Abstract
Introduction:
In recent years, bioresorbable plates have undergone remarkable development. However, there has been no attendant improvement in their strength, because strength requires thickness, and complications such as palpability are related to the thickness of bioresorbable plate systems. In this clinical study, we compared the surgical management of zygomatic fractures using newly developed thinner bioresorbable materials or conventional titanium miniplates.
Methods:
Twelve patients with zygomatic fractures were randomly divided equally into 2 groups (6 with new bioresorbable osteosynthesis materials and 6 with standard titanium miniplates). Using computed tomography, we evaluated the thickness of the soft tissue and plate at the zygomaticofrontal sutures in each patient with the help of detailed radiographic computed tomography data at 6 months postoperatively. We compared the amount of soft-tissue volume increase between the uninjured healthy and injured operated sides in each patient.
Results:
Both groups eventually achieved satisfactory healing, with a favorable restoration of form and function and without any complications, including palpability. The amount of soft-tissue volume increase at the operated side relative to the uninjured healthy side using new thin bioresorbable plates was 131.1% (range: 101.5–165.8). On the other hand, that of titanium miniplates was 126.4% (range: 102.2–167.6). There was no statistically significant difference (P > 0.05).
Conclusion:
This newly developed thinner flat-type bioresorbable plate system could be considered clinically useful in the treatment of zygomatic fractures even in easily palpated areas, such as the infraorbital rim or zygomaticofrontal sutures, without any healing differences in skeleton as compared with conventional titanium miniplates.
Keywords: Bioresorbable plate, flat-type osteosynthesis device, zygomatic fracture
The application of bioresorbable materials has gained acceptance in the management of patients with maxillofacial trauma, particularly those with midfacial fractures. These materials combine the benefits of rigid internal fixation with the amenities of biodegradation, precluding the need for their removal and reducing their interference with craniofacial growth in children.1,2 Therefore, these materials are safe, effective, and sufficiently flexible for use at many craniofacial sites.3 Their common constituents are polyhydroxyl acids: polymers and copolymers of poly-l-lactic acid (PLLA), poly-d-lactic acid, polyglycolic acid, and polydioxanone sulfate.4–7 Developed bioresorbable osteosynthesis materials comprise a composite of PLLA as a base, an osteoconductive material such as hydroxyapatite,8 and an accelerator of bioresorption such as polyglycolic acid.9 However, despite the remarkable advances in bioresorbable osteosynthesis systems, there have been no significant improvements in their strength compared with that of titanium plate systems; sufficient thickness is still required to maintain strength, and complications such as palpability are related to the thickness of bioresorbable plate systems.10–13 Although the bioresorbable plate system degraded eventually, it takes several years to complete absorption.14,15 Therefore, the influence due to the thickness of the osteosynthesis plate is very important.
GRAND FIX (Gunze, Kyoto, Japan) is a conventional, bioresorbable bone fixation device made from pure PLLA that is gradually hydrolyzed and absorbed into the human body. This conventional plate system was further modified to develop a new system made commercially available as a thinner, flat, bioresorbable plate system. This thin, flat plate is stiff, has a similar mechanical strength to that of conservative PLLA plates by giving width, and is suitable for use in the treatment of maxillofacial fractures.
In this clinical study, we compared the surgical management of zygomatic fractures using this new thin bioresorbable plate system or conventional titanium miniplates.
MATERIALS AND METHODS
Patients
In this clinical study, we compared the performance of a bioresorbable osteosynthesis material (GRAND FIX) with that of a standard titanium miniplate (MatrixMIDFACE Plates; Synthes, Oberdorf, Switzerland) for the internal fixation of zygomatic fractures. Twelve systemically healthy patients with zygomatic bone fractures who required open reduction and internal fixation, treated between 2012 and 2014 at the Division of Oral and Maxillofacial Surgery, Kagawa Prefectural Central Hospital, Takamatsu, Kagawa, Japan, and who agreed to attend this clinical study were divided randomly into 2 treatment groups (6 in the bioresorbable osteosynthesis materials group and the other 6 in the standard titanium miniplates group).
