Abstract
Background
Older people living in residential aged care facilities (RACFs) are at a higher risk of suffering fractures than the community-dwelling older population. The first Consensus Conference on Treatment of Osteoporosis in RACFs in Australia, held in Sydney in July 2009, aimed to address some of the issues relating to the treatment of older residents with osteoporosis in RACFs. Considering that the field of osteoporosis diagnosis and management has significantly advanced in the last 5 years and that new evidence has been generated from studies performed within RACFs, a Second Consensus Conference was held in Sydney in November 2014.
Methods
An expert panel met in November 2014 in Penrith, NSW, Australia in an attempt to reach a consensus on diverse issues related to the treatment of osteoporosis at RACFs. Participants were selected by the scientific committee on the basis of their practice in an RACF and/or major published articles. The co-chairs distributed topics randomly to all participants, who then had to propose a statement on each topic for approval by the conference after a short, evidence-based presentation, when possible.
Results
This article provides an update on the most relevant evidence on osteoporosis in older people living in RACFs graded according to its level, quality, and relevance.
Conclusion
As with the first consensus, it is hoped that this statement will constitute an important guide to aid physicians in their decision making while practicing at RACFs.
Keywords: Osteoporosis, fractures, nursing homes, falls, vitamin D
In 2012, people aged 65 years and over made up 14% of Australia’s population. This figure is projected to increase to 22% in 2061 and to 25% in 2101.1 In Australia, the number of total admissions into residential aged care facilities (RACFs) has risen steadily in recent years. This is consistent with the increase in both the places available in the aged care system and the number of older people as a proportion of the population. During the 2013–2014 financial year, 254,929 separate individuals were residing in RACFs, with a total of 137,948 admissions. The average age of residents is 83 years, with an average length of stay of just under 3 years.2 The typical profile of an institutionalized older person in Australia includes chronic diseases, multiple medications, cognitive disorders, vision and hearing impairment, poor muscle strength, a high prevalence of urinary and fecal incontinence, high risk of falls, and low bone mineral density (BMD).3–5 General practitioners (GPs) are the primary care providers in RACFs in Australia. When possible, the same GP who has been treating the resident before admission would be responsible for his/her care while at the RACFs. In the majority of cases, however, a new GP becomes involved in the resident’s care after institutionalization, which may affect continuity of care.
Once an older person enters an RACF, several changes occur in his or her care including the opportunity to maximize adherence to medications.6,7 Osteoporosis treatment is a particularly challenging area in RACFs. The majority of residents in this setting are at high risk of suffering a fracture,8 but only a minority receives treatment according to their level of risk.9–11
Methods
The first Consensus Conference on Treatment of Osteoporosis in RACFs in Australia, held in Sydney in July 2009,12 aimed to address some of the issues relating to the treatment of older residents with osteoporosis in RACFs. Considering that the field of osteoporosis diagnosis and management has significantly advanced in the last 5 years and that new evidence has been generated from studies performed within RACFs, a Second Consensus Conference was held in Sydney in November 2014. This article provides an update on the most relevant evidence on osteoporosis in older people living in RACFs graded according to their level, quality, and relevance (Table 1).13 As with our first consensus, it is hoped that this statement will constitute an important guide to aid Australian physicians in their decision making.
Table 1.
Consensus Process and Methods
| Aim: To update previous recommendations for the clinical management of osteoporosis in residential aged care facilities.12 |
| Source: The participants included experts in the field of osteoporosis, geriatric medicine, and rehabilitation (n = 5) who acted as moderators of the small groups and as speakers at the plenary sessions. In addition, geriatricians and general practitioners practicing at the residential aged care level (n = 45) from all over Australia acted as participants at the workshops and plenary sessions. |
| Methods: A search of peer-reviewed journals was conducted using MEDLINE (1966–15 November 2014). Relevant articles were identified using combinations of the subject headings “osteoporosis,” “nursing homes,” “residential care,” “long-term care,” “fractures,” “fracture prevention,” “calcium,” “vitamin D,” “bisphosphonates,” “antiresorptives,” “denosumab,” “strontium ranelate,” “teriparatide,” “hip protectors,” “falls,” and “falls prevention.” |
| Levels of evidence: Articles retrieved were graded according to their level of evidence based on the NHMRC levels of evidence: |
| Level I: A systematic review of level II studies |
| Level II: A randomized controlled trial |
| Level III-1: A pseudorandomized controlled trial (ie, alternate allocation or some other method) |
Level III-2: A comparative study with concurrent controls:
|
Level III-3: A comparative study without concurrent controls:
|
| Level IV: Case series with either posttest of pretest/posttest outcomes |
| When an NHMRC level of evidence for a clinically relevant aspect of fracture and fall prevention in the aged cared residential setting was lacking, consensus expert opinion (designated evidence V) was applied. |
| Final recommendations: Comments from all participants (experts and participants) on the draft position statement were received and considered. Final clinical recommendations were prepared by the small groups and approved at the final plenary. |
NHMRC, National Health and Medical Research Council.
Results
Risk Factors for Fractures
Eighty-five percent of all nursing home residents are reported to have osteoporosis worldwide.14 In fact, approximately 40% of all hip fractures occur in this population,15 which is associated with a disability and high mortality.16 Identification of patients at risk should therefore be actively pursued in this population.
Although the risk factors for fractures in noninstitutionalized populations are well known,15–18 the risk factors for people in RACFs remain less studied. Chen and colleagues reported the results of the Fracture Risk Epidemiology in the Frail Elderly (FREE) study.19 This prospective cohort study was designed to evaluate risk factors for falls and fractures in a population of 1894 older people (1433 women and 461 men) recruited from 52 nursing homes and 30 hostels in Northern Sydney. It was found that risk factors for individuals in RACFs differed from those for community-dwelling older people. Bringing together the results reported by Chen et al19 and other related evidence on risk assessment for osteoporosis in RACFs,8,20–22 we summarized a new risk profile for osteoporotic fractures in people in RACFs (Table 2).
