Abstract
Background
Primary hyperparathyroidism is caused by the excessive growth of parathormone secretion, its consequence being hypercalcemia. The parathyroid adenoma is responsible for over half of primary hyperparathyroidism cases. The mandibular tumor can be the initial sign in the case of primary hyperparathyroidism.
Case presentation
We present the case of a 33 year old patient with history of a mandibular operated tumor, repetitive pathological fractures and hypercalcemia manifestations. The level of the parathormone at the first measurement indicated a very high value. The parathyroid scintigraphy with 99mTc-MIBI (methoxy-isobutyl-isonitrile) evidenced a high uptake of the tracerin the superior mediastinum, suggestive for an ectopic parathyroid adenoma. The histopathological examination after surgery leads to the diagnosis of parathyroid adenoma.
The association between the primary hyperparathyroidism, the mandibular tumour, the clinical history and the nuclear imaging lead to the diagnosis of primary hyperparathyroidism – Jaw tumor syndrome.
Conclusion
The hyperparathyroidism - Jaw tumor syndrome has a special clinical importance because of the severe and progressive symptomatology, and because of the risk of developing neoplasia of parathyroid glands, which have a reserved prognosis.
Keywords: primary hyperparathyroidism, jaw tumor, bone scan, 99m Tc-MIBI
Background
The most frequent cause of hypercalcemia in the general population is primary hyperparathyroidism, produced through an excessive parathormone secretion by one or more pathologic parathyroid glands [1,2]. In about 80% of cases it is produced by a parathyroid adenoma, confirmed after surgery by a histopathological examination.
It may be associated to a familial endocrinopathy, for example: MEN 1, MEN 2 [3–5].
It is more frequent in female patients, in the fifth decade of life. The association between chronic hypercalcemia and clinical manifestations in bones and kidneys, and non-specific symptoms (digestive, neuromuscular, psychiatric) led us to the diagnosis of primary hyperparathyroidism [6]. In a small number of cases, especially in young patients in the third decade of life, the first manifestation can be the emergence of bone tumors, the most frequent being mandibular tumors [7,8].
The nuclear medicine imaging - especially the parathyroid scintigraphy with 99mTc-MIBI (methoxy-isobutyl-isonitrile)- has an important role in outlining the diagnosis, being the chosen examination for the imaging representation of the parathyroid metabolism [9–11].
We present the case of a 33-year-old woman with chronic hypercalcemia, bone manifestations (resected mandibular tumor and bone fractures) in which the parathyroid scintigraphy evidenced an increased uptake in the superior mediastinum - an ectopic hyperfunctional parathyroid adenoma; there were skeleton lesions seen on bone scintigraphy. The histopathological examination after surgical removal describes the existence of anatypical parathyroid adenoma.
Case Report
A 33-year-old woman with personal pathologic history of acute right salpingo-oophoritis and giant cells granuloma of the right mandible, operated in 2010 - excision of tumor, right mandibular hemiresection with reconstruction, is hospitalized two years later in the orthopaedic - traumatology department for the treatment of left femur and right humerus fracture sites, after a minor trauma. The patient underwent fracture osteosynthesis and was discharged with the diagnostic of disseminated genital neoplasm (not confirmed on initial histology) with multiple bone metastases; pathological bone fractures; the treatment consisted only in pain therapy and palliative care.
At discharge, the patient has the tumor markers tested: carcinoembryonic antigen CA 15.3 was 5.90 IU/mL (N.V.<31.3 IU/mL) and CA 19.9 was 0.12 IU/mL (N.V.<37 IU/mL).
Shortly afterwards the patient is hospitalized in the endocrinology clinic for asthenia, diffuse bone pain, constipation, depression, muscle fasciculation; the patient was completely immobilized and a possible primary hyperparathyroidism, was suspected.
The patient was sent to the Institute of Oncology in Cluj, where she was indicated a parathyroid scan and a bone scintigraphy. The serum parathormone (PTH) had extremely high values – 2112.90 pg/mL (N.V.<65 pg/mL).
The laboratory analysis pointed out a continuous growing PTH 2194 pg/mL in a second sample at 24h, ionic calcium 7.57 mg/dL (N.V. 3.82–4.82 mg/dL) and serum calcium 17.2 mg/dL (N.V. 8.6–10.2 mg/dL), values that fit into the pathology.
