Abstract
Background and study aims: Mucosal views can be impaired by residual bubbles and mucus during gastroscopy. This study aimed to determine whether a pre-gastroscopy drink containing simethicone and N-acetylcysteine improves mucosal visualisation.
Patients and methods: We conducted a randomized controlled trial recruiting 126 subjects undergoing routine gastroscopy. Subjects were randomized 1:1:1 to receive: A—pre-procedure drink of water, simethicone and N-acetylcysteine (NAC); B—water alone; or C—no preparation. Study endoscopists were blinded to group allocation. Digital images were taken at 4 locations (lower esophagus/upper gastric body/antrum/fundus), and rated for mucosal visibility (MV) using a 4-point scale (1 = best, 4 = worst) by 4 separate experienced endoscopists. The primary outcome measure was mean mucosal visibility score (MVS). Secondary outcome measures were procedure duration and volume of fluid flush required to achieve adequate mucosal views.
Results: Mean MVS for Group A was significantly better than for Group B (1.35 vs 2.11, P < 0.001) and Group C (1.35 vs 2.21, P < 0.001).
Mean flush volume required to achieve adequate mucosal views was significantly lower in Group A than Group B (2.0 mL vs 31.5 mL, P = 0.001) and Group C (2.0 mL vs 39.2 mL P < 0.001). Procedure duration did not differ significantly between any of the 3 groups.
MV scores at each of the 4 locations demonstrated significantly better mucosal visibility in Group A compared to Group B and Group C (P < 0.0025 for all comparisons).
Conclusions: A pre-procedure drink containing simethicone and NAC significantly improves mucosal visibility during gastroscopy and reduces the need for flushes during the procedure. Effectiveness in the lower esophagus demonstrates potential benefit in Barrett’s oesophagus surveillance gastroscopy.
Introduction
Survival from upper gastrointestinal cancer is largely determined by stage at diagnosis, hence early detection is key to improving outcomes in patients with this group of malignancies. The miss rate for esophageal and gastric cancer at upper gastrointestinal endoscopy is well document, with studies reporting rates of 4 % to 13 % at index endoscopy for cancers diagnosed on subsequent investigations, including repeat endoscopy 1 2 3 4 5 6.
It is common to find views in the upper gastrointestinal tract impaired by mucus and bubbles. That can hamper identification of subtle abnormalities, such as dysplasia within Barrett’s esophagus, or early gastric cancer. Several studies have demonstrated that drinking a defoaming agent before a procedure improves mucosal visibility 7 8. Results are conflicting among studies that have examined whether the addition of a mucolytic such as N-acetylcysteine (NAC) to a defoaming agent offers any further benefit 9 10 11 12 13.
The majority of studies to date have been carried out in Asian populations. The only published study in a Western population of a pre-endoscopy drink containing a defoaming agent and mucolytic was performed by Neale et al in the UK 14. In a pragmatic design with 2 control arms, they compared no preparation with water alone, or a solution of water/simethicone/NAC. The mean volume of procedural flush required and proportion of patients requiring use of flush was significantly lower in the group that received the active solution.
Patients and methods
This study (NICEVIS) was a randomized controlled clinical trial. The primary objective was to determine whether water plus simethicone and NAC, given as a pre-endoscopic drink, improved mucosal visualization compared to an unprepared upper gastrointestinal tract or one prepared with water alone. The trial was registered with the European Clinical Trials agency (EudraCT 2013-001097-24), and approved by the local research ethics committee (13/SC/0248). The study was conducted between July 2013 and March 2014.
Inclusion and exclusion criteria
Patients referred for routine or urgent outpatient upper gastrointestinal endoscopy with a minimum age of 18 years were eligible for inclusion. Predefined exclusion criteria were as follows: emergency cases, patients who would already receive NAC/simethicone pre-endoscopy as part of their standard care, patients with a known stricture, pregnant or breastfeeding women, known upper gastrointestinal malignancy, pharyngeal weakness/paralysis bulbar or pseudobulbar palsy, previous oesophageal or gastric surgery and known allergy to NAC or simethicone.
Baseline patient data on age, gender, medication usage (particularly gastrointestinal medications) were recorded.