Table 2.
Risk Factors for Osteoporotic Fractures (Level II)
| Low bone mass (by Dual-energy X-ray absorptiometry or ultrasound) |
| Female gender* |
| Older age* |
| Maternal history of fracture |
| History of previous fractures* |
| History of falls in the last 12 months |
| Low body weight* |
| Oral glucocorticoids at a dose of ≥5 mg prednisolone (or equivalent) for more than 3 months |
| Alcohol intake of ≥30 g/day |
| Current smoking |
| Previous hyperthyroidism |
| Diabetes mellitus |
| Vision loss |
| Psychotropic medication use |
| Postural instability* |
| Male residents* |
| Low serum vitamin D* |
| Bowel or bladder incontinence* |
| Cognitive impairment* |
| Poorer balance* |
| Ambulatory* |
Higher hazard ratio in institutionalized older persons versus community dwelling individuals.
Adapted from Chen et al.19
Assessing Fracture Risk
Two risk assessment tools are available to facilitate the identification of fracture risk in community-dwelling individuals. The FRAX and the Garvan fracture risk assessment tools have become pivotal in closing the gap in care for people with osteoporosis.23 Although these tools have been validated in predominantly community-dwelling populations, their applicability to residents of RACFs (who have a different risk profile to community populations) remains unknown. One study26 determined the prevalence of vertebral fracture among 151 nursing home residents using vertebral fracture assessment on dual-energy X-ray absorptiometry (DXA). While the prevalence of osteoporosis and vertebral fractures was high (52% and 36%, respectively) this did not significantly alter FRAX scores. Therefore, medical history, especially incorporating age and previous fractures may be the most practical way to determine fracture risk in this population.
Fracture Prevention
Despite the high risk of fracture in institutionalized older people, osteoporosis treatment rates in RACFs remain markedly low.27–29 Some of the potential causes for this treatment gap include limited access to diagnostic methods for fractures and BMD, lack of knowledge about evidence-based interventions for osteoporosis in RACFs, assumptions about length of stay and survival, and family and patients’ concerns about polypharmacy and potential side effects.8 Nevertheless, hip fractures in institutionalized older adults constitute an important cause of morbidity and mortality that could be prevented with an appropriate evidence-based approach to prevention.15
Several initiatives have been tested to improve physicians’ awareness of the importance of identifying and treating osteoporosis. A randomized trial to improve fracture prevention in nursing home residents demonstrated that audit feedback and education interventions are ineffective in improving fracture prevention.28 In this study, nursing homes (n = 67) with >or = 10 residents with a diagnosis of osteoporosis or recent hip fracture (n = 606) were randomized to receive an early or delayed intervention consisting of audit and feedback, educational modules, teleconferences, and academic detailing. Medical record abstraction and the Minimum Data Set were used to measure the prescription of osteoporosis therapies before and after the intervention period, with no significant improvements being observed in any of the quality indicators.
In contrast, new approaches to diagnosing and treating osteoporosis in nursing homes have obtained very promising results, at least by increasing the number of vitamin D supplements among nursing home residents.30 It is expected that the use of a similar structured and multidisciplinary approach, which includes pharmacological as well as nonpharmacological interventions, could be very useful in the Australian context where access to prescriptions for osteoporosis is highly regulated and based on evidence of cost effectiveness.
Fracture Prevention Interventions
Nonpharmacological
Fall prevention in nursing homes
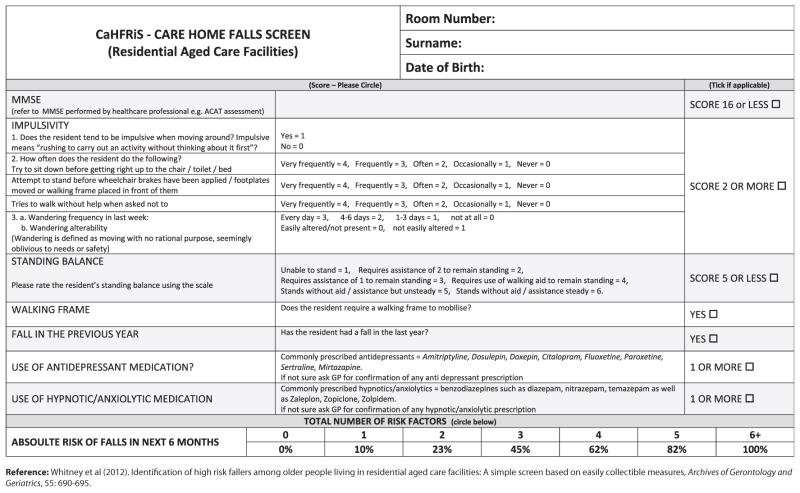
As fall risk is an important determinant factor for fractures in institutionalized older people, there is agreement that all residents of RACFs should be screened for fall risk (Table 3). Recently, Whitney et al31 evaluated a fall risk screening in the nursing home setting. The authors concluded that the tool was useful for identifying older people living in RACFs who were at increased risk of falls and provided important information about risk factors amenable to intervention. The risk of falling over a 6-month prospective period increased from 0% in those with no risk factors to 100% in those with six or more risk factors. The screening tool, presented in Figure 1, is easy to administer and contains items that are routinely collected in RACFs in Australia.
Table 3.
Recommendations for Fall and Fall Injury Preventions
|
RACFs, residential aged care facilities.
