KPL), and absorbance at 450 nm was measured using an iMark microplate reader (Bio-Rad Laboratories) after quenching the reaction with 1 N HCl. To measure the amount of noradrenaline, LNs were homogenized in 0.01 N HCl in the presence of 1 mM EDTA and 4 mM sodium metabisulfite. The pH of the collected supernatants was adjusted to ∼7 by adding 1 N NaOH. The concentration of noradrenaline in the supernatants was measured with a kit (Labor Diagnostika Nord). The amount of noradrenaline was normalized to the weight of the LNs.
Statistical analysis
GraphPad Prism 6 (GraphPad Software) was used for all statistical analyses. The means of two groups were compared with unpaired Student’s t test. For multigroup comparisons, we performed one-way or two-way ANOVA with post-hoc testing using Dunnett’s or Tukey’s multiple comparison test, respectively.
Online supplemental material
Fig. S1 shows flow cytometric gating strategies for lymphocyte populations in unimmunized mice. Fig. S2 shows flow cytometric gating strategies for transferred cells. Fig. S3 shows flow cytometric gating strategies for lymphocyte populations in immunized mice.
Supplementary Material
Acknowledgments
We thank H. Kikutani, T. Kurosaki, A. Kumanogoh, and Y. Baba for discussion, E. Hara for supporting mouse experiments, and T. Inoue for reagents.
K. Suzuki is supported by grants from the Japan Society for the Promotion of Science (JP15H05656 and JP15K15153), the Ministry of Education, Culture, Sports, Science and Technology, Japan (JP15H01157), the Japan Medical Association (the Medical Research Encouragement Prize), the Uehara Memorial Foundation, the Naito Foundation, the Takeda Science Foundation, the Astellas Foundation for Research on Metabolic Disorders, the Mochida Memorial Foundation for Medical and Pharmaceutical Research, and the SENSHIN Medical Research Foundation.
The authors declare no competing financial interests.
Author contributions: K. Suzuki conceived and designed the study, performed experiments, analyzed the data, and wrote the manuscript. Y. Hayano, A. Nakai, and F. Furuta performed experiments and analyzed the data. M. Noda provided Adrb2−/− mice on a C57BL/6 background.
Footnotes
Abbreviations used:
- 6-OHDA
- 6-hydroxydopamine
- β2AR
- β2-adrenergic receptor
- GC
- germinal center
- NP
- (4-hydroxy-3-nitrophenyl) acetyl
- Tfh
- follicular helper T
References
- Clark D.W.J., Laverty R., and Phelan E.L.. 1972. Long-lasting peripheral and central effects of 6-hydroxydopamine in rats. Br. J. Pharmacol. 44:233–243. 10.1111/j.1476-5381.1972.tb07259.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curtis A.M., Fagundes C.T., Yang G., Palsson-McDermott E.M., Wochal P., McGettrick A.F., Foley N.H., Early J.O., Chen L., Zhang H., et al. 2015. Circadian control of innate immunity in macrophages by miR-155 targeting Bmal1. Proc. Natl. Acad. Sci. USA. 112:7231–7236. 10.1073/pnas.1501327112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cyster J.G., and Schwab S.R.. 2012. Sphingosine-1-phosphate and lymphocyte egress from lymphoid organs. Annu. Rev. Immunol. 30:69–94. 10.1146/annurev-immunol-020711-075011 [DOI] [PubMed] [Google Scholar]
- Dibner C., Schibler U., and Albrecht U.. 2010. The mammalian circadian timing system: organization and coordination of central and peripheral clocks. Annu. Rev. Physiol. 72:517–549. 10.1146/annurev-physiol-021909-135821 [DOI] [PubMed] [Google Scholar]
- Elenkov I.J., Wilder R.L., Chrousos G.P., and Vizi E.S.. 2000. The sympathetic nerve--an integrative interface between two supersystems: the brain and the immune system. Pharmacol. Rev. 52:595–638. [PubMed] [Google Scholar]
- Felten D.L., Felten S.Y., Carlson S.L., Olschowka J.A., and Livnat S.. 1985. Noradrenergic and peptidergic innervation of lymphoid tissue. J. Immunol. 135(2, Suppl):755s–765s. [PubMed] [Google Scholar]
- Grebe K.M., Takeda K., Hickman H.D., Bailey A.L., Embry A.C., Bennink J.R., and Yewdell J.W.. 2010. Cutting edge: Sympathetic nervous system increases proinflammatory cytokines and exacerbates influenza A virus pathogenesis. J. Immunol. 184:540–544. 10.4049/jimmunol.0903395 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanyu R., Wehbi V.L., Hayata T., Moriya S., Feinstein T.N., Ezura Y., Nagao M., Saita Y., Hemmi H., Notomi T., et al. 2012. Anabolic action of parathyroid hormone regulated by the β2-adrenergic receptor. Proc. Natl. Acad. Sci. USA. 109:7433–7438. 10.1073/pnas.1109036109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haus E., and Smolensky M.H.. 1999. Biologic rhythms in the immune system. Chronobiol. Int. 16:581–622. 10.3109/07420529908998730 [DOI] [PubMed] [Google Scholar]
