Abstract
The diagnosis and management of nonvenereal diseases are always a tough challenge for the dermatologist due to lack of studies on its diagnostic criteria and standard treatment guidelines. Zoon balanitis (ZB) is one of the benign nonvenereal dermatoses, which presents as a solitary, persistent erythematous plaque usually on the glans penis primarily in the uncircumcised, middle-aged to old-aged men. Although it was described by Zoon in 1952, its etiopathogenesis still remains hypothetical. This article provides an overview of the epidemiology, clinical presentation, histopathological features, and diagnostic criteria and diagnostic methods of ZB. In addition to this, it is rather very important to differentiate this lesion from its clinical equivocal lesions such as erythroplasia of Queyrat, infective and other inflammatory penile dermatoses, which has been discussed in this review. The treatment modalities have also been reviewed in details, and the importance of circumcision as the treatment of choice has been emphasized.
Key words: Circumcision, lasers, nonvenereal disease, topical calcineurin inhibitors, Zoon balanitis
INTRODUCTION
All the genital lesions are not sexually transmitted. A dermato-venereologist must be familiar with these “nonvenereological diseases” which are a cause of grave concern for the patient as they either consider it as a sexually transmitted disease or as a malignancy, which enhances their anxiety. Here arises the importance of a venereologist who not only has to diagnose and treat the condition effectively but also has to allay the patient's anxiety associated with this condition.
Zoon balanitis (ZB) is one of the nonvenereal conditions, which usually affects middle-aged to older men who are uncircumcised. It is an idiopathic, chronic, benign inflammatory mucositis of the genitalia that clinically presents as a solitary, shiny, well-defined erythematous plaque on the glans.[1] ZB is also known as balanitis circumscripta plasmacellularis or plasma cell balanitis of Zoon.[1] It has been described as rare by the textbooks and literature, but probably it is underdiagnosed.[2] Analogous lesions have been described in females with similar clinical and histological features of ZB and termed as Zoon's vulvitis, plasma cell vulvitis, or vulvitis circumscripta plasmacellularis.[1]
ZB is an entity of utmost importance both for the patients due to their concern regarding its prognosis and its management can be really challenging for the dermato-venereologists. ZB is an entity of utmost importance both for the patients due to their concern regarding its prognosis and for the demato-venereologists due to its management being really challenging. Thus, the main objective of this article is to present a systematic review of the available published literature regarding clinical presentations and efficacy of various recent treatment modalities in the management of ZB.
HISTORY
In 1952, Zoon first recognized this entity in eight male patients with chronic balanitis.[3] As all these patients had similar histopathological features, Zoon named this condition as “balanoposthite chronique circonscrite bénigne á plasmocytes” or “balanitis chronica circumscripta plasmacellularis” and considered it as a distinct entity.[3] Garnier in 1954 reported similar lesions in the vulva.[4] Subsequently, Nikolowski [5] described identical lesion in the oral mucosa and Kortnig [6] detected them in the conjunctiva.
Epidemiology
There is a scarcity of published data regarding the incidence and prevalence of ZB. An earlier study by Mallon et al.[7] reported 27 cases of ZB out of 357 males with genital skin disease. In a recent study by Pearce et al.,[8] out of 226 patients examined in a genitourinary medicine clinic over a period of 3 years, 26 (10%) patients had ZB. As far as Indian literature is concerned, there are no published data regarding the incidence and prevalence of ZB in Indian patients.
Etiology
Etiology and pathogenesis of this condition are still speculative. As it is mostly seen in uncircumcised men, it is thought to be because of irritation, due to retention of urine and smegma in context of “dysfunctional prepuce,” leading to poor genital hygiene and repeated local infection.[9] In addition, trauma, friction, heat, and constant rubbing may be a contributory factors.[9] Thus, the two most important triggering factors are the constant exposure of the mucosa to humid condition and to chronic irritation.[10] This explains why lesions of ZB undergo prolonged remission after circumcision.[10]
In addition, other possible causes of ZB that have been described in the literature include chronic infection with Mycobacterium smegmatis and human papillomaviruses (HPV).[11] However, no evidence has yet been reported for bacterial infection and polymerase chain reaction has also failed to detect DNA of HPV.[12] Similarly, there is no evidence for the supposition that ZB may be caused by local disturbance of circulation.[13] It has also been related to lichen aureus due to marked hemorrhage in association with lichenoid infiltrate that is seen in ZB.[14] However, lichen aureus usually affects the lower limbs and is not associated with common histopathological signs of ZB such as erosions, neutrophils, and plasma cells. Thus, there is a lack of supportive evidence for this hypothesis.[13] Furthermore, there is no supportive evidence for the hypothesis given by Nishimura et al.,[15] who had suggested that immediate hypersensitivity response mediated by IgE class of antibodies plays an important role in the etiopathogenesis of ZB. Hyman and Leider speculated that “extramedullary plasmacytic infiltrations that persists are expressions of occult multiple myeloma” and could be a cause ZB.[16] However, it has been contradicted by subsequent studies that have demonstrated clearly the polyclonal nature of the plasmacytic infiltration in ZB.[13]
CLINICAL FEATURE
Symptoms
It is usually asymptomatic and patient only presents with change in appearance of the genitalia. However, sometimes, it might be accompanied with symptoms such as pruritus, dysuria, pain, and burning sensation. Rarely blood-stained discharge or dyspareunia has been described.[17]
Clinical appearance
It presents as single or multiple well-circumscribed, orange-red, shiny, moist, glistening macular to slightly raised plaque(s) [Figures 1 and 2]. The clinical criteria given by Kumar et al. are given in Table 1.[18] Multiple pinpoint, brighter red spots may be speckled on the background of this orange-red plaque, called as “cayenne pepper spots” due to microhemorrhage and hemosiderin deposition.[1] Sometimes, prepuce may display “kissing lesion” on areas that is in direct contact with the lesions. Subsequently, these may erode and leave behind a “rusty stain.”[1] Two distinct clinical variants of ZB have been reported, which include erosive type with bleeding, particularly on the inner surface of prepuce and vegetative type.[11]
Figure 1.
