Sir,
Human papilloma virus is the most common sexually transmitted infection (STI) worldwide and genital warts are a manifestation of infection by this virus.[1] There are multiple treatment options available depending on the number and location of lesions, response to previous treatments, local availability of the medications, cost, and patient's wishes. For fewer lesions, and in compliant patients, topical therapy such as podofilox solution or imiquimod works well. But these have a long response time and if applied incorrectly can cause damage. Destructive modalities such as cryotherapy and electrofulguration [2] have the advantage of rapid response, but in cases of extensive lesions, these may have to be done in a phased manner to avoid patient trauma and mutilation.
Circumcision as treatment for genital warts is rarely resorted to as most of the cases respond to conventional modes of treatment. But in cases where the lesions have extensive involvement of the prepuce, and the other modalities have failed or caused harm, it can be employed with good results. We treated three cases of genital warts which were resistant to the usual line of management and were treated by circumcision with excellent clinical outcome.
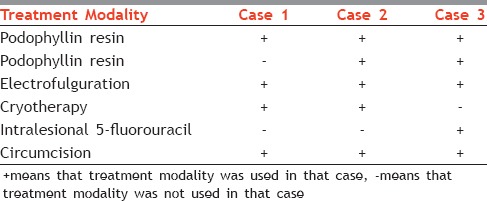
Three males in their third decade of life presented to us with similar complaints of multiple, skin colored, nonitchy, painless lesions over penis of few months duration. There was no history suggestive of any other STI. Their general and systemic examinations was normal. Dermatological examination revealed multiple skin colored verrucous papules distributed circumferentially over prepuce [Figure 1a]. Laboratory evaluation was negative for HIV, herpes simplex virus 1 and 2 IgM, hepatitis B antigen, antihepatitis C virus – IgM, and Venereal Disease Research Laboratory. All these patients had been managed previously with the conventional treatment modalities as described above with partial clinical response and recurrence. Based on this and the favorable location of the lesions, they were managed by circumcision by dorsal slit technique [Figure 1b and c]. There were no postoperative complications, and the patients have remained disease free after 6 months [Figure 1d]. Treatment details of the patients have been presented in Table 1.
Figure 1.
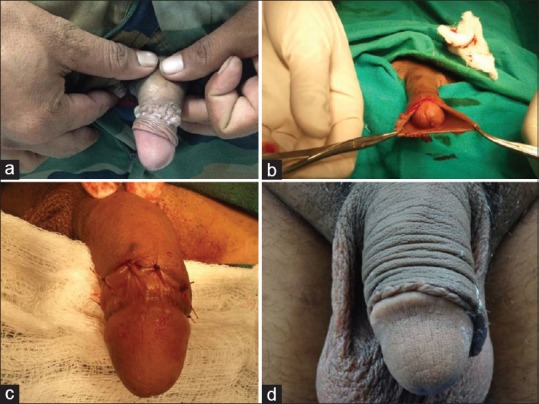
(a) Circumferential genital warts, (b) circumcision by dorsal slit technique, (c) postoperative photograph, (d) follow-up at 6 months
Table 1.
Treatment modalities used
Genital warts have a long array of treatment options, ranging from medical to surgical. The primary treatment hurdle is the failure of therapy or recurrence of lesions. Circumcision as a treatment modality is not mentioned as an option.
About one-third of males worldwide are circumcised. The reasons are mostly religious, personal preferences, or for certain therapeutic or prophylactic indications. It has been found to protect against HIV infection, urinary tract infections, and ulcerative STI's if done at appropriate times.[3] It has also been associated with reduced oncogenic HPV prevalence and risk of penile cancer.[4]
Apart from the psychological aspects, extensive genital warts on prepuce can cause discomfort during sexual intercourse, bleeding, ulceration, or even phimosis in severe cases. The treatment itself can cause scarring and phimosis if used incorrectly or aggressively. Circumcision is a good option for patients with extensive prepucial involvement, especially with a history of persistence or recurrence.[5]
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Centre for Disease Control and Prevention. Genital HPV Infection – Fact Sheet. [Last accessed on 2014 Sep 20; Last updated on 2014 Mar 20]. Available from: http://www.cdc.gov/std/hpv/stdfact-hpv.htm .
- 2.Summary of the 2012 CDC Sexually Transmitted Diseases (STD) Treatment Guidelines New Hampshire Infectious Disease Prevention, Investigation and Care Services Section. [Last accessed on 2014 Sep 20]. Available from: http://www.dermakuwait.com/Summary_STDs_tt_Guidelines_2010 .
- 3.Yanofsky VR, Patel RV, Goldenberg G. Genital warts: A comprehensive review. J Clin Aesthet Dermatol. 2012;5:25–36. [PMC free article] [PubMed] [Google Scholar]
- 4.Albero G, Castellsagué X, Giuliano AR, Bosch FX. Male circumcision and genital human papillomavirus: A systematic review and meta-analysis. Sex Transm Dis. 2012;39:104–13. doi: 10.1097/OLQ.0b013e3182387abd. [DOI] [PubMed] [Google Scholar]
- 5.Dogra S, Kumar B. Circumcision in genital warts – Let us not forget! Sex Transm Infect. 2003;79:265. doi: 10.1136/sti.79.3.265. [DOI] [PMC free article] [PubMed] [Google Scholar]


