Abstract
Evidence indicates that many barriers exist to the integration of genetic case finding into primary care. We conducted an exploratory study of the determinants of three specific behaviours related to using breast cancer genetics referral guidelines effectively: ‘taking a family history', ‘making a risk assessment', and ‘making a referral decision'. We developed vignettes of primary care consultations with hypothetical patients, representing a wide range of genetic risk for which different referral decisions would be appropriate. We used the Theory of Planned Behavior to develop a survey instrument to capture data on behavioural intention and its predictors (attitude, subjective norm, and perceived behavioural control) for each of the three behaviours and mailed it to a sample of Canadian family physicians. We used correlation and regression analyses to explore the relationships between predictor and dependent variables. The response rate was 96/125 (77%). The predictor variables explained 38–83% of the variance in intention across the three behaviours. Family physicians' intentions were lower for ‘making a risk assessment' (perceived as the most difficult) than for the other two behaviours. We illustrate how understanding psychological factors salient to behaviour can be used to tailor professional educational interventions; for example, considering the approach of behavioural rehearsal to improve confidence in skills (perceived behavioural control), or vicarious reinforcement as where participants are sceptical that genetics is consistent with their role (subjective norm).
Introduction
The Genetic Testing Registry (http://www.ncbi.nlm.nih.gov/gtr/docs/about/) lists tests for over 6600 genes, covering 3000 conditions. Family physicians (FPs) are often considered to be in an ideal position to provide initial genetic risk assessment and counselling to patients, and studies over more than a decade suggest that practitioners themselves agree that this is an appropriate role.1, 2, 3, 4, 5, 6, 7 However, there is little evidence that FPs are actually integrating genetic case finding into their practices,7, 8, 9, 10 and primary care may be poorly prepared for the expansion of genomics technologies, and changing patient expectations.
Family physicians need to be adequately prepared to assess genetic risk, identify, and counsel those who are eligible for referral to specialist clinics, and help plan preventive and health promotion strategies tailored to patients' disease risks. There are multiple barriers to achieving this, including concerns about the complexities of genetic testing;5, 6 discomfort about the absence of effective interventions;4, 7 and lack of skills in collecting genetic family histories and providing appropriate counselling.3, 4, 7, 9 These influence confidence in managing patients' concerns, and FPs may not feel adequately prepared for these roles.
The fundamental attributes of family practice are common across many health systems, but interventions designed to encourage the integration of genetics into practice need to be sustainable and cost-effective. Continuing medical education programmes offer the most widely available vehicle for initiating and supporting behaviour change. In general, small behaviour changes may be attainable through interactive educational interventions,11, 12 but their effects are likely to be limited. In relation to genetics, studies have demonstrated that educational programmes may enhance knowledge and confidence without necessarily altering utilisation of genetic counselling services13 or referral behaviour.14 A Cochrane review suggested that educational meetings alone are not effective in optimising clinical care by health professionals.15 Taken together, these observations suggest that a deeper understanding of the complex influences on health professionals' behaviour may be required to develop educational strategies that are more finely tuned to learners' needs, although still deliverable through current continuing medical education approaches.16, 17, 18, 19
In an effort to contribute to this understanding, we embedded a theoretically-based study within a randomised controlled trial (the GenetiKit trial, reported elsewhere).20 The trial intervention was a multifaceted ‘knowledge translation' approach, with an interactive and peer-led educational session, a portfolio of point-of-care tools (eg, for family history taking), a ‘push' knowledge service that provided timely, rapid, evidence-based, practitioner-friendly summaries of genetic tests in the news, and a website with reference information. Participants in the control arm received the recently developed provincial guidelines for cancer genetics referral.
The analyses presented here were based on the data collected during the pre-intervention phase. We used the Theory of Planned Behavior (TPB)21, 22 to examine the determinants of participants' referral intentions. The TPB is one of the most thoroughly tested and robust of the social psychological models, and has well defined psychological constructs that are straightforward to operationalise.23 Meta-analyses have found the TPB useful for predicting a range of behaviours,24 particularly health behaviours.25, 26 The model has frequently been used to explore health professionals' beliefs and intentions towards various clinical behaviours (eg, ref. 27, 28, 29, 30).
