Abstract
HIV/AIDS-related immune alteration poses many diagnostic and therapeutic challenges. HIV-positive 44-year-old male, on second-line antiretroviral therapy (ART) presented with asymptomatic non healing, well-defined, erythematous ulcer over penis since 8 months with serosanguinous discharge. Inguinal lymph nodes were not palpable. Tzanck smear was negative. Biopsy was not done as the patient was not willing for the same. Acyclovir was given considering herpes infection to which there was no response, and hence azithromycin and metronidazole were given, without improvement. Minocycline was given to take care of possible atypical mycobacterial infection. Due to lack of response, corticosteroid was given for 2 weeks keeping in mind possibility of vasculitis, but there was no improvement. Although investigations to rule out tuberculous etiology were negative, empirical anti-Koch's therapy Category 2 was given without response even after 3 months. Finally, a biopsy was taken from lesion which was suggestive of donovanosis. Trimethoprim Sulfamethoxazole in higher dose was started to which he responded after 2 weeks, and therapy was continued till complete response. Patient is on second-line ART for last 7 years. He is clinically stable, but his CD4 count is hovering at around 250–300 suggestive of ART failure. Virological evaluation was not feasible. Diagnostic challenges posed include possibility of resistant bacterial, viral infection, vasculitis, or drug reaction in a setting of probable ART failure.
Key words: HIV/AIDS, nonhealing genital ulcer, response to co-trimoxazole
INTRODUCTION
HIV/AIDS-related immune alteration poses many diagnostic and therapeutic challenges in cases having sexually acquired penile ulceration. Clinical diagnosis has to be corroborated with microbiological findings and serology. In case ulcerations do not respond to antibiotic as well as antiviral therapy, tuberculosis and vasculitis need to be ruled out. Biopsy becomes essential. In nonresponders, drug resistance may be a possibility and older antimicrobials such as Co-trimoxazole now not used conventionally for the treatment of sexually transmitted disease (STD) can be considered if the etiology is established.
CASE REPORT
A 44-year-old married male, an accountant by profession, with AIDS since 2003, who was started on ART Category 2 (tenofovir, lamivudine, atazanavir, and ritonavir) since 2007 presented to our outpatient department with complaints of penile ulcer since 8 months. It started as nodules over the shaft of penis, breaking down to form an ulcer which was initially small in size and progressed to the current size over a period of 8 months. He did not complain of pain or itching. There was a history of serosanguinous discharge from the ulcer. On questioning, he gave a history of unprotected extramarital sexual contact 1 year ago. He also had a history of pulmonary tuberculosis 10 years ago for which anti-Koch's therapy (AKT) Category 1 was taken for 6 months. He had no history of similar lesions or blood transfusion in the past. His wife was HIV negative.
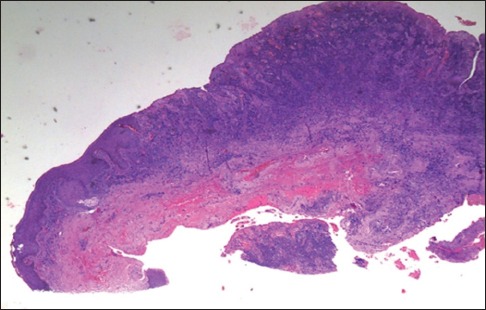
General and systemic examination was within normal limits. Genital examination revealed a non healing, well-defined, erythematous ulcer over shaft of penis with serosanguinous discharge [Figure 1]. Inguinal lymph nodes were not palpable. The perianal region was normal.
Figure 1.

Pretreatment
On investigation, hemogram was normal. Patient was HIV positive with CD4 count of 233 cells/cmm of blood. HIV viral load was not done (due to lack of resources). Venereal disease research laboratory was nonreactive. Hepatitis B surface antigen and Hepatitis C virus were negative; herpes serology was negative. Ultrasound abdomen was within normal limits. Tzanck smear for multinucleated giant cells and crush smear done for donovanosis were negative. Biopsy was not taken as patient was reluctant for the same.