All the surgical procedures were carried out by 2 expert surgeons, the first and the second authors, who are well experienced in handling both bioresorbable and titanium miniplate fixation systems based at Kagawa Prefectural Central Hospital, Kagawa, Japan. This study was approved by the Ethics Committee of Kagawa Prefectural Central Hospital (approval number: 403). All patients provided written informed consent to participate.
Methods
Bioresorbable Material
The newly developed thin flat-type bioresorbable plate system GRAND FIX is composed of a monopolymer of PLLA (Fig. 1). Its molecular weight and crystallinity are, respectively, 2.0 to 2.5 × 105 and about 50%. The bending strength of this plate is 175 to 215 MPa, and the cortical bone has the equivalent of the value (ie, 200 MPa).16 Decomposition of PLLA occurs gradually, causing small cracks to appear. In vivo, pure PLLA is absorbed and lost in about 3 years to a few years.15,17 We used a plate 0.95 mm thick and 5.5 mm wide with screws 2.2 mm in diameter and 5 or 7 mm long. Flexible templates, torque-limiting screwdrivers, a heat bender system, custom-made self-drilling taps, and a special torque driver were used to shape and fit the plate. After the reduction of the fracture, a template was adapted to the contours of the bone. Next, the bioresorbable plate was held in contact with the template in the heat bender system and heated above its glass transition temperature (approximately 65°C) until it adopted the shape of the template.
FIGURE 1.

The new design of the GRAND FIX (Gunze) osteosynthesis device composed of poly-l-lactide. It is available as thin and flat-type bioresorbable plate systems.
Titanium Plates
The titanium miniplate system used was MatrixMIDFACE. We used plates 0.5 mm thick with screws 1.55 mm in diameter and 4 mm long at the frontozygomatic fracture site. For other midfacial fractures, we used plates 0.7 or 0.8 mm thick with screws 1.55 mm in diameter and 4 or 5 mm long.
Surgical Procedure
We performed the standard surgical procedures according to Arbeitsgemeinschaft für Osteosynthesefragen principles. Zygomatic fractures were stabilized using 2- or 3-point fixation (Figs. 2-3). Three-point fixation at the infraorbital rim was used if the orbit required exploration or reconstruction, or if doing so helped to stabilize the fracture for 2-point fixation. In patients undergoing 2-point fixation, the frontozygomatic sutures were approached via a lateral eyebrow incision. The zygomaticomaxillary buttress was exposed using an intraoral buccal sulcus incision. In patients undergoing 3-point fixation, additional exposure of the infraorbital rim was accomplished via the transconjunctival approach. For 2-point fixation, patients underwent fixation at the frontozygomatic suture and in the zygomaticomaxillary buttress region, whereas for 3-point fixation, patients underwent fixation at the frontozygomatic suture, infraorbital margin, and zygomaticomaxillary buttress region. We were able to adjust the shape of the GRAND FIX bioresorbable plates by bending or twisting them to match a contoured template using a heat bender. Finally, we fixed the plate to the bone with screws using the following 3 procedures. First, we drilled a guide hole with a custom-made drill bit to a depth of approximately 1 mm, shallower than the total length of the screw. Second, we tapped the screw hole carefully with a custom-made tap, and washed out any bone chips present in the foramen. Third, we carefully inserted a screw using a special torque driver to fasten the plate to the bone. In contrast, when fitting titanium miniplates, we inserted a screw using a torque driver after bending and drilling the plate to the bone. Regarding postoperative management, about 1 month after surgery, we instructed the patients to follow a soft diet until the occlusal pain improved. In patients with mandible fracture, although we did not use intermaxillary fixation, guiding elastics were used to guide occlusion in mandibular fracture where appropriate. As a postoperative step to prevent infection, the patient was administered a first-generation cephalosporin antibiotic every 12 hours for 3 days.
FIGURE 2.
