Abstract
Background
Recently, the emergence of long working hours and the associated conditions such as coronary heart disease (CHD) and stroke have gained attention. The aim of this study was to investigate the association between long working hours and the 10-year-risk of CHD and stroke, estimated by Jee’s health risk-appraisal model for ischemic heart disease.
Methods
We analyzed data from Koreans who randomly enrolled in Korean National Health and Nutrition Examination Survey 2008–2012 and finally included 13,799 participants. The participants were classified as per their working hours: 0–30 h/week, 31–39 h/week, 40 h/week, 41–50 h/week, 51–60 h/week, 61–70 h/week, 71–80 h/week, and >80 h/week. The risks for CHD and stroke were determined using Jee’s health risk-appraisal model. Multiple logistic regression was used to analyze the association between working hours and 10-year risk for CHD.
Results
The 10-year risks for CHD and stroke were significantly and positively associated with working hours in both men and women. Furthermore, higher risks for CHD and stroke were associated with longer working hours in women.
Conclusion
Long working hours are significantly associated with the risks of CHD and stroke, estimated by Jee’s health risk-appraisal model. This study suggests the need for proper management of working hours to reduce CHD risk and stroke risk in the Korean population.
Electronic supplementary material
The online version of this article (doi:10.1186/s40557-016-0149-5) contains supplementary material, which is available to authorized users.
Keywords: Coronary heart disease, Stroke, Long working hours, Korean national health and nutrition examination survey
Background
Long working hours can cause health problems such as hypertension, musculoskeletal discomfort, diabetes, occupational injury, increased suicide rate, sleep problems, preterm birth, poor psychological health, and unhealthy lifestyle conditions [1, 2]. Recently, the emergence of long working hours and the associated conditions such as coronary heart disease (CHD) and stroke, have gained attention [3–6]. However, the association of long working hours with CHD and stroke has not yet been clearly established. A recently published meta-analysis study reported that long working hours could be associated with CHD, but evidence for a dose-response relationship between working hours and CHD was insufficient, despite sufficient evidence for its association with stroke [7].
In the Korean population, studies have shown that long working hours may increase the risk of CHD, especially in people who work extremely long hours [8]. However, a limitation of this study was the use of the Framingham equation to determine the 10-year risk; this equation is derived from the participants mainly comprising middle-income Caucasians.
However, the risk could be overestimated in Asian population when estimating the risk by the Framingham equation model [9]. Ahn et al. suggested that the Framingham equation model overestimates the risk of ischemic heart disease in the Korean population [10]. Therefore, estimation of the accurate risks of CHD and stroke is warranted to investigate the relationship of long working hours with CHD and stroke in Korea.
To overcome the limitation of the Framingham equation model in Korean populations, Jee et al. developed an individualized health risk-appraisal model for ischemic heart disease and stroke, by using well-known risk factors such as hypertension and hypercholesterolemia, using data derived from the Korean population. Outcomes were ascertained from data on the National Health Insurance Corporation claim and death certificate. They used Cox proportional hazard model when developing health-appraisal model to estimate the 10-year risk for ischemic heart disease and stroke. They applied split-half method that the first half of data was used for developing a model and the rest was used for testing for validity of models. This health-appraisal model accurately predicted the actual rates of events [11, 12]. The actual ischemic heart disease event rates were similar to the event rates predicted by the Korean risk prediction model for ischemic heart disease [13].
The primary aim of this study was to investigate the association between long working hours and risks of CHD and stroke estimated by Jee’s health risk-appraisal model. In this assessment, differences between genders were taken in account. Considering that the risks of CHD and stroke are preventable, it is important to understand the characteristics of these events, specific risk factors, and populations at risk. Therefore, this study also aimed to identify specific risk factors for CHD and stroke, which may be associated with working hours.
Methods
Study design and participants
The current study used data derived from the Korean National Health and Nutrition Examination Survey (KNHANES) 2007–2013. The KNHANES is a cross-sectional, nationally representative survey, conducted by the Korean Centers for Disease Control and Prevention (KCDC). Multistage probability sampling, stratified according to geographic location, gender, and age, was used. It collects information about the participants’ socioeconomic status, anthropometric measures, health interview, health examination, and nutrition survey. All participants of the KNHANES used in the current study provided written informed consent. This nationwide survey was approved by the Institutional Review Board (IRB) of the KCDC (IRB: 2007-02-CON-04-P; 2008-04EXP-01-C; 2009-01CON-03-2C; 2010-02CON-21-C; 2011-02CON-06-C; 2012-01EXP-01-2C; 2013-07CON-03-4C).
In total, 58,423 individuals (24,871 individuals from the 4th KNHANES, 25,534 individuals from the 5th KNHANES, and 8,018 individuals from the 6th KNHANES) participated in the surveys. For our analysis, we excluded participants who were younger than 30 years of age and older than 60 years of age. Because Jee’s health-appraisal models for CHD and stroke were developed using Korean individuals between the age of 30 years - 60 years of age, we only included those age groups in our analysis (n = 32,972). Subjects who were unemployed or lacked information on economic activity (n = 9,311) as well as subjects with a history of cerebrovascular or cardiovascular disorders (n = 254) were excluded. The risk for CHD was calculated by combining 8 risk factors, and the risk for stroke was calculated by combining 8 risk factors. Subjects with missing values were also excluded (2,035 subjects were eliminated due to absence of one value for these risk factors and 52 subjects were eliminated due to missing information on shift work or working hours). Finally, of 15,886 eligible participants, the final sample size for analysis was 13,799 (7,565 men and 6,234 women) after excluding subjects with missing values (Fig. 1).
Fig. 1.
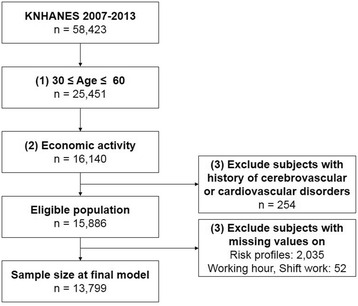
Schematic diagram of the number of participants
Data collection
The KNHANES survey included questions about a wide array of characteristics. We used the following variables: age, gender, occupation-related variables, chronic disease diagnosis, and health behaviour. Completed questionnaires were reviewed by trained staff and entered into a database.