Randomization and study procedures
Patients were randomized to 3 groups:-
Group A – Simethicone/NAC pre-endoscopy drink (50 mL water, 1000 mg N-acetylcysteine, 60 mg simethicone)
Group B – 50 mL water pre-endoscopy drink
Group C – no pre-endoscopy drink (current standard practice)
Randomization was performed by random sequence generation in permuted blocks of varying sizes by an independent statistician. Allocations were placed in sealed envelopes to be opened by the nurse preparing the pre-endoscopy drink.
The pre-endoscopy drink was given 5 to 10 minutes before the procedure and subjects were asked to roll onto their left and right sides briefly to aid coverage of the gastric mucosa.
The endoscopist was blinded to the preparation used. Following intubation excess fluid in the stomach was removed via the endoscope suction channel. Electronic photographs were taken at 4 predefined locations (Lower oesophagus/Upper body greater curve/Antrum/Fundus) during the procedure, prior to any mucosal flushing. Images were digitally stored for subsequent mucosal visibility scoring.
Fluid flushes of the simethicone/NAC solution were then used to remove residual mucus/foam to achieve adequate mucosal views. The volume of flushes required and the total procedure duration were recorded.
Photographs were rated for mucosal visibility by 4 experienced endoscopists (scorers). Visibility scores were rated on a 4-point scale (Fig. 1):
Fig. 1.
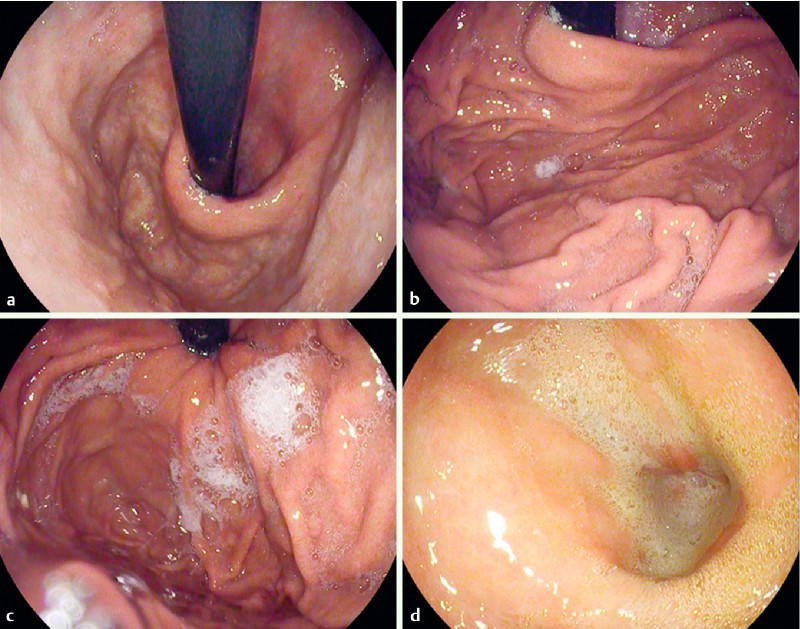
Mucosal visibility score examples; a fundus view score 1, b fundus view score 2, c fundus view score 3, d antrum view score 4.
No adherent mucus and clear views of the mucosa
A thin coating of mucus that did not obscure views of the mucosa
Some mucus/bubbles partially obscuring views of the mucosa (a small mucosal lesion might be missed without flushing).
Heavy mucus/bubbles obscuring views of the mucosa (a small mucosal lesion could easily be missed without flushing)
Therefore the total score based on 4 photographs ranged from 4 (best) to 16 (worst). The scorers were trained in the use of the visibility score with photographic examples prior to scoring the study photographs. A pre-study test was performed to check that there was sufficient interobserver agreement before the study photographs were scored with a prespecified kappa value of > 0.4 required before the study images could be rated. The scorers were blinded to the pre-endoscopy preparation relating to each photograph. The mean visibility scores for the 3 groups were compared.
Primary and secondary endpoints
The primary endpoint was mean total mucosal visibility score at 4 predefined locations rated by 4 blinded assessors. Secondary endpoints were: 1) volume of fluid flushes required to achieve adequate mucosal views; and 2) total procedure time.