The cervical echography reveals a normal thyroid aspect, with no pathologic findings.
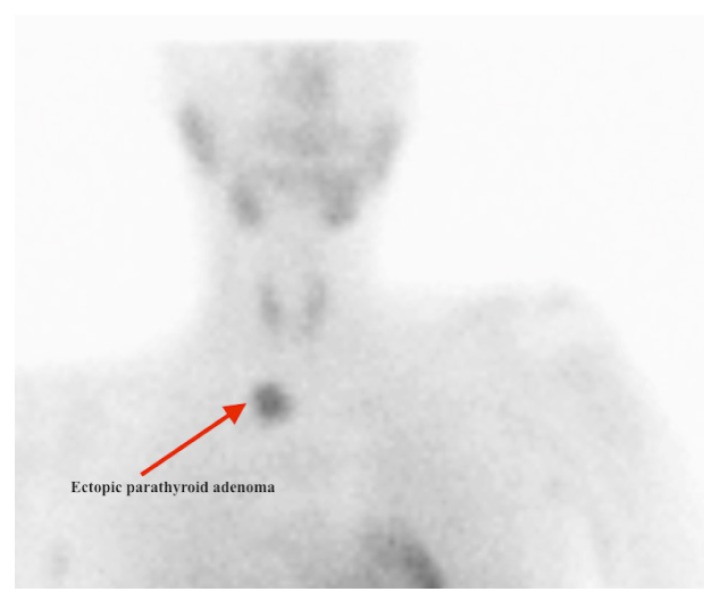
The patient was submitted for a parathyroid scintigraphy with a specific tracer, 99mTc-MIBI (methoxy-isobutyl-isonitrile) - Figure 1 - and a bone scintigraphy, Figure 2.
Figure 1.
Parathyroid scintigraphy with 99mTc-MIBI. Ectopic parathyroid macroadenoma in the superior mediastinum.
Figure 2.
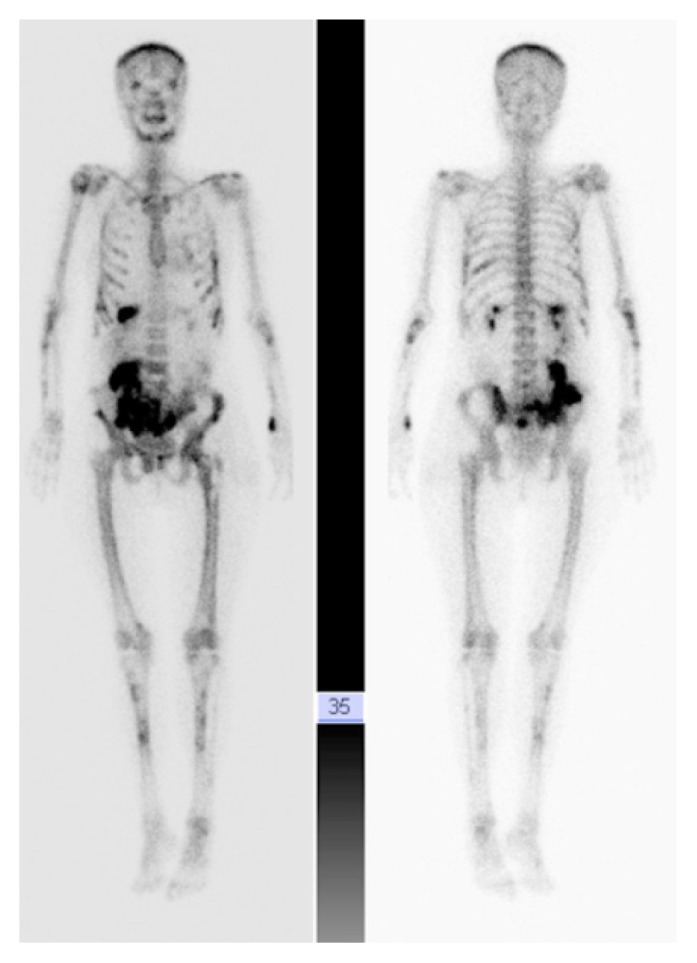
Bone scan 99mTc-MDP; multiple bone lesions.