Working hours were measured as the actual number of hours the respondent worked per week without mealtime at all jobs. According to the Korean labour law, standard working hours are 40 h/week, and the reference group included people who worked 40 h/week. Working-hour groups were defined as 0–30 h/week, 31–39 h/week, 40 h/week, 41–50 h/week, 51–60 h/week, 61–70 h/week, 71–80 h/week, and >80 h/week. Occupations were classified into 6 groups: “managers and professionals,” “office workers,” “service and sales workers,” “agriculture, forestry and fisheries workers,” “craft, device, and machine operators, and assembly workers,” and “manual workers.” Daytime work is a full-time schedule in which subjects usually worked between 6 am and 6 pm, excluding rotators. The shift-work group included any schedule other than daytime work such as day-night shift, fixed night, regular rotation, 24-h shift, split shift, and irregular shifts. Smoking status was categorized as non-smoker, ex-smoker, and current smoker. In order to estimate the risk with Jee’s health-appraisal model, the alcohol consumption level at the interview was calculated as consumed alcohol in grams per day. Physical inactivity was defined as engaging in ≥10 min of mild physical activity less than 5 times per week.
Height and weight were measured during the physical examination. Body mass index (BMI) was calculated as weight in kilograms divided by height in meters squared. BMI was classified into 2 groups: <25 kg/m2 and ≥25 kg/m2. Blood pressure (BP) was measured in the right arm at the level of the heart using a standard mercury sphygmomanometer (Baumanometer; WA Baum, Copiague, NY, USA) while the subjects were seated and after they had rested for 5 min. The average of 2 systolic and diastolic blood pressure (SBP and DBP, respectively) readings, which were recorded at an interval of 5 min, was used for analysis. After a 12-h overnight fast, blood samples were obtained from the subjects through an antecubital vein. Total cholesterol (TC) and high-density lipoprotein (HDL) were measured using an ADVIA 1650 autoanalizer (Bayer, Tarrytown, NY, USA) from 2007 to 2008, and Hitachi Automatic Analyzer 7600 (Hitachi, Japan) from 2009 to 2012. Therefore, we used the corrected value of HDL by using conversion formula suggested by KCDC. The participants were considered to have diabetes mellitus (DM) if they met one of the following conditions: (1) fasting plasma glucose level ≥ 126 mg/dL, (2) medical diagnosis of DM by a trained medical professional, or (3) treatment with oral hypoglycemic agents or insulin injections.
Estimation of the 10-year risks for CHD and stroke
Individuals’ risk for CHD was determined using Jee’s health risk-appraisal model for ischemic heart disease, which is based on data collected nationwide from health screenings, cause of death statistics, and insurance claims. This is the first CHD risk-prediction model in Korea that incorporated risk predictors of age, TC, HDL, SBP, DBP, smoking status, and diabetes by gender. After development, the model was validated in another random sample representative of the Korean population. Individuals’ 10-year risk for stroke was also estimated using Jee’s health risk-appraisal model for stroke, which is based on similar methods of the model for CHD. This model estimated the 10-year risk of stroke in Koreans by using age, SBP, diabetes, smoking status, physical inactivity, BMI, alcohol consumption, and total cholesterol by gender. To estimate the future risk of CHD and stroke, we calculated the number of points for each risk factor, after which the individual’s 10-year risk was computed using risk functions for Korean men and women, separately. As both model for CHD and model for stroke was validated by comparing actual event and prediction of event according to decile of predicted risk in each sex, we defined cases as high-risk group when the each risk was ≥90 percentile in each sex. To evaluate the association between weekly working hours and high risk for CHD, and weekly working hours and high risk for stroke, the odds ratios (ORs) and 95% confidence intervals (CIs) were calculated after adjustment for household income, employment condition, occupation, and work shift.
Statistical analysis
The basic characteristics were described by means and standard deviation (SD) or frequencies with percentages for men and women, separately. Risk profiles used for estimating risks for CHD and stroke were presented as means and SD, and categorical values were presented as frequencies and percentage by each gender. First, we performed nonparametric analyses of the associations between weekly working hours and 10-year risks for CHD and stroke to visualize the association. After adjustment for household income, employment condition, occupation, and shift work, generalized additive models considering Poisson distribution were constructed for each outcome using the gam package of R version 2.12.2 (R Foundation for Statistical Computing, Vienna, Austria). Subsequently, the average 10-year risks for CHD and stroke by working-hour schedule were calculated for each gender. Finally, multiple logistic regression was conducted to assess the association between working hours and 10-year risks for CHD and stroke, estimated by Jee’s health risk-appraisal model. As these risks differ according to weekly working hours, we compared the 40 h/week group (reference group) with other working-hour groups. As the risk function used to estimate 10-year risks for CHD and stroke already considered age, SBP, and any other risk profiles, these variables were not used for adjusting variables. After adjustment for household income, employment condition, occupation, work shift, and weekly working hours, multiple logistic regression was performed using PROC LOGISTIC of SAS version 9.3 (SAS Institute, Cary, NC, USA). Two-tailed p-values < 0.05 were considered statistically significant. Additionally, the nonparametric analyses to visualize the association and multiple logistic regression were performed by stratifying 2 age group: <45y and ≥45y.
Results
Table 1 shows the occupational characteristics of the study population. Among the 13,799 participants, 7,565 (54.8%) were men and 6,234 (45.2%) were women. The proportion of paid workers was 61.7% among men and 61.5% among women. In addition, among women, 13.7% were unpaid family workers. In both male and female subjects, <25% of the subjects did shift work, and 25.1% of male and 17.3% of female subjects worked >60 h/week.
Table 1.