Statistics and sample size calculation
Based on the results of similar previous studies, we expected the mean score in Groups B and C to be 8.2 with a standard deviation of 2.7. The standard deviation of Group A was expected to be 1.2. We aimed to be able to detect a 20 % improvement in overall visibility score. Working with a significance level of 0.017 to allow for multiple comparisons between the 3 groups and a power of 80 %, a sample size of 40 patients in each group (120 in total) was required. To allow for missing or spurious data occurring in 5 % of cases, the sample size was increased to 126 (42 patients per group).
Interobserver agreement was calculated using mean weighted Fleiss’s kappa. Mean total mucosal visibility scores between groups were compared using one-way analysis of variance with Tukey’s test to detect between group differences. In post-hoc testing the Chi-squared test was used to compare the proportion of images with inadequate visibility scores (score 3 or 4) between groups. Procedure duration and mean flush volume were compared using 1-way analysis of variance with Tukey’s test to detect differences between groups.
Results
Enrollment and exclusions
A total of 126 patients were enrolled and randomized to the 3 study groups. Three patients were excluded as their procedure could not be completed and 1 was excluded as severe esophagitis was found ( Fig. 2). In a further 2 patients 1 of the 4 study photographs was not captured due to technical reasons. The remaining 3 study photographs for each of these participants were included for analysis.
Fig. 2.
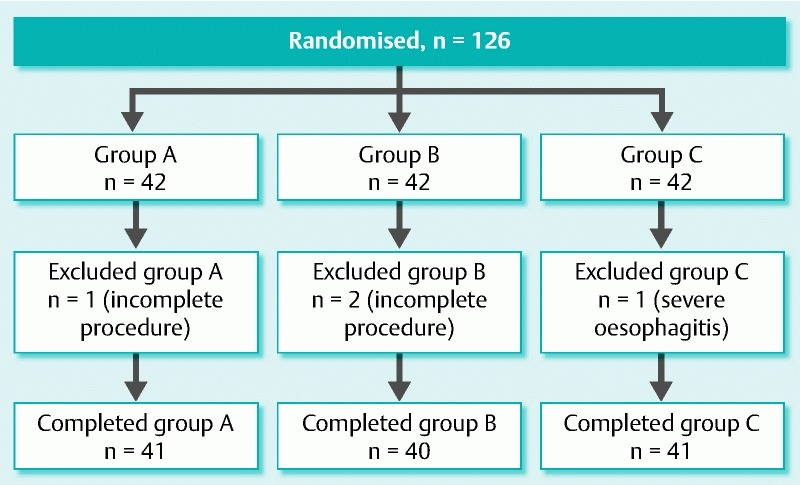
Study enrolment and exclusions flow chart.
One further patient was excluded from the analysis for procedure duration and flush volume because of actively bleeding angiodysplasia that required endoscopic intervention.
Baseline group demographics
The 3 study groups were well matched in terms of baseline demographics and indications for endoscopy (Table 1). A significant difference was found between groups in the number of patients referred for investigation of dysphagia (P = 0.04), but not for any other indications for gastroscopy.
Table 1. Baseline demographics, indications for endoscopy, significant regular medications, relevant comorbidities and procedural medications.
