Abstract
Stroke, which is defined as a neurologic deficit caused by sudden impaired blood supply, has been considered as a common cause of death and disability for decades. The World Health Organization has declared that almost every 5 seconds a new stroke occurs, placing immense socioeconomic burdens. However, the effective and available treatment strategies are still limited. Additionally, the most effective therapy, such as thrombolysis and stenting for ischemic stroke, generally requires a narrow therapeutic time window after the event. A large majority of patients cannot be admitted to hospital and receive these effective treatments for reperfusion timely. Hyperbaric oxygen therapy (HBOT) has been frequently applied and investigated in stroke since 1960s. Numerous basic and clinical studies have shown the beneficial efficacy for neurological outcome after stroke, and meanwhile many underlying mechanisms associated with neuroprotection have been illustrated, such as cerebral oxygenation promotion and metabolic improvement, blood-brain barrier protection, anti-inflammation and cerebral edema, intracranial pressure modulation, decreased oxidative-stress and apoptosis, increased vascular and neural regeneration. However, HBOT in human stroke is still not sufficiently evidence-based, due to the insufficient randomized double-blind controlled clinical studies. To date, there are no uniform criteria for the dose and session duration of HBOT in different strokes. Furthermore, the additional effect of HBOT combined with drugs and other treatment strategies are being investigated recently. Therefore, more experimental and clinical research is imperative to identify the mechanisms more clearly and to explore the best protocol of HBOT in stroke treatment.
Keywords: hyperbaric oxygen therapy, hyperbaric oxygen preconditioning, stroke, experimental studies, clinical studies, ischemia, cerebrovascular disease
INTRODUCTION
Stroke is identified as a sudden neurological deficit of cerebrovascular origin and has been considered as an important leading cause of death and disability all over the world (Bath and Lees, 2000). The high morbidity and mortality as well as disability rate of this catastrophic illness create a huge burden for human society and families, making it a public health issue. In addition, as the aging of population in many industrialized nations (Toole, 2011), the severity of stroke will increase year by year. As a result, the number of neurologists, neuroscientists and neurosurgeons focusing on stroke research as well as the amount of the funding for stroke study has grown substantially in the past few decades (Zhu et al., 2015).
Generally speaking, stroke can be divided into ischemic and hemorrhagic stroke, the former accounting for approximate 80% of them (Grysiewicz et al., 2008). Current studies have shown that both hemorrhage within the brain and primary ischemia can cause a lack of oxygenation and nutritional supply and a series of neurochemical events that lead to spreading brain damage. At present, anti-stroke therapies mainly concentrate on stenting and angioplasty, thrombolytic agents, surgical treatment, neuroprotective drugs, stabilization of intracranial pressure and rehabilitation training (Zhao et al., 2014; Kuan and Sun, 2015). As a result of such limited available therapeutic options, new treatment strategies need to be developed to improve the long-term neurological outcome following stroke.
Hyperbaric oxygen therapy (HBOT), as a nondrug and noninvasive treatment, has long been commonly applied in the treatment of stroke since 1960s and has been proved to be a safe and beneficial treatment strategy, although some controversies still exist (Ding et al., 2014). It is well acknowledged that brain cells rely exclusively on aerobic metabolism and need a high consumption of oxygen as well as glucose to produce adequate tri-phosphate for neuronal signal transduction (Wang et al., 2014), therefore brain is one of the most vulnerable organ to hypoxia. Numerous previous studies (Nemoto and Betterman, 2007; Matchett et al., 2009) have demonstrated that HBOT can enhance the cerebral oxygenation and have many other neuroprotective effects through various physiologic, biochemical and metabolic mechanisms. In this article, we will discuss the HBOT influence for stroke injury and the potential mechanisms on the basis of experimental research and clinical studies.
MECHANISMS OF HBOT IN STROKE
At the pressure of sea level which represents 1 atmosphere absolute (1 ATA=101.3 kPa), we breathe the air with only about 21% oxygen. The amount of blood oxygen includes hemoglobin-bounded oxygen and dissolved oxygen in the blood plasm. The arterial oxygen saturation in the blood is nearly 100% in physiologic conditions, which means almost all the hemoglobin is bounded with oxygen and only little can be increased (Calvert et al., 2007; Michalski et al., 2011a). However, the approximate proportion of oxygen dissolved in plasma is merely 0.29 mL every 100 mL blood (0.3% (v/v)). While inspiring 100% oxygen in high pressures (more than 1 ATA) under the hyperbaric oxygen condition, the amount of oxygen dissolved in blood plasma can increase to 3.26% (v/v) at 1.5 ATA and to 5.6% (v/v) at 2.5 ATA. Thereby, HBOT is mainly used to improve this part of dissolved oxygen in plasma then increase tissue oxygen concentration in the ischemic area. According to common knowledge, oxygen spread along the pressure gradient, so hyperbaric condition can make oxygen diffuse to hypoxic tissue more easily and for a longer effective diffusion distance than normabaric oxygen (Gjedde, 2005). HBOT involves a well-sealed chamber with pure oxygen to maintain high pressures. Frequently animal studies use pressures ranging from 1.5 to 3.0 ATA, and duration of treatment ranging 1–3 hours (Michalski et al., 2011a). Clinical studies may apply single or multiple therapeutic sessions with each duration lasting 30-90 minutes and pressures varying from 1.3 to 2.5 ATA (Helms et al., 2011; Michalski et al., 2011a; Efrati et al., 2013; Efrati and Ben-Jacob, 2014), but a study by Efrati and Ben-Jacob (2014) indicated HBOT above 2.0 ATA may have undesirable neurofunctional inhibition and even focal toxicity. Besides, gradual compression and decompression (5-15 minutes) before and after treatment is usually used for the safety and comfort of patients with stroke insult.