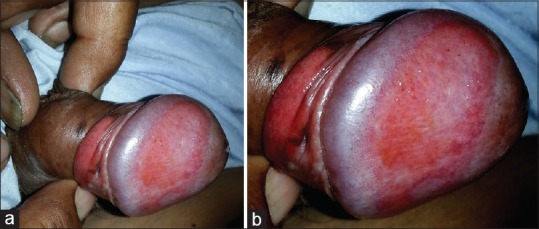
(a and b) Well-circumscribed orange-red, shiny plaque on the glans penis and undersurface of the prepuce with multiple pinpoint red spots
Figure 2.

Orange-red shiny plaque on the glans penis and undersurface of the prepuce
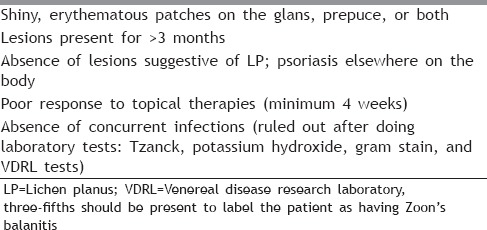
Table 1.
Clinical criteria for diagnosing Zoon balanitis[18]
Sites affected
It is most commonly located on the glans penis, but inner surface of prepuce and coronal sulcus may be involved.[1] Female genitalia, especially labia minora, may be affected by similar lesions. Other sites are oral mucosa (gingiva, hard palate, buccal mucosa), conjunctiva, urethra, cheeks, and epiglottis.[13] It usually affects uncircumcised males, but only one case report of ZB affecting circumcised male in a HIV-positive patient had been described in the literature.[19]
Schuermann in 1960 proposed that these lesions at different sites were variants of the same pathologic process and suggested the term “plasmacytosis circumorificialis.”[20] Other authors supported their concept, but they gave their own name, for example, “plasmacytosis mucosae” and “plasma cell orificial mucositis.”[21]
Differential diagnosis
It includes candidiasis, lichen planus, secondary syphilis, erythroplasia of Queyrat (squamous cell carcinoma in situ [CIS]), or Bowen's disease of the glans penis, which clinically simulate ZB. Furthermore, fixed drug eruption, allergic contact dermatitis, genital herpes, pemphigus vulgaris, flexural psoriasis, and Reiter's disease should be differentiated from ZB.[11]
Other association
Some authors have found an association between ZB and erythroplasia of Queyrat; while others believe that ZB can precede carcinoma of the penis, supposing that the carcinogenic changes may arise in the chronically inflamed mucosa of ZB. On the detailed scan of literature, there are four case reports, i.e., three of erythroplasia of Queyrat and one of carcinoma of the penis arising on lesions of ZB.[22,23,24] Identification of this condition is important owing to the risk of invasive cancer and institute timely appropriate treatment. Thus, patients of ZB must be carefully followed for persistence or worsening of lesions and repeated biopsies should be done to rule out the underlying malignancy.
In addition, a case of lichen sclerosus et atrophicus developing in a patient of ZB after treatment with carbon dioxide (CO2) laser has also been reported.[10] However, multicenter long-term studies with more number of patients are required to prove these associations.
DIAGNOSIS
The clinical differentiation between ZB and its clinically equivocal dermatosis may be sometimes challenging. Hence, following diagnostic methods are helpful to make a definite diagnosis of ZB:
Histopathological examination
ZB has very distinct histopathological changes affecting both epidermis and dermis.[13]
Epidermal changes → Earliest histopathological changes show epidermal thickening, acanthosis, and parakeratosis. This is followed by epidermal atrophy, at times erosions and spongiosis. These superficial erosions can be associated with scattered neutrophils in the upper reaches of epidermis. Accentuation of spongiosis occurs in the lower half of the spinous zone. Additional features such as subepidermal clefts, necrotic keratinocytes, and lozenge keratinocytes (i.e., elongated keratinocytes in the lower half of the spinous zone arranged parallel to the skin surface) may be seen in the later stages of ZB.
Dermal changes → Initially, there is a patchy lichenoid infiltrate of lymphocytes and some plasma cells in papillary dermis, which is subsequently replaced by dense band-like infiltrate of plasma cells, neutrophils, eosinophils, lymphocytes, and erythrocytes. Among all these infiltrate, plasmocytes are predominant usually exceeding 50% of all the cells. It may be associated with siderophages (i.e., macrophage that has absorbed iron-containing particles), hemosiderin deposition and extravasated red blood cells. Changes in dermal vasculature include vascular dilatation with singular vertical or oblique orientation of proliferated individual vessels, which is characteristic of ZB. These are more common in cases with a dense infiltrate. In the later stages, upper dermis shows fibrosis which correlates well with subepidermal clefts, epidermal atrophy, and plasma cell infiltrates. Immunohistochemical studies of plasmocytes in ZB show that plasmocytes produce immunoglobulin G (IgG) predominantly to a lesser degree IgA and IgM.[10]
It is relatively simple to differentiate the premalignant lesions from ZB histopathologically as one can see dysplastic epithelium in the premalignant lesions while it is absent in case of ZB. Histologically, benign conditions such as pemphigus vulgaris, flexural psoriasis, lichen planus, and Reiter's disease may show features in common with ZB but lack the typical changes in the epidermis and dermal blood vessels.
