Abstract
Almost all pregnant women (98%) in 24 Cape Town neighborhoods were randomized by neighborhood to: 1) the standard care (SC) condition (n=12 neighborhoods; n=594 pregnant women), or 2) the Philani Intervention Program (PIP) in which home visits by Community Health Workers (CHW) were conducted (n=12 neighborhoods; n=644 pregnant women). At 36 months post-birth (84.6% follow-up) PIP mothers were significantly less depressed at compared to the SC mothers. Children in PIP are significantly less likely to be stunted (24.3% vs 18.1%, p=0.013), to have better vocabularies and are less likely to be hospitalized than children in the SC condition. These data suggest home visits may need to continue for several years post-birth. Sustainable, scalable perinatal intervention models are needed in LMIC.
Keywords: maternal depression, perinatal home visiting, community health workers
Introduction
Investment in children's early years is critical for improving lifelong well-being (Victora et al., 2008). Delivering interventions in the first 1000 days and in the early years has been shown to be cost effective (Heckman, 2006), to reduce health inequities (Marmot et al., 2008), and there is an increasing evidence base for how early childhood investments can substantially improve adult health (Campbell & Scott, 2011). However, poverty and both infectious and non-communicable diseases in low and middle-income countries (LMIC) are implicated in poor child outcomes. Traditionally, global health programs have focused on disease targeted ‘magic bullet’ solutions to complex health problems, with a proliferation of a silo mentality (Panter-Brick, Eggerman, & Tomlinson, 2014). Increasingly however, many programmes in LMIC are focusing on multiple behaviors and risk and protective factors. In most LMIC, it is community health workers (CHW) who are the primary work-force that will have to deliver these generalist interventions. While a rigorous evidence base exists for the efficacy of single disease targeted CHW interventions, there is a dearth of evidence detailing whether CHWs can be trained to deliver broader interventions focusing on multiple domains and risk factors with the same positive outcomes.
Perinatal nurse home visiting is the most efficacious EBI to date (Olds et al., 2014). When mounted in LMIC, paraprofessionals deliver home visits, typically to address only one risk, and efficacy has been repeatedly demonstrated in RCTs (Peacock, Konrad, Watson, Nickel, & Muhajarine, 2013). Most of these trials have been in the U.S. (Michalopoulos et al., 2015). However, when scaling these programs, efficacy typically disappears (Peacock et al., 2013). There have been at least four studies in LMIC in the most recent reviews that meet rigorous scientific standards and demonstrate efficacy (Peacock et al., 2013). Perinatal home visitors in Pakistan (Rahman, Iqbal, Roberts, & Husain, 2009) intervened in maternal depression and had benefits not only on maternal depression, but also in breastfeeding; children's growth did not change, however. Home visiting in Jamaica over one year (Grantham-McGregor, Powell, Walker, & Himes, 1991) and in Bangladesh (Nahar et al., 2012) and Chile (Aracena et al., 2009) provided nutritional supplements and early stimulation - improving children's outcomes. Our project, the Philani Intervention Model (PIM) (M. J. Rotheram-Borus et al., 2011) was one of the successful programs in LMIC (Peacock et al., 2013).
Philani Intervention
In the Philani+ intervention, paraprofessional community health workers (CHW) were trained to address multiple health challenges during home visits. The CHW aimed to reduce mother's risk of acquiring HIV; follow protocols to Prevent Maternal to Child Transmission (PMTCT); improve maternal and child health including TB and illness detection; reduce maternal alcohol use; improve infant and child nutrition; and, foster children's growth and development. A cluster randomized controlled trial (RCT) was mounted in the townships of Cape Town, South Africa in 2009-2010 (M. J. Rotheram-Borus et al., 2011). Local township women were trained to be CHW and to apply cognitive-behavioral skills to support mothers to manage daily activities and improve their children's outcomes. Atypically, the Philani effectiveness trial had both high internal (85% follow-up) and external validity (98% recruitment), and a longitudinal follow-up lasting 36 months post-birth. This cohort included all Mothers Living with HIV (MLH) in a neighborhood, unlike the perinatal HIV cohorts of MLH and their children which are clinic-based samples. Also different from the perinatal HIV cohorts, which had substantial loss-to-follow-up (from 19% to 89% at one year; (Kalembo & Zgambo, 2012), there were very high follow-up rates over 36 months. The CHW did not replicate a manual with fidelity, as typically advocated by prevention researchers (Flay et al., 2005).