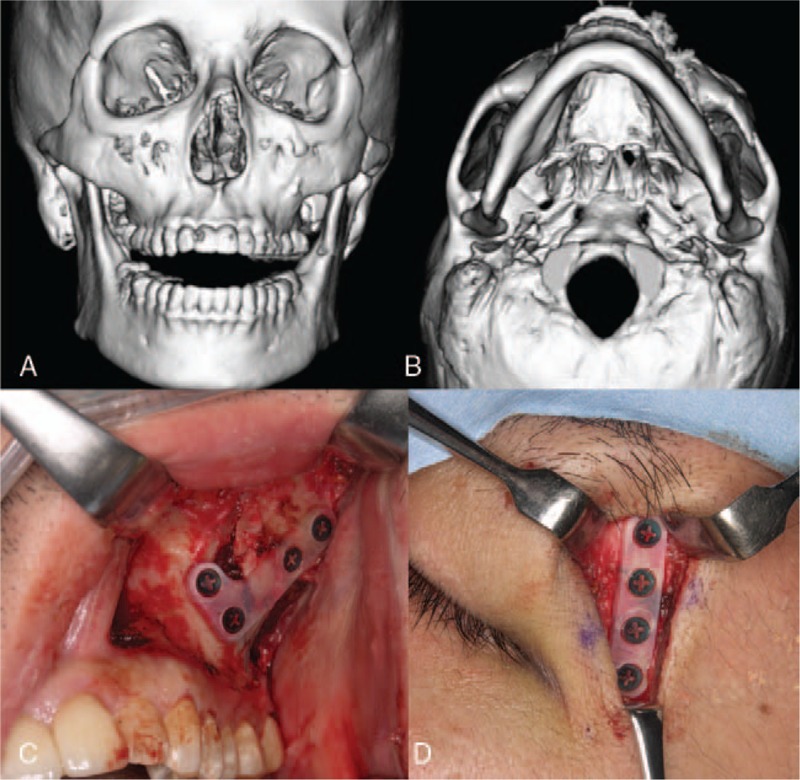
The 2-point fixation technique for the treatment of zygomatic fractures (bioresorbable osteosynthesis materials group (patient 1): (A and B) frontal and axial views of 3-dimensional computed tomography image showing inferior dislocation of the zygomatic body due to zygomatic fracture; (C) placement of a plate across the frontozygomatic fracture area via a lateral eyebrow incision; (D) placement of a plate across the fracture of the zygomaticomaxillary buttress through the maxillary vestibular approach.
FIGURE 3.
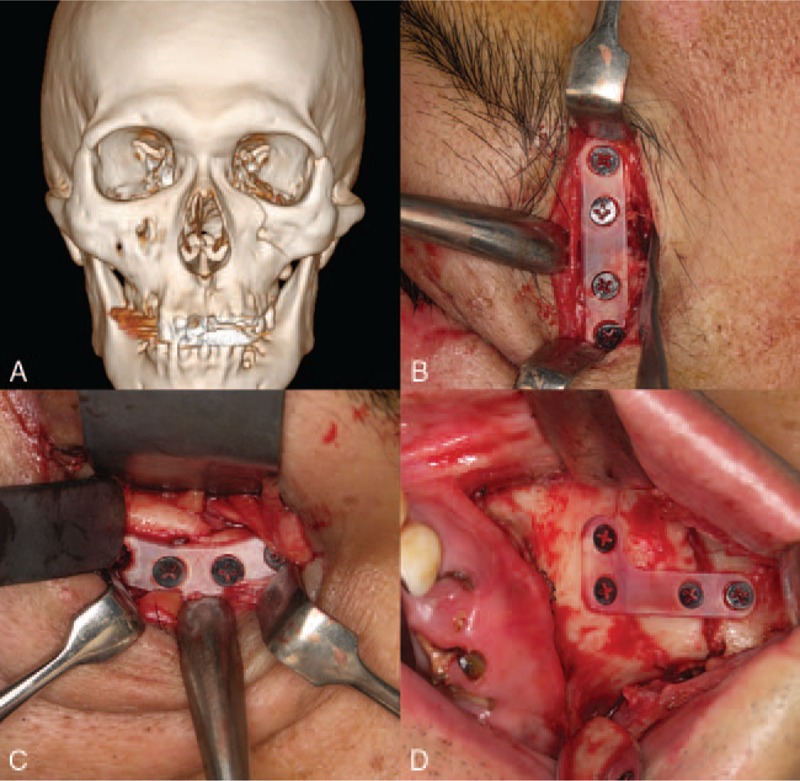
The 3-point fixation technique for the treatment of zygomatic fractures (bioresorbable osteosynthesis materials group (patient 4): (A) frontal view of 3-dimensional computed tomography image showing inferior dislocation of the zygomatic body; (B) placement of a plate across the frontozygomatic fracture area via a lateral eyebrow incision; (C) placement of a plate across the infraorbital rim fracture area through a transconjunctival approach; (D) placement of a plate across the fracture of the zygomaticomaxillary buttress through the maxillary vestibular approach.