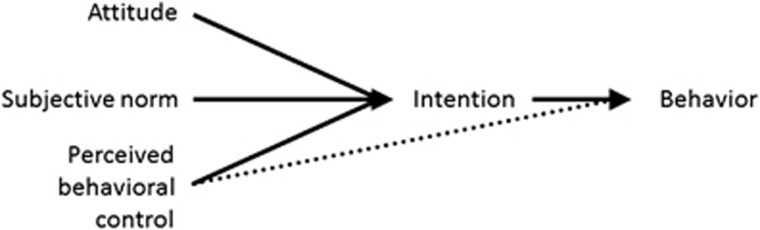
The TPB proposes that proximal determinants of a behaviour of interest are (a) the strength of an individual's behavioural intention and (b) the degree of control felt by the individual over that behaviour.21 Behavioural intention is determined by the three constructs: attitude (being in favour of, or against, carrying out the behaviour), subjective norm (perceived pressure from others to do or not to do it), and perceived behavioural control (beliefs about factors likely to facilitate or inhibit the behaviour) (Figure 1). Demographic and personality factors are assumed to affect behaviour indirectly through their influence on attitude, subjective norm, and perceived behavioural control.21
Figure 1.
Theory of Planned Behavior.21
The aim of this study was to use the TPB as a lens to examine the behaviours underlying cancer genetics referral decision making by FPs, to clarify whether tailoring continuing medical education interventions might offer a useful way forward to support the implementation of genetics in primary care.
Materials and methods
Participants and recruitment
Study participants were FPs in active practice at four locations in Ontario, Canada, who had agreed to take part in the GenetiKit trial.20
Measures
Within the general idea of ‘genetics referral decision making' about hereditary breast/ovarian cancer, we identified three target behaviours for examination, which we explained fully in the preamble to the questionnaire:
Taking a family history when a patient presents with concerns about risk of hereditary breast/ovarian cancer (‘taking a family history').
Using the information to make one's own assessment of the patient's risk of hereditary breast/ovarian cancer (‘making a risk assessment').
Making a decision about whether or not to refer the patient to specialist genetic services, based on current guidance (‘making a referral decision').
We selected these behaviours as clinically important and related directly to the intended use of the guideline. The dependent variable was behavioural intention, used as a proxy for actual behaviour, for two reasons. First, the primary outcome for the main trial related to responses to a set of clinical vignettes, not actual referral behaviour. Second, behavioural intention is commonly used as the dependent variable in TPB studies and has been shown to be consistently correlated with actual behaviour.31, 32
Items measuring the relevant psychological variables were derived from those developed for the previous studies, and a survey instrument was developed and piloted in its entirety using standard approaches with five FPs not involved in the study.21, 33 Supplementary Table S1 (online) provides the wording for all items in the instrument. To illustrate, we present the sample items relating to ‘taking a family history':
‘I expect to take a family history when patients present with concerns about risk of hereditary breast/ovarian cancer' (strongly agree/strongly disagree); (intention).
‘Taking a family history when patients present with concerns about risk of hereditary breast/ovarian cancer is (very easy/very difficult)' (perceived behavioural control, three items).
Responses were measured on seven-point likert scales and, for analyses, responses were coded so that higher scores reflected stronger intention to perform the behaviour, more positive attitude towards the behaviour, perception of stronger social pressure to perform the behaviour, or perception of greater control over the behaviour. For each variable, a mean score was calculated from the relevant items.
Procedure
Questionnaires were mailed to GenetiKit trial participants (intervention and control) in the pre-intervention phase (2006). Reminders were sent at 3 and 6 weeks. Participants were given CAD125 to partially compensate them for time spent completing questionnaires throughout the study.
Sample size and analysis
The sample size was determined by the primary outcome measures and analysis plan developed for the main trial.20 For the TPB analyses, a minimum sample size of 50+8m (where m is the number of predictors) is recommended for testing the multiple correlation in a regression equation.34 Given three predictor variables for each behavioural outcome variable, we estimated a minimum required sample size of 75.
The internal consistency of the items used to measure the TPB constructs was explored using Cronbach's α. Spearman's correlation coefficients were computed between all the studied variables. Multiple linear regression analyses were performed to explore the predictive value of each construct for behavioural intentions of the three target behaviours. The relative importance of predictor constructs was assessed by inspecting the standardised regression coefficients (β). Three partial correlations were computed to assess any association between two behavioural intention scores whereas controlling for the third.