Characteristics of the study population
| Men | Women | |||
|---|---|---|---|---|
| n | % | n | % | |
| Age (years) | ||||
| 30–39 | 2475 | 32.7 | 1785 | 28.6 |
| 40–49 | 2661 | 35.2 | 2249 | 36.1 |
| 50–60 | 2429 | 32.1 | 2200 | 35.3 |
| Education | ||||
| Below elementary school | 546 | 7.2 | 1041 | 16.7 |
| Middle school graduate | 771 | 10.2 | 872 | 14.0 |
| High school graduate | 2802 | 37.0 | 2487 | 39.9 |
| Above college graduate | 3446 | 45.6 | 1834 | 29.4 |
| Income status | ||||
| 1st Quartile | 437 | 5.8 | 545 | 8.7 |
| 2nd Quartile | 1733 | 22.9 | 1573 | 25.2 |
| 3rd Quartile | 2518 | 33.3 | 1993 | 32.0 |
| 4th Quartile | 2877 | 38.0 | 2123 | 34.1 |
| Employment condition | ||||
| Paid worker | 4671 | 61.7 | 3836 | 61.5 |
| Self-employed or employer | 2743 | 36.3 | 1547 | 24.8 |
| Unpaid family worker | 151 | 2.0 | 851 | 13.7 |
| Occupation | ||||
| Managers and professionals | 1822 | 24.1 | 1298 | 20.8 |
| Office workers | 1264 | 16.7 | 819 | 13.1 |
| Service and sales workers | 1193 | 15.8 | 2025 | 32.5 |
| Agriculture, forestry, and fishery workers | 576 | 7.6 | 553 | 8.9 |
| Craft, device, and machine operators and assembly workers | 2188 | 28.9 | 411 | 6.6 |
| Manual workers | 522 | 6.9 | 1128 | 18.1 |
| Work shift | ||||
| Fixed-day schedule | 6392 | 84.5 | 5144 | 82.5 |
| Any schedule other than fixed-day schedule* | 1173 | 15.5 | 1090 | 17.5 |
| Weekly working hours | ||||
| < 30 | 460 | 6.1 | 1357 | 21.8 |
| 30–40 | 649 | 8.6 | 974 | 15.6 |
| 40 | 1406 | 18.6 | 981 | 15.7 |
| 40–50 | 1567 | 20.7 | 1085 | 17.4 |
| 50–60 | 1587 | 21.0 | 757 | 12.1 |
| 60–70 | 1009 | 13.3 | 488 | 7.8 |
| 70–80 | 555 | 7.3 | 367 | 5.9 |
| ≥ 80 | 332 | 4.4 | 225 | 3.6 |
| Total | 7565 | 54.8 | 6234 | 45.2 |
*Any schedule other than fixed-day schedule includes day-night shift, fixed night, regular rotation, 24-h shift, split shift, irregular shift, and another schedule
A summary of the each component for Jee’s health risk-appraisal model according to weekly working hours for each gender is presented in Table 2. The mean age (SD) of the male and female subjects was 44.56 (±8.43 SD) and 45.22 (±8.26 SD) years. The levels of TC were similar in men and women, while the BP was slightly lower in women. Likewise, the other risk factors for CHD, such as prevalence of diabetes, current smoking, and alcohol consumption were higher among male subjects than among female subjects. Generally, the level of each variable increased as the weekly work hours increased from 40 h/week to >80 h/week, while those who worked 30–40 h/week and <30 h/week showed higher values than those who worked 40 h/week.
Table 2.
Cardiovascular and stroke risk profiles
| Weekly working hours | SBP | DBP | TC | HDL | Physical Inactivity | DM | Smoking | BMI | Drinking | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | n | % | n | % | n | % | Mean | SD | n | % | |
| Men | ||||||||||||||||||
| < 30 | 122.33 | 16.1 | 81.90 | 11.4 | 193.37 | 35.4 | 48.62 | 12.7 | 247 | 53.7 | 54 | 11.7 | 230 | 50.0 | 24.50 | 3.1 | 358 | 77.8 |
| 30–40 | 120.90 | 14.6 | 81.88 | 10.3 | 194.21 | 35.3 | 50.03 | 12.0 | 317 | 48.8 | 64 | 9.9 | 318 | 49.0 | 24.44 | 2.9 | 520 | 80.1 |
| 40 | 118.97 | 14.3 | 81.20 | 10.8 | 191.79 | 33.0 | 48.15 | 10.9 | 720 | 51.2 | 120 | 8.5 | 616 | 43.8 | 24.51 | 2.9 | 1164 | 82.8 |
| 40–50 | 119.04 | 14.5 | 80.72 | 10.6 | 193.68 | 36.5 | 49.04 | 11.4 | 783 | 50.0 | 115 | 7.3 | 738 | 47.1 | 24.34 | 3.1 | 1260 | 80.4 |