Clinical Evaluation
Patients were followed up postoperatively every 2 months, and the functional status and complications (including infection, swelling, nonunion, malunion, and exposure of the plate) of treatment were assessed through clinical and radiographical examinations.
Image Acquisition
Computed tomography (CT) scans were obtained for all patients at 6 months postoperatively using the following parameters: matrix, 512 × 512 pixels; slice thickness, 1 mm; speed per rotation, 1 mm; reconstructed slice increment, 1 mm; and reconstruction algorithm bone gantry tilt, 0°.
Computer Image Analysis
We evaluated the postoperative CT data using SimPlant 11.04 (Materialise Dental Inc, Leuven, Belgium). First, we set the midpoint of the medial and distal edges of the frontozygomatic suture (Fig. 4A). Next, we drew a vertical line to the zygomatic bone from the midpoint to set the point of intersection with the soft tissue. In this way, we measured the distance between the soft tissue and the bone (Fig. 4B). All measurements were collected 3 times from 1 CT scan data, and the mean value was calculated. For each group, we compared the amount of soft-tissue volume increase of the uninjured healthy side with that of the injured operated side.
FIGURE 4.
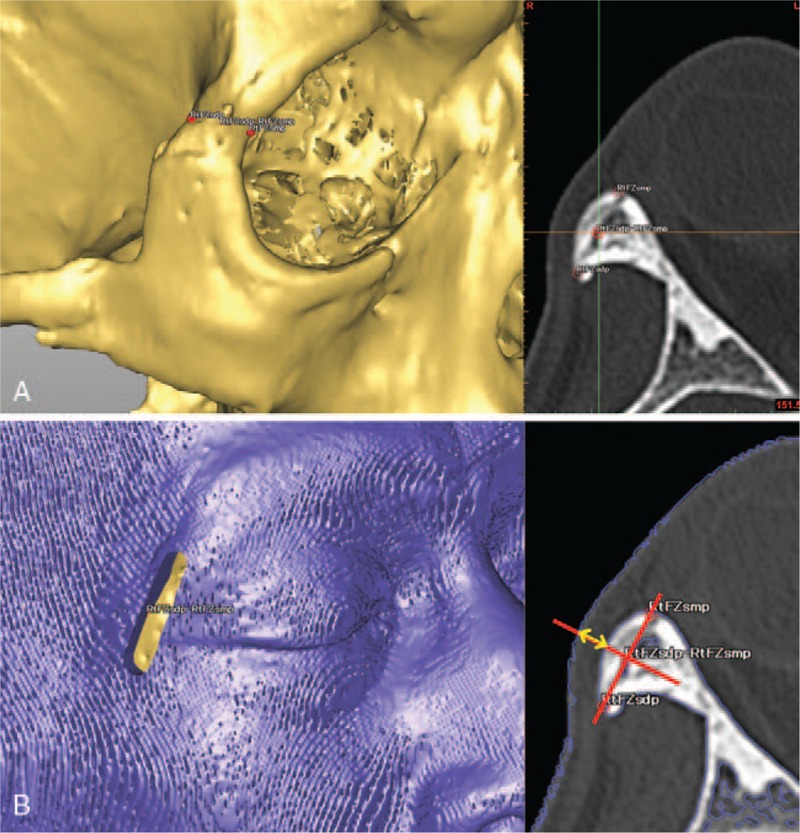
Evaluation of the postoperative computed tomography data using SimPlant 11.04 (Materialise Dental Inc): (A) determination of the midpoint from the medial and distal edges of the frontozygomatic sutures; (B) drawing a vertical line to the zygomatic bone from the midpoint to set the point of intersection with the soft tissue. Then the distance to the soft tissue from the bone was measured.