The parathyroid scan was performed on a Siemens Ecam-Signature gamma camera; planar imaging of the neck and thorax was recorded starting 15 min and then 2–3 h after the intravenous injection of 99mTc- MIBI (approximately 740 MBq [20 mCi]), using a low energy high-resolution collimator. The scan is considered positive for parathyroid disease when an area of increased uptake that persists on late imaging is found. In our case the parathyroid scintigraphy emphasizes the existence of a pathologic uptake due to a macronodule of 25/22 mm, in the superior mediastinum, expression of an ectopic parathyroid tissue with high metabolism.
The bone scintigraphy performed on the same equipment with 99mTc-methylen diphosphonate (99mTc-MDP), 720 MBq at three hours emphasizes a highly modified pathological uptake on skeleton, with a pathological high metabolic activity at the spine, both humerus, bilateral femoral, tibiae and ribs levels, scintigraphic signs suggesting a complicated hyperparathyroidism and bone fractures.
For the first time, the discussions led to the diagnostic of primary hyperparathyroidism - Jaw tumor syndrome, after the imaging investigations.
Surgery was indicated for the excision of the ectopic parathyroid tissue.
Before surgery, the following serum levels were as follows: high alkaline phosphatase - 345 IU/L (N.V. 35–104 U/L), low magnesium −1.03 mg/dL (N.V 1.58–2.55 mg/dL) and a slight anaemic syndrome.
After removing the adenoma, the PTH marked an important decrease from the initial value (from 2194 pg/mL to 92.5 pg/mL); one day after surgery the analysis showed a decreasing alkaline phosphatase-315 IU/L and normal serum calcium and ionic calcium.
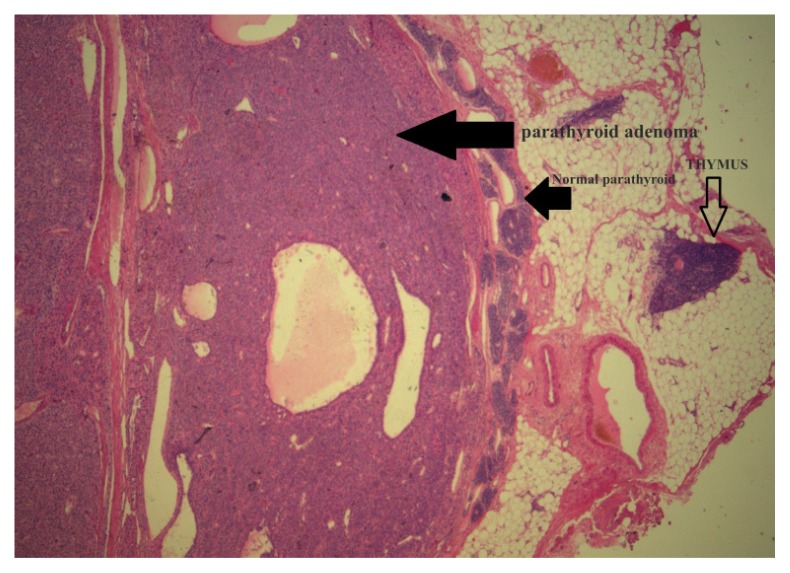
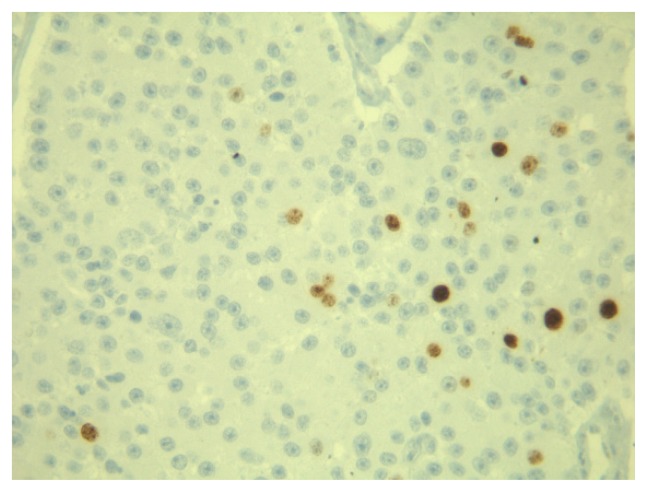
The histological examination performed in the usual hematoxylin-eosin staining confirms the diagnostic of parathyroid adenoma, Figure 3, with a minimal thymus inclusion in the specimen. The immunostaining for proliferation index ki-67 showed a value <10%, which suggested a low aggressive compound and arose the diagnostic of atypical parathyroid adenoma (Figure 4).