The differential diagnosis considered were herpes progenitalis and granuloma inguinale (GI). As herpes progenitalis is the most common cause of genital ulcer in AIDS patient and manifestations are protean and diverse, we considered herpes as the first diagnosis and started Acyclovir.[1]
Acyclovir 400 mg thrice a day was given for 1 week, but there was no improvement of ulcer, so azithromycin 500 mg 1 OD for 14 days given considering GI. On follow-up, there was no response, so an attempt was made to rule out tuberculosis. Chest X-ray and Mantoux test were done; acid-fast bacilli culture was also done from growth, but all were negative. Empirical AKT Category 2 (isoniazid, rifampicin, ethambutol, pyrazinamide along with streptomycin) was given for 3 months, also tablet Minocycline 100 mg BD for 15 days. No improvement on follow-up prompted us to consider vasculitis for which tablet methylprednisolone 24 mg/day was given for 2 weeks.
Finally, when the ulcer did not yield to any of the above drugs, patient consented for biopsy. Histopathology revealed diffuse dense lymphoplasmacytic infiltrate on a background of granulation tissue with a few large histiocytes containing coccobacilli. Small foci of neutrophilic collection were seen within the dermis, and Giemsa stain was positive for Donovan bodies which is considered the gold standard for diagnosis of donovanosis [Figures 2 and 3].[2]
Figure 2.
Lymphoplasmacytic infiltrate, granulation tissue in dermis (histopathology, ×10)
Figure 3.
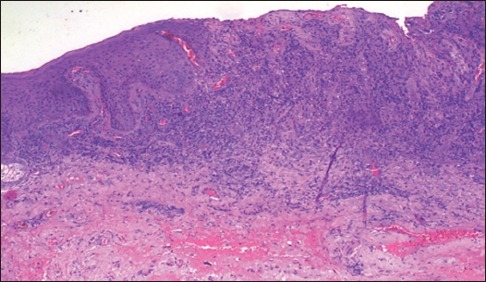
Histiocytes containing coccobacilli, neutrophils in dermis. Giemsa stain positive for Donovan bodies (histopathology, ×10)
As patient had already received Azithromycin, Streptomycin, and Minocycline, he was started on Injection Gentamycin 80 mg IV OD plus Azithromycin 500 mg 1 OD for 15 days. When he did not respond, Co-trimoxazole (800 mg Sulfamethoxazole and 160 mg Trimethoprim) was given in higher dose, three times a day, presuming that this may take care of possible drug resistance.
After 2 weeks, patient started responding to high-dose Co-trimoxazole [Figures 4–6] which was continued till complete healing which took 2 months.
Figure 4.

Two weeks follow-up after starting co-trimoxazole
Figure 6.

Two months after starting co-trimoxazole-posttreatment
Figure 5.

Four weeks follow-up after starting co-trimoxazole
DISCUSSION
AIDS patient having genital ulcer not responding to different therapeutic modalities need thorough investigation (serology, microbiology, and biopsy) to come to a precise diagnosis.
In most cases, donovanosis is obvious clinically, but for its confirmation, the demonstration of Donovan bodies in histological sections and cytological preparation is essential.[3]
In the case discussed, smear for Donovan bodies was negative, but as per a study done by Ganguly et al., out of 26 biopsy-proven cases of donovanosis, only ten were smear positive.[4] Cleaning of genital ulcer with topical antimicrobials is a usual practice and may be the reason for smear negativity. Our patient was initially reluctant for biopsy, but nonresponsive to antiviral, antibiotic, AKT, and systemic steroid compelled him to give consent for biopsy.
In spite of having laboratory supported diagnosis, when patient failed to respond to all recommended treatment for GI such as Azithromycin, Minocycline, Streptomycin, Gentamycin, drug resistance was suspected.