Statistical Analysis
The paired Student t test was used to compare the amount of soft-tissue volume increase at the frontozygomatic sutures of the injured operated side relative to that of the uninjured healthy side between patients treated with bioresorbable plates and patients treated with titanium miniplates. The software package used for computer-assisted statistical analysis was JMP 11.0 for Mac (SAS Institute Inc, Cary, NC). Results were considered statistically significant when the P value was <0.05.
RESULTS
Patients were followed up postoperatively, and the functional status and complications (including palpability, infection, swelling, nonunion, malunion, and exposure of the plate) of the treatment were assessed by clinical and radiographic examinations both in patients fitted with bioresorbable plates and in those fitted with titanium miniplates (Table 1). All patients eventually achieved satisfactory healing with favorable restoration of form and function without any complication including palpability (Table 1). The fracture lines healed completely in all patients.
TABLE 1.
Clinical Analysis of 12 Patients Treated With a Thin-Type Bioresorbable Osteosynthesis Device or Titanium Miniplates for the Internal Fixation of Zygomatic Fractures
| Patient | Age (y) | Sex | Region of Fracture (R/L) | Associated Maxillofacial Fractures | Cause of Trauma | Fixation Area | Complication |
| Thin flat-type bioresorbable osteosynthesis device (GRAND FIX) | |||||||
| 1 | 28 | M | L | Stumble | 2-Point fixation | None | |
| 2 | 91 | F | L | Traffic accident | 2-Point fixation | None | |
| 3 | 34 | M | R | Mandible fracture | Fall | 3-Point fixation | None |
| 4 | 34 | M | L | Fall | 3-Point fixation | None | |
| 5 | 33 | F | L | Traffic accident | 3-Point fixation | None | |
| 6 | 74 | M | L | Syncope | 2-Point fixation | None | |
| 53.2 | |||||||
| Titanium osteosynthesis device (MatrixMIDFACE) | |||||||
| 1 | 25 | M | R | Mandible fracture | Traffic accident | 3-Point fixation | None |
| 2 | 64 | F | L | Traffic accident | 3-Point fixation | None | |
| 3 | 60 | M | L | Traffic accident | 3-Point fixation | None | |
| 4 | 35 | M | R | Traffic accident | 3-Point fixation | None | |
| 5 | 29 | M | L | Traffic accident | 3-Point fixation | None | |
| 6 | 75 | M | L | Traffic accident | 2-Point fixation | None | |
| 48.0 | |||||||
F, female; L, left; M, male; R, right.
The amount of soft-tissue volume increase at the injured operated side relative to the uninjured healthy side using bioresorbable plates was 131.1% (range: 101.5–165.8). The amount of soft-tissue volume increase at the operated side relative to the healthy side using titanium miniplates was 126.4% (range: 102.2–167.6). There was no statistically significant difference (P = 0.69; >0.05) in the amount of soft-tissue volume increase at the operated side relative to the healthy side at the frontozygomatic sutures between patients treated with the bioresorbable material and those treated with titanium miniplates (Table 2).
TABLE 2.