The study was approved by the Mount Sinai Hospital Research Ethics Board, the North York General Hospital Ethics Board, and the Ottawa Hospital Research Ethics Board.
Results
Of 125 FPs who consented to participate in the GenetiKit trial, 96 responded to the baseline survey (response rate 76.8%). Fifty four (56%) were females, with a mean (SD) age of 50 10 years. On average, they had been practising for 18.8 (10.8) years, with ~30 h (11.2) of direct patient care weekly. Eighty (83%) worked in medium-to-large cities and 59 (61%) worked in group practice settings.
Tables 1, 2, 3 show the mean values for the four psychological measures relating to the three behaviours. Acceptable levels of internal reliability (Cronbach's α >0.7) were achieved except for the measures of attitude and perceived behavioural control for ‘taking a family history' (Table 1). Internal reliability for the subjective norm was not assessed as different sources of social pressure may be perceived to exert independent effects.33 The skewness statistic for the frequency distributions (Table 1) fell within the acceptable range of −1 to 1 except for behavioural intention and subjective norms for ‘taking a family history' and intention for ‘making a referral decision'. These were negatively skewed beyond −1, suggesting scores clustered towards the upper end of the scale. χ2-tests for homogeneity revealed no differences in intention scores between male and female physicians, or between physicians aged <50 and ≥50, for ‘making risk assessment' and ‘making referral decision' (P=0.783 and P=0.085, respectively). Noting a ceiling effect for intention scores relating to ‘taking a family history', we did not conduct tests for homogeneity for this with the demographic variables.
Table 1. Psychological measures.
| Behaviour | Measure | No. of items | Cronbach's α | Mean (SD) | Median (range) | Percentile (25, 75) | Skewness |
|---|---|---|---|---|---|---|---|
| Taking a family history | Behavioural intention | 3 | 0.87 | 6.80 (0.38) | 7.0 (5.67–7.0) | 6.67, 7.0 | −1.88 |
| Attitude | 4 | 0.54 | 6.57 (0.46) | 6.75 (5.25–7.0) | 6.25, 7.0 | −0.93 | |
| Subjective norm | 4 | a | 6.38 (0.68) | 6.5 (3.5–7.0) | 6.0, 7.0 | −1.48 | |
| Perceived behavioural control | 3 | 0.52 | 5.48 (1.1) | 5.67 (2.33–7.0) | 4.67, 6.33 | −0.60 | |
| Making a risk assessment | Behavioural intention | 3 | 0.87 | 4.63 (1.57) | 4.67 (1.0–7.0) | 3.67, 6.0 | −0.49 |
| Attitude | 4 | 0.91 | 5.17 (1.35) | 5.50 (1.5–7.0) | 4.25, 6.25 | −0.65 | |
| Subjective norm | 4 | a | 4.79 (1.49) | 5.0 (1.0–7.0) | 3.75, 6.0 | −0.51 | |
| Perceived behavioural control | 3 | 0.66 | 3.88 (1.21) | 4.0 (1.0–7.0) | 3.0, 4.67 | −0.05 | |
| Making a referral decision | Behavioural intention | 3 | 0.85 | 6.07 (0.93) | 6.00 (2.67–7.0) | 5.50, 7.0 | −1.11 |
| Attitude | 4 | 0.84 | 5.99 (0.82) | 6.00 (3.75–7.0) | 5.50, 6.75 | −0.58 | |
| Subjective norm | 4 | a | 5.82 (0.96) | 6.00 (3.25–7.0) | 5.25, 6.75 | −0.60 | |
| Perceived behavioural control | 3 | 0.64 | 5.04 (1.17) | 5.0 (2.0–7.0) | 4.30, 6.75 | −0.57 |
Not assessed.
Table 2. Correlations between psychological variables (Spearman's rho).
| Behavioural intention | Attitude | Subjective norm | |
|---|---|---|---|
| Taking a family history | |||
| Attitude | 0.58* | — | — |
| Subjective norm | 0.47* | 0.56* | — |
| Perceived behavioural control | 0.25** | 0.28* | 0.32* |
| Making a risk assessment | |||
| Attitude | 0.83* | — | — |
| Subjective norm | 0.86* | 0.80* | — |
| Perceived behavioural control | 0.61* | 0.52* | 0.52* |
| Making a referral decision | |||
| Attitude | 0.82* | — | — |
| Subjective norm | 0.79* | 0.74* | — |
| Perceived behavioural control | 0.63* | 0.59* | 0.52* |
P<0.05 (two-tailed).