Tissue hypoxia has been considered as the key contributor to cellular injury after stroke, so most of early studies were based on the higher dissolved oxygen concentration in plasma achieved with HBOT. In recent years, studies (Singhal, 2007) have illustrated that HBOT may also accomplish neuroprotective effects in stroke via a variety of complex molecular, biochemical and hemodynamic mechanisms: (1) HBOT is capable of enhancing the arterial partial pressure of oxygen, improving oxygen delivery and increasing oxygen supply for brain tissue; (2) HBOT can stabilize the blood-brain barrier (BBB) and reduce cerebral edema (Chen et al., 2011b); (3) ameliorate cerebral microcirculation and improve brain metabolism to create sufficient energy, preserve cellular ion homeostasis (Zhang et al., 2005); (4) decrease the intracranial pressure via modulating cerebral blood flow and brain edema reduction; (5) HBOT alleviates post-stroke neuroinflammation; (6) inhibit post-stroke cell apoptosis and necrosis; (7) improve the microcirculation of anoxic area and reduce cerebral hypoxia-ischemia (Siesjo, 1988); (8) appropriate and timely application of HBOT will alleviate oxidative stress and suppress the ischemia-reperfusion injury which is generally recognized as one of the core pathophysiology in stroke injury (Sanchez, 2013); (9) furthermore, it has been demonstrated that when HBOT is used to treat patients with aneurysmal subarachnoid hemorrhage (SAH), it may attenuate cerebral vascular spasm induced by SAH (Ostrowski and Zhang, 2011); (10) finally, HBOT is also confirmed favorable to neurogenesis and angiogenesis.
EXPERIMENTAL STUDIES OF HBOT IN STROKE
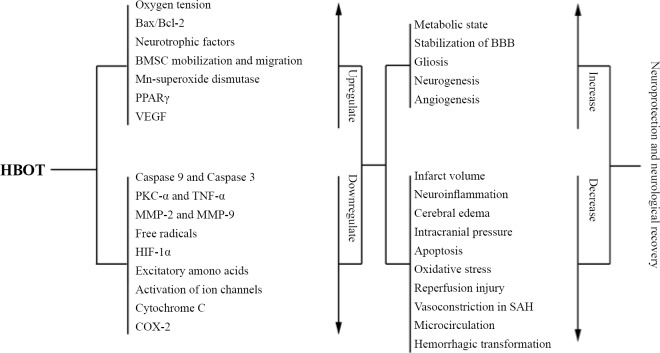
In animal experimental studies, animal models of hemorrhagic or ischemic stroke were successfully made firstly, then hyperbaric oxygen was applied to treat the subject after stroke insult, and finally the investigators detected the effects on stroke of HBOT and explored the potential mechanisms of the effects. In general, animal studies belong to basic medical research or preclinical research and quite a number of them were aimed to investigate the possible rationale of hyperbaric oxygen in neurological influence following stroke (Figure 1). The conclusion of these studies may be different or even contrary owing to different experimental conditions and methods. We analyze several recent experimental studies related to HBOT for stroke treatment in this paper, and most relevant studies have been reported in ischemic stroke animal model.
Figure 1.
Possible mechanisms of hyperbaric oxygen therapy (HBOT) in stroke treatment.
Note: BMSC: Bone marrow stem cell; PPARγ: peroxisome proliferator activated receptor-γ; VEGF: vascular endothelial growth factor; PKC-α: phospho-protein kinase C-alpha; TNF-α: tumor necrosis factor-alpha; MMP: matrix metalloproteinases; HIF-1α: hypoxia-inducible factor-1α; COX-2: cyclooxygenase-2; BBB: blood-brain barrier; SAH: subarachnoid hemorrhage.
Subsequently, we summarize some valuable and representative experimental results involving HBOT and stroke: (1) HBOT can decrease infarction size and reperfusion injury. Early HBOT in rats with permanent middle cerebral artery occlusion (MCAO) has neuroprotective effects, possibly via the inhibition of phospho-protein kinase C-alpha (PKC-α) and tumor necrosis factor-alpha (TNF-α). It was observed that the brain infarction area and edema decreased with the expression of TNF-α and PKC-α in the ischemic penumbra tissue down-regulated in the HBOT group which was immediately given HBOT after MCAO model successfully made (Yu et al., 2015). (2) In a mouse MCAO model, a single session of HBOT immediately applied in MCAO followed by 24 hours’ reperfusion may significantly reduce cerebral edema and brain damage via improvement of the ischemic area perfusion. In addition, the protection effect provided by HBOT was more robust than that provided by toll-like receptor 4 knockout (Dharmasaroja, 2016; Pushkov et al., 2016). However, another study of Rink et al. (2010) surprisingly showed HBOT may increase MCAO damage in rats model, different with most investigators that hold HBOT as a safe and effective option on the whole, even though controversial. (3) Hyperbaric oxygen preconditioning (HBO-PC) that means pretreating with hyperbaric oxygen has been shown to be neuroprotective via stabilizing blood-brain barrier permeability and decreasing oxidative stress in animal stroke models. Recently, HBO-PC has been widely investigated in preclinical research, for instance, Li et al. (2009) divided the experimental rats into three groups: control group with no treatment, transient MCAO group with clipping unilateral internal carotid artery for 90 minutes, HBO-PC group with four treatment sessions of HBOT at 2.5 ATA per day, once for 1 hour, for 2 days. Finally, they found the rats post HBO-PC showed infarct size reduction by triphenyltetrazolium chloride staining, decreased expression of caspase 9 and 3 as well as increased expression of Bax/Bcl-2 by western-blot assay. Besides, Soejima et al. (2013) concluded that HBO-PC can attenuate hyperglycemia-enhanced hemorrhagic transformation after ischemic stroke and reduce hemorrhagic volume and other beneficial effects: decrease infarction size and BBB disruption, improve neurological deficits, down-regulate the expression of hypoxia-inducible factor-1α (HIF-1α), and reduce the activity of matrix metalloproteinases (MMP)-2 and MMP-9. They also found HBOT might decrease post-stroke hemorrhagic transformation through increasing peroxisome proliferator activated receptor-γ (PPARγ) in hyperglycemia rats (Soejima et al., 2012, 2013; Bian et al., 2015). Additionally, HBO-PC and HBOT during ischemia was manifested to have neuroprotective effect by the suppression of the increased glutamate and hydroxyl radical level besides modulating energy metabolism in the penumbral area (Yang et al., 2010; Gao-Yu et al., 2011; Bian et al., 2015). (4) In our review (Ploughman et al., 2015), several studies indicated the post-stroke dendritic branching and synaptogenesis probably represent neuroplasticity implicated in neurological