| 50–60 | 119.06 | 14.2 | 80.77 | 10.4 | 191.08 | 33.6 | 48.75 | 11.3 | 797 | 50.2 | 115 | 7.2 | 775 | 48.8 | 24.35 | 3.1 | 1301 | 82.0 |
| 60–70 | 118.95 | 14.9 | 80.65 | 10.8 | 192.61 | 34.4 | 49.28 | 11.2 | 507 | 50.2 | 77 | 7.6 | 508 | 50.3 | 24.24 | 3.1 | 813 | 80.6 |
| 70–80 | 119.80 | 15.0 | 80.90 | 11.0 | 192.00 | 35.4 | 48.79 | 12.7 | 252 | 45.4 | 49 | 8.8 | 283 | 51.0 | 24.69 | 3.0 | 446 | 80.4 |
| ≥ 0. | 120.77 | 14.9 | 81.50 | 10.6 | 197.04 | 36.3 | 48.17 | 10.2 | 157 | 47.3 | 44 | 13.3 | 171 | 51.5 | 24.37 | 3.1 | 269 | 81.0 |
| Total | 119.51 | 14.7 | 81.03 | 10.7 | 192.69 | 34.7 | 48.85 | 11.5 | 3780 | 50.0 | 638 | 8.4 | 3639 | 48.1 | 24.41 | 3.0 | 6131 | 81.0 |
| Women | ||||||||||||||||||
| < 30 | 112.91 | 15.8 | 74.12 | 10.0 | 190.26 | 35.3 | 55.69 | 12.4 | 717 | 52.8 | 62 | 4.6 | 71 | 5.2 | 23.39 | 3.4 | 544 | 40.1 |
| 30–40 | 113.71 | 16.0 | 74.48 | 10.2 | 190.95 | 35.4 | 55.79 | 12.4 | 492 | 50.5 | 41 | 4.2 | 55 | 5.6 | 23.29 | 3.5 | 433 | 44.5 |
| 40 | 111.85 | 15.0 | 74.00 | 9.7 | 184.69 | 33.9 | 56.17 | 12.2 | 487 | 49.6 | 44 | 4.5 | 45 | 4.6 | 23.05 | 3.2 | 436 | 44.4 |
| 40–50 | 113.69 | 16.4 | 74.83 | 10.8 | 187.96 | 35.4 | 56.25 | 12.5 | 557 | 51.3 | 43 | 4.0 | 58 | 5.3 | 23.27 | 3.3 | 501 | 46.2 |
| 50–60 | 115.42 | 16.7 | 75.18 | 10.1 | 190.20 | 34.0 | 55.34 | 12.4 | 393 | 51.9 | 39 | 5.2 | 53 | 7.0 | 23.62 | 3.3 | 360 | 47.6 |
| 60–70 | 115.38 | 16.3 | 74.89 | 10.4 | 191.65 | 35.2 | 55.69 | 13.2 | 245 | 50.2 | 26 | 5.3 | 35 | 7.2 | 23.74 | 3.3 | 216 | 44.3 |
| 70–80 | 118.29 | 17.9 | 76.83 | 11.1 | 193.66 | 36.9 | 54.60 | 11.6 | 156 | 42.5 | 23 | 6.3 | 28 | 7.6 | 24.02 | 3.4 | 172 | 46.9 |
| 6.8 | 117.88 | 17.0 | 76.57 | 10.1 | 199.32 | 39.7 | 55.43 | 12.6 | 98 | 43.6 | 16 | 7.1 | 14 | 6.2 | 24.50 | 3.2 | 106 | 47.1 |
| Total | 114.00 | 16.2 | 74.72 | 10.3 | 189.72 | 35.3 | 55.76 | 12.4 | 3145 | 50.4 | 294 | 4.7 | 359 | 5.8 | 23.43 | 3.4 | 2768 | 44.4 |
SBP systolic blood pressure, DBP diastolic blood pressure, TC total cholesterol, HDL high density lipoprotein, DM diabetes mellitus, BMI body mass index
The nonparametric associations between weekly working hours and 10-year risks for CHD and stroke were evaluated for each gender (Fig. 2). Ten-year risks of both CHD and stroke increased with increasing weekly working hours in subjects working >50 h/week, while decreased with increasing weekly working hours in subjects working <40 h/week.
Fig. 2.
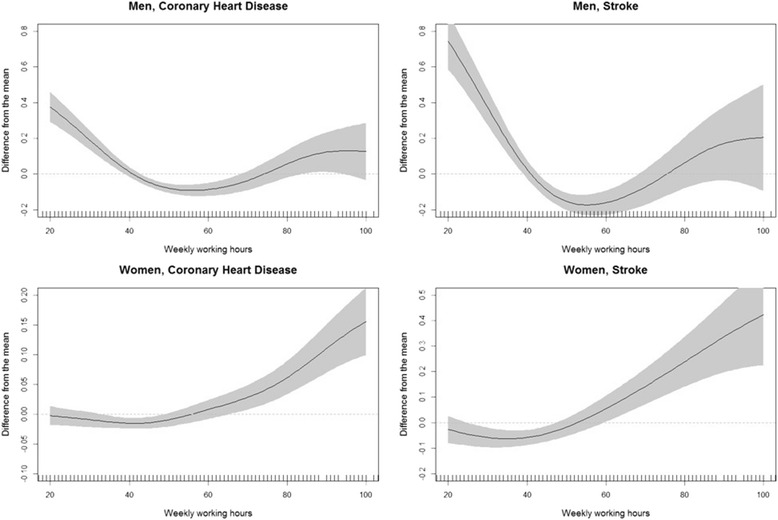
Nonlinear association between weekly working hours, risk for CHD, and risk for stoke in men and women
The risk of CHD and stroke, estimated by Jee’s health risk-appraisal model, is presented according to weekly working hours in Table 3. The average risk of CHD predicted by Jee’s model was 1.11% and 0.26% in male and female subjects, respectively, and that of stroke was 1.97% and 1.45% in male and female subjects, respectively. On comparing those who worked 40 h/week and those who worked >80 h/week, the ORs for high risk of CHD were 1.76 (95% CI: 1.23–2.52) in men and 1.63 (95% CI: 1.03–2.58) in women. The ORs for high risk of stroke were 1.49 (95% CI: 1.03–2.16) in women who worked between 50 and 60 h/week and 2.32 (95% CI: 1.46–3.69) in women who worked >80 h/week, as compared to women who worked 40 h/week. Trend tests were performed after excluding participants who worked <40 h/week. A statistically significant dose-response relationship was found between weekly working hours and high risk for stroke among female subjects.
Table 3.