Reflectance confocal microscopy [25]
Reflectance confocal microscopy (RCM) is an in vivo imaging method used to obtain morphologic information about both the architecture and single cells in the epidermis and superficial dermis by Vivascope 1500.[25] Generally, genital skin is suitable for confocal microscopy because of its thin or absent cornified layer. It is very useful tool to differentiate ZB from CIS. The most relevant features for CIS on RCM are atypical honeycomb pattern, disarranged epidermal pattern/focal loss, and round nucleated cells.[25] A nucleated honeycomb pattern and vermicular vessels is a clue for benign inflammatory genital skin disease. In contrast to this, the adjacent normal skin shows a typical honeycomb pattern and round papillary vessels. Thus, RCM may be helpful in avoiding biopsies at sensitive sites by differentiating between balanitis and CIS.[25]
Dermoscopy [26]
The two most commonly observed dermoscopic features are focal/diffuse orange-yellowish structure – less areas (representing to hemosiderin deposition) and curved vessels (corresponding to vascular dilatation/proliferation).[26] The presence of fairly focused curved vessels having different width includes serpentine, convoluted, and chalice-shaped vessels. Most of the curved vessels are fairly focused due to the epidermal thinning usually encountered in ZB, which makes the dermal vessels fairly closer to the surface and thus making them sharper and brighter.[26] Studies have also reported other less common features such as linear irregular blurry vessels, dotted vessels, and spermatozoa-like vessels.[26]
Thus, these dermoscopic findings are helpful in distinguishing ZB from its important differential diagnosis such as erythroplasia of Queyrat (which has been reported to show scattered glomerular vessels), psoriasis (that commonly show regular dotted/glomerular vessels), and nonspecific balanitis usually displaying linear irregular unspecific blurry vessels.[26]
Management
General measures
Promotion of good hygiene is an easy and potentially beneficial measure. Patients should be instructed to retract the foreskin regularly and perform gentle cleansing of entire glans, preputial sac, and foreskin.[17] In addition, patients may also require treatment for anxiety, cosmetic disfigurement, discomfort, and irritation.
Medical management [Table 2]
Table 2.
Various medical management of Zoon's balanitis
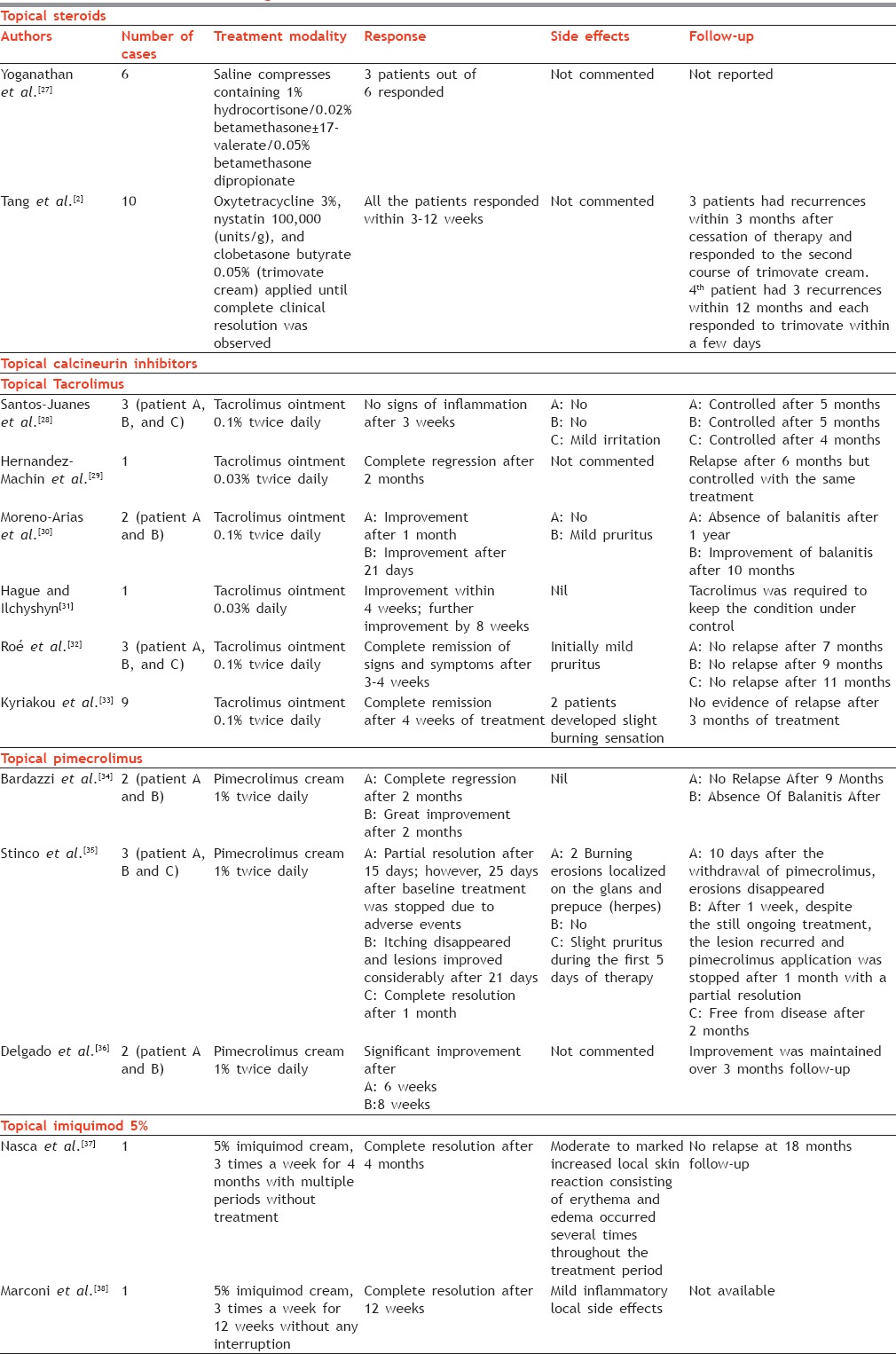
Topical steroids preparations - There are mainly two studies one by Yoganathan et al.[27] and another by Tang et al.,[2] who had highlighted the importance of topical steroids in ZB. According to these studies, moderately potent steroid preparation with or without topical antibiotics is effective alternative to surgical management although these studies did not raise the level of evidence [Table 2]