| Study group | A (Water/NAC/Simethicone) n = 41 | B (Water) n = 40 |
C (No prep.) n = 41 |
P value |
| Male gender | ||||
| n (%) | 22 (53.7) | 20 (50.0) | 20 (48.8) | 0.90 |
| Age (Years) | ||||
| mean (SD) | 63.8 (15.8) | 62.3 (15.4) | 61.9 (16.2) | 0.84 |
| Indication – n | ||||
| Dyspepsia/heartburn | 21 | 22 | 13 | 0.10 |
| Dysphagia | 4 | 7 | 13 | 0.04 |
| Anaemia | 6 | 4 | 5 | 0.80 |
| Barrett’s surveillance | 7 | 6 | 8 | 0.84 |
| Weight loss | 2 | 4 | 2 | 0.59 |
| Duodenal biopsies ( + ve TTG) | 1 | 1 | 1 | 1.00 |
| Abnormal radiology | 1 | 0 | 0 | 0.37 |
| Ulcer healing check | 1 | 0 | 4 | 0.07 |
| Other | 5 | 9 | 4 | 0.26 |
| Regular medication – n | ||||
| PPI/H2RA | 31 | 27 | 30 | 0.61 |
| Prokinetic | 5 | 2 | 4 | 0.50 |
| Calcium channel antagonist | 9 | 6 | 6 | 0.60 |
| Comorbidities – n | ||||
| Type 1 Diabetes | 2 | 0 | 0 | 0.13 |
| Type 2 Diabetes | 5 | 5 | 6 | 0.93 |
| Gastroparesis | 0 | 0 | 1 | 0.37 |
| Procedural medication – n | ||||
| Throat spray | 33 | 30 | 29 | 0.59 |
| Sedation | 19 | 23 | 26 | 0.31 |
PPI, proton pump inhibitor; H2RA, histamine 2 receptor antagonist
Use of medications that may affect gastric fluid secretion or gastric emptying (PPI, H2RA, prokinetics and calcium-channel antagonists) did not differ significantly between the 3 groups. There were also no significant differences in the prevalence of conditions that may affect gastric emptying (diabetes mellitus, gastroparesis).
Interobserver agreement prior to rating study images
80 non-study images were used to ensure adequate inter-observer agreement when using the 4-point mucosal visibility rating scale prior to rating of the study images. The mean weighted kappa value between the 4 assessors was 0.583.
Mucosal visibility scores
Analysis of the primary outcome measure of mean total mucosal visibility score (TMVS) showed significant differences between groups. Mucosal visibility was significantly better in Group A compared to Groups B and C (P < 0.001 for both comparisons). No significant difference in mean TMVS was found between Groups B and C (P = 0.541) (Table 2).
Table 2. Mucosal visibility scores overall and by location.
| Study group | ||||||
| Location score (mean, 95 %CI) |
A (Water/NAC/ Simethicone) n = 41 |
B (Water) n = 40 |
C (No prep.) n = 41 |
P value A vs B |
P value A vs C | P value B vs C |
| Lower esophagus | ||||||
| Upper body | 1.18 (1.09 – 1.28) | 1.69 (1.48 – 1.89) | 1.93 (1.66 – 2.21) | 0.002 | < 0.001 | 0.210 |
| Antrum | 1.58 (1.39 – 1.77) | 2.34 (2.11 – 2.57) | 2.36 (2.10 – 2.62) | < 0.001 | < 0.001 | 0.992 |
| Fundus | 1.20 (1.09 – 1.30) | 2.31 (2.02 – 2.60) | 2.40 (2.08 – 2.71) | < 0.001 | < 0.001 | 0.869 |
| Total | 1.45 (1.27 – 1.63) | 2.10 (1.90 – 2.30) | 2.16 (1.92 – 2.40) | < 0.001 | < 0.001 | 0.914 |
| 5.40 (5.02 – 5.80) | 8.44 (7.91 – 8.97) | 8.85 (8.17 – 9.53) | < 0.001 | < 0.001 | 0.541 | |
Subanalysis of the results for each of the 4 predefined locations showed very similar results, with significantly better mean visibility score for each of the 4 locations in Group A compared to Groups B/C and no significant difference in mean score between Groups B and C.
The results of post-hoc testing was carried out to assess the distribution of mucosal visibility scores between groups are shown n Table 3.
Table 3. Distribution of mucosal visibility scores.
| Group | A (Water/NAC/ Simethicone) n = 41 |
B (Water) n = 40 |
C (No prep.) n = 41 |
P value |
| Score – n (%) | ||||
| 1 | 459 (70.4 %) | 176 (27.7 %) | 162 (24.7 %) | |
| 2 | 167 (25.6 %) | 258 (40.6 %) | 286 (43.6 %) | |
| 3 | 16 (2.5 %) | 160 (25.2 %) | 115 (17.5 %) | |
| 4 | 10 (1.5 %) | 42 (6.6 %) | 93 (14.2 %) | |
| Images rated as inadequate prep (3 /4) – n (%) | 26 (4.0 %) | 202 (31.8 %) | 208 (31.7 %) | A vs B < 0.001 |
| A vs C < 0.001 | ||||
| B vs C 0.983 | ||||
| Total image scores – n | 652 | 636 | 656 | |
Significant differences were found between Groups A and B and Groups A and C in the distribution of mucosal visibility scores (P < 0.001). In Group A, 96 % of images were rated as not requiring additional use of flushing to achieve adequate views, compared to 68.2 % in Group B and 68.3 % in Group C.