Odds ratios for high 10-year risk of CHD and stroke
| Weekly working hours | Estimated 10-year CHD risk | ≥90th percentile of estimated risk of CHD | Estimated 10-year stroke risk | ≥90th percentile of estimated risk of stroke | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % | mean | SD | n | % | aORa | 95% CI | mean | SD | n | % | aORa | 95% CI | |||
| Men | ||||||||||||||||
| < 30 | 460 | 6.1 | 1.59 | 14.7 | 89 | 19.4 | 1.75 | 1.28 | 2.40 | 1.59 | 14.7 | 97 | 21.1 | 1.77 | 1.29 | 2.42 |
| 30–40 | 649 | 8.6 | 1.25 | 19.3 | 72 | 11.1 | 1.04 | 0.76 | 1.42 | 1.25 | 19.3 | 86 | 13.3 | 1.24 | 0.91 | 1.68 |
| 40 | 1406 | 18.6 | 1.05 | 5.4 | 122 | 8.7 | 1.00 | Reference | 1.05 | 5.4 | 115 | 8.18 | 8.2 | Reference | ||
| 40–50 | 1567 | 20.7 | 1.03 | 13.2 | 137 | 8.7 | 0.89 | 0.69 | 1.16 | 1.03 | 13.2 | 130 | 8.3 | 0.85 | 0.65 | 1.11 |
| 50–60 | 1587 | 21.0 | 1.01 | 36.0 | 137 | 8.6 | 0.87 | 0.67 | 1.12 | 1.01 | 36 | 127 | 8.0 | 0.79 | 0.60 | 1.03 |
| 60–70 | 1009 | 13.3 | 1.06 | 46.0 | 88 | 8.7 | 0.83 | 0.62 | 1.11 | 1.06 | 46 | 93 | 9.2 | 0.87 | 0.65 | 1.17 |
| 70–80 | 555 | 7.3 | 1.13 | 14.4 | 52 | 9.4 | 0.83 | 0.59 | 1.19 | 1.13 | 14.4 | 63 | 11.4 | 0.99 | 0.70 | 1.39 |
| .39 | 332 | 4.4 | 1.37 | 4.9 | 59 | 17.8 | 1.76 | 1.23 | 2.52 | 1.37 | 4.86 | 45 | 13.6 | 1.23 | 0.83 | 1.82 |
| Total | 7565 | 100.0 | 1.11 | 21.8 | 756 | 10.0 | 1.97 | 15 | 756 | 10.0 | ||||||
| p trend | 0.43 | 0.94 | ||||||||||||||
| Women | ||||||||||||||||
| < 30 | 1357 | 21.8 | 0.26 | 18.2 | 136 | 10.0 | 1.11 | 0.81 | 1.54 | 1.45 | 10.2 | 141 | 10.4 | 1.41 | 1.00 | 1.99 |
| 30–40 | 974 | 15.6 | 0.26 | 122.0 | 95 | 9.8 | 1.08 | 0.77 | 1.53 | 1.42 | 6.2 | 96 | 9.9 | 1.34 | 0.94 | 1.93 |
| 40 | 981 | 15.7 | 0.19 | 16.8 | 65 | 6.6 | 1.00 | Reference | 1.14 | 26.5 | 53 | 5.40 | 5.4 | Reference | ||
| 40–50 | 1085 | 17.4 | 0.23 | 106.0 | 88 | 8.1 | 1.01 | 0.71 | 1.43 | 1.33 | 28.8 | 84 | 7.7 | 1.18 | 0.82 | 1.71 |
| 50–60 | 757 | 12.1 | 0.28 | 24.6 | 81 | 10.7 | 1.06 | 0.74 | 1.51 | 1.59 | 10 | 91 | 12.0 | 1.49 | 1.03 | 2.16 |
| 60–70 | 488 | 7.8 | 0.29 | 14.5 | 61 | 12.5 | 1.09 | 0.74 | 1.61 | 1.65 | 10.1 | 60 | 12.3 | 1.31 | 0.87 | 1.98 |
| 70–80 | 367 | 5.9 | 0.33 | 8.5 | 58 | 15.8 | 1.32 | 0.88 | 1.97 | 1.81 | 2.4 | 54 | 14.7 | 1.47 | 0.96 | 2.25 |
| .25 | 225 | 3.6 | 0.4 | 37.3 | 39 | 17.3 | 1.63 | 1.03 | 2.58 | 2.06 | 7.5 | 44 | 19.6 | 2.32 | 1.46 | 3.69 |
| Total | 6234 | 100.0 | 0.26 | 0.3 | 623 | 10.0 | 1.45 | 1.4 | 623 | 10.0 | ||||||
| p trend | 0.06 | 0.01 | ||||||||||||||
CHD coronary heart disease
aadjusted for household income, employment condition, occupation, work shift, and weekly working hour; values displaying significant differences are given in bold (p-value ≤ 0.05)
*p for trend was tested after excluding participants with <40 weekly working hours
In stratified analysis by age, the nonlinear association was weaker in younger age group (<45y), while similar in older age group (≥45y) (Additional file 1: Figure S1, S2). Long working hours (80 h/week) were associated with the high risk of CHD in men (OR: 1.85, 95% CI: 1.25–2.75) and associated with the high risk of stroke in women (OR: 1.65, 95% CI: 1.01–2.67) (Additional file 2: Table S1).
Discussion
The results of our study show that the 10-year risks for CHD and stroke were significantly associated with working hours. Furthermore, higher risks for CHD and stroke were associated with longer working hours in women. Among the male participants, compared to those who worked 40 h/week, the longest working-hour group showed statistically significant differences in high risk for CHD. However, no such difference was found high risk for stroke. In addition, among female participants, the longest working-hour group showed higher OR for both CHD and stroke.
After stratified by age group, the nonparametric analyses in older age group (≥45y) were consistent with the analyses in main result, while the nonparametric analyses in younger age group (<45y) show weaker association in younger age group. Among older age group, it was statistically significant that the association between the longest working-hours and the risk of CHD in men and between the longest working-hours and the risk of stroke in women.
In our study, compared to the regular working hours, the ORs of high risk for CHD in the longest working-hour group (≥80 h/week) were 1.76 in men and 1.63 in women and were statistically significant. Although our results shows significant associations only in longest working-hour group, these results are in line with those of previous studies, which reported an association between long working hours and CHD. A meta-analysis study concluded that longer working hours was related with the risk of CHD with an OR of 1.37 [14]. Another meta-analysis of 4 prospective studies reported a relative risk of 1.39 for long working hours on CHD [4]. However, recent meta-analysis of large data performed by Kivimaki et al. reported that there was no statistically significant association between working 55 h per week or longer and coronary heart disease [7]. Further studies to investigate how long working hours is associated with coronary heart disease are necessary.