Fig. 1.
Care Home Falls Screen (CaHFRIS).
Furthermore, a pharmacist (if available) in association with the GP should perform a regular medication review to identify potential or actual medication-related problems and support appropriate prescribing. This medication review should be particularly focused on benzodiazepines, other psychotropic medications, and medicines that contribute to a high drug burden index (ie, those with anticholinergic or sedative properties).6,32–34
Other interventions to prevent falls have been multifactorial in nature and have addressed risk factors pertaining to the individual (eg, strength and balance training) as well as his or her ability to safely interact with the environment. A meta-analysis by Cameron et al35 reported that multifactorial interventions reduce falls and risk of falling in hospitals and may do so in nursing care facilities. They also reported that vitamin D supplementation significantly reduced the rate of falls (Relative attributable risk [RaR], 0.63; 95% confidence interval, 0.46 to 0.86; five trials, 4603 participants), thus confirming a recent report by Kennedy et al30 supporting the correction of vitamin D deficiency as an effective intervention to prevent falls in this setting.
Regarding the effect of exercise on fall prevention in RACFs, a recent meta-analysis36 concluded that combined frequent and long-term exercise programs (strength and balance exercises combined) are effective to prevent falls in long-term care facilities, possibly by addressing sarcopenia.37 However, no effect of exercise on fracture prevention was observed in this population.
Hip protectors
Studies of the efficacy of hip protectors to prevent hip fractures in residents of RACFs have reported conflicting results, possibly due to potential bias from cluster randomization designs and modest adherence to intervention.38–42 A multicenter, randomized controlled trial in 37 nursing homes by Kiel et al,41 which included 1042 residents, was unable to detect a protective effect on the risk of hip fracture despite good adherence to the protocol. In contrast, a Bayesian meta-analysis of four trials on the effect of hip protectors on fracture risk reported that hip protectors decrease the risk of hip fracture in elderly nursing home residents.40 More recently, Cameron et al42 tested different adherence strategies aimed at improving hip protector use in RACFs. Providing free hip protectors to older people living in nursing care facilities was necessary to increase initial acceptance and adherence. After 6 months, the achieved level of adherence was not high enough to be associated with a reduction of hip fracture. In addition, the provision of educational sessions and demonstrations to nursing staff and participants had no added value in this trial.
The most recent Cochrane Collaboration review of 19 studies and 17,000 people43 concluded that for older people living in nursing care facilities, providing a hip protector probably decreases the chance of a hip fracture marginally but may increase the small chance of a pelvic fracture slightly. When wearing hip protectors, very few people had side effects, such as skin irritation. Often, however, people did not wear them, and a better understanding is needed of the personal and design factors that may influence acceptance and adherence.
Pharmacological
Pharmacological treatment of osteoporosis has been found to be cost effective in community populations and nursing home residents aged 85 years and older based on BMD (Table 4).44,45 Nevertheless, considering the particular characteristics of this population, and the difficulties involved in performing BMD assessment in RACF residents, physicians make the ultimate decision after consultation with the patients and their families, after involving the members of the multidisciplinary team, and after assessing the harm/benefit ratio of medication interventions. The consensus conference concluded that, at the very least, residents with a history of prior low trauma fracture should be offered treatment with currently available agents (Table 4).
Table 4.
Pharmacological Prevention of Fractures in RACF Residents Versus Community-Dwelling Older Persons
| Agent | Dose | Evidence in Institutionalized Older Persons | Hip Fracture (RRR) General Population |
|---|---|---|---|
| Cholecalciferol | 800–1000 IU/day | Yes (Fx prevention) (level I) | 0.12–0.29 |
| Alendronate | 70 mg/weekly | Yes (only BMD) (level II) | 0.45–0.51 |
| Risedronate | 35 mg/weekly | No | 0.30–0.40 |
| Zoledronate | 5 mg/annually | No | 0.41 |
| Denosumab | 60 mg/6 mo | No | 0.40 (0.60 in older) |
| Teriparatide | 40 μg/day | No | 0.25 |
BMD, bone mineral density; Fx, fracture; RACF, residential aged care facility; RRR, relative risk reduction.
With the exception of those residents with limited life expectancy (<1 year) or advanced disease stage (ie, dementia), and given the proven anti-fracture efficacy for most of the current medications for osteoporosis, their low risk of drug interactions with other medications and their relatively low incidence of adverse effects, osteoporosis medications should not be considered as “inappropriate prescriptions” in RACFs.46,47 Despite strong evidence supporting the use of osteoporosis medications in RACFs, however, their utilization remains extremely low.15
Selection of the most appropriate osteoporosis medication for the patient should include consideration of the likely potential benefit (bedridden individuals would have limited potential to benefit, given the low exposure to risk), optimal dose frequency and route of administration, potential side effects and tolerance, adherence and compliance issues, cost-effectiveness, and ability to prevent fractures early.9 The present statement provides an update on the evidence on osteoporosis medications revised and discussed at the consensus conference. Although still very scarce in the current literature, relevant evidence obtained from the residential aged care setting or frail older people is provided. In addition, evidence obtained in similar populations (noninstitutionalized old-old and frail older persons) was discussed and summarized due to its relevance and potential benefit in the institutionalized population.
Calcium and vitamin D supplementation
There is evidence that vitamin D supplementation (Table 5) is beneficial for most residential aged care residents.48–50 Benefits include prevention of falls and fractures.35 Cholecalciferol (vitamin D3) should be administered at a dose of 800 IU/day or higher.49–53 This is relatively inexpensive and achieves serum 25(OH) D concentrations >50 nmol/L in most subjects, so it can be implemented without baseline or follow-up measurement of serum 25(OH) D concentrations, which can be relatively expensive. Recent studies suggest that weekly doses of vitamin D may be more effective in correcting deficiency than small regular doses, have an effect on preventing both fractures and falls, and might achieve higher compliance, which is a major limitation of this therapy.54 In addition, access to the sunshine for nursing home residents also improves vitamin D status,55,56 although it is not enough to correct serum levels of vitamin D in severely deficient residents.