CHW were selected on the basis of having their own children that were thriving (positive peer deviants), good communication skills as well as having good problem solving skills. CHW were trained for one month using role-plays, watching videotapes of common challenging situations that CHW might face during home visits. This study offers a different option for diffusing EBI: CHW were trained on 1) foundational skills common across many EBI; 2) application of key health information about HIV, alcohol use, malnutrition, and general maternal and child health; and 3) coping with their own life challenges.
Previous results
Earlier analyses of outcomes for households in the home visiting condition compared to households in a control condition demonstrated multiple benefits of the intervention up to the age of 18 months for mothers and their children (le Roux et al., 2013; M.J. Rotheram-Borus et al., 2014) including fewer post-birth complications and hospitalizations for children; longer and exclusive breastfeeding; 50% higher cumulative rate of adherence to PMTCT tasks; higher rates of condom use; and, less stunting. The intervention also had fewer low birth weight (LBW) infants than the control condition.
Given the likelihood that mothers and children living in adversity will be subjected to ongoing and sustained adversity and risk, as well as the fact that there is an increasing evidence base about how initial benefits of early interventions may not be sustained over time (Maselko et al., 2015), this paper examines maternal and child outcomes at 36 months.
Methods
Ethics statement
The Institutional Review Boards of University of California Los Angeles (UCLA), Stellenbosch University, and Emory University approved the study, whose methods have previously been published (M. J. Rotheram-Borus et al., 2011). Written, voluntary, informed consent was received from all study mothers. Three independent teams conducted the assessment (Stellenbosch), intervention (Philani Project), and randomization and data analyses (UCLA). This cluster randomised control trial is registered with ClinicalTrials.gov (NCT00996528; https://clinicaltrials.gov/ct2/show/NCT00972699).
Participants
Neighborhood clusters (N=24) of 450-600 households were identified and matched based on the housing type, presence of electricity, water, sanitation, size and density, alcohol bars, child care resources, distance to clinics, and length of residence. Buffer neighborhoods prevented cross-neighborhood contamination. UCLA randomized neighborhoods in six blocked sets of four neighborhoods each, for 12 PIP neighborhoods (n=644) and 12 SC neighborhoods (n=594).
Recruiters
Township women conducted house-to-house visits every other month from May 2009 to September 2010 to identify all pregnant women and refer to the study; only 2% refused participation. Assessments were conducted at a research office in the township, with transport provided. Table 1 shows that at recruitment, the women were nearly equivalent across conditions on almost all measures (le Roux et al., 2013; M.J. Rotheram-Borus et al., 2014).
Table 1.
Characteristics of the sample grouped by the Intervention (N=644) and Standard Care (N=594) conditions.
| Intervention (N=644) | Standard Care (N=594) | Total (N=1238) | ||||
|---|---|---|---|---|---|---|
| n | % | N | % | n | % | |
| Demographic Characteristics | ||||||
| Mean age (SD) | 26.5 | 5.5 | 26.3 | 5.6 | 26.4 | 5.5 |
| Mean highest education level (SD) | 10.3 | 1.8 | 10.3 | 1.8 | 10.3 | 1.8 |
| Currently employed | 129 | 20.0 | 104 | 17.5 | 233 | 18.8 |
| Married or lives with partner | 377 | 58.5 | 324 | 54.6 | 701 | 56.6 |
| Monthly household income >2000 Rand | 280 | 45.6 | 279 | 48.1 | 559 | 46.8 |
| Formal housing | 197 | 30.