P<0.01 (two-tailed).
Table 3. Regression analyses predicting intentions.
| Behaviour | Standardised β | Adjusted R2 | df | F |
|---|---|---|---|---|
| Taking a family history | ||||
| Intention | 0.385 | 3.91 | 20.61 | |
| Predictor | ||||
| Attitude | 0.439* | |||
| Subjective norm | 0.268* | |||
| Perceived behavioural control | 0.069 | |||
| Making a risk assessment | ||||
| Intention | 0.833 | 3.91 | 156.85 | |
| Predictor | ||||
| Attitude | 0.396* | |||
| Subjective norm | 0.453* | |||
| Perceived behavioural control | 0.166* | |||
| Making a referral decision | ||||
| Intention | 0.75 | 3.90 | 94.08 | |
| Predictor | ||||
| Attitude | 0.527* | |||
| Subjective norm | 0.221* | |||
| Perceived behavioural control | 0.241* | |||
P<0.05 (two-tailed)
.
Behaviour 1: taking a family history
As shown in Table 1, the median behavioural intention score for this behaviour (7.0) was very high, with little variation within the respondent sample. The mean scores for measures of attitude, subjective norm, and perceived behavioural control were also clearly positive, although the SD for the last (1.1) was greater than for the other measures. Using Cohen's interpretation35 for describing the effect sizes of correlations, and relationships between the predictor measures and intention were low to moderate for this behaviour (Table 2). The multiple regression analysis (Table 3) indicated that, together, the predictor variables explained 38% of the variance in behavioural intention for ‘taking a family history', with attitude and subjective norm both being statistically significant predictors (P<0.05).
Behaviour 2: making a risk assessment
Table 1 shows that mean scores indicating positive evaluations were observed for behavioural intention, attitude, and subjective norm, with highly variable responses (SDs in the range 1.35–1.57). The scores for this behaviour covered the entire range of possible responses, from 1 to 7, the widest observed for the three behaviours of interest. The mean score for perceived behavioural control (3.88) indicated a negative evaluation, with a similar SD (1.21) to the other measures. The correlations between the predictor measures, and between the predictor measures and behavioural intention, were moderate to high (Table 2). Together, the predictor variables explained 83% of the variance in behavioural intention for making a risk assessment, with all the three predictor variables reaching statistical significance (Table 3).
Behaviour 3: making a referral decision
The mean intention score for this behaviour (6.07) was very high, with high scores also observed for attitude, subjective norm, and perceived behavioural control (Table 1). The SD for perceived behavioural control (1.17) was highest, and for all the measures the range of responses encompassed clearly negative evaluations (<4) as well as very positive. Moderate to high correlations were observed between the individual predictor measures, and between the predictor variables and behavioural intention (Table 2). Table 3 indicates that the predictor variables explained 75% of the variance in behavioural intention, all statistically significant.
We found only one statistically significant partial correlation between intention scores, between ‘taking a family history' and ‘making a referral decision' (r=0.31, P<0.01).
Discussion
This study was designed to understand more deeply some individual psychological factors that might facilitate or impede FPs in carrying out tasks associated with their role in genetics. Overall, we found that the TPB constructs provided useful insight into three key behaviours, and the analyses suggest potential targets for continuing medical education beyond standard information provision about genetic disorders. Separating the complex behaviour of applying referral criteria in patient assessment and management into three tasks was informative. Overall, the scores suggest very high FP intentions for ‘taking a family history' and ‘making a referral decision', but more moderate and variable intentions relating to ‘making a risk assessment'.
Important differences emerged when the three behaviours were compared. ‘Taking a family history' had the most positive scores across all the variables, with extremely high and consistent scores for intention in particular. This appeared to be driven both by positive evaluations of the value of family history taking (attitude) and of this as a normal activity for FPs (subjective norm). However, the range of responses for the subjective norm and perceived behavioural control variables (and the wider SD for the latter) indicate that not all respondents rated family history taking in this context as either expected of them or as something about which they felt confident. These data suggest that although FPs appeared consistently supportive of family history taking in inherited cancer risk assessment, a proportion were in fact sceptical that this should be part of their own practice and, for some, low intentions were associated with lack of confidence in taking a family history.