Table 5.
Recommendations for Vitamin D and Calcium Supplementation
Vitamin D
|
Calcium
|
An Australian position statement on calcium and bone health57 concluded that adequate vitamin D status was essential for active calcium absorption in the gut. A total daily intake of 1300 mg calcium—optimally from dietary—needs to be achieved (up to 500 mg/d of calcium supplementation), which may have a beneficial effect on BMD. Although there is no evidence of increased cardiovascular events in nursing home residents on calcium supplementation, recent evidence suggesting that it may increase the risk of cardiovascular diseases warrants caution58 As recommended by our previous Consensus Conference, resolution of this issue (risk vs benefit) will determine the appropriateness of supplemental nondietary calcium in fracture prevention. Currently, no high dosing of vitamin D, either oral or parenteral, has been approved for falls and fracture prevention in Australia. Based on the evidence suggesting that very high doses have an effect on increasing falls and fractures in older subjects,59,60 however, use of very high doses (>500,000 IU/year or 24,000 IU/monthly) of vitamin D is not considered an alternative in the RACFs.
Antiresorptives
Bisphosphonates are the most commonly used medications for fracture prevention in the general population. However, the evidence supporting the use of bisphosphonates in institutionalized older persons is limited to just two randomized controlled studies. Greenspan et al demonstrated the utility of alendronate in improving BMD in nursing home residents.61 A more recent study by the same author tested the safety and efficacy of single-dose zoledronic acid for osteoporosis in a population of nursing home residents.62 There was no difference in terms of the incidence of fractures between the treatment and placebo groups. However, the power of the study was limited by the small sample size and by the significant differences between both groups in terms of comorbidities.
A particular limitation of oral bisphosphonates in the RACF environment is the fact that adherence could be affected by the administrative burden on both nursing staff and patients due to complex directions, difficult administration to patients with cognitive impairment, and a high prevalence of swallowing problems among residents. If oral therapy is considered, the enteric coated preparation of risedronate may be the preferred option when fasting is difficult. In this setting, intravenous bisphosphonates could become a useful alternative to oral bisphosphonates due to the lack of gastrointestinal side effects, prolonged dose intervals (1 year), and 100% adherence over 12 months at least.63–65
Denosumab is another type of antiresorptive agent, which has demonstrated a strong anti-fracture effect in several populations.66,67 Denosumab is a fully human monoclonal antibody, which is injected subcutaneously every 6 months. Although no studies have tested denosumab in RACFs, overall, the advantages of denosumab in this population include (1) convenient biannual subcutaneous administration that could improve adherence, (2) lack of gastrointestinal side effects, (3) reversibility, because it targets RANKL and is not incorporated into the bone mineral, and (4) useful for impaired renal function because of nonelimination by the kidneys. This last advantage is more evident in older persons in whom low glomerular filtration rate is a common finding. However, the risk of hypocalcemia increases in this population; therefore, appropriate serum levels of calcium and vitamin D should be ensured prior to the administration of denosumab.
Therefore, and considering the limited evidence available on the use of antiresorptives in RACFs, the consensus conference reviewed the current evidence on the effectiveness of this group of medications on fracture prevention in the closest type of populations, the old-old and the frail older population.63–67 A summary of the evidence is provided in Table 6.
Table 6.
Antiresorptives Recommendations
General Considerations
|
Primary Prevention
|
Secondary Prevention
|
Fractures Occurring on Antiresorptive Therapy
|
Side Effects of Antiresorptive Therapy
|
BMD, bone mineral density; eGFR, estimated glomerular filtration rate; FREE, Fracture Risk Epidemiology in the Frail Elderly.
The number of potential side effects associated with the use of antiresorptives is a common concern of physicians when deciding on an osteoporosis treatment.67–71 Osteonecrosis of the jaw (ONJ) and atypical fractures are the potential side effects of most concern.68 Although there are no reports on the prevalence of ONJ or atypical fractures in nursing home patients treated with antiresorptives, a recent International Consensus Conference69 concluded that the risk of ONJ associated with antiresorptive therapy for osteoporosis was low, and that routine pre-treatment dental assessment should only be performed in individuals at high risk, such as patients with cancer receiving oncology-dose parenteral antiresorptive therapy of bisphosphonates and denosumab, which is not yet a common occurrence in nursing home residents. In terms of atypical fractures, these events follow longer-term use of antiresorptives. As with ONJ, a recent consensus70 has concluded that the absolute risk of atypical fractures in patients on bisphosphonates is low, ranging from 3.2 to 50 cases per 100,000 person-years. Nevertheless, this side effect could be observed in nursing home residents who have been on antiresorptives for long periods of time; therefore, prodromal symptoms (ie, thigh pain) should be actively explored in these patients.
Other treatments
Strontium ranelate (Table 7)
Table 7.
Other Treatments
|
A systematic review by Inderjeeth et al63 on the safety and efficacy of pharmacological agents in managing osteoporosis in people 85 years and older concluded that there is good evidence for the benefit of current treatments in reducing vertebral fractures, but that data are limited for nonvertebral and hip fracture reduction. However, the use of strontium ranelate in clinical practice has been affected by recent evidence reporting a higher incidence of cardiovascular events in post-menopausal women receiving treatment for osteoporosis with this compound71; therefore, its use in RACFs is not recommended.