recovery. It has been illustrated that delayed HBOT which begins at 7 days after MCAO and lasts for 42 days can provide certain benefits for neurogenesis and neuroprotection including motor sensory recovery, but the promotion may be reversed by inhibition of reactive oxygen species (ROS) and HIF-1α. That is to say, if ROS and HIF-1α are inhibited experimentally prior to the treatment of HBOT, the beneficial effects of delayed HBOT will finally decrease. Thereby, it is deduced that delayed HBOT as an alternative treatment could enhance endogenous neurogenesis and improve the long-term prognosis of stroke survivors (Hu et al., 2014). (5) In an experimental study in rats related to pre-ischemic HBOT and post-ischemic aminoguanidine (AG), all the rats were equally divided into four groups (n = 7): control group, HBOT group, HBO + AG group, and AG group. The infarction rate was measured at 3 days after MCAO, the investigators found: 22.2 ± 3.1% in control group, 16.1 ± 2.7% in HBOT group, 14.4 ± 3.3% in AG group, and 15.2 ± 1.9% in HBO + AG group. As a result, they came to the conclusion that in permanent MCAO model of rats, AG and HBOT have a protective effect on the infarct rate, but no additive effect (Harman et al., 2012). (6) However, the results of an in vitro study showed that an increase of oxygen partial pressure and exposure time resulted in elevated free radical, enhanced viscosity of the whole blood and lipid peroxidation in erythrocyte, but attenuated erythrocyte deformability (Chen et al., 2011a). Another finding in ischemia/reperfusion rat models showed that HBOT enlarged the infarct ratio via blocking autophagy by ROS generation and activation of extracellular signal-regulated kinase 1/2 (Lu et al., 2014). The results shown above indicate that not all the effects of HBOT are directly beneficial and some effects are still under debate. (7) In the present study, cyclooxygenase-2 (COX-2) in cerebral tissues is indicated as a critical component of post-stoke neuroinflammation, and HBO-PC has the capability of protecting brain from global ischemia injury. In the transient global cerebral ischemic rat model, Cheng et al. (2011) showed that HBO-PC leaded to an inhibition of COX-2 expression, improved neurofunctional performance, and even decreased the incidence of seizures and mortality, while these beneficial effects of HBO-PC were weakened by COX-2 selective inhibitor pretreatment. It was concluded that HBO-PC may provide brain protection against global ischemia via the suppression of COX-2. Thereby, COX-2 probably acts as a mediator of HBO-PC within the transient ischemic brain tissue. (8) We reviewed a research referring to the early functional outcome and BBB integrity after co-administered HBOT and thrombolysis treatment using tissue-plasminogen activator (tPA) in the early phase of experimental stroke (Michalski et al., 2011b, 2012; Hafez et al., 2014). In summary, thrombolysis tended to increase BBB permeability while HBOT tended to stabilize BBB but surprisingly failed to improve the early neurofunction as hypothesis. Treatment applied both HBOT and tPA improved early functional outcome but BBB permeability was found to be increased to a certain degree than HBOT alone, potentially owing to enhanced reperfusion in the infarct area and increased BBB permeability and MMP-2 activation via tPA. In another report addressing long-term neurofunctional outcome, combined treatment of tPA and HBOT in early phase of stroke even leaded to delayed brain damage and resulted in neurological deterioration in the long-term follow-up phase (Michalski et al., 2009). As above, simultaneous treatment with hyperoxia and thrombolysis may result in unfavorable therapeutic effects out of our expectation. So further studies are warranted to identify the effect of this combined treatment at molecular level and avoid unfavorable courses of combined treatment in acute stroke. (9) In addition to decreasing infarction volume and ischemia-reperfusion injury, neuronal repair after stroke is also crucial. Investigators have demonstrated that HBOT can stimulate the expression of neurotrophic factors, promote neurogenesis and gliosis. Bone marrow stem cell (BMSC) transplantation, which is important in regenerative therapy, has been demonstrated favorable to improve the outcomes of many neuronal diseases. In cases of animal stroke, the mobilization and migration of BMSCs in brain are also found enhanced by long-course HBOT (Lee et al., 2013). These beneficial effects described above could potentially contribute to neuronal repair after stroke injury. (10) Thrombolysis potentially improves the risk of post-thrombolytic intracerebral hemorrhage by 6-flod in clinical trials related to cerebral infarction (Hacke et al., 2004). In a MCAO model treated with thrombolysis, HBOT tended to decrease the secondary hemorrhage and reduce the infarct volume if reperfusion was successful (Sun et al., 2010). (11) HOBT can enhance the efficiency of some neuroprotective drugs and provide additive neuroprotection against ischemia-induced neurodegeneration, for example, when combine HBOT and the c-Jun N-terminal kinases inhibitor XG-102, the infarct size caused by MCAO was diminished by 78%, while XG-102 and HBOT alone only 43% and 63% (Liu et al., 2010). Moreover, the combination also reduced brain edema and improved neurological outcome more robust than each alone. Nevertheless, not every combined treatment will provide additional benefit, such as combination of HBOT and second generation perfluorochemicals (Schneider et al., 2014), it does not tend to show significantly smaller necrosis than HBOT only. (12) Hemorrhagic stroke which is more fatal and complex generally involves SAH and intracerebral hemorrhage (ICH) (Pandey and Xi, 2014). Effect of HBOT in hemorrhagic stroke was also studied in animals, mainly involving the suppression of brain edema, neuroinflammation, cerebral vasospasm and the promotion of both angiogenesis and neurogenesis (Peng et al., 2014; Xiong and Yang, 2015; Yang et al., 2015; Zhou et al., 2015). The associated molecular mechanism is basically consistent with that in ischemic stroke.