Figure 3.
Hematoxilin-eosin staining 25× of the ectopic adenoma.
Figure 4.
Proliferation index ki-67 in the atypical parathyroid adenoma.
Discussion
The parathyroid hormone (PTH) is produced by the parathyroid glands and has a role in adjusting the calcium and phosphate level in the body. It acts primarily on the bone level, stimulating bone resorption with the release of calcium and phosphate, and calcium resorption in the kidneys from the distal tube and phosphaturia [2]. The general plasmatic effect implies the rise of calcium and the reduction of phosphate.
The calcium metabolism disorders are highlighted through combined determinations of the intact PTH and calcium/phosphorus metabolism.
A plasmatic concentration of the intact PTH greater than normal associated with hypercalcaemia indicates a primary hyperparathyroidism.
The patients diagnosed with primary hyperparathyroidism can have a clinical history of MEN 1 and MEN 2 syndrome, irradiation in the cervical region, familial hyperparathyroidism, mandibular tumors [12,13].
In the case of primary hyperparathyroidism, the diagnostic appears late in the pathology and the symptoms of hypercalcaemia are manifested at renal, intestinal and bone level.
In the case of hypercalcaemia occurring during the malignant diseases, the PTH has normal values as compared to primary hyperparathyroidism, where the values of PTH are high. The nuclear imaging has an important role in localizing the parathyroid glands. The association between cervical echography and 99mTc- MIBI scintigraphy has a sensibility of 78–96% [9].
The parathyroidectomy is the treatment of choice for this pathology [10,13]. Postoperatively, a decrease of more than 50% of the level of PTH confirms the excision of the pathological parathyroid tissue and the existence of a single affected parathyroid.
The brown bone tumors frequently have a regression after the treatment of hyperparathyroidism, without the need of surgical resection. The association between hyperparathyroidism and mandibular tumor is extremely rare; the primary hyperparathyroidism- Jaw tumor syndrome - is an autosomal dominant disorder with incomplete penetration and variable expression. The mandibular tumors are present in 30% of cases, and the uterine tumors in 40% of cases [8].
The pathogenesis of the syndrome involves an inactivation of the HRPT2 gene, which codes a parafibromine protein, with a role in tumor suppression [14,15]. Mutations in the CDC73 (HRPT2) gene are the cause of two related genetic disorders resulting in hyperparathyroidism. HPT-JT- multiple endocrine neoplasia syndrome characterized by primary hyperparathyroidism due to tumors of the parathyroid gland, ossifying fibromas of the maxilla or mandible, and renal involvement in some patients (bilateral cysts and less frequently solid tumors such as hamartomas and Wilms tumor). The risk of malignancy of the parathyroid glands in HPT-JT has been estimated to be 15% [15].
In the reported case the presence of a uterine pathology and bone complications (pathological fractures and mandibular tumor) lead to the diagnostic of neoplasia with bone disseminations. The normal tumor markers, the existence of hypercalcemia and hyperparathyroidism confirmed through biochemical specimens, symptomatology, nuclear imaging and histopathological examination lead to the diagnostic of primary hyperparathyroidism - Jaw tumor syndrome (HPT-JT).
The normalization of the biological samples and of the patient’s general condition reconfirms the validity of the mentioned diagnosis. The screening for the HRPT2 gene was not realized because of personal reasons of the patient.
After 2 years, the actual condition of the patient is much better, without clinical complaints, no imaging recurrence and normal serum PTH.
The particularity of this case report is related to the severity of the disease, the delay of the diagnosis and the wrong interpretation of the pathology, due to the previous gynaecologic intervention. We would like to underline the necessity of an extensive endocrine evaluation of every patient with hypercalcemia, regarding the possibility of parathyroid involvement, in order that a curable pathology be not missed.
Acknowledgments
Prof. Dr. Ileana Duncea, Clinic of Endocrinology, Emergency County Hospital Cluj-Napoca.