Teriparatide is an anabolic medication that is administered subcutaneously on a daily basis. No studies have assessed the effect of teriparatide in RACFs. Although compliance with this medication should not be an issue in RACFs, major limitations to using this medication in RACFs include the Australian Pharmaceutical Benefits Scheme requirements and the high cost of the medication. Indications to use teriparatide in RACFs include several possible scenarios: (1) patients with severe osteoporosis with use of bisphosphonates for a number of years with recurrent fracture and (2) in cases where an osteoporotic fracture has failed to unite after surgical treatment. In general, although highly effective in hip fracture prevention,72 teriparatide should not be considered as a first-line treatment for fracture prevention, and even less so in the RACF population.73
Conclusion
Prevention of falls and fractures in older persons living in RACFs should include risk identification, fracture/BMD documentation, nonpharmacological and pharmacological interventions, staff education, and involve residents and their families, where appropriate. In addition, research in the field of fall and fracture prevention in RACFs, including major clinical trials, should be encouraged. Our recommendations closely correspond with those recently published in Canada.74 Although there are substantial differences between the Canadian and the Australian RACFs, we all agree that only by increasing awareness on the consequences of osteoporotic fractures in this population, we will generate an important change in practice with a major impact on quality of life in this high-risk population.
Acknowledgments
The Consensus Conference was funded with an unrestricted educational grant from Amgen Australia and a grant from the Nepean Medical Research Foundation.
Dr. Gustavo Duque received honoraria, as an advisory board member, from Amgen and Eli Lilly. His employing institution received grants from Novartis, Amgen, and Lilly. He received honoraria from Amgen, Lilly and Novartis.
Dr. Alexandra Papaioannou received a travel grant and honorarium from Amgen.
References
- 1.Australian Bureau of Statistics. [Accessed February 20, 2016];3222.0-Population Projections, Australia, 2012 (base) to 2101. Available at: http://www.abs.gov.au/ausstats/abs@.nsf/Lookup/3222.0main+features32012%20(base)%20to%202101.
- 2.Australian Institute of Health and Welfare. [Accessed February 20, 2016];Admissions into aged care. Available at: http://www.aihw.gov.au/aged-care/residential-and-home-care-2013-14/admissions/
- 3.Broad JB, Ashton T, Gott M, et al. Likelihood of residential aged care use in later life: A simple approach to estimation with international comparison. Aust N Z J Public Health. 2015;39:374–379. doi: 10.1111/1753-6405.12374. [DOI] [PubMed] [Google Scholar]
- 4.Russell M, Clapperton A, Vu T, et al. Trends in fall-related hospitalisations in older people living in aged care facilities. Osteoporos Int. 2015;26:1219–1224. doi: 10.1007/s00198-014-2946-4. [DOI] [PubMed] [Google Scholar]
- 5.Australian Institute of Health and Welfare. [Accessed February 22, 2016];Use of aged care services before death. Available at: http://www.aihw.gov.au/publication-detail/?id=60129550413.
- 6.Advinha AM, de Oliveira-Martins S, Mateus V, et al. Medication regimen complexity in institutionalized elderly people in an aging society. Int J Clin Pharm. 2014;36:750–756. doi: 10.1007/s11096-014-9963-4. [DOI] [PubMed] [Google Scholar]
- 7.Cestac P, Tavassoli N, Vellas B, et al. Improving medication use in the nursing homes: A European perspective. J Am Med Dir Assoc. 2013;14:6–9. doi: 10.1016/j.jamda.2012.09.013. [DOI] [PubMed] [Google Scholar]
- 8.Aguilar EA, Barry SD, Cefalu CA, et al. Osteoporosis diagnosis and management in long-term care facility. Am J Med Sci. 2015;350:357–363. doi: 10.1097/MAJ.0000000000000562. [DOI] [PubMed] [Google Scholar]
- 9.Jachna C, Shireman T, Whittle J, et al. Differing patterns of antiresorptive pharmacotherapy among nursing facility residents and community dwellers. J Am Geriatr Soc. 2005;53:1275–1281. doi: 10.1111/j.1532-5415.2005.53401.x. [DOI] [PubMed] [Google Scholar]
- 10.Kamel H. Underutilization of calcium and vitamin D supplements in an academic long-term care facility. J Am Med Dir Assoc. 2004;5:98–100. doi: 10.1097/01.JAM.0000110649.22467.B4. [DOI] [PubMed] [Google Scholar]
- 11.Kennedy CC, Ioannidis G, Thabane L, et al. Osteoporosis prescribing in long-term care: Impact of a provincial knowledge translation strategy. Can J Aging. 2015;34:137–148. doi: 10.1017/S0714980815000057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Duque G, Close JJ, de Jager JP, et al. Treatment for osteoporosis in Australian residential aged care facilities: Consensus recommendations for fracture prevention. Med J Aust. 2010;193:173–179. doi: 10.5694/j.1326-5377.2010.tb03839.x. [DOI] [PubMed] [Google Scholar]
- 13.National Health and Medical Research Council. [Accessed February 22, 2016];A guide to the development, implementation and evaluation of clinical practice guidelines. Available at: http://www.nhmrc.gov.au/_files_nhmrc/file/publications/synopses/cp30.pdf.
- 14.International Osteoporosis Foundation. [Accessed February 22, 2016];Facts and statistics. Available at: http://www.iofbonehealth.org/facts-statistics.