Topical calcineurin inhibitors (TCIs) - This includes topical tacrolimus ointment (both 0.1% and 0.03%) and topical pimecrolimus 1% cream. The exact mechanism of action of TCIs in these conditions is not known. It has been postulated that tacrolimus may affect the plasma cell response via its action on helper T-cells or a possible underlying T-cell dysfunction.[28,29,30,31,32,33] Pimecrolimus exhibits its immunosuppressive action via inhibition of helper T-cells and by inhibiting plasma cells, thus avoiding colonization of plasma cells and TH cells in the dermis. Furthermore, pimecrolimus leads to inhibition of histamine release by mast cells, which may result in improvement of the symptoms.[34,35,36] TCI are being used in the management of several dermatological conditions, due to their efficacy, safety profile, lack of rebound effect, and absence of tachyphylaxis. Most of the researchers have used TCIs in ZB for 4–8 weeks resulting in significant clinical improvement without any severe side effect.[28,29,30,31,32,33,34,35,36] However, concern regarding its relationship with carcinogenesis has been mentioned in the literature.[22,39,40] Therefore, before starting treatment with these agents, carcinogenic and precarcinogenic conditions should be carefully ruled out as they may promote evolution of preexisting neoplastic conditions [Table 2]
Imiquimod 5% - There are only two case reports of ZB treated with imiquimod.[37,38] The mechanism of action of imiquimod in ZB is unknown. However, it is postulated that it acts via triggering the upregulation of cellular immunity which may overcome local response to some unknown causative agents.[37] Adverse effects including local reactions, i.e., edema and erythema, are frequently seen with imiquimod and are usually managed with good patient's education and dose titration. However, long-term controlled studies are needed to confirm its effect and to know the dose and duration of therapy for complete clearance in ZB [Table 2].
Surgical management [Table 3]
Table 3.
Various surgical modalities for Zoon's balanitis
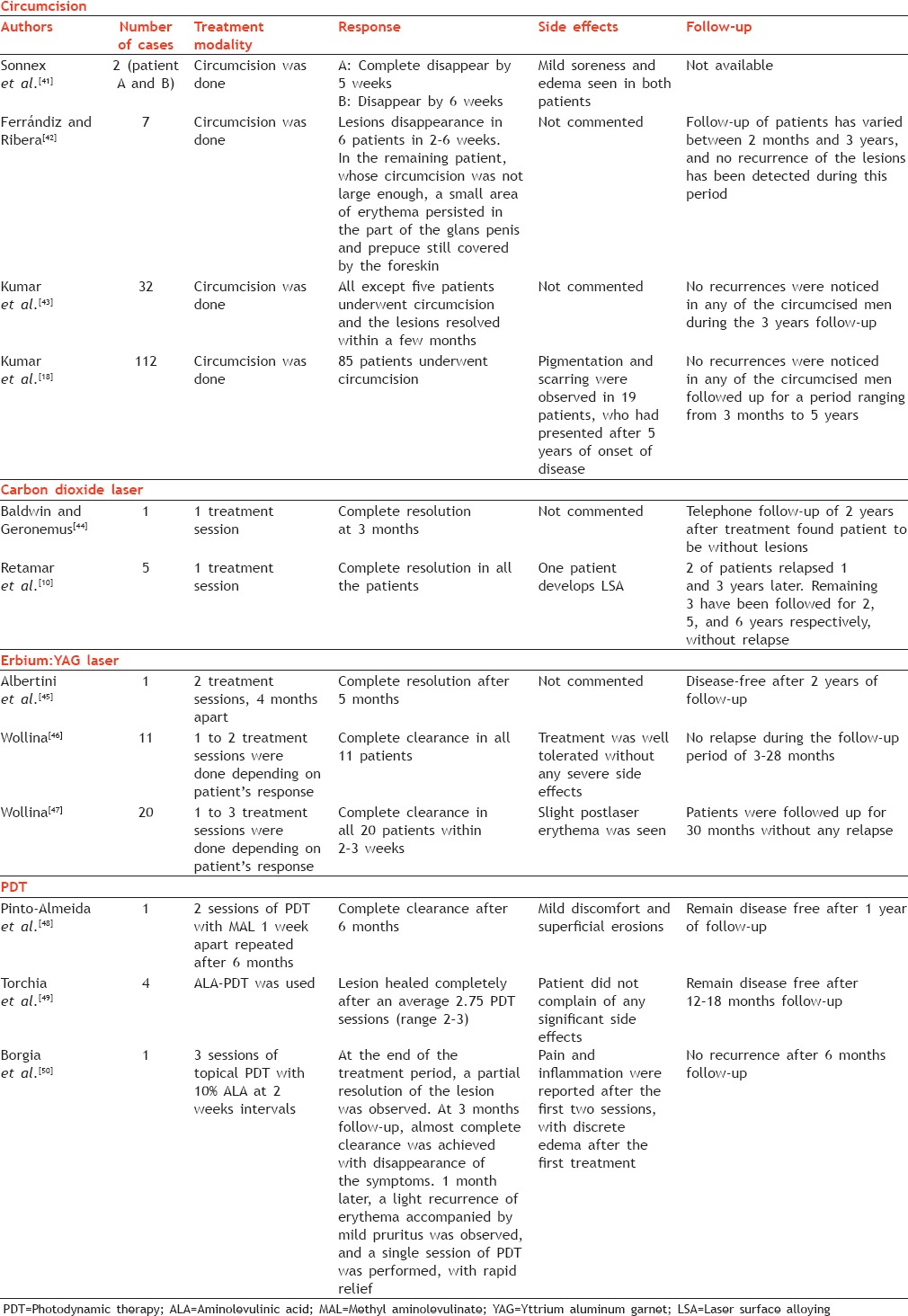
Circumcision is the definite treatment of ZB according to the 2013 European guidelines for the management of balanoposthitis.[17] Circumcision was first recommended as a cure in 1956 by Sutton.[51] Subsequently, this relatively simple but not very popular procedure has been used satisfactorily and the response was reported as excellent according to the various studies.[18,41,42,43] Resolution of symptoms after circumcision might be due to the removal of factors, i.e., chronic irritation, along with constant friction and poor hygiene caused by the overlying prepuce. Some authors have also suggested that aseptic technique applied during circumcision, followed by regular cleaning during healing, might lead to improvement of the condition.[18] It is associated with minimal postoperative side effects such as initial soreness and edema, which get resolved within a week.[18] Most of the earlier studies have reported resolution of lesions of ZB after 6 weeks to few months after circumcision.[18,41,42,43] Thus, it seems to be the treatment of choice for ZB