CLINCAL STUDIES OF HBOT IN STROKE
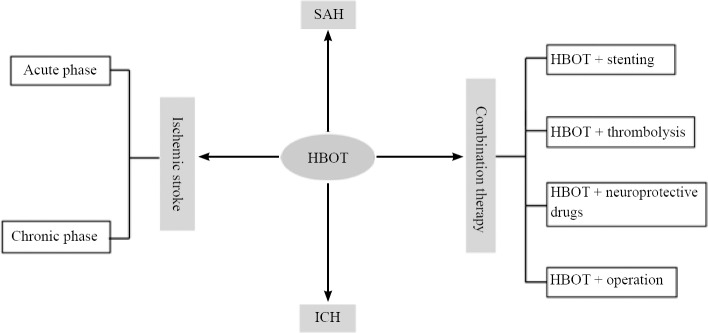
The first reported clinical application of HBOT was performed about half a century ago, shortly after the first experimental study in animal. To date, HBOT has been broadly and commonly used as an optional treatment for both ischemic and hemorrhagic stroke (Figure 2), although lack of uniform therapeutic standard, such as time window of treatment and optimal dose (oxygen pressure level). In recent years, more and more new clinical trials have provided evidence base for HBOT induced cerebral plasticity which can lead to brain function recovery and significant life quality improvement for post-stroke patient. Nevertheless, most clinical studies still lack of standard outcome measurement and negative control. To the best of our knowledge, only three well-designed randomized controlled trials have been published (Anderson et al., 1991; Nighoghossian et al., 1995; Rusyniak et al., 2003), but the discrepancy among the conclusions leaves the final efficacy in human stroke treatment still unclear.
Figure 2.
The common clinical application of hyperbaric oxygen therapy (HBOT) in stroke.
Note: SAH: Subarachnoid hemorrhage; ICH: intracerebral hemorrhage.
To better understand the current application of HBOT, several latest clinical studies are systematically summarized and analyzed, as shown below. (1) HBOT exerts therapeutic effects on cognitive recovery from stroke, even at late chronic stage. In a retrospective clinical trial conducted by Ploughman et al. (2015), they analyzed the data of 91 patients suffering memory impairments due to either hemorrhagic or ischemic stroke. All the subjects were in 3-180 months after the initial episode. The HBOT protocol administered in the participants was set at 2.0 ATA, 40-60 sessions per day, 90 minutes each, 5 days per week. Before and after the therapy, the memory function was both measured by a specific test and compared with the brain metabolic changes assessed by single-photon emission computed tomography. Finally, the results illustrate statistically significant memory improvements in almost all the patients and the improvements was in good agreement with an improvement in brain metabolic state, mainly in the temporal lobe. Recently, another retrospective analysis of chronic cognitive impairments caused by cardiac arrest has shown a similar result, reconfirmed the therapeutic effect on cognitive functions and the well correlated brain metabolic changes in relevant areas (Hadanny et al., 2015). Hence in the future, HBOT might play as a considerable effective treatment for more and more patients with post-stroke memory impairment. (2) HBOT is known capable to modulate vasoreactivity and cerebral blood flow (CBF). The response of regional CBF to HBOT in human was firstly investigated and confirmed in 2013. When HBOT at a pressure of 2.5 ATA and a perfusion tracer was used in healthy subjects observing CBF distribution, an increased regional CBF distribution mainly on the dominant hemisphere was observed in sensory-motor area, premotor, posterior cingulate and visual cortices, middle/inferior temporal gyrus, superior frontal gyrus, angular gyrus and cerebellum (Micarelli et al., 2013). The findings in this research unfold a possible underlying mechanism of HBOT related beneficial effects on the cognitive and motor improvement in stroke patients. (3) A regression statistical analysis on the basis of the Heyman 1966 HBOT study focused on treatment time window and time in chamber as well as dose of HBOT. In conclusion, only time window post stroke affects the recovery efficacy significantly and the chance of recovery is decreased over time. As a result, the most promising time window for HBOT efficacy in acute stroke is within the first 3 hours. In addition, the earlier the time window, the better the HBOT efficacy (McCormick et al., 2011). (4) Stroke induced by iatrogenic cerebral air embolism can occur in a lot of invasive therapy, such as catheter insertion and removal, laparoscopic surgery, cardiac surgery, but a potential fatal complication is uncommon. In our review, there are two articles associated to HBOT in this condition. They both retrospectively reviewed the outcome and some factors related to the response to HBOT, appraised the evidence base for the use of it in this setting. A large proportion of the subjects achieved a favorable outcome-full recovery or neurological improvement to varying degrees. The multivariate analysis further indicated HBOT within 6 hours from event increased the therapeutic effect whereas the infarct and edema shown on brain CT or MRI will reduce the benefit from HBOT. So far, HBOT is the only definitive treatment for gas embolism caused stroke with acute neurologic deficits, so timely administration of HBOT appears to be essential to the patients’ function recovery. (5) As shown above, early HBOT in acute stroke need to be applied within the time window of 3 to 6 hours, but if patients arrive too late, whether HBOT should be used? It has been suggest that delayed but repeated HBOT can also provide salvage of brain cells and promotion of neurofunction. As described in a case report, a patient with acute infarction on the corona radiate was admitted to hospital more than 5 hours after symptom onset (> 4.5 hours), so intravenous thrombolysis could not be performed. However, on the 3rd day, a daily HBOT at 2.0 ATA was preferred and continuously administered for 2 weeks. At last, prominent neurofunctional improvement was demonstrated by several clinical parameters, correlated with the regional CBF and penumbra amelioration noted in image tests (Chen et al., 2011b). (6) Post-stroke depression frequently affects the quality of life and functional recovery of the patients. Fortunately, HBOT combined with antidepressants has been declared to have a supplementary beneficial effect. In a prospective clinical trial, the combination of HBOT and fluoxetine resulted in significantly higher efficacy than HBOT or fluoxetine alone (Yan et al., 2015). Further investigation is needed to verify the effect of this combination therapy. (7) The correlation between HBOT and clinical outcome in patients with postoperative intracranial aneurysm has also been investigated. Early HBOT initiated within 1-3 days post-operation has been proved to be a valuable neuroprotective therapy, mainly via ameliorating cerebral vasospasm and ischemia (Ostrowski and Zhang, 2011; Tang et al., 2011). (8) Clinical trials concerning HBOT in ICH are scarcely reported, although they have been widely used in this field. Our experience indicates that HBOT should be applied as early as possible if the patient is in stable condition, and it may provide an additional chance for the neurological deficits caused by ICH.