- 15.Zarowitz BJ, Cheng LI, Allen C, et al. Osteoporosis prevalence and characteristics of treated and untreated nursing home residents with osteoporosis. J Am Med Dir Assoc. 2015;16:341–348. doi: 10.1016/j.jamda.2015.01.073. [DOI] [PubMed] [Google Scholar]
- 16.Neuman MD, Silber JH, Magaziner JS, et al. Survival and functional outcomes after hip fracture among nursing home residents. JAMA Intern Med. 2014;174:1273–1280. doi: 10.1001/jamainternmed.2014.2362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cumming RG. Nursing home residence and risk of hip fracture. Am J Epidemiol. 1996;143:1191–1194. doi: 10.1093/oxfordjournals.aje.a008706. [DOI] [PubMed] [Google Scholar]
- 18.Norton R, Campbell AJ, Reid IR, et al. Residential status and risk of hip fracture. Age Ageing. 1999;28:135–139. doi: 10.1093/ageing/28.2.135. [DOI] [PubMed] [Google Scholar]
- 19.Chen JS, Simpson JM, March LM, et al. Fracture risk assessment in frail older people using clinical risk factors. Age Ageing. 2008;37:536–541. doi: 10.1093/ageing/afn128. [DOI] [PubMed] [Google Scholar]
- 20.Spector W, Shaffer T, Potter DE, et al. Risk factors associated with the occurrence of fractures in U.S. nursing homes: Resident and facility characteristics and prescription medications. J Am Geriatr Soc. 2007;55:327–333. doi: 10.1111/j.1532-5415.2007.01081.x. [DOI] [PubMed] [Google Scholar]
- 21.Girman CJ, Chandler JM, Zimmerman SI, et al. Prediction of fracture in nursing home residents. J Am Geriatr Soc. 2002;50:1341–1347. doi: 10.1046/j.1532-5415.2002.50354.x. [DOI] [PubMed] [Google Scholar]
- 22.Chandler JM, Zimmerman SI, Girman CJ, et al. Low bone mineral density and risk of fracture in white female nursing home residents. JAMA. 2000;284:972–977. doi: 10.1001/jama.284.8.972. [DOI] [PubMed] [Google Scholar]
- 23.Leslie WD, Lix LM. Comparison between various fracture risk assessment tools. Osteoporos Int. 2014;25:1–21. doi: 10.1007/s00198-013-2409-3. [DOI] [PubMed] [Google Scholar]
- 24.Best Practice Guidelines for Australian Residential Aged Care Facilities. [Accessed March 16, 2016];Preventing Falls and Harm From Falls in Older People. 2009 Available at: http://www.safetyandquality.gov.au/wp-content/uploads/2012/01/Guidelines-RACF.pdf.
- 25.Kouladjian L, Gnjidic D, Chen TF, et al. Drug burden index in older adults: Theoretical and practical issues. Clin Interv Aging. 2014;9:1503–1515. doi: 10.2147/CIA.S66660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rodondi A, Chevalley T, Rizzoli R. Prevalence of vertebral fracture in oldest old nursing home residents. Osteoporos Int. 2012;23:2601–2606. doi: 10.1007/s00198-012-1900-6. [DOI] [PubMed] [Google Scholar]
- 27.Curtis JR, Arora T, Xi J, et al. Do physicians within the same practice setting manage osteoporosis patients similarly? Implications for implementation research. Osteoporos Int. 2009;20:1921–1927. doi: 10.1007/s00198-009-0900-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Colón-Emeric CS, Lyles KW, House P, et al. Randomized trial to improve fracture prevention in nursing home residents. Am J Med. 2007;120:886–892. doi: 10.1016/j.amjmed.2007.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wright RM. Use of osteoporosis medications in older nursing facility residents. J Am Med Dir Assoc. 2007;8:453–457. doi: 10.1016/j.jamda.2007.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kennedy CC, Ioannidis G, Thabane L, et al. Successful knowledge translation intervention in long-term care: Final results from the vitamin D and osteoporosis study (ViDOS) pilot cluster randomized controlled trial. Trials. 2015;16:214. doi: 10.1186/s13063-015-0720-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Whitney J, Close JCT, Lord SR, et al. Identification of high risk fallers among older people living in residential care facilities: A simple screen based on easily collectable measures. Arch Gerontol Geriatr. 2012;55:690–695. doi: 10.1016/j.archger.2012.05.010. [DOI] [PubMed] [Google Scholar]
- 32.Gheewala PA, Peterson GM, Curtain CM, et al. Impact of the pharmacist medication review services on drug-related problems and potentially inappropriate prescribing of renally cleared medications in residents of aged care facilities. Drugs Aging. 2014;31:825–835. doi: 10.1007/s40266-014-0208-y. [DOI] [PubMed] [Google Scholar]
- 33.Wallerstedt SM, Kindblom JM, Nylén K, et al. Medication reviews for nursing home residents to reduce mortality and hospitalization: Systematic review and meta-analysis. Br J Clin Pharmacol. 2014;78:488–497. doi: 10.1111/bcp.12351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wilson NM, Hilmer SN, March LM, et al. Associations between Drug burden index and falls in older people in residential aged care. J Am Geriatr Soc. 2011;59:875–880. doi: 10.1111/j.1532-5415.2011.03386.x. [DOI] [PubMed] [Google Scholar]
- 35.Cameron ID, Gillespie LD, Robertson MC, et al. Interventions for preventing falls in older people in care facilities and hospitals. Cochrane Database Syst Rev. 2012;12:CD005465. doi: 10.1002/14651858.CD005465.pub3. [DOI] [PubMed] [Google Scholar]