Carbon dioxide (CO2) laser - There are only two reports showing efficacy of CO2 laser in ZB. First, CO2 laser was used by Baldwin et al.[44] in the defocused mode that is capable of highly precise vaporization of tissue within a small area with negligible transfer of heat energy to the surrounding tissues, resulting in selective damage of the target area. In another study, Retamar et al.[10] had employed CO2 laser using “silk touch” laser technology in their five patients with ZB. The “silk touch” technique has a scanner that spins the laser beam rapidly in a spiral pattern so that each treated point absorbs laser energy during a shorter time than the tissue's thermal relaxation time.[10] This is a well-tolerated procedure and re-epithelialization is achieved in 1–2 weeks without any postsurgical complication. Thus, CO2 laser can be used as a viable alternative and certainly less traumatic surgical therapy for treatment of ZB than circumcision
Erbium (Er):YAG laser - Few studies have reported Er:YAG laser to produce complete resolution in ZB.[45,46,47] Irradiation by Er:YAG laser produces relatively pure ablation with minimal thermal damage. Because ablation is directly proportional to fluence, Er:YAG laser can be finely adapted to this clinical scenario.[47] Thus, it offers a precise superficial ablation with low thermal injury, low risk of scarring, low pain, and rapid healing.[47]
Photodynamic therapy
Recently, photodynamic therapy(PDT) using topical porphyrin precursors, 5-aminolaevulinic acid (ALA) or methyl aminolevulinate (MAL), has been proposed for refractory lesions of ZB.[48,49,52] Till now, its precise mechanism of action is unknown, but it is proposed that the particular sensitivity of activated T-lymphocytes to PDT might induce immunosuppression with subsequent inhibition of cytokines attracting the plasma cells, thus inhibiting the colonization of plasma cells in the dermis. On analyzing the limited data in the literature, ALA-PDT seems to be slightly better than MAL-PDT.[49] In all the cases, the treatment was well-tolerated with no long-term side effects.[48,49,52]
Miscellaneous drugs
Topical fusidic acid 2% cream has also been used in ZB. Fusidic acid shares a similar molecular structure with corticosteroid, thus having both anti-inflammatory and antibiotic activity. According to a study by Petersen et al.,[50] once-daily application of fusidic acid cream for 8–16 weeks had induced both suppression and 6-month cure in 5 of the 8 patients despite an unclear mechanism of action. However, further studies are required to substantiate these findings. Oral dapsone has also been used in resistant lesions of ZB. There is only one case report of ZB treated with oral dapsone without any side effect although the mechanism of action was not clear.[53] Radiotherapy (currently not indicated for this entity), superficial electrodesiccation, cryotherapy, and topical antifungals have been used with little to no improvement.[7,10,42] Griseofulvin therapy has also been tried without success.[54]
Follow-up
The exact follow-up regime for ZB after treatment is still unclear. Although it is described as benign in nature, its association with premalignant conditions such as erythroplasia of Queyrat really puts the clinician in a great dilemma. For erythroplasia of Queyrat, a minimum of 5 years follow-up is recommended.[55] Thus, a logical and standard protocol should be used for ZB also, especially due to its risk of recurrence and risk of malignant transformation. Patients should be followed up for at least 5 years although lifelong follow-up would be better as it will give a precise insight about the natural course of this condition.