ADVERSE EFFECTS OF HBOT
HBOT is considered safe and adverse effects are rarely seen in patients treated in pressures below 3.0 ATA. However, extreme hyperbaric condition or excess duration may result in oxygen toxicity, mainly including central nervous system toxicity, pulmonary injury, middle ear barotrauma, and retinopathy of prematurity (Calvert et al., 2004). Elevated pressures (5.0 ATA) can increase the risk of agitation and seizures substantially (Chavko et al., 2001). HBOT at 4.0 ATA or higher will aggravate oxidative stress in brain tissue, probably via the upregulation of lipid peroxidation and ROS and other free radicals. Thus, the guideline for HBOT recommended the maximum therapeutic pressure no greater than 3.0 ATA (Matchett et al., 2009).
CONCLUSION
Beneficial effects of HBOT in stroke have been reported in a lot of experimental and clinical trials, although assessed by different outcome measurements. In most experimental studies, strongest positive effects of HBOT were observed; but in patients with stroke injury, the effectiveness has not been well-proven due to the lack of good-quality multicenter randomized controlled trials. Nevertheless, the favorable neurological outcome so far published in our review should support the administration of HBOT in patients suffering stroke. Furthermore, in order to attain optimum efficiency, the protocol including the optimal pressure, duration for each session, the number of sessions and the time-window of starting HBOT should be specified. Therefore, more studies are needed to establish uniform standards of HBOT for each specific phase and condition.
Footnotes
Funding: This work was supported by a grant from Suzhou Key Medical Center of China, No. Szzx201501; grants from the National Natural Science Foundation of China, No. 81571115, 81422013, and 81471196; and a grant from Scientific Department of Jiangsu Province in China, No. BL2014045; Suzhou Government in China, No. LCZX201301, SZS201413, and SYS201332; and a project funded by the Priority Academic Program Development of Jiangsu Higher Education Institutions.
Conflicts of interest
The authors declare that they have no competing interests.
REFERENCES
- Anderson DC, Bottini AG, Jagiella WM, Westphal B, Ford S, Rockswold GL, Loewenson RB. A pilot study of hyperbaric oxygen in the treatment of human stroke. Stroke. 1991;22:1137–1142. doi: 10.1161/01.str.22.9.1137. [DOI] [PubMed] [Google Scholar]
- Bath PM, Lees KR. ABC of arterial and venous disease. Acute stroke. BMJ. 2000;320:920–923. doi: 10.1136/bmj.320.7239.920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bian H, Hu Q, Liang X, Chen D, Li B, Tang J, Zhang JH. Hyperbaric oxygen preconditioning attenuates hemorrhagic transformation through increasing PPARgamma in hyperglycemic MCAO rats. Exp Neurol. 2015;265:22–29. doi: 10.1016/j.expneurol.2014.12.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calvert JW, Zhou C, Zhang JH. Transient exposure of rat pups to hyperoxia at normobaric and hyperbaric pressures does not cause retinopathy of prematurity. Exp Neurol. 2004;189:150–161. doi: 10.1016/j.expneurol.2004.05.030. [DOI] [PubMed] [Google Scholar]
- Calvert JW, Cahill J, Zhang JH. Hyperbaric oxygen and cerebral physiology. Neurol Res. 2007;29:132–141. doi: 10.1179/016164107X174156. [DOI] [PubMed] [Google Scholar]
- Chavko M, Xing G, Keyser DO. Increased sensitivity to seizures in repeated exposures to hyperbaric oxygen: role of NOS activation. Brain Res. 2001;900:227–233. doi: 10.1016/s0006-8993(01)02301-0. [DOI] [PubMed] [Google Scholar]
- Chen CH, Chien MY, Liang YC, Liu DZ, Hu ML. An in vitro hyperbaric oxygen system for evaluation of free radical damage and protection by catechins on hemorheological parameters. Clin Hemorheol Microcirc. 2011a;48:211–221. doi: 10.3233/CH-2011-1412. [DOI] [PubMed] [Google Scholar]
- Chen SY, Huang E, Wang V, Fan YM, Ho CF, Yip PK. Improvement of clinical outcome and cerebral perfusion in a patient of atherosclerotic cerebral infarction after repetitive hyperbaric oxygen treatment--a case report and literature review. Undersea Hyperb Med. 2011b;38:375–379. [PubMed] [Google Scholar]
- Cheng O, Ostrowski RP, Wu B, Liu W, Chen C, Zhang JH. Cyclooxygenase-2 mediates hyperbaric oxygen preconditioning in the rat model of transient global cerebral ischemia. Stroke. 2011;42:484–490. doi: 10.1161/STROKEAHA.110.604421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dharmasaroja PA. Fluid intake related to brain edema in acute middle cerebral artery infarction. Transl Stroke Res. 2016;7:49–53. doi: 10.1007/s12975-015-0439-1. [DOI] [PubMed] [Google Scholar]