Although several studies have reported an association between long working hours and CHD risk, only a few studies have investigated the association between long working hours and stroke. For example, in a census-based longitudinal study in the United Kingdom, O’reilly and Rosato reported that those who worked ≥55 h/week showed a higher risk of stroke, but the difference was not statistically significant [5]. In the Korean population, however, a case-control study of 940 cases of incident hemorrhagic stroke concluded that longer regular working time and extended duration of strenuous activity during work could increase the risk of hemorrhagic stroke [15]. Recent multi-national studies using unpublished studies reported that long working hours was associated with stroke in a dose-response relationship. We also found a statistically significant association between long working hours and stroke. The ORs for stroke in the longest working-hour group were remarkable (1.22 in men and 1.48 in women), but statistically significant values were found only in women.
We defined high risks for CHD and stroke when the risk for each disease was higher than or equal to the 90th percentile of risk in each gender while considering differences in the risk-estimating methods and risk profiles, and weekly working hours as per gender. Among women, longer working hours showed a statistically significant association with the risk for stroke and marginally significant association with the risk for CHD (p for trend = 0.01 and 0.06, respectively). However, we did not find any such statistically significant association among men. It is possible that these contrasting findings reflect gender differences in influences on the cardiovascular system according to social role. Incomplete recovery from work is known to be associated with death by cardiovascular disease and the employee’s imbalance between work and family responsibilities. Complete recovery away from the workplace is an important component for preventing CHD and stroke [16, 17]. In eastern countries, married women are expected to do unpaid family work such as childcare, cleaning, preparing meals, and caring for elders, regardless of the individual’s working condition. In these cultures, female employees who work longer hours could be overloaded with unpaid family work. These excessive demands could cause excessive stress or lack of time spent on health promotion.
The results of the generalized additive model to nonlinear association suggest a difference in the direction of the association between participants who worked <40 h/week and those who worked ≥40 h/week. Furthermore, we observed a positive association between reduced working hours (<30 h/week) and risk of CHD and stroke in men, and between reduced working hours and risk of stroke in women. One possible explanation of the result is that the workers working less than 40 h per week, which is legal working hours in the Korea, may have inferior socioeconomic status and working condition comparing to the workers working 40 h or longer. Those who have short working hours per week are probably precarious workers and non-regular workers in the Korea, and they could have relatively large work stress from their position [18]. Another explanation may be that selection process between those who works longer hours and those who works reduced hours. In our study, participants with short working hours had higher SBP, DBP, total cholesterol level, physical inactivity, diabetes prevalence. It means that the possibility that those who reduced working hours had poorer health status than those who works general hours (40 h/week) or long hours. As people who have disease would not work long hours, health problem could affect how long time people works. Unfortunately, our cross-sectional study design cannot identify in which direction the selection process between working hours and risks for CHD and stroke may have occurred. Therefore, further studies with a longitudinal design are needed.
Several studies have suggested that long working hours are positively correlated with risk factors for CHD and stroke. The association between work hours and self-reported hypertension has been reported in California [19]. In Japan, increased BP and heart rate were reported among those who periodically worked overtime [20]. In a meta-analysis, a positive association between longer working hours and type 2 diabetes was reported [21]. An individual’s lifestyle such as smoking or frequent drinking was also associated with longer working hours [22, 23]. In our study, we observed higher SBP and DBP among subjects with longer working hours in both men and women (Table 2). Higher TC, higher prevalence of diabetes, and higher prevalence of smoking were seen in those with longer working hours. Compared to those who worked 40 h/week and those who worked ≥80 h/week, the prevalence of diabetes (8.53% vs. 13.25%, respectively) and the percentage of smokers (43.81% vs. 51.51%, respectively) showed significant differences among men, whereas the TC (184.69 mg/dl vs. 199.32 mg/dl, respectively), body mass index (23.05 kg/m2 vs. 24.50 kg/m2, respectively), and prevalence of diabetes (4.49% vs. 7.11%) showed significant differences among women.
Regarding its association with CHD and stroke, working hours could affect an individual’s health through various mechanisms. First, the person’s physical recovery may remain incomplete. Long working hours are associated with reduced time for recovery and limited relaxation time after work. Chronic health impairment could be caused by incomplete physical recovery due to prolonged exposure to work demands such as long working hours [24]. An effect-recovery model suggested that work effort draws upon one’s resources, thereby causing strain reaction [25]. Considering that long working hours could be associated with high job demands, employees who spend more time in the workplace could be restrained and may not be able to avail of appropriate relaxation time to reduce their strain [26, 27]. Second, work-life imbalance could be caused by long working hours. Bad family relationships are have been shown to be associated with sickness-related absence, psychological distress, and poor health [28]. These associations may be more important to Korean women who tend to be the primary care-giver of the family. As such, long working hours could have a larger effect on women’s health because of the domestic burden. In our study, women showed a dose-response relationship between weekly working hours and risks for CHD and stroke (Table 3). Similarly, in Japan, long working hours was associated with poor social dysfunction and poor general health among female factory employees [29]. Third, long working hours could adversely affect an individual’s health, causing physical inactivity, longer time spent in the sitting position, or risky drinking, which are risk factors for CHD or stroke [30–32].
Our study has some strengths. As the results were derived from a representative sample of the general Korean population, we could investigate the population with better variance by using a large sample size with longer working hours than that used in other studies. In addition, by using Jee’s health-appraisal model that was developed and validated in the Korean population for predicting 10-year risk for CHD and stroke, we could more accurately predict the risk as compared to previous studies. Moreover, accurate measurements of BP, TC, and HDL support the validity of the estimated 10-year risks for CHD and stroke.