In contrast, for the behaviour ‘making a risk assessment', the analyses indicate a much broader set of reactions, such that some respondents appeared extremely positive in all respects, whereas others clearly did not intend to carry out this behaviour, saw no value in it, felt little pressure from colleagues to do it, and/or would not feel confident in doing it anyway. If valid, these observations indicate a quite different set of educational challenges.
Finally, for the behaviour ‘making a referral decision', overall positive scores were observed, again with some heterogeneity in all the psychological measures. The perceived behavioural control variable had the largest SD, and all measures had some responses in the negative range of the scale (though not as extreme as for ‘making a risk assessment'). All three predictor variables appeared to contribute independently to behavioural intention. This is perhaps the most difficult behaviour of the three to interpret. Although we took pains to describe this behaviour carefully in the survey instrument (referral criteria being actively applied in a decision about whether or not to refer a patient for specialist assessment), and pilot tested for comprehension, it is possible that some respondents interpreted it as ‘deciding to refer'.
Taken at face value, moderate to high scores were observed for this behaviour and its predictor variables, with the range for each encompassing negative as well as extremely positive evaluations. As well as receiving the lowest mean score within this set, perceived behavioural control also had a larger SD than the other variables. All three variables statistically significantly predicted intention, and together they explained three quarters of the variance in behavioural intention.
The implications of these findings for the design of interventions to support practice improvements are presented in Table 4. We argue that interventions to support clinical behaviour change may be more effective if they are tailored to specific barriers to change.36 The recent behaviour change literature provides evidence to inform this approach. Theoretical constructs (eg, attitude and subjective norm) may be characterised in terms of ‘theoretical domains' (clusters of similar constructs).37 Framing barriers to change in terms of theoretical domains provides a systematic method for intervention design: specific evidence-based techniques can be selected to target each domain38 and combined to design a bespoke intervention. To illustrate, Table 4 presents the key constructs that predicted intention in the present study, the theoretical domains that these constructs imply, the behaviour change techniques that would address these domains,39 and examples of how they might be delivered in the context of an educational intervention: overall, a systematic approach to tailored intervention design. Further examples of this approach are published in the implementation science literature (eg, ref. 40). The behaviour change techniques could also be delivered as part of the other approaches to enhancing quality of care, such as communities of practice, local opinion leaders, or tailored interventions.41
Table 4. Constructs predicting intention, implied theoretical domains, and behaviour change techniques.
| Constructs predicting intentiona | Relevant theoretical domain37 | Behaviour change techniques targeting domain38, 39 | Example of intervention tailored to target behaviour |
|---|---|---|---|
| Attitude | Beliefs about consequences | Social and environmental consequences | Facilitator points out expectations of concerned patients for immediate risk assessment and likelihood of greater satisfaction if this occurs. |
| Pros and cons | Facilitator asks participants to generate a list of the positive and negative consequences of making a risk assessment during the consultation. | ||
| Subjective norm | Social influences | Social comparison | Facilitator asks participants who routinely make a risk assessment in this context to describe a recent example. |
| Modelling/demonstrating the behaviour | Facilitator asks participants who routinely make a risk assessment to talk through the factors they consider. | ||
| Social reward | Facilitator congratulates participants on their good practice. | ||
| Vicarious reinforcement | Facilitator congratulates participants who already perform the action on their good practice, in the presence of those who do not. | ||
| Perceived behavioural control | Beliefs about capabilities | Verbal persuasion to boost self-efficacy | Facilitator points out that participants often do risk assessment well in other clinical situations, and the similarity of the skills required in this context. |
| Focus on past success | Facilitator asks participants to reflect their risk assessment skills in other contexts, then demonstrates the behaviour to illustrate the skills as generic. | ||
| Skills | Graded tasks, behavioural rehearsal/practice | Facilitator provides a template listing key family history information that is taken into account in a risk assessment and in three patient scenarios. Participants complete template to generate risk assessments. Starting with very easy, the three scenarios are of increasing difficulty. The scenarios and decisions are then discussed in break-out groups. |
From Table 3.