- Ding Z, Tong WC, Lu XX, Peng HP. Hyperbaric oxygen therapy in acute ischemic stroke: a review. Interv Neurol. 2014;2:201–211. doi: 10.1159/000362677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Efrati S, Ben-Jacob E. Reflections on the neurotherapeutic effects of hyperbaric oxygen. Expert Rev Neurother. 2014;14:233–236. doi: 10.1586/14737175.2014.884928. [DOI] [PubMed] [Google Scholar]
- Efrati S, Fishlev G, Bechor Y, Volkov O, Bergan J, Kliakhandler K, Kamiager I, Gal N, Friedman M, Ben-Jacob E, Golan H. Hyperbaric oxygen induces late neuroplasticity in post stroke patients--randomized, prospective trial. PLoS One. 2013;8:e53716. doi: 10.1371/journal.pone.0053716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gao-yu C, Cong-yina D, Li-jun Z, Fei L, Hua F. Effects of hyperbaric oxygen preconditioning on energy metabolism and glutamate level in the peri-infarct area following permanent MCAO. Undersea Hyperb Med. 2011;38:91–99. [PubMed] [Google Scholar]
- Gjedde A. The pathways of oxygen in brain. I. Delivery and metabolism of oxygen. Adv Exp Med Biol. 2005;566:269–275. doi: 10.1007/0-387-26206-7_36. [DOI] [PubMed] [Google Scholar]
- Grysiewicz RA, Thomas K, Pandey DK. Epidemiology of ischemic and hemorrhagic stroke: incidence, prevalence, mortality, and risk factors. Neurol Clin. 2008;26:871–895. doi: 10.1016/j.ncl.2008.07.003. vii. [DOI] [PubMed] [Google Scholar]
- Hacke W, Donnan G, Fieschi C, Kaste M, von Kummer R, Broderick JP, Brott T, Frankel M, Grotta JC, Haley EC, Jr, Kwiatkowski T, Levine SR, Lewandowski C, Lu M, Lyden P, Marler JR, Patel S, Tilley BC, Albers G, Bluhmki E, et al. Association of outcome with early stroke treatment: pooled analysis of ATLANTIS, ECASS, and NINDS rt-PA stroke trials. Lancet. 2004;363:768–774. doi: 10.1016/S0140-6736(04)15692-4. [DOI] [PubMed] [Google Scholar]
- Hadanny A, Golan H, Fishlev G, Bechor Y, Volkov O, Suzin G, Ben-Jacob E, Efrati S. Hyperbaric oxygen can induce neuroplasticity and improve cognitive functions of patients suffering from anoxic brain damage. Restor Neurol Neurosci. 2015;33:471–486. doi: 10.3233/RNN-150517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hafez S, Coucha M, Bruno A, Fagan SC, Ergul A. Hyperglycemia, acute ischemic stroke, and thrombolytic therapy. Transl Stroke Res. 2014;5:442–453. doi: 10.1007/s12975-014-0336-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harman F, Hasturk AE, Duz B, Gonul E, Korkmaz A. An evaluation of the effectiveness of pre-ischemic hyperbaric oxygen and post-ischemic aminoguanidine in experimental cerebral ischemia. Neurosciences (Riyadh) 2012;17:121–126. [PubMed] [Google Scholar]
- Helms A, Evans AW, Chu J, Sahgal A, Ostrowski R, Sosiak T, Wolf G, Gillett J, Whelan H. Hyperbaric oxygen for neurologic indications--action plan for multicenter trials in: stroke, traumatic brain injury, radiation encephalopathy & status migrainosus. Undersea Hyperb Med. 2011;38:309–319. [PubMed] [Google Scholar]
- Hu Q, Liang X, Chen D, Chen Y, Doycheva D, Tang J, Tang J, Zhang JH. Delayed hyperbaric oxygen therapy promotes neurogenesis through reactive oxygen species/hypoxia-inducible factor-1alpha/beta-catenin pathway in middle cerebral artery occlusion rats. Stroke. 2014;45:1807–1814. doi: 10.1161/STROKEAHA.114.005116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuan CY, Sun YY. Towards reperfusion-centric preclinical stroke research: outside the box of “reperfusion injury”. Neural Regen Res. 2015;10:534–536. doi: 10.4103/1673-5374.155412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee YS, Chio CC, Chang CP, Wang LC, Chiang PM, Niu KC, Tsai KJ. Long course hyperbaric oxygen stimulates neurogenesis and attenuates inflammation after ischemic stroke. Mediators Inflamm 2013. 2013:512978. doi: 10.1155/2013/512978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li JS, Zhang W, Kang ZM, Ding SJ, Liu WW, Zhang JH, Guan YT, Sun XJ. Hyperbaric oxygen preconditioning reduces ischemia-reperfusion injury by inhibition of apoptosis via mitochondrial pathway in rat brain. Neuroscience. 2009;159:1309–1315. doi: 10.1016/j.neuroscience.2009.01.011. [DOI] [PubMed] [Google Scholar]
- Liu JR, Zhao Y, Patzer A, Staak N, Boehm R, Deuschl G, Culman J, Bonny C, Herdegen T, Eschenfelder C. The c-Jun N-terminal kinase (JNK) inhibitor XG-102 enhances the neuroprotection of hyperbaric oxygen after cerebral ischaemia in adult rats. Neuropathol Appl Neurobiol. 2010;36:211–224. doi: 10.1111/j.1365-2990.2009.01047.x. [DOI] [PubMed] [Google Scholar]