- 36.Silva RB, Eslick GD, Duque G. Exercise for falls and fracture prevention in long term care facilities: A systematic review and meta-analysis. J Am Med Dir Assoc. 2013;14:685–689. doi: 10.1016/j.jamda.2013.05.015. [DOI] [PubMed] [Google Scholar]
- 37.Hassan BH, Hewitt J, Keogh JW, et al. Impact of resistance training on sarcopenia in nursing care facilities: A pilot study. Geriatr Nurs. 2016;37:116–121. doi: 10.1016/j.gerinurse.2015.11.001. [DOI] [PubMed] [Google Scholar]
- 38.Zimmerman S, Magaziner J, Birge SJ, et al. Adherence to hip protectors and implications for U.S. Long-term care settings. J Am Med Dir Assoc. 2010;11:106–115. doi: 10.1016/j.jamda.2009.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sawka AM, Boulos P, Beattie K, et al. Hip protectors decrease hip fracture risk in elderly nursing home residents: A Bayesian meta-analysis. J Clin Epidemiol. 2007;60:336–344. doi: 10.1016/j.jclinepi.2006.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sawka AM, Boulos P, Beattie K, et al. Do hip protectors decrease the risk of hip fracture in institutional and community-dwelling elderly? A systematic review and meta-analysis of randomized controlled trials. Osteoporos Int. 2005;16:1461–1474. doi: 10.1007/s00198-005-1932-2. [DOI] [PubMed] [Google Scholar]
- 41.Kiel DP, Magaziner J, Zimmerman S, et al. Efficacy of a hip protector to prevent hip fracture in nursing home residents: The HIP PRO randomized controlled trial. JAMA. 2007;298:413–422. doi: 10.1001/jama.298.4.413. [DOI] [PubMed] [Google Scholar]
- 42.Cameron ID, Kurrle SE, Quine S, et al. Improving adherence with the use of hip protectors among older people living in nursing care facilities: A cluster randomized trial. J Am Med Dir Assoc. 2011;12:50–57. doi: 10.1016/j.jamda.2010.02.010. [DOI] [PubMed] [Google Scholar]
- 43.Santesso N, Carrasco-Labra A, Brignardello-Petersen R. Hip protectors for preventing hip fractures in older people. Cochrane Database Syst Rev. 2014;(3):CD001255. doi: 10.1002/14651858.CD001255.pub5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Schousboe JT, Taylor BC, Fink HA, et al. Cost-effectiveness of bone densitometry followed by treatment of osteoporosis in older men. JAMA. 2007;298:629–637. doi: 10.1001/jama.298.6.629. [DOI] [PubMed] [Google Scholar]
- 45.Schousboe JT, Ensrud KE, Nyman JA, et al. Universal bone densitometry screening combined with alendronate therapy for those diagnosed with osteoporosis is highly cost-effective for elderly women. J Am Geriatr Soc. 2005;53:1697–1704. doi: 10.1111/j.1532-5415.2005.53504.x. [DOI] [PubMed] [Google Scholar]
- 46.García-Gollarte F, Baleriola-Júlvez J, Ferrero-López I, et al. Inappropriate drug prescription at nursing home admission. J Am Med Dir Assoc. 2012;13:83.e9–83.e15. doi: 10.1016/j.jamda.2011.02.009. [DOI] [PubMed] [Google Scholar]
- 47.García-Gollarte F, Baleriola-Júlvez J, Ferrero-López I, et al. An educational intervention on drug use in nursing homes improves health outcomes resource utilization and reduces inappropriate drug prescription. J Am Med Dir Assoc. 2014;15:885–891. doi: 10.1016/j.jamda.2014.04.010. [DOI] [PubMed] [Google Scholar]
- 48.Rolland Y, de Souto Barreto P, Abellan Van Kan G, et al. Vitamin D supplementation in older adults: Searching for specific guidelines in nursing homes. J Nutr Health Aging. 2013;17:402–412. doi: 10.1007/s12603-013-0007-x. [DOI] [PubMed] [Google Scholar]
- 49.Demontiero O, Herrmann M, Duque G. Supplementation with vitamin D and calcium in long-term care residents. J Am Med Dir Assoc. 2011;12:190–194. doi: 10.1016/j.jamda.2010.09.013. [DOI] [PubMed] [Google Scholar]
- 50.Avenell A, Mak JC, O’Connell D. Vitamin D and vitamin D analogues for preventing fractures in post-menopausal women and older men. Cochrane Database Syst Rev. 2014;(4):CD000227. doi: 10.1002/14651858.CD000227.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Przybelski R, Agrawal S, Krueger D, et al. Rapid correction of low vitamin D status in nursing home residents. Osteoporos Int. 2008;19:1621–1628. doi: 10.1007/s00198-008-0619-x. [DOI] [PubMed] [Google Scholar]
- 52.Abizanda P, López MD, García VP, et al. Effects of an oral nutritional supplementation plus physical exercise intervention on the physical function, nutritional status, and quality of life in frail institutionalized older adults: The ACTIVNES Study. J Am Med Dir Assoc. 2015;16:439.e9–439.e16. doi: 10.1016/j.jamda.2015.02.005. [DOI] [PubMed] [Google Scholar]
- 53.Veleva BI, Chel VG, Achterberg WP. Efficacy of daily 800 IU vitamin D supplementation in reaching vitamin D sufficiency in nursing home residents: Cross-sectional patient file study. BMC Geriatr. 2014;14:103. doi: 10.1186/1471-2318-14-103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Buckinx F, Reginster JY, Cavalier E, et al. Determinants of vitamin D supplementation prescription in nursing homes: A survey among general practitioners. Osteoporos Int. 2016;27:881–886. doi: 10.1007/s00198-015-3469-3. [DOI] [PubMed] [Google Scholar]