The mean weighted kappa for the study images was 0.605, indicating good interobserver agreement 15.
Procedure duration and volume of flush used
No significant differences in mean procedure duration between the 3 groups were found ( Table 4). In Group A, a trend towards shorter procedure duration was seen but it did not reach statistical significance.
Table 4. Procedure duration and volume of intraprocedural flush required.
| Group | A (Water/NAC/ Simethicone) n = 41 |
B (Water) n = 40 |
C (No prep.) n = 41 |
P value A vs B |
P value A vs C |
P value B vs C |
| Procedure duration, mean (+ /–SD) – seconds | 309 (+ /– 129) | 352 (+ /– 216) | 334 (+ /– 118) | 0.438 | 0.758 | 0.863 |
| Flush volume, mean (+ /–SD) – mL | 2.0 (+ /– 9.3) | 31.5 (+ /– 38.3) | 39.2 (+ /– 45.4) | 0.001 | < 0.001 | 0.583 |
Mean flush volume required to achieve mucosal views during gastroscopy was 2 mL for Group A compared to 31.5 mL for Group B and 39.2 mL for Group C. The difference in mean volume between Groups A and B and also Groups A and C were highly statistically significant (Table 4). No significant difference in flush volume was found between Groups B and C.
Adverse events
One serious adverse event (AE) occurred during the study. A participant who received water pre-procedure developed laryngospasm shortly after intubation of the esophagus. The procedure was abandoned and the participant recovered quickly with no long-term sequelae. Independent review considered this to be unrelated to the water administered pre-procedure.
Discussion
This randomized controlled trial examined the impact of a pre-gastroscopy drink containing the mucolytic agent N-acetylcysteine and defoaming agent simethicone on mucosal visibility during routine outpatient gastroscopy. Two control groups were used, 1 that receiving water and the other that received no preparation. The endoscopists performing study procedures and the 4 separate endoscopists who assessed the study images were all blinded to group allocation. The active study medication was well tolerated by all participants and did not result in any AEs or reactions.
Analysis of the primary outcome showed significant improvement in mucosal visibility in the group receiving the active study medication compared to both control groups. Hence the findings of this study are in keeping with those of several previous studies demonstrating improvements in gastric mucosal visibility with a pre-gastroscopy drink containing a mucolytic and a defoaming agent 9 10 14. This is the first study to specifically assess the effect of the combination of simethicone and NAC on the quality of mucosal visibility in a Western population. In a post-hoc analysis only 4 % of images in the group receiving the active study medication were deemed to show inadequate mucosal visibility compared to 32 % in the water and no preparation groups. This study was not designed to determine whether the addition of NAC offers any benefit over simethicone and water alone.
Secondary outcome measures demonstrated a marked reduction in the volume of flush required to achieve adequate mucosal views in the group receiving the active pre-gastroscopy drink. We hypothesized that reduced need for flushes may reduce procedure time, but although there was a trend towards reduced time in Group A, it did not reach significance. That may be due to confounding factors such as indication for endoscopy and findings during the procedure. Barrett’s surveillance cases tend to result in a longer procedure time due to the need to carefully assess the Barrett’s mucosa and take multiple biopsies. However the proportion of Barrett’s cases was similar in the 3 study groups. A larger study may have sufficient statistical power to show a significant difference in procedure time between the groups. While no significant difference in procedure time was demonstrated, it can be argued that for subjects in Group A more time could be spent carefully assessing a mucosal surface that was free of mucus and bubbles. In contrast in Groups B & C some of the procedure time would be spent flushing the mucosal surface before adequate views could be achieved, thus reducing the amount of procedure time utilized for careful mucosal inspection.