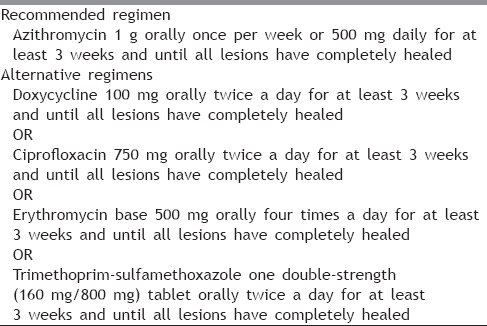
In a report by Manior and Desai, HIV-positive patients with Donovanosis had high failure rate to first-line antibiotic therapy.[6,7] As patient had already received the other recommended drugs, Co-trimoxazole was started in high dose suspecting drug resistance, to which he started responding after 2 weeks, and the treatment was continued till complete response, almost for a period of 2 months [Table 1].
Table 1.
The CDC 2015 guidelines for treatment of donovanosis[5]
According to a study conducted in Mumbai, the mean healing time in HIV-positive patients with Donovanosis was 25.7 days compared to 16.8 days in HIV-negative subjects.[8]
There is a paucity of date on HIV-related GI and further clarification of the role of Azithromycin in the management of Donovanosis in HIV-positive patients is awaited.[9]
CONCLUSION
Manifestations of ulcerative STDs are diverse and varied in AIDS cases, and clinical diagnosis may not correlate with underlying etiology. In AIDS patient with nonhealing genital ulcer, thorough Investigation is the key to precise diagnosis and facilitates etiology-based drug therapy. In the case under discussion, biopsy settled the final diagnosis.
In such cases, response to recommended drug may not be achieved and hence, possibility of drug resistance must be kept in mind. No response to Azithromycin, Aminoglycosides, Minocycline, and complete response to high-dose Co-trimoxazole therapy suggest possible resistance to those antimicrobials on clinical ground.
Limitation of the study
Culture and antibiotic sensitivity pattern could not be done on feasibility ground.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Bhavsar C, Patel RM, Marfatia Y. A study of 113 cases of genital ulcerative disease and urethral discharge syndrome with validation of syndromic management of sexually transmitted diseases. Indian J Sex Transm Dis. 2014;35:35–9. doi: 10.4103/2589-0557.132426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rajam RV, Rangiah PN. Donovanosis; granuloma inguinale, granuloma venereum. Monogr Ser World Health Organ. 1954;24:1–72. [PubMed] [Google Scholar]
- 3.Agrawal M, Arora SK, Agarwal A. A forgotten disease reminds itself with a rare complication. Indian J Dermatol. 2011;56:430–1. doi: 10.4103/0019-5154.84752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ganguly DD, Sundharam JA, Bhargava NC, Nayar M, Chandra M, Saxena HM. A clinicopathological study of donovanosis. Indian J Dermatol Venereol Leprol. 1983;49:205–9. [PubMed] [Google Scholar]
- 5.The Centers for Disease Control and Prevention (CDC, 2015) [Last accessed on 2016 Sep 04]. Available from: http://www.cdc.gov/std/tg2015/donovanosis.htm .
- 6.Veeranna S, Raghu TY. A clinical and investigational study of donovanosis. Indian J Dermatol Venereol Leprol. 2003;69:159–62. [PubMed] [Google Scholar]
- 7.Manior 1K, Desai V. GUD and HIV status correlation in Bomb presented at 8' int conf. On AIDS. Adstract 3512, Amsterdam. 1992 [Google Scholar]
- 8.Jamkhedkar PP, Hira SK, Shroff HJ, Lanjewar DN. Clinico-epidemiologic features of granuloma inguinale in the era of acquired immune deficiency syndrome. Sex Transm Dis. 1998;25:196–200. doi: 10.1097/00007435-199804000-00004. [DOI] [PubMed] [Google Scholar]
- 9.NIgel O'Farell. Donovanosis. In: Kumar B, Gupta S, editors. Sexually transmitted infections. 2nd ed. New Delhi: Elsevier; 2011. p. 536. [Google Scholar]