Despite these strengths, there are limitations to this study. The results from the cross-sectional data preclude us from commenting on causal inferences. To overcome this issue, a longitudinal study design using established outcomes as recorded CHD or stroke event should be performed. Furthermore, we could not consider other factors that may affect the association between working hours, and CHD and stroke, such as job-demand level, poor mental health, and social support. Considering these limitations, further studies are required to confirm our findings.
Conclusion
Long working hours increase the risks of CHD and stroke. These associations were more significantly observed among women than men, especially for the risk of stroke. These results suggest the need for proper management of working hours to reduce the incidence of CHD and stroke in the Korean population. We hope that this study will contribute to the improvement in labor management and reduce the risks of CHD and stroke that are associated with long working hours.
Acknowledgement
Youn-hee Lim contributed to consultation for analysis of data.
Funding
We have nothing to declare.
Availability of data and materials
KNHANES data are available on the KNHANES website (http://knhanes.cdc.go.kr).
Authors’ contribution
D-WL and M-Y K designed the study; D-WL acquired the data; D-W L and M-Y K analyzed data and wrote the manuscript; Y-C H, K-B M, T-SK, M-SK, and M-Y K critically revised the manuscript. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Obtained.
Ethics approval and consent to participate
All participants of the KNHANES used in the current study provided written informed consent. This nationwide survey was approved by the Institutional Review Board (IRB) of the KCDC (IRB: 2007-02-CON-04-P; 2008-04EXP-01-C; 2009-01CON-03-2C; 2010-02CON-21-C; 2011-02CON-06-C; 2012-01EXP-01-2C; 2013-07CON-03-4C).
Abbreviations
- BMI
Body mass index
- BP
Blood pressure
- CHD
Coronary heart disease
- DBP
Diastolic blood pressure
- DM
Diabetes mellitus
- HDL
High-density lipoprotein
- KCDC
Korean centers for disease control and prevention
- KNHANES
Korean national health and nutrition examination survey
- SBP
Systolic blood pressure
- TC
Total cholesterol
Additional files
Nonlinear association between weekly working hours, risk for CHD, and risk for stroke, stratified by age (<45y). Figure S2. Nonlinear association between weekly working hours, risk for CHD, and risk for stroke, stratified by age (≥45y). (DOCX 463 kb)
Odds ratios for high 10-year risk of CHD and stroke among participants ≥ 45y. (DOCX 35 kb)
Contributor Information
Dong-Wook Lee, Email: is2uz@snu.ac.kr.
Yun-Chul Hong, Email: ychong1@snu.ac.kr.
Kyoung-Bok Min, Email: minkb@snu.ac.kr.
Tae-Shik Kim, Email: tekno0713@snu.ac.kr.
Min-Seok Kim, Email: blukey372@gmail.com.
Mo-Yeol Kang, Phone: 82-2-740-8340, Email: snaptoon@snu.ac.kr.
References
- 1.Caruso CC, Hitchcock EM, Dick RB, Russo JM, Schmit JM. Overtime and extended work shifts: recent findings on illnesses, injuries, and health behaviors, vol. 2004-143. Cincinanati: DHHS (NIOSH) Publication; 2004.
- 2.Sparks K, Cooper C, Fried Y, Shirom A. The effects of hours of work on health: a meta‐analytic review. J Occup Organ Psychol. 1997;70(4):391–408. doi: 10.1111/j.2044-8325.1997.tb00656.x. [DOI] [Google Scholar]
- 3.Holtermann A, Mortensen OS, Burr H, Søgaard K, Gyntelberg F, Suadicani P. Long work hours and physical fitness: 30-year risk of ischaemic heart disease and all-cause mortality among middle-aged Caucasian men. Heart. 2010;96(20):1638–44. doi: 10.1136/hrt.2010.197145. [DOI] [PubMed] [Google Scholar]
- 4.Virtanen M, Heikkilä K, Jokela M, Ferrie JE, Batty GD, Vahtera J, et al. Long working hours and coronary heart disease: a systematic review and meta-analysis. Am J Epidemiol. 2012;176(7):586–96. doi: 10.1093/aje/kws139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.O’reilly D, Rosato M. Worked to death? A census-based longitudinal study of the relationship between the numbers of hours spent working and mortality risk. Int J Epidemiol. 2013;42(6):1820–30. doi: 10.1093/ije/dyt211. [DOI] [PubMed] [Google Scholar]
- 6.Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2013;380(9859):2224–60. doi: 10.1016/S0140-6736(12)61766-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kivimäki M, Jokela M, Nyberg ST, Singh-Manoux A, Fransson EI, Alfredsson L, et al. Long working hours and risk of coronary heart disease and stroke: a systematic review and meta-analysis of published and unpublished data for 603 838 individuals. Lancet. 2015;386(10005):1739–46. doi: 10.1016/S0140-6736(15)60295-1. [DOI] [PubMed] [Google Scholar]
- 8.Kang MY, Cho SH, Yoo MS, Kim T, Hong YC. Long working hours may increase risk of coronary heart disease. Am J Ind Med. 2014;57(11):1227–34. doi: 10.1002/ajim.22367. [DOI] [PubMed] [Google Scholar]
- 9.D'Agostino RB, Sr, Grundy S, Sullivan LM, Wilson P. Validation of the Framingham coronary heart disease prediction scores: results of a multiple ethnic groups investigation. JAMA. 2001;286(2):180–7. doi: 10.1001/jama.286.2.180. [DOI] [PubMed] [Google Scholar]
- 10.Ahn KA, Yun JE, Cho ER, Nam CM, Jang Y, Jee SH. Framingham equation model overestimates risk of ischemic heart disease in Korean men and women. Korean J Epidemiol. 2006;28(2):162–70. [Google Scholar]