The importance of adequate bowel cleansing preparation prior to colonoscopy is well understood and numerous studies have demonstrated the importance of good bowel preparation to improve adenoma detection 16 17 18 19. In contrast, at least in the West, the concept of giving preparation prior to gastroscopy is not familiar to most endoscopists and pre-procedure “gastric prep” is not part of routine care. In a nationwide survey, no UK endoscopy units were routinely using a mucolytic drink prior to gastroscopy 20. Adequate preparation prior to gastroscopy is now of even greater importance than in previous years; with improved endoscopic technology, enhancement techniques, and training, endoscopists can detect and remove subtle precancerous lesions and early cancer. However, for that to be possible, good views of the mucosal surface are paramount.
Whereas previous studies of pre-endoscopy preparatory drinks have demonstrated improvement in gastric mucosal visibility, this is the first study to demonstrate improved mucosal visibility in the lower esophagus. This is a vital area for careful inspection during gastroscopy, particularly as the incidence of esophageal adenocarcinoma and gastro-oesophageal junction adenocarcinoma has risen rapidly in the UK in recent years. Early dysplastic lesions arising in Barrett’s oesophagus, the precursor of esophageal adenocarcinoma, can be subtle and easily missed, hence clear views of this particular area of the upper gastrointestinal tract are vital.
There are of course downsides to giving a pre-gastroscopy drink: Time to prepare the drink may lengthen the overall time to complete the procedure. In practice it takes 2 to 3 minutes for a nurse to prepare and administer the drink. In this study the drink was given 5 to 10 minutes prior to the procedure, which led to a further delay while waiting for the drink to take effect. With careful planning, however, patients could be administered the drink in advance of entering the endoscopy suite. There are also cost implications. At current prices the drink costs £ 1.21 per patient. A busy endoscopy unit such as ours performs around 6,000 gastroscopies per annum, which would result in additional annual costs of around £ 7,000.
The main concerns regarding safety of administering a drink prior to endoscopy are those of potential aspiration of fluid. In this study no patient developed aspiration and no AEs related to study medication occurred. Similarly none have been reported in other similar studies.
The ideal outcome measure for any study of this type would be detection of neoplasia, and ideally early upper gastrointestinal neoplasia where curative treatment is still possible. However, given the low rate of neoplasia detection in patients attending for diagnostic gastroscopy, such a study would require many thousands of participants to demonstrate a significant benefit. Therefore, we used mucosal visibility as a surrogate outcome measure.
Conclusion
In summary this study confirms that a pre-gastroscopy drink containing simethicone and NAC significantly improves mucosal visibility in the lower esophagus and stomach and reduces the need for procedural flushing. This has the potential to become part of standard pre-gastroscopy preparation to improve the detection of upper gastrointestinal neoplasia.
Footnotes
Competing interests: None
References
- 1.Yalamarthi S, Witherspoon P, McCole D. et al. Missed diagnoses in patients with upper gastrointestinal cancers. Endoscopy. 2004;36:874–879. doi: 10.1055/s-2004-825853. [DOI] [PubMed] [Google Scholar]
- 2.Raftopoulos S C, Segarajasingam D S, Burke V. et al. A cohort study of missed and new cancers after esophagogastroduodenoscopy. Am J Gastroenterol. 2010;105:1292–1297. doi: 10.1038/ajg.2009.736. [DOI] [PubMed] [Google Scholar]
- 3.Amin A, Gilmour H, Graham L. et al. Gastric adenocarcinoma missed at endoscopy. J R Coll Surg Edinb. 2002;47:681–684. [PubMed] [Google Scholar]