- 55.Reid IR, Gallagher DJ, Bosworth J. Prophylaxis against vitamin D deficiency in the elderly by regular sunlight exposure. Age Ageing. 1986;15:35–40. doi: 10.1093/ageing/15.1.35. [DOI] [PubMed] [Google Scholar]
- 56.Chel VG, Ooms ME, Pavel S, et al. Prevention and treatment of vitamin D deficiency in Dutch psychogeriatric nursing home residents by weekly half-body UVB exposure after showering: A pilot study. Age Ageing. 2011;40:211–214. doi: 10.1093/ageing/afq159. [DOI] [PubMed] [Google Scholar]
- 57.Sanders KM, Nowson CA, Kotowicz MA, et al. Calcium and bone health: Position statement for the Australian and New Zealand Bone and Mineral Society, Osteoporosis Australia and the Endocrine Society of Australia. Med J Aust. 2009;190:316–320. doi: 10.5694/j.1326-5377.2009.tb02421.x. [DOI] [PubMed] [Google Scholar]
- 58.Reid IR, Bristow SM, Bolland MJ. Cardiovascular complications of calcium supplements. J Cell Biochem. 2015;116:494–501. doi: 10.1002/jcb.25028. [DOI] [PubMed] [Google Scholar]
- 59.Bischoff-Ferrari HA, Dawson-Hughes B, Orav EJ, et al. Monthly high-dose vitamin D treatment for the prevention of functional decline: A randomized clinical trial. JAMA Intern Med. 2016;176:175–183. doi: 10.1001/jamainternmed.2015.7148. [DOI] [PubMed] [Google Scholar]
- 60.Sanders KM, Stuart AL, Williamson EJ, et al. Annual high-dose oral vitamin D and falls and fractures in older women: A randomized controlled trial. JAMA. 2010;303:1815–1822. doi: 10.1001/jama.2010.594. [DOI] [PubMed] [Google Scholar]
- 61.Greenspan SL, Schneider DL, McClung MR, et al. Alendronate improves bone mineral density in elderly women with osteoporosis residing in long-term care facilities. A randomized, double-blind, placebo-controlled trial. Ann Intern Med. 2002;136:742–746. doi: 10.7326/0003-4819-136-10-200205210-00009. [DOI] [PubMed] [Google Scholar]
- 62.Greenspan SL, Perera S, Ferchak MA, et al. Efficacy and safety of single-dose zoledronic acid for osteoporosis in frail elderly women: A randomized clinical trial. JAMA Intern Med. 2015;175:913–921. doi: 10.1001/jamainternmed.2015.0747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Inderjeeth CA, Foo AC, Lai MM, et al. Efficacy and safety of pharmacological agents in managing osteoporosis in the old old: Review of the evidence. Bone. 2009;44:744–751. doi: 10.1016/j.bone.2008.12.003. [DOI] [PubMed] [Google Scholar]
- 64.Kamel HK. Update on osteoporosis management in long-term care: Focus on bisphosphonates. J Am Med Dir Assoc. 2007;8:434–440. doi: 10.1016/j.jamda.2007.06.005. [DOI] [PubMed] [Google Scholar]
- 65.Lewiecki EM. A clinician’s perspective on the use of zoledronic acid in the treatment of postmenopausal osteoporosis. J Clin Densitom. 2008;11:478–484. doi: 10.1016/j.jocd.2008.07.003. [DOI] [PubMed] [Google Scholar]
- 66.McClung MR, Boonen S, Törring O, et al. Effect of denosumab treatment on the risk of fractures in subgroups of women with postmenopausal osteoporosis. J Bone Miner Res. 2012;27:211–218. doi: 10.1002/jbmr.536. [DOI] [PubMed] [Google Scholar]
- 67.McHorney CA, Schousboe JT, Cline RR, et al. The impact of osteoporosis medication beliefs and side-effect experiences on non-adherence to oral bisphosphonates. Curr Med Res Opin. 2007;23:3137–3152. doi: 10.1185/030079907X242890. [DOI] [PubMed] [Google Scholar]
- 68.Reid IR. Short-term and long-term effects of osteoporosis therapies. Nat Rev Endocrinol. 2015;11:418–428. doi: 10.1038/nrendo.2015.71. [DOI] [PubMed] [Google Scholar]
- 69.Khan AA, Morrison A, Hanley DA, et al. Diagnosis and management of osteonecrosis of the jaw: A systematic review and international consensus. J Bone Miner Res. 2015;30:3–23. doi: 10.1002/jbmr.2405. [DOI] [PubMed] [Google Scholar]
- 70.Shane E, Burr D, Abrahamsen B, et al. Atypical subtrochanteric and diaphyseal femoral fractures: Second report of a task force of the American Society for Bone and Mineral Research. J Bone Miner Res. 2014;29:1–23. doi: 10.1002/jbmr.1998. [DOI] [PubMed] [Google Scholar]
- 71.Yu J, Tang J, Li Z, et al. History of cardiovascular events and cardiovascular risk factors among patients initiating strontium ranelate for treatment of osteoporosis. Int J Womens Health. 2015;7:913–918. doi: 10.2147/IJWH.S88627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Collinge C, Favela J. Use of teriparatide in osteoporotic fracture patients. Injury. 2016;47:S36–S38. doi: 10.1016/S0020-1383(16)30009-2. [DOI] [PubMed] [Google Scholar]
- 73.Inderjeeth CA, Chan K, Glendenning P. Teriparatide: Its Use in the Treatment of Osteoporosis. Clin Med Insights Ther. 2011;3:67–80. [Google Scholar]
- 74.Papaioannou A, Santesso N, Morin SN, et al. Recommendations for preventing fracture in long-term care. CMAJ. 2015;187:1135–1144. E450–61. doi: 10.1503/cmaj.141331. [DOI] [PMC free article] [PubMed] [Google Scholar]