- Lu Y, Kang J, Bai Y, Zhang Y, Li H, Yang X, Xiang X, Wang X, Huang Y, Su J, Chen Y, Li B, Sun L. Hyperbaric oxygen enlarges the area of brain damage in MCAO rats by blocking autophagy via ERK1/2 activation. Eur J Pharmacol. 2014;728:93–99. doi: 10.1016/j.ejphar.2014.01.066. [DOI] [PubMed] [Google Scholar]
- Matchett GA, Martin RD, Zhang JH. Hyperbaric oxygen therapy and cerebral ischemia: neuroprotective mechanisms. Neurol Res. 2009;31:114–121. doi: 10.1179/174313209X389857. [DOI] [PubMed] [Google Scholar]
- McCormick JG, Houle TT, Saltzman HA, Whaley RC, Roy RC. Treatment of acute stroke with hyperbaric oxygen: time window for efficacy. Undersea Hyperb Med. 2011;38:321–334. [PubMed] [Google Scholar]
- Micarelli A, Jacobsson H, Larsson SA, Jonsson C, Pagani M. Neurobiological insight into hyperbaric hyperoxia. Acta Physiol. 2013;209:69–76. doi: 10.1111/apha.12116. [DOI] [PubMed] [Google Scholar]
- Michalski D, Hartig W, Schneider D, Hobohm C. Use of normobaric and hyperbaric oxygen in acute focal cerebral ischemia-a preclinical and clinical review. Acta Neurol Scand. 2011a;123:85–97. doi: 10.1111/j.1600-0404.2010.01363.x. [DOI] [PubMed] [Google Scholar]
- Michalski D, Kuppers-Tiedt L, Weise C, Laignel F, Hartig W, Raviolo M, Schneider D, Hobohm C. Long-term functional and neurological outcome after simultaneous treatment with tissue-plasminogen activator and hyperbaric oxygen in early phase of embolic stroke in rats. Brain Res. 2009;1303:161–168. doi: 10.1016/j.brainres.2009.09.038. [DOI] [PubMed] [Google Scholar]
- Michalski D, Hobohm C, Weise C, Pelz J, Heindl M, Kamprad M, Kacza J, Hartig W. Interrelations between blood-brain barrier permeability and matrix metalloproteinases are differently affected by tissue plasminogen activator and hyperoxia in a rat model of embolic stroke. Med Gas Res. 2012;2:2. doi: 10.1186/2045-9912-2-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michalski D, Pelz J, Weise C, Kacza J, Boltze J, Grosche J, Kamprad M, Schneider D, Hobohm C, Hartig W. Early outcome and blood-brain barrier integrity after co-administered thrombolysis and hyperbaric oxygenation in experimental stroke. Exp Transl Stroke Med. 2011b;3:5. doi: 10.1186/2040-7378-3-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nemoto EM, Betterman K. Basic physiology of hyperbaric oxygen in brain. Neurol Res. 2007;29:116–126. doi: 10.1179/016164107X174138. [DOI] [PubMed] [Google Scholar]
- Nighoghossian N, Trouillas P, Adeleine P, Salord F. Hyperbaric oxygen in the treatment of acute ischemic stroke. A double-blind pilot study. Stroke. 1995;26:1369–1372. doi: 10.1161/01.str.26.8.1369. [DOI] [PubMed] [Google Scholar]
- Ostrowski RP, Zhang JH. Hyperbaric oxygen for cerebral vasospasm and brain injury following subarachnoid hemorrhage. Transl Stroke Res. 2011;2:316–327. doi: 10.1007/s12975-011-0069-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pandey AS, Xi G. Intracerebral hemorrhage: a multimodality approach to improving outcome. Transl Stroke Res. 2014;5:313–315. doi: 10.1007/s12975-014-0344-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peng ZR, Yang AL, Yang QD. The effect of hyperbaric oxygen on intracephalic angiogenesis in rats with intracerebral hemorrhage. J Neurol Sci. 2014;342:114–123. doi: 10.1016/j.jns.2014.04.037. [DOI] [PubMed] [Google Scholar]
- Ploughman M, Austin MW, Glynn L, Corbett D. The effects of poststroke aerobic exercise on neuroplasticity: a systematic review of animal and clinical studies. Transl Stroke Res. 2015;6:13–28. doi: 10.1007/s12975-014-0357-7. [DOI] [PubMed] [Google Scholar]
- Pushkov D, Nicholson JD, Michowiz S, Novitzky I, Weiss S, Ben Hemou M, Hochhauser E, Goldenberg-Cohen N. Relative neuroprotective effects hyperbaric oxygen treatment and TLR4 knockout in a mouse model of temporary middle cerebral artery occlusion. Int J Neurosci. 2016;126:174–181. doi: 10.3109/00207454.2014.1002609. [DOI] [PubMed] [Google Scholar]
- Rink C, Roy S, Khan M, Ananth P, Kuppusamy P, Sen CK, Khanna S. Oxygen-sensitive outcomes and gene expression in acute ischemic stroke. J Cereb Blood Flow Metab. 2010;30:1275–1287. doi: 10.1038/jcbfm.2010.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rusyniak DE, Kirk MA, May JD, Kao LW, Brizendine EJ, Welch JL, Cordell WH, Alonso RJ Hyperbaric Oxygen in Acute Ischemic Stroke Trial Pilot Study. Hyperbaric oxygen therapy in acute ischemic stroke: results of the Hyperbaric Oxygen in Acute Ischemic Stroke Trial Pilot Study. Stroke. 2003;34:571–574. doi: 10.1161/01.str.0000050644.48393.d0. [DOI] [PubMed] [Google Scholar]