CONCLUSION
ZB is not so common clinical entity, but very less attention has been paid in the literature regarding its etiology and management of this peculiar nonvenereal genital dermatosis. Circumcision and recently lasers seems to be viable therapeutic options for its management. Furthermore, a regular careful clinical and histopathological monitoring is definitely required in the management of this complex and demanding entity.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
MULTIPLE-CHOICE QUESTIONS
-
“Cayenne pepper spots” in Zoon balanitis is due to:
- Siderophages and extravasated red blood cells
- Microhemorrhage and hemosiderin deposition
- Changes in dermal vasculature which include vascular dilatation with proliferated individual vessels
- Dense infiltrate of plasma cells at dermoepidermal junction
-
Vulval counterpart of Zoon balanitis, i.e. Zoon's vulvitis, was first described by:
- J.J. Zoon
- Nikolowski
- Garnier
- Kortnig
-
Clinical Criteria for Diagnosing Zoon balanitis includes all of the following except:
- Shiny, erythematous patches on the glans, prepuce, or both
- Presence of lesions for less than 2 months
- Absence of lesions suggestive of LP; psoriasis elsewhere on the body
- Poor response to topical therapies for minimum 4 weeks
-
All are the dermoscopic features of Zoon balanitis except:
- Orange-yellowish structure-less areas
- Convoluted and chalice-shaped vessels
- Scattered glomerular vessels
- Dotted vessels and spermatozoa-like vessels.
-
According to the 2013 European guidelines for management of balanoposthitis, the definitive treatment of ZB is:
- CO2 laser
- Topical tacrolimus 0.1% ointment
- Circumcision
- Dorsal split of prepuce
ANSWERS
(b).
(c)
(b)
(c)
(c)
REFERENCES
- 1.Cooper SM, Wojnarowska F. Anogenital (nonvenereal) disease. In: Bolognia JL, Jorizzo JL, Schaffer JV, editors. Dermatology. 3rd ed. United States: Elsevier; 2012. pp. 1171–86. [Google Scholar]
- 2.Tang A, David N, Horton LW. Plasma cell balanitis of Zoon: Response to Trimovate cream. Int J STD AIDS. 2001;12:75–8. doi: 10.1258/0956462011916811. [DOI] [PubMed] [Google Scholar]
- 3.Zoon JJ. Chronic benign circumscript plasmocytic balanoposthitis. Dermatologica. 1952;105:1–7. [PubMed] [Google Scholar]
- 4.Garnier G. Benign plasma cell erythroplasia. Br J Dermatol. 1982;106:585–8. doi: 10.1111/j.1365-2133.1957.tb13232.x. [DOI] [PubMed] [Google Scholar]
- 5.Nikolowski W, Wiehl R. Pareiitis und balanitis plasmacellularis. Arch Klin Exp Dermatol. 1956;202:347–57. [PubMed] [Google Scholar]
- 6.Korting GW, Theisen H. Circumscribed plasma cell balanoposthitis and conjunctivitis in the same patient. Arch Klin Exp Dermatol. 1963;217:495–504. [PubMed] [Google Scholar]
- 7.Mallon E, Hawkins D, Dinneen M, Francics N, Fearfield L, Newson R, et al. Circumcision and genital dermatoses. Arch Dermatol. 2000;136:350–4. doi: 10.1001/archderm.136.3.350. [DOI] [PubMed] [Google Scholar]
- 8.Pearce J, Fernando I. The value of a multi-specialty service, including genitourinary medicine, dermatology and urology input, in the management of male genital dermatoses. Int J STD AIDS. 2015;26:716–22. doi: 10.1177/0956462414552695. [DOI] [PubMed] [Google Scholar]
- 9.Porter WM, Bunker CB. The dysfunctional foreskin. Int J STD AIDS. 2001;12:216–20. doi: 10.1258/0956462011922922. [DOI] [PubMed] [Google Scholar]
- 10.Retamar RA, Kien MC, Chouela EN. Zoon's balanitis: Presentation of 15 patients, five treated with a carbon dioxide laser. Int J Dermatol. 2003;42:305–7. doi: 10.1046/j.1365-4362.2003.01304.x. [DOI] [PubMed] [Google Scholar]
- 11.Pastar Z, Rados J, Lipozencic J, Skerlev M, Loncaric D. Zoon plasma cell balanitis: An overview and role of histopathology. Acta Dermatovenerol Croat. 2004;12:268–73. [PubMed] [Google Scholar]
- 12.Kiene P, Fölster-Holst R. No evidence of human papillomavirus infection in balanitis circumscripta plasmacellularis Zoon. Acta Derm Venereol. 1995;75:496–7. doi: 10.2340/0001555575496497. [DOI] [PubMed] [Google Scholar]
- 13.Weyers W, Ende Y, Schalla W, Diaz-Cascajo C. Balanitis of Zoon: A clinicopathologic study of 45 cases. Am J Dermatopathol. 2002;24:459–67. doi: 10.1097/00000372-200212000-00001. [DOI] [PubMed] [Google Scholar]
- 14.Kossard S, Shumack S. Lichen aureus of the glans penis as an expression of Zoon's balanitis. J Am Acad Dermatol. 1989;21:804–6. doi: 10.1016/s0190-9622(89)80278-6. [DOI] [PubMed] [Google Scholar]