- 4.Khalil Q, Gopalswamy N, Agrawal S. et al. Missed esophageal and gastric cancers after esophagogastroduodenoscopy in a midwestern military veteran population. South Med J. 2014;107:225–228. doi: 10.1097/SMJ.0000000000000092. [DOI] [PubMed] [Google Scholar]
- 5.Bloomfeld R S, Bridgers D I 3rd, Pineau B C. et al. Sensitivity of upper endoscopy in diagnosing esophageal cancer. Dysphagia. 2005;20:278–282. doi: 10.1007/s00455-005-0025-x. [DOI] [PubMed] [Google Scholar]
- 6.Voutilainen M E, Juhola M T. Evaluation of the diagnostic accuracy of gastroscopy to detect gastric tumours: clinicopathological features and prognosis of patients with gastric cancer missed on endoscopy. Eur J Gastroenterol Hepatol. 2005;17:1345–1349. doi: 10.1097/00042737-200512000-00013. [DOI] [PubMed] [Google Scholar]
- 7.McDonald G B, O’Leary R, Stratton C. Pre-endoscopic use of oral simethicone. Gastrointest Endosc. 1978;24:283. doi: 10.1016/s0016-5107(78)73542-x. [DOI] [PubMed] [Google Scholar]
- 8.Bertoni G, Gumina C, Conigliaro R. et al. Randomized placebo-controlled trial of oral liquid simethicone prior to upper gastrointestinal endoscopy. Endoscopy. 1992;24:268–270. doi: 10.1055/s-2007-1010479. [DOI] [PubMed] [Google Scholar]
- 9.Fujii T, Iishi H, Tatsuta M. et al. Effectiveness of premedication with pronase for improving visibility during gastroendoscopy: a randomized controlled trial. Gastrointest Endosc. 1998;47:382–387. doi: 10.1016/s0016-5107(98)70223-8. [DOI] [PubMed] [Google Scholar]
- 10.Kuo C H, Sheu B S, Kao A W. et al. A defoaming agent should be used with pronase premedication to improve visibility in upper gastrointestinal endoscopy. Endoscopy. 2002;34:531–534. doi: 10.1055/s-2002-33220. [DOI] [PubMed] [Google Scholar]
- 11.Chang C C, Chen S H, Lin C P. et al. Premedication with pronase or N-acetylcysteine improves visibility during gastroendoscopy: an endoscopist-blinded, prospective, randomized study. World J Gastroenterol. 2007;13:444–447. doi: 10.3748/wjg.v13.i3.444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Asl S M, Sivandzadeh G R. Efficacy of premedication with activated Dimethicone or N-acetylcysteine in improving visibility during upper endoscopy. World J Gastroenterol. 2011;17:4213–4217. doi: 10.3748/wjg.v17.i37.4213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chang W K, Yeh M K, Hsu H C. et al. Efficacy of simethicone and N-acetylcysteine as premedication in improving visibility during upper endoscopy. J Gastroenterol Hepatol. 2014;29:769–774. doi: 10.1111/jgh.12487. [DOI] [PubMed] [Google Scholar]
- 14.Neale J R, James S, Callaghan J. et al. Premedication with N-acetylcysteine and simethicone improves mucosal visualization during gastroscopy: a randomized, controlled, endoscopist-blinded study. Eur J Gastroenterol Hepatol. 2013;25:778–783. doi: 10.1097/MEG.0b013e32836076b2. [DOI] [PubMed] [Google Scholar]
- 15.Landis J R, Koch G G. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–174. [PubMed] [Google Scholar]
- 16.Harewood G C, Sharma V K, de Garmo P. Impact of colonoscopy preparation quality on detection of suspected colonic neoplasia. Gastrointest Endosc. 2003;58:76–79. doi: 10.1067/mge.2003.294. [DOI] [PubMed] [Google Scholar]
- 17.Hong S N, Sung I K, Kim J H. et al. The Effect of the Bowel Preparation Status on the Risk of Missing Polyp and Adenoma during Screening Colonoscopy: A Tandem Colonoscopic Study. Clin Endosc. 2012;45:404–411. doi: 10.5946/ce.2012.45.4.404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Froehlich F, Wietlisbach V, Gonvers J J. et al. Impact of colonic cleansing on quality and diagnostic yield of colonoscopy: the European Panel of Appropriateness of Gastrointestinal Endoscopy European multicenter study. Gastrointest Endosc. 2005;61:378–384. doi: 10.1016/s0016-5107(04)02776-2. [DOI] [PubMed] [Google Scholar]
- 19.Sherer E A, Imler T D, Imperiale T F. The effect of colonoscopy preparation quality on adenoma detection rates. Gastrointest Endosc. 2012;75:545–553. doi: 10.1016/j.gie.2011.09.022. [DOI] [PubMed] [Google Scholar]
- 20.Callaghan J, Neale J R, Boger P. et al. Patient preparation prior to gastroscopy: a UK wide survey. Gut. 2012;61:A271–A272. [Google Scholar]