- Hemmers S., and Rudensky A.Y.. 2015. The cell-intrinsic circadian clock is dispensable for lymphocyte differentiation and function. Cell Reports. 11:1339–1349. 10.1016/j.celrep.2015.04.058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawate T., Abo T., Hinuma S., and Kumagai K.. 1981. Studies of the bioperiodicity of the immune response. II. Co-variations of murine T and B cells and a role of corticosteroid. J. Immunol. 126:1364–1367. [PubMed] [Google Scholar]
- Liapakis G., Chan W.C., Papadokostaki M., and Javitch J.A.. 2004. Synergistic contributions of the functional groups of epinephrine to its affinity and efficacy at the β2 adrenergic receptor. Mol. Pharmacol. 65:1181–1190. 10.1124/mol.65.5.1181 [DOI] [PubMed] [Google Scholar]
- Lo C.G., Xu Y., Proia R.L., and Cyster J.G.. 2005. Cyclical modulation of sphingosine-1-phosphate receptor 1 surface expression during lymphocyte recirculation and relationship to lymphoid organ transit. J. Exp. Med. 201:291–301. 10.1084/jem.20041509 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matloubian M., Lo C.G., Cinamon G., Lesneski M.J., Xu Y., Brinkmann V., Allende M.L., Proia R.L., and Cyster J.G.. 2004. Lymphocyte egress from thymus and peripheral lymphoid organs is dependent on S1P receptor 1. Nature. 427:355–360. 10.1038/nature02284 [DOI] [PubMed] [Google Scholar]
- Moon J.J., Chu H.H., Pepper M., McSorley S.J., Jameson S.C., Kedl R.M., and Jenkins M.K.. 2007. Naive CD4+ T cell frequency varies for different epitopes and predicts repertoire diversity and response magnitude. Immunity. 27:203–213. 10.1016/j.immuni.2007.07.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakai A., Hayano Y., Furuta F., Noda M., and Suzuki K.. 2014. Control of lymphocyte egress from lymph nodes through β2-adrenergic receptors. J. Exp. Med. 211:2583–2598. 10.1084/jem.20141132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen K.D., Fentress S.J., Qiu Y., Yun K., Cox J.S., and Chawla A.. 2013. Circadian gene Bmal1 regulates diurnal oscillations of Ly6C(hi) inflammatory monocytes. Science. 341:1483–1488. 10.1126/science.1240636 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pape K.A., Catron D.M., Itano A.A., and Jenkins M.K.. 2007. The humoral immune response is initiated in lymph nodes by B cells that acquire soluble antigen directly in the follicles. Immunity. 26:491–502. 10.1016/j.immuni.2007.02.011 [DOI] [PubMed] [Google Scholar]
- Rosen H., and Goetzl E.J.. 2005. Sphingosine 1-phosphate and its receptors: an autocrine and paracrine network. Nat. Rev. Immunol. 5:560–570. 10.1038/nri1650 [DOI] [PubMed] [Google Scholar]
- Sanders V.M. 2012. The beta2-adrenergic receptor on T and B lymphocytes: do we understand it yet? Brain Behav. Immun. 26:195–200. 10.1016/j.bbi.2011.08.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scheiermann C., Kunisaki Y., Lucas D., Chow A., Jang J.E., Zhang D., Hashimoto D., Merad M., and Frenette P.S.. 2012. Adrenergic nerves govern circadian leukocyte recruitment to tissues. Immunity. 37:290–301. 10.1016/j.immuni.2012.05.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwab S.R., and Cyster J.G.. 2007. Finding a way out: lymphocyte egress from lymphoid organs. Nat. Immunol. 8:1295–1301. 10.1038/ni1545 [DOI] [PubMed] [Google Scholar]
- Silver A.C., Arjona A., Walker W.E., and Fikrig E.. 2012. The circadian clock controls toll-like receptor 9-mediated innate and adaptive immunity. Immunity. 36:251–261. 10.1016/j.immuni.2011.12.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suzuki S., Toyabe S., Moroda T., Tada T., Tsukahara A., Iiai T., Minagawa M., Maruyama S., Hatakeyama K., Endoh K., and Abo T.. 1997. Circadian rhythm of leucocytes and lymphocytes subsets and its possible correlation with the function of the autonomic nervous system. Clin. Exp. Immunol. 110:500–508. 10.1046/j.1365-2249.1997.4411460.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- von Andrian U.H., and Mempel T.R.. 2003. Homing and cellular traffic in lymph nodes. Nat. Rev. Immunol. 3:867–878. 10.1038/nri1222 [DOI] [PubMed] [Google Scholar]
- Xu J., Grewal I.S., Geba G.P., and Flavell R.A.. 1996. Impaired primary T cell responses in L-selectin-deficient mice. J. Exp. Med. 183:589–598. 10.1084/jem.183.2.589 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu X., Rollins D., Ruhn K.A., Stubblefield J.J., Green C.B., Kashiwada M., Rothman P.B., Takahashi J.S., and Hooper L.V.. 2013. TH17 cell differentiation is regulated by the circadian clock. Science. 342:727–730. 10.1126/science.1243884 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.