Tailoring of educational approaches may also need to take account of different FP roles or patient populations, for example, those with an emphasis on prenatal practice compared with those providing care across the lifespan. Genetic case finding will tend to emphasise different conditions at different life stages, and discomfort with, for example, ethical implications might vary across genetic tests and patient populations. This may introduce differences between FP groups across any of the theoretical domains, supporting the case for thoughtful educational ‘needs assessment' as a prerequisite for intervention design.7,41
This study had several strengths. It used a well established psychological theory shown to be of value in research across many areas of clinical behaviour27, 28, 29, 30 and achieved a high response rate. In assessing multiple related behaviours, it recognises the complexity of clinical care in this area. In addition to confirming the importance of attitude, it illuminates the influence of peers and patients in promoting expectations, and the importance of identifying perceived barriers to carrying out desired behaviours. This approach lends itself to identifying modifiable predictors of behaviour for which specific interventions can be developed, and then tested formally in experimental studies.
A major limitation was the absence of objective measures of the behaviours of interest. This is often difficult because of patient confidentiality as well as logistics. A recent review of 10 prospective studies reported a correlation of 0.15–0.40 between intention and behaviour.31 A separate synthesis estimated that, on average, 28% of the variance in behaviour is accounted for by intention.32
It is likely that the GenetiKit trial participants were more interested in genetics than the average FP, thus generating higher scores for attitude and possibly other domains, limiting the study's external validity. On the other hand, the confidence levels of this sample for genetics case finding may be higher than for the typical FP, emphasising the need for interventions that focus on behaviour change rather than information provision. The cross-sectional design also does not allow us to infer causality. We noted that our measures had lower than desirable internal consistency, which could have led to an underestimation of the strength of the true relationships. In addition, the high intention scores we observed may be explained in part by social desirability bias.
Overall, this study raises further questions. The very positively skewed results for the behavioural intention ‘taking a family history', may reflect the targeted and condition-specific approach. We might expect that greater variation would be observed for family history taking in other contexts (eg, independent of patient complaint or guideline) emphasising importance of specifying a target behaviour very precisely. Similarly, we need to understand better why consistently lower scores on all the psychological factors were observed for ‘making a risk assessment' compared with the other behaviours. Risk stratification criteria for hereditary cancer syndromes may be presented in ways that do not facilitate easy use by primary care practitioners, suggesting scope for improvement.42 In considering ‘education' in a field as complex and evolving as genomics in health care, it might be productive to consider the role of point-of-care tools designed specifically to complement the focus on competencies, content knowledge, and attitudes.43
In conclusion, this study demonstrated that the application of a psychological model such as the TPB offers useful and specific insights into the factors that influence practitioners' behaviour relating to hereditary cancer risk assessment and referral decision making. The findings suggest that, to be effective, educational approaches would need to be different for the three behaviours of interest. Future research should focus on further exploring factors influencing FPs' practice regarding making genetic risk assessments, identifying intention-behaviour relationships, and exploring the generalisability of the findings to other aspects of genetics in primary care.
Acknowledgments
JCC holds the Sydney G Frankfort Chair in Family Medicine. JMG holds a Canada Research Chair in Health Knowledge Transfer and Uptake. Heather Howley provided research administrative support. Project funded by Canadian Institutes of Health Research Knowledge Translation Strategies grant KTS-62357. The Health Services Research Unit is funded by the Chief Scientist Office of the Scottish Government Health and Social Care Directorates.
The authors declare no conflict of interest.