Comparison of Soft-Tissue Thickness in Patients Treated With Bioresorbable Osteosynthesis Materials and Titanium Miniplates Used for the Internal Fixation of Zygomatic Fractures
| Patient | Injured Operated Side | Uninjured Healthy Side | Operated Side/Healthy Side (%) | ||
| Mean | Standard Deviation | Mean | Standard Deviation | ||
| Thin-type bioresorbable osteosynthesis device (GRAND FIX) | |||||
| 1 | 5.72 | 0.08 | 3.87 | 0.04 | 147.59 |
| 2 | 4.75 | 0 | 4.35 | 0.09 | 109.36 |
| 3 | 5.96 | 0.03 | 3.6 | 0.02 | 165.8 |
| 4 | 4.75 | 0.09 | 4.35 | 0.09 | 139.56 |
| 5 | 3.87 | 0.05 | 3.81 | 0.03 | 101.49 |
| 6 | 4.75 | 0.1 | 4.15 | 0.1 | 129.36 |
| 131.06 ± 24.05 | |||||
| Metal titanium osteosynthesis device (MatrixMIDFACE) | |||||
| 1 | 4.38 | 0.05 | 4.18 | 0.02 | 104.78 |
| 2 | 3.85 | 0.11 | 3.77 | 0.03 | 102.21 |
| 3 | 7.28 | 0.14 | 5.65 | 0.09 | 128.71 |
| 4 | 4.54 | 0.02 | 3.96 | 0.07 | 114.83 |
| 5 | 8.9 | 0.06 | 5.31 | 0.05 | 167.57 |
| 6 | 9.15 | 0.09 | 6.52 | 0.04 | 140.29 |
| 126.4 ± 24.82 | |||||
DISCUSSION
The mechanical properties of titanium, which include strength, ease of handling, and lack of propensity for dimensional changes, prompted its widespread adoption as the material of choice for the manufacture of fixation devices. However, patients with titanium fixation devices may require a second operation to remove them, and the devices occasionally trigger immunoinflammatory responses when used in the treatment of maxillofacial fractures, where they generate fine metal particles.18–20 In contrast, a second operation is unnecessary to remove bioresorbable plate systems. In this respect, they represent very effective devices. However, the thickness of bioresorbable plates is, on average, 2 to 3 times that of metal plates of comparable flexural strength. Indeed, the bioresorbable plates used in this study were about 2 times thicker than the metal plates. Generally, the adverse effects of bioresorbable plates are related to their increased thickness, equating to greater postoperative visibility and palpablity.10–12 Additionally, the frontozygomatic area is traditionally used for fixation in the treatment of fractures of the lateral face of the orbital rim; however, this enhances their undesirable effects.21,22 Kubota et al21 reported that patients fitted with plates at the frontozygomatic sutures were more likely to undergo plate removal surgery. Nagase et al23 showed that higher rates of plate discomfort were experienced with plates fitted near the supraorbital, infraorbital, and mental foramina. Furthermore, Chrcanocic et al22 stated that plates applied to the lateral face of the orbital rim produced undesirable effects, such as palpability and visibility. Taken together, these observations suggest that care is required when using bioresorbable plates at the frontozygomatic sutures and orbital rim in patients with zygomatic fracture to avoid palpability.
In this study, no patients treated with bioresorbable plates or titanium miniplates experienced palpability in the region of the frontozygomatic sutures and orbital rim. The bioresorbable plate system used in this study was of reduced thickness compared with conventional bioresorbable plates. The GRAND FIX plate system is 0.95 mm thick, and is characterized by a counterbore system that enables the plate to remain 0.95 mm thick even when affixed to the bone using screws. Usually, screws (especially screwheads) add their own thickness to the thickness of the plate. Of the commercially available bioresorbable plates at the time of this writing, this plate system is the thinnest when containing screws (Table 3). In addition, it is a flat, smooth structure resembling a stepped plate, eliminating the grip portion of the screwhead by a cross-type of drive mechanism for this screw (Fig. 5). Accordingly, this could reduce discomfort during palpation. The combined thickness of the soft tissue and plate was smallest using the titanium miniplate. Nevertheless, no patients treated with bioresorbable plates complained of foreign body sensation. We believe that this is because of the form of the bioresorbable plate, which is characterized by thinness and evenness as a result of the counterbore structure, and smoothness relative to the surrounding tissue.
TABLE 3.
Distance From the Bone of the Soft Tissue, Including the Osteosynthesis Plate, and the Rate of Increase in Soft-Tissue Thickness of the Affected Side Relative to the Healthy Side
| Bioresorbable Fixation System | Metallic Fixation System | |||||||||||
| SuperFIXORBMX (mm) | FIXORBMX (mm) | LactoSorb (mm) | Sonic Weld (mm) | GrandFix (mm) | MatrixMIDFACE (mm) | |||||||
| Only plate | 1.5 | 2.1 | 1.5 | 0.9 | 1.4 | 1.0 | 1.0 | 0.95 | 1.0 | 0.5 | 0.7 | 0.8 |
| Plate and screw | 1.7–1.8 | 2.1–2.2 | 2.3 | 1.15 | 2.2 | 1.0 | 1.0 | 0.95 | 1.47 | 0.75 | 0.85 | 0.9 |
| Screw thread, outer diameter | 2.2 | 2.2 | 2.5 | 1.6 | 2.4 | 1.85 | ||||||
FIGURE 5.