- 11.Jee SH, Park JW, Lee S-Y, Nam B-H, Ryu HG, Kim SY, et al. Stroke risk prediction model: a risk profile from the Korean study. Atherosclerosis. 2008;197(1):318–25. doi: 10.1016/j.atherosclerosis.2007.05.014. [DOI] [PubMed] [Google Scholar]
- 12.Jee SH, Jang Y, Oh DJ, Oh B-H, Lee SH, Park S-W, et al. A coronary heart disease prediction model: the Korean Heart Study. BMJ Open. 2014;4(5):e005025. doi: 10.1136/bmjopen-2014-005025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jung KJ, Jang Y, Oh DJ, Oh B-H, Lee SH, Park S-W, et al. The ACC/AHA 2013 pooled cohort equations compared to a Korean Risk Prediction Model for atherosclerotic cardiovascular disease. Atherosclerosis. 2015;242(1):367–75. doi: 10.1016/j.atherosclerosis.2015.07.033. [DOI] [PubMed] [Google Scholar]
- 14.Kang M-Y, Park H, Seo J-C, Kim D, Lim Y-H, Lim S, et al. Long working hours and cardiovascular disease: a meta-analysis of epidemiologic studies. J Occup Environ Med. 2012;54(5):532–7. doi: 10.1097/JOM.0b013e31824fe192. [DOI] [PubMed] [Google Scholar]
- 15.Kim BJ, Lee SH, Ryu WS, Kim CK, Chung JW, Kim D, et al. Excessive work and risk of haemorrhagic stroke: a nationwide case‐control study. Int J Stroke. 2013;8(A100):56–61. doi: 10.1111/j.1747-4949.2012.00949.x. [DOI] [PubMed] [Google Scholar]
- 16.Kivimäki M, Leino-Arjas P, Kaila-Kangas L, Luukkonen R, Vahtera J, Elovainio M, et al. Is incomplete recovery from work a risk marker of cardiovascular death? Prospective evidence from industrial employees. Psychosom Med. 2006;68(3):402–7. doi: 10.1097/01.psy.0000221285.50314.d3. [DOI] [PubMed] [Google Scholar]
- 17.Berg P, Kalleberg AL, Appelbaum E. Balancing work and family: The role of high‐commitment environments. Ind Relat. 2003;42(2):168–88. doi: 10.1111/1468-232X.00286. [DOI] [Google Scholar]
- 18.Jang T-W, Kim H-R, Lee H-E, Myong J-P, Koo J-W. Long work hours and obesity in Korean adult workers. J Occup Health. 2013;55(5):359–66. doi: 10.1539/joh.13-0043-OA. [DOI] [PubMed] [Google Scholar]
- 19.Yang H, Schnall PL, Jauregui M, Su T-C, Baker D. Work hours and self-reported hypertension among working people in California. Hypertension. 2006;48(4):744–50. doi: 10.1161/01.HYP.0000238327.41911.52. [DOI] [PubMed] [Google Scholar]
- 20.Hayashi T, Kobayashi Y, Yamaoka K, Yano E. Effect of overtime work on 24-hour ambulatory blood pressure. J Occup Environ Med. 1996;38(10):1007–11. doi: 10.1097/00043764-199610000-00010. [DOI] [PubMed] [Google Scholar]
- 21.Kivimäki M, Virtanen M, Kawachi I, Nyberg ST, Alfredsson L, Batty GD, et al. Long working hours, socioeconomic status, and the risk of incident type 2 diabetes: a meta-analysis of published and unpublished data from 222 120 individuals. Lancet Diabetes Endocrinol. 2015;3(1):27–34. doi: 10.1016/S2213-8587(14)70178-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Maruyama S, Morimoto K. Effects of long workhours on life-style, stress and quality of life among intermediate Japanese managers. Scand J Work Environ Health. 1996;22(5);353–9. [DOI] [PubMed]
- 23.Cho Y-S, Kim H-R, Myong J-P, Kim HW. Association between work conditions and smoking in South Korea. Saf Health Work. 2013;4(4):197–200. doi: 10.1016/j.shaw.2013.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Geurts SA, Sonnentag S. Recovery as an explanatory mechanism in the relation between acute stress reactions and chronic health impairment. Scand J Work Environ Health. 2006;32(6);482–92. [DOI] [PubMed]
- 25.Meijman TF, Mulder G, Drenth P, Thierry H. Psychological aspects of workload. In: Drenth PJD, Thierry H, editors. Handbook of work and organizational psychology: Work psychology. Hove: Psychology Press; 1998. pp. 5–33. [Google Scholar]
- 26.Rissler A, editor. Stress reactions at work and after work during a period of quantitative overload. Ergonomics. London: Taylor & Francis Ltd One Gunpowder Square; 1977. [Google Scholar]
- 27.Spurgeon A, Harrington JM, Cooper CL. Health and safety problems associated with long working hours: a review of the current position. Occup Environ Med. 1997;54(6):367–75. doi: 10.1136/oem.54.6.367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Väänänen A, Kevin MV, Ala-Mursula L, Pentti J, Kivimäki M, Vahtera J. The double burden of and negative spillover between paid and domestic work: associations with health among men and women. Women Health. 2005;40(3):1–18. doi: 10.1300/J013v40n03_01. [DOI] [PubMed] [Google Scholar]
- 29.Ezoe S, Morimoto K. Behavioral lifestyle and mental health status of Japanese factory workers. Prev Med. 1994;23(1):98–105. doi: 10.1006/pmed.1994.1014. [DOI] [PubMed] [Google Scholar]
- 30.Virtanen M, Jokela M, Nyberg ST, Madsen IE, Lallukka T, Ahola K, et al. Long working hours and alcohol use: systematic review and meta-analysis of published studies and unpublished individual participant data. BMJ. 2015;350:g7772. doi: 10.1136/bmj.g7772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kumar A, Prasad M, Kathuria P. Sitting occupations are an independent risk factor for Ischemic stroke in North Indian population. Int J Neurosci. 2014;124(10):748–54. doi: 10.3109/00207454.2013.879130. [DOI] [PubMed] [Google Scholar]
- 32.Schneider S, Becker S. Prevalence of physical activity among the working population and correlation with work-related factors: results from the first German National Health Survey. J Occup Health. 2005;47(5):414–23. doi: 10.1539/joh.47.414. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
KNHANES data are available on the KNHANES website (http://knhanes.cdc.go.kr).