Footnotes
Supplementary Information accompanies this paper on European Journal of Human Genetics website (http://www.nature.com/ejhg)
Supplementary Material
References
- Carroll JC, Brown JB, Blaine S, Glendon G, Pugh P, Medved W: Genetic susceptibility to cancer: family physicians' experience. Can Fam Physician 2003; 49: 45–52. [PMC free article] [PubMed] [Google Scholar]
- Trinidad SB, Fryer-Edwards K, Crest A, Kyler P, Lloyd-Puryear MA, Burke W: Educational needs in genetic medicine: primary care perspectives. Community Genet 2008; 11: 150–155. [DOI] [PubMed] [Google Scholar]
- Wood ME, Stockdale A, Flynn BS: Interviews with primary care physicians regarding taking and interpreting the cancer family history. Fam Pract 2008; 25: 334–340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McMahon D, Holder R, Metcalfe A et al: General practitioners' attitudes to assessment of genetic risk of common disorders in routine primary care. Clin Genet 2009; 76: 544–551. [DOI] [PubMed] [Google Scholar]
- Houwink EJF, van Luijk SJ, Henneman L, van der Vleuten C, Dinant GJ, Cornel MC: Genetic educational needs and the role of genetics in primary care: a focus group study with multiple perspectives. BMC Fam Pract 2011; 12: 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mainous AG3rd, Johnson SP, Chirina S, Baker R: Academic family physicians' perception of genetic testing and integration into practice: a CERA study. Fam Med 2013; 45: 257–262. [PubMed] [Google Scholar]
- Mikat-Stevens NA, Larson IA, Tarini BA: Primary-care providers' perceived barriers to integration of genetics services: a systematic review of the literature. Genet Med 2015; 17: 169–176. [DOI] [PubMed] [Google Scholar]
- Bonter K, Desjardins C, Currier N, Pun J, Ashbury FD: Personalised medicine in Canada: a survey of adoption and practice in oncology, cardiology and family medicine. BMJ Open 2011; 1: e000110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christianson CA, Powell KP, Hahn SE et al: The use of a family history risk assessment tool within a community health care system: views of primary care providers. J Genet Couns 2012; 21: 652–661. [DOI] [PubMed] [Google Scholar]
- Bell RA, McDermott H, Fancher TL, Green MJ, Day FC, Wilkes MS: Impact of a randomized controlled educational trial to improve physician practice behaviors around screening for inherited breast cancer. J Gen Intern Med 2014; 30: 334–341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis D, O'Brien MAT, Freemantle N, Wolf FM, Mazmanian P, Taylor-Vaisey A: Impact of formal continuing medical education. Do conferences, workshops, rounds, and other traditional continuing education activities change physician behavior or health care outcomes? JAMA 1999; 282: 867–874. [DOI] [PubMed] [Google Scholar]
- Grimshaw JM, Eccles MP, Walker AE, Thomas RE: Changing physicians' behavior: what works and thoughts on getting more things to work. J Contin Educ Health 2002; 22: 237–243. [DOI] [PubMed] [Google Scholar]
- Clyman JC, Nazir F, Tarolli S, Black E, Lombardi RQ, Higgins JJ: The impact of a genetics education program on physicians' knowledge and genetic counseling referral patterns. Med Teach 2007; 29: 143–150. [DOI] [PubMed] [Google Scholar]
- Houwink EJF, Muijtjens AMM, van Teeffelen SR et al: Effect of comprehensive oncogenetics training interventions for general practitioners, evaluated at multiple performance levels. PLoS One 2015; 10: e0122648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forsetlund L, Bjørndal A, Rashidian A et al: Continuing education meetings and workshops: effects on professional practice and health care outcomes. Cochrane Database Syst Rev 2009; CD003030. [DOI] [PMC free article] [PubMed]
- Farndon PA, Bennett C: Genetics education for health professionals: strategies and outcomes from a national initiative in the United Kingdom. J Genet Couns 2008; 17: 161–169. [DOI] [PubMed] [Google Scholar]
- Graham ID, Tetroe J: Some theoretical underpinnings of knowledge translation. Acad Emerg Med 2007; 14: 936–941. [DOI] [PubMed] [Google Scholar]
- Eccles M, Grimshaw J, Walker A, Johnston M, Pitts N: Changing the behavior of healthcare professionals: the use of theory in promoting the uptake of research findings. J Clin Epidemiol 2005; 58: 107–112. [DOI] [PubMed] [Google Scholar]
- Godin G, Bélanger-Gravel A, Eccles M, Grimshaw J: Healthcare professionals' intentions and behaviours: a systematic review of studies based on social cognitive theories. Implement Sci 2008; 3: 36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll JC, Wilson BJ, Allanson J et al: GenetiKit: a randomized controlled trial to enhance delivery of genetics services by family physicians. Fam Pract 2011; 28: 614–623. [DOI] [PubMed] [Google Scholar]