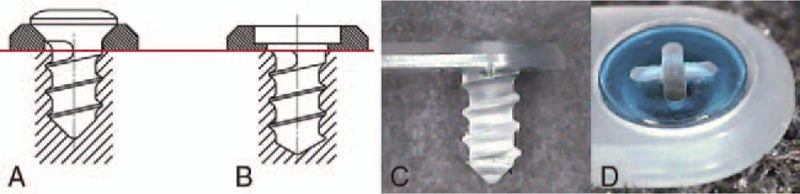
(A) A conventional plate system with a thick plate, further increased by the thickness of the screwhead; (B–D) the thin-type GRAND FIX (Gunze) has a thickness of 0.95 mm, and is characterized by a counterbore system. In the counterbore system, the thickness of the plate is not increased even when fixed using a screw.
In both the bioresorbable materials group and the titanium miniplates group, all patients eventually achieved satisfactory healing with favorable restoration of form and function. As the osteosynthesis material used in zygomatic fracture treatment, this newly bioresorbable plate is effective, and just as safe and reliable as titanium plate. Furthermore, concerning the complication of palpability that has been observed using conventional methods, thin plates could reduce postoperative palpability; thus, they are very effective in areas where patients are likely to report postoperative palpability, such as at the frontozygomatic sutures and infraorbital rim area. In our study, the postoperative course of all patients was uneventful. The foreign body sensation with this thin, flat plate system was negligible, and the plates were almost undetectable to the touch. However, because these plates remain considerably thicker than titanium miniplates, further improvement is necessary in future.
CONCLUSION
In this clinical study, we demonstrated the successful treatment of patients with zygomatic fractures using a thin, flat bioresorbable plate system without complications, including palpability. The difference in palpability between titanium miniplates and thin bioresorbable plates is the result of the difference in thickness of these plates. However, the use of GRAND FIX plates, which have the same strength as the cortical bone yet are much thinner than conventional plates, reduces the burden of palpability. This bioresorbable plate system can be considered clinically useful in the treatment of zygomatic fractures in easily palpated areas such as the infraorbital rim and frontozygomatic sutures.
Footnotes
The authors report no conflicts of interest.
REFERENCES
- 1.Enislidis G, Pichorner S, Lambert F, et al. Fixation of zygomatic fractures with a new bioresorbable copolymer osteosynthesis system. Preliminary results. Int J Oral Maxillofac Surg 1998; 27:352–355. [DOI] [PubMed] [Google Scholar]
- 2.Eppley BL, Sadove MA. Effects of resorbable fixation on craniofacial growth: a pilot experimental study. J Craniomaxillofac Surg 1992; 3:190–196. [DOI] [PubMed] [Google Scholar]
- 3.Eppley BL. Resorbable biotechnology for craniomaxillofacial surgery. J Craniofac Surg 1997; 2:85–86. [PubMed] [Google Scholar]
- 4.Suuronen R, Haers PE, Lindqvist C, et al. Update on bioresorbable plates in maxillofacial surgery. Facial Plast Surg 1999; 15:61–72. [DOI] [PubMed] [Google Scholar]
- 5.Yerit KC, Enislidis G, Schopper C, et al. Fixation of mandibular fractures with bioresorbable plates and screws. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2002; 94:294–300. [DOI] [PubMed] [Google Scholar]
- 6.Ewers R, Harle F. Experimental and clinical results of new advances in the treatment of facial trauma. Plast Reconstr Surg 1985; 75:25–31. [DOI] [PubMed] [Google Scholar]
- 7.Eglin D, Alini M. Degradable polymeric materials for osteosynthesis: tutorial. Eur Cell 2008; 16:80–91. [DOI] [PubMed] [Google Scholar]