- 15.Nishimura M, Matsuda T, Muto M, Hori Y. Balanitis of Zoon. Int J Dermatol. 1990;29:421–3. doi: 10.1111/j.1365-4362.1990.tb03826.x. [DOI] [PubMed] [Google Scholar]
- 16.Hyman AB, Leider M. Erythroplasia of the female genitalia. Report of two cases of a benign from (plasmacytosis pudendi) Arch Dermatol. 1961;84:381–5. doi: 10.1001/archderm.1961.01580150027004. [DOI] [PubMed] [Google Scholar]
- 17.Edwards SK, Bunker CB, Ziller F, van der Meijden WI. 2013 European guideline for the management of balanoposthitis. Int J STD AIDS. 2014;25:615–26. doi: 10.1177/0956462414533099. [DOI] [PubMed] [Google Scholar]
- 18.Kumar B, Narang T, Dass Radotra B, Gupta S. Plasma cell balanitis: Clinicopathologic study of 112 cases and treatment modalities. J Cutan Med Surg. 2006;10:11–5. doi: 10.1007/7140.2006.00008. [DOI] [PubMed] [Google Scholar]
- 19.Adégbidi H, Atadokpèdé F, Dégboé B, Saka B, Akpadjan F, Yédomon H, et al. Zoon's balanitis in circumcised and HIV infected man, at Cotonou (Benin) Bull Soc Pathol Exot. 2014;107:139–41. doi: 10.1007/s13149-014-0359-4. [DOI] [PubMed] [Google Scholar]
- 20.Schuermann H. Plasmocytosis circumorificialis. Dtsch Zahnärztl Z. 1960;15:601–7. [Google Scholar]
- 21.White JW, Jr, Olsen KD, Banks PM. Plasma cell orificial mucositis. Report of a case and review of the literature. Arch Dermatol. 1986;122:1321–4. doi: 10.1001/archderm.122.11.1321. [DOI] [PubMed] [Google Scholar]
- 22.Starritt E, Lee S. Erythroplasia of Queyrat of the glans penis on a background of Zoon's plasma cell balanitis. Australas J Dermatol. 2008;49:103–5. doi: 10.1111/j.1440-0960.2008.00440.x. [DOI] [PubMed] [Google Scholar]
- 23.Joshi UY. Carcinoma of the penis preceded by Zoon's balanitis. Int J STD AIDS. 1999;10:823–5. doi: 10.1258/0956462991913484. [DOI] [PubMed] [Google Scholar]
- 24.Divakaruni AK, Rao AV, Mahabir B. Erythroplasia of Queyrat with Zoon's balanitis: A diagnostic dilemma. Int J STD AIDS. 2008;19:861–3. doi: 10.1258/ijsa.2007.007171. [DOI] [PubMed] [Google Scholar]
- 25.Arzberger E, Komericki P, Ahlgrimm-Siess V, Massone C, Chubisov D, Hofmann-Wellenhof R. Differentiation between balanitis and carcinoma in situ using reflectance confocal microscopy. JAMA Dermatol. 2013;149:440–5. doi: 10.1001/jamadermatol.2013.2440. [DOI] [PubMed] [Google Scholar]
- 26.Errichetti E, Lacarrubba F, Micali G, Stinco G. Dermoscopy of Zoon's plasma cell balanitis. J Eur Acad Dermatol Venereol. 2015 doi: 10.1111/jdv.13538. http://www.doi.org//10.1111/jdv.13538. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 27.Yoganathan S, Bohl TG, Mason G. Plasma cell balanitis and vulvitis (of Zoon).A study of 10 cases. J Reprod Med. 1994;39:939–44. [PubMed] [Google Scholar]
- 28.Santos-Juanes J, Sánchez del Río J, Galache C, Soto J. Topical tacrolimus: An effective therapy for Zoon balanitis. Arch Dermatol. 2004;140:1538–9. doi: 10.1001/archderm.140.12.1538. [DOI] [PubMed] [Google Scholar]
- 29.Hernandez-Machin B, Hernando LB, Marrero OB, Hernandez B. Plasma cell balanitis of Zoon treated successfully with topical tacrolimus. Clin Exp Dermatol. 2005;30:588–9. doi: 10.1111/j.1365-2230.2005.01806.x. [DOI] [PubMed] [Google Scholar]
- 30.Moreno-Arias GA, Camps-Fresneda A, Llaberia C, Palou-Almerich J. Plasma cell balanitis treated with tacrolimus 0.1% Br J Dermatol. 2005;153:1204–6. doi: 10.1111/j.1365-2133.2005.06945.x. [DOI] [PubMed] [Google Scholar]
- 31.Hague J, Ilchyshyn A. Successful treatment of Zoon's balanitis with topical tacrolimus. Int J Dermatol. 2006;45:1251–2. doi: 10.1111/j.1365-4632.2006.02934.x. [DOI] [PubMed] [Google Scholar]
- 32.Roé E, Dalmau J, Peramiquel L, Pérez M, López-Lozano HE, Alomar A. Plasma cell balanitis of zoon treated with topical tacrolimus 0.1%: Report of three cases. J Eur Acad Dermatol Venereol. 2007;21:284–5. doi: 10.1111/j.1468-3083.2006.01857.x. [DOI] [PubMed] [Google Scholar]
- 33.Kyriakou A, Patsatsi A, Patsialas C, Sotiriadis D. Therapeutic efficacy of topical calcineurin inhibitors in plasma cell balanitis: Case series and review of the literature. Dermatology. 2014;228:18–23. doi: 10.1159/000357153. [DOI] [PubMed] [Google Scholar]
- 34.Bardazzi F, Antonucci A, Savoia F, Balestri R. Two cases of Zoon's balanitis treated with pimecrolimus 1% cream. Int J Dermatol. 2008;47:198–201. doi: 10.1111/j.1365-4632.2008.03392.x. [DOI] [PubMed] [Google Scholar]