- Ajzen I: The theory of planned behavior. Org Behav Hum Dec 1991; 50: 179–211. [Google Scholar]
- Conner M, Sparks P: The theory of planned behaviour and health behaviour; in Conner M, Norman P (eds): Predicting Health Behaviour. Maidenhead, UK: Open University Press, 2005; pp 170–222. [Google Scholar]
- Gagné C, Godin G: Les Theories Sociales Cognitives: Guide pour la Mesure des Variables et le Developpement de Questionnaire. Quebec, QC, Canada: Faculté des Sciences Infirmières, Université Laval, 1999. [Google Scholar]
- Armitage CJ, Conner M: Efficacy of the theory of planned behavior: a meta analytic review. Br J Soc Psychol 2001; 40: 471–499. [DOI] [PubMed] [Google Scholar]
- Godin G, Kok G: The theory of planned behavior: a review of its applications to health-related behaviors. Am J Health Promot 1996; 1: 87–98. [DOI] [PubMed] [Google Scholar]
- Sheeran P, Orbell S: Do intentions predict condom use? Meta-analysis and examination of six moderator variables. Br J Soc Psychol 1998; 37: 231–250. [DOI] [PubMed] [Google Scholar]
- Braithwaite D, Sutton S, Smithson WH, Emery J: Internet-based risk assessment and decision support for the management of familial cancer in primary care: a survey of GPs attitudes and intentions. Fam Pract 2002; 19: 587–590. [DOI] [PubMed] [Google Scholar]
- Jenner EA, Watson PWB, Miller L, Jones F, Scott GM: Explaining hand hygiene practice: an extended application of the theory of planned behavior. Psychol Health Med 2002; 7: 311–326. [Google Scholar]
- Limbert C, Lamb R: Doctors' use of clinical guidelines: two applications of the theory of planned behavior. Psychol Health Med 2002; 7: 301–310. [Google Scholar]
- Walker A, Watson M, Grimshaw J, Bond C: Applying the theory of planned behavior to pharmacists' beliefs and intentions about the treatment of vaginal candidiasis with non-prescription medicines. Fam Pract 2004; 21: 670–676. [DOI] [PubMed] [Google Scholar]
- Eccles MP, Hrisos S, Francis J et al: Do self-reported intentions predict clinicians' behavior: a systematic review. Implement Sci 2006; 1: 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheeran P: Intention-behavior relations: a conceptual and empirical review. Eur Rev Soc Psychol 2002; 12: 1–36. [Google Scholar]
- Francis JJ, Eccles MP, Johnston M et alConstructing questionnaires based on the theory of planned behaviour: a manual for health services researchers 2004. Available at http://openaccess.city.ac.uk/1735/1/ accessed 23 January 2014.
- Green SB: How many subjects does it take to do a regression analysis. Multivariate Behav Res 1991; 26: 499–510. [DOI] [PubMed] [Google Scholar]
- Cohen J: A power primer. Psychol Bull 1992; 112: 155–159. [DOI] [PubMed] [Google Scholar]
- Baker R, Camosso-Stefinovic J, Gillies C et al: Tailored interventions to address determinants of practice. Cochrane Database Syst Rev 2015; 4: CD005470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cane J, O'Connor D, Michie S: Validation of the theoretical domains framework for use in behaviour change and implementation research. Implement Sci 2012; 7: 37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cane J, Richardson M, Johnston M, Ladha R, Michie S: From lists of BCTs to structured hierarchies: comparison of two methods of developing a hierarchy of BCTs. Br J Health Psychol 2015; 20: 130–150. [DOI] [PubMed] [Google Scholar]
- Michie S, Richardson M, Johnston M et al: The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med 2013; 46: 81–95. [DOI] [PubMed] [Google Scholar]
- French SD, Green SE, O'Connor D et al: Developing theory-informed interventions to implement evidence into practice: a systematic approach using the theoretical domains framework. Implement Sci 2012; 7: 38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Presseau J, Ivers NM, Newham JJ, Knittle K, Danko KJ, Grimshaw JM: Using a behaviour change techniques taxonomy to identify active ingredients within trials of implementation interventions for diabetes care. Implement Sci 2015; 10: 55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gagliardi AR, Brouwers MC, Palda VA, Lemieux-Charles L, Grimshaw JM: How can we improve guideline use? A conceptual framework of implementability. Implement Sci 2011; 6: 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korf BR: Genetic and genomic competency in medical practice. Virtual Mentor 2012; 14: 622–626. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.