- 8.Landes C, Ballon A, Ghanaati S, et al. Treatment of malar and midfacial fractures with osteoconductive forged unsintered hydroxyapatite and poly-l-lactide composite internal fixation devices. J Oral Maxillofac Surg 2014; 72:1328–1338. [DOI] [PubMed] [Google Scholar]
- 9.Pietrzak WS. Effects of ethylene oxide sterilization on 82: 18 PLLA/PGA copolymer craniofacial fixation plates. J Craniofac Surg 2010; 21:177–181. [DOI] [PubMed] [Google Scholar]
- 10.Buijs GJ, van Bakelen NB, Jansma J, et al. A randomized clinical trial of bioresorbable and titanium fixation systems in maxillofacial surgery. J Dent Res 2012; 91:299–304. [DOI] [PubMed] [Google Scholar]
- 11.Menon S, Chowdhury SK. Evaluation of bioresorbable vis-à-vis titanium plates and screws for craniofacial fractures and osteotomies. Med J Armed Forces India 2007; 63:331–333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Norholt SE, Pedersen TK, Jensen J. Le Fort I miniplate osteosynthesis: a randomized, prospective study comparing resorbable PLLA/PGA with titanium. Int J Oral Maxillofac Surg 2004; 33:245–252. [DOI] [PubMed] [Google Scholar]
- 13.Sukegawa S, Kanno T, Katase N, et al. Clinical evaluation of an unsintered hydroxyapatite/poly-l-lactide osteoconductive composite device for the internal fixation of maxillofacial fractures. J Craniofacial Surg 2016; 27:1391–1397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sukegawa S, Kannno T, Kawai H, et al. Long-term bioresorption of bone fixation devices made from composites of unsintered hydroxyapatite particles and poly-l-lactide. J Hard Tissue Biol 2015; 24:219–224. [Google Scholar]
- 15.Matsusue Y, Hanafusa S, Yamamuro T, et al. Tissue reaction of bioabsorbable ultra high strength poly (l-lactide) rod: a long-term study in rabbits. Clin Orthop 1995; 317:246–253. [PubMed] [Google Scholar]
- 16.Shikinami Y, Okuno M. Bioresorbable devices made of forged composites of hydroxyapatite (HA) particles and poly l-lactide (PLLA). Part I: basic characteristics. Biomaterials 1999; 20:859–877. [DOI] [PubMed] [Google Scholar]
- 17.Suuronen R, Pohjonen T, Hietanen J, et al. A 5-year in vitro and in vivo study of the biodegradation of polylactide plates. J Oral Maxillofac Surg 1998; 56:604–614. [DOI] [PubMed] [Google Scholar]
- 18.Katou F, Andoh N, Motegi K, et al. Immuno-inflammatory responses in the tissue adjacent to titanium miniplates used in the treatment of mandibular fractures. J Craniomaxillofac Surg 1996; 24:155–162. [DOI] [PubMed] [Google Scholar]
- 19.Weingert D, Steinemann S, Schilli W, et al. Titanium deposition in regional lymph nodes after insertion of titanium screw implants in maxillofacial region. Int J Oral Maxillofac Surg 1994; 23:450–452. [DOI] [PubMed] [Google Scholar]
- 20.Eppley BL, Morales L, Wood R, et al. Resorbable plate fixation in pediatric craniofacial surgery: long-term outcome. Plate Reconstr Surg 2004; 114:850–856. [DOI] [PubMed] [Google Scholar]
- 21.Kubota Y, Kuroki T, Akita S, et al. Association between plate location and plate removal following facial fracture repair. J Plast Reconstr Aesthet Surg 2012; 65:372–378. [DOI] [PubMed] [Google Scholar]
- 22.Chrcanocic BR, Cavalcanti YS, Reher P. Temporal miniplates in the frontozygomatic area—an anatomical study. Oral Maxillofac Surg 2009; 13:201–206. [DOI] [PubMed] [Google Scholar]
- 23.Nagase DY, Courtemanche DJ, Peters DA. Plate removal in traumatic facial fractures: 13-year practice review. Ann Plast Surg 2005; 55:608–611. [DOI] [PubMed] [Google Scholar]