- Sanchez EC. Mechanisms of action of hyperbaric oxygenation in stroke: a review. Crit Care Nurs Q. 2013;36:290–298. doi: 10.1097/CNQ.0b013e318294e9e3. [DOI] [PubMed] [Google Scholar]
- Schneider UC, Karutz T, Schilling L, Woitzik J. Administration of a second generation perfluorochemical in combination with hyperbaric oxygenation does not provide additional benefit in a model of permanent middle cerebral artery occlusion in rats. Springerplus. 2014;3:32. doi: 10.1186/2193-1801-3-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siesjo BK. Mechanisms of ischemic brain damage. Crit Care Med. 1988;16:954–963. doi: 10.1097/00003246-198810000-00006. [DOI] [PubMed] [Google Scholar]
- Singhal AB. A review of oxygen therapy in ischemic stroke. Neurol Res. 2007;29:173–183. doi: 10.1179/016164107X181815. [DOI] [PubMed] [Google Scholar]
- Soejima Y, Ostrowski RP, Manaenko A, Fujii M, Tang J, Zhang JH. Hyperbaric oxygen preconditioning attenuates hyperglycemia enhanced hemorrhagic transformation after transient MCAO in rats. Med Gas Res. 2012;2:9. doi: 10.1186/2045-9912-2-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soejima Y, Hu Q, Krafft PR, Fujii M, Tang J, Zhang JH. Hyperbaric oxygen preconditioning attenuates hyperglycemia-enhanced hemorrhagic transformation by inhibiting matrix metalloproteinases in focal cerebral ischemia in rats. Exp Neurol. 2013;247:737–743. doi: 10.1016/j.expneurol.2013.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun L, Zhou W, Mueller C, Sommer C, Heiland S, Bauer AT, Marti HH, Veltkamp R. Oxygen therapy reduces secondary hemorrhage after thrombolysis in thromboembolic cerebral ischemia. J Cereb Blood Flow Metab. 2010;30:1651–1660. doi: 10.1038/jcbfm.2010.50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang XP, Tan M, Zhang T, Peng H, Duan JW. Effects of early hyperbaric oxygen therapy on clinical outcome in postoperative patients with intracranial aneurysm. Undersea Hyperb Med. 2011;38:493–501. [PubMed] [Google Scholar]
- Toole J. Hyperbaric oxygen for stroke treatment. Med Gas Res. 2011;1:4. doi: 10.1186/2045-9912-1-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y, Chen D, Chen G. Hyperbaric oxygen therapy applied research in traumatic brain injury: from mechanisms to clinical investigation. Med Gas Res. 2014;4:18. doi: 10.1186/2045-9912-4-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiong XY, Yang QW. Rethinking the roles of inflammation in the intracerebral hemorrhage. Transl Stroke Res. 2015;6:339–341. doi: 10.1007/s12975-015-0402-1. [DOI] [PubMed] [Google Scholar]
- Yan D, Shan J, Ze Y, Xiao-yan Z, Xiao-hua H. The effects of combined hyperbaric oxygen therapy on patients with post-stroke depression. J Phys Ther Sci. 2015;27:1295–1297. doi: 10.1589/jpts.27.1295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang L, Tang J, Chen Q, Jiang B, Zhang B, Tao Y, Li L, Chen Z, Zhu G. Hyperbaric oxygen preconditioning attenuates neuroinflammation after intracerebral hemorrhage in rats by regulating microglia characteristics. Brain Res. 2015;1627:21–30. doi: 10.1016/j.brainres.2015.08.011. [DOI] [PubMed] [Google Scholar]
- Yang ZJ, Xie Y, Bosco GM, Chen C, Camporesi EM. Hyperbaric oxygenation alleviates MCAO-induced brain injury and reduces hydroxyl radical formation and glutamate release. Eur J Appl Physiol. 2010;108:513–522. doi: 10.1007/s00421-009-1229-9. [DOI] [PubMed] [Google Scholar]
- Yu M, Xue Y, Liang W, Zhang Y, Zhang Z. Protection mechanism of early hyperbaric oxygen therapy in rats with permanent cerebral ischemia. J Phys Ther Sci. 2015;27:3271–3274. doi: 10.1589/jpts.27.3271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang JH, Lo T, Mychaskiw G, Colohan A. Mechanisms of hyperbaric oxygen and neuroprotection in stroke. Pathophysiology. 2005;12:63–77. doi: 10.1016/j.pathophys.2005.01.003. [DOI] [PubMed] [Google Scholar]
- Zhao B, Shang G, Chen J, Geng X, Ye X, Xu G, Wang J, Zheng J, Li H, Akbary F, Li S, Lu J, Ling F, Ji X. A more consistent intraluminal rhesus monkey model of ischemic stroke. Neural Regen Res. 2014;9:2087–2094. doi: 10.4103/1673-5374.147936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou W, Marinescu M, Veltkamp R. Only very early oxygen therapy attenuates posthemorrhagic edema formation and blood-brain barrier disruption in murine intracerebral hemorrhage. Neurocrit Care. 2015;22:121–132. doi: 10.1007/s12028-014-0013-9. [DOI] [PubMed] [Google Scholar]
- Zhu L, He D, Han L, Cao H. Stroke research in China over the past decade: analysis of NSFC funding. Transl Stroke Res. 2015;6:253–256. doi: 10.1007/s12975-015-0404-z. [DOI] [PubMed] [Google Scholar]