- 35.Stinco G, Piccirillo F, Patrone P. Discordant results with pimecrolimus 1% cream in the treatment of plasma cell balanitis. Dermatology. 2009;218:155–8. doi: 10.1159/000161119. [DOI] [PubMed] [Google Scholar]
- 36.Delgado L, Brandt HR, Ortolan DG, Patriota RC, Criado PR, Belda Junior W. Zoon's plasma cell balanitis: A report of two cases treated with pimecrolimus. An Bras Dermatol. 2011;86(4 Suppl 1):S35–8. doi: 10.1590/s0365-05962011000700008. [DOI] [PubMed] [Google Scholar]
- 37.Nasca MR, De Pasquale R, Micali G. Treatment of Zoon's balanitis with imiquimod 5% cream. J Drugs Dermatol. 2007;6:532–4. [PubMed] [Google Scholar]
- 38.Marconi B, Campanati A, Simonetti O, Savelli A, Conocchiari L, Santinelli A, et al. Zoon's balanitis treated with imiquimod 5% cream. Eur J Dermatol. 2010;20:134–5. doi: 10.1684/ejd.2010.0829. [DOI] [PubMed] [Google Scholar]
- 39.Niwa Y, Terashima T, Sumi H. Topical application of the immunosuppressant tacrolimus accelerates carcinogenesis in mouse skin. Br J Dermatol. 2003;149:960–7. doi: 10.1111/j.1365-2133.2003.05735.x. [DOI] [PubMed] [Google Scholar]
- 40.Bunker CB, Neill S, Staughton RC. Topical tacrolimus, genital lichen sclerosus, and risk of squamous cell carcinoma. Arch Dermatol. 2004;140:1169. doi: 10.1001/archderm.140.9.1169-a. [DOI] [PubMed] [Google Scholar]
- 41.Sonnex TS, Dawber RP, Ryan TJ, Ralfs IG. Zoon's (plasma-cell) balanitis: Treatment by circumcision. Br J Dermatol. 1982;106:585–8. doi: 10.1111/j.1365-2133.1982.tb04563.x. [DOI] [PubMed] [Google Scholar]
- 42.Ferrándiz C, Ribera M. Zoon's balanitis treated by circumcision. J Dermatol Surg Oncol. 1984;10:622–5. doi: 10.1111/j.1524-4725.1984.tb01266.x. [DOI] [PubMed] [Google Scholar]
- 43.Kumar B, Sharma R, Rajagopalan M, Radotra BD. Plasma cell balanitis: Clinical and histopathological features – Response to circumcision. Genitourin Med. 1995;71:32–4. doi: 10.1136/sti.71.1.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Baldwin HE, Geronemus RG. The treatment of Zoon's balanitis with the carbon dioxide laser. J Dermatol Surg Oncol. 1989;15:491–4. doi: 10.1111/j.1524-4725.1989.tb03407.x. [DOI] [PubMed] [Google Scholar]
- 45.Albertini JG, Holck DE, Farley MF. Zoon's balanitis treated with Erbium: YAG laser ablation. Lasers Surg Med. 2002;30:123–6. doi: 10.1002/lsm.10037. [DOI] [PubMed] [Google Scholar]
- 46.Wollina U. Erbium-YAG-laser treatment of balanoposthitis chronica circumscripta benigna plasmacellularis Zoon. Med Laser Appl. 2006;21:23–6. [Google Scholar]
- 47.Wollina U. Ablative erbium: YAG laser treatment of idiopathic chronic inflammatory non-cicatricial balanoposthitis (Zoon's disease) – A series of 20 patients with long-term outcome. J Cosmet Laser Ther. 2010;12:120–3. doi: 10.3109/14764171003706125. [DOI] [PubMed] [Google Scholar]
- 48.Pinto-Almeida T, Vilaça S, Amorim I, Costa V, Alves R, Selores M. Complete resolution of Zoon balanitis with photodynamic therapy – A new therapeutic option? Eur J Dermatol. 2012;22:540–1. doi: 10.1684/ejd.2012.1779. [DOI] [PubMed] [Google Scholar]
- 49.Borgia F, Vaccaro M, Foti A, Giuffrida R, Cannavò SP. Zoon's balanitis successfully treated with photodynamic therapy: Case report and literature review. Photodiagnosis Photodyn Ther. 2016;13:347–9. doi: 10.1016/j.pdpdt.2015.08.010. [DOI] [PubMed] [Google Scholar]
- 50.Petersen CS, Thomsen K. Fusidic acid cream in the treatment of plasma cell balanitis. J Am Acad Dermatol. 1992;27:633–4. doi: 10.1016/s0190-9622(08)80206-x. [DOI] [PubMed] [Google Scholar]
- 51.Sutton RL. Non-venereal diseases of male genitalia. 11th ed. St. Louis: CV Mosby; 1956. Diseases of the skin; pp. 894–8. [Google Scholar]
- 52.Torchia D, Cappugi P. Photodynamic therapy for Zoon balanitis. Eur J Dermatol. 2014;24:707. doi: 10.1684/ejd.2014.2439. [DOI] [PubMed] [Google Scholar]
- 53.Mahajan BB, Mehta V. Zoon's balanitis: Treated successfully with dapsone. Indian J Sex Transm Dis. 2005;26:91. [Google Scholar]
- 54.Gerbig AW, Hunziker T. Griseofulvin ineffective in balanitis circumscripta plasmacellularis. J Am Acad Dermatol. 1995;33:319. doi: 10.1016/0190-9622(95)90271-6. [DOI] [PubMed] [Google Scholar]
- 55.Shabbir M, Minhas S, Muneer A. Diagnosis and management of premalignant penile lesions. Ther Adv Urol. 2011;3:151–8. doi: 10.1177/1756287211412657. [DOI] [PMC free article] [PubMed] [Google Scholar]