References
- 1.Maria V, Saad AM, Ioannis F. Parathyroid adenoma associated with thymoma in a female adult with primary hyperparathyroidism. Int J Surg Case Rep. 2013;4(1):105–107. doi: 10.1016/j.ijscr.2012.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sisodiya R, Kumar S, Palankar N, BVD Case report on giant parathyroid adenoma with review of literature. Indian J Surg. 2013;75(Suppl 1):21–22. doi: 10.1007/s12262-011-0306-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Doherty GM, Lairmore TC, DeBenedetti MK. Multiple endocrine neoplasia type 1 parathyroid adenoma development over time. World J Surg. 2004;28(11):1139–1142. doi: 10.1007/s00268-004-7560-8. [DOI] [PubMed] [Google Scholar]
- 4.Dralle H, Altenahr E. Pituitary adenoma, primary parathyroid hyperplasia and papillary (non-medullary) thyroid carcinoma. A case of multiple endocrine neoplasia (MEN) Virchows Arch A Pathol Anat Histol. 1979;381(2):179–187. doi: 10.1007/BF01257883. [DOI] [PubMed] [Google Scholar]
- 5.Rone JK, Lane AG, Grinkemeyer MD. Papillary thyroid carcinoma, parathyroid adenoma, and unexplained hypercalcitoninemia: an unusual presentation of multiple endocrine neoplasia type 2A? Thyroid. 1998;8(9):781–785. doi: 10.1089/thy.1998.8.781. [DOI] [PubMed] [Google Scholar]
- 6.Migliore M, Pulvirenti G, Okatyeva V, Cannizzaro MA. Persistent hyperparathyroidism owing to a giant parathyroid adenoma in posterior mediastinum. Surgery. 2013;154(1):132–133. doi: 10.1016/j.surg.2012.04.003. [DOI] [PubMed] [Google Scholar]
- 7.Qiu ZL, Wu CG, Zhu RS, Xue YL, Luo QY. Unusual case of solitary functioning bone metastasis from a “parathyroid adenoma”: imagiologic diagnosis and treatment with percutaneous vertebroplasty--case report and literature review. J Clin Endocrinol Metab. 2013;98(9):3555–3561. doi: 10.1210/jc.2013-2014. [DOI] [PubMed] [Google Scholar]
- 8.Eklioglu BS, Atabek ME, Akyurek N. Parathyroid adenoma presented with multiple brown tumors and nephrocalcinosis. J Pediatr Endocrinol Metab. 2013;26(3–4):213–214. doi: 10.1515/jpem-2012-0275. [DOI] [PubMed] [Google Scholar]
- 9.Dasgupta DJ, Navalkissoor S, Ganatra R, Buscombe J. The role of single-photon emission computed tomography/computed tomography in localizing parathyroid adenoma. Nucl Med Commun. 2013;34(7):621–626. doi: 10.1097/MNM.0b013e3283617d5b. [DOI] [PubMed] [Google Scholar]
- 10.Grassetto G, Rubello D. The increasing role of minimal invasive radioguided parathyroidectomy for treating single parathyroid adenoma. J Postgrad Med. 2013;59(1):1–3. doi: 10.4103/0022-3859.109477. [DOI] [PubMed] [Google Scholar]
- 11.Piciu D, Irimie A, Kontogeorgos G, Piciu A, Buiga R. Highly aggressive pathology of non-functional parathyroid carcinoma. Orphanet J Rare Dis. 2013;8:115. doi: 10.1186/1750-1172-8-115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pallan S, Khan A. Primary hyperparathyroidism: Update on presentation, diagnosis, and management in primary care. Can Fam Physician. 2011;57(2):184–189. [PMC free article] [PubMed] [Google Scholar]
- 13.Meszaros L, Kajdacsi Z, Toth M, Revai T, Vadasz P. Mediastinal parathyroid adenoma: a surgically treated case. Magy Seb. 2013;66(4):191–193. doi: 10.1556/MaSeb.66.2013.4.1. [DOI] [PubMed] [Google Scholar]
- 14.Carlson AL, Smith CL. Primary hyperparathyroidism and jaw tumor syndrome: a novel mutation of the HRPT2 gene. Endocr Pract. 2008;14(6):743–747. doi: 10.4158/EP.14.6.743. [DOI] [PubMed] [Google Scholar]
- 15.Howell VM, Haven CJ, Kahnoski K, Khoo SK, Petillo D, Chen J, et al. HRPT2 mutations are associated with malignancy in sporadic parathyroid tumours. J Med Genet. 2003;40(9):657–663. doi: 10.1136/jmg.40.9.657. [DOI] [PMC free article] [PubMed] [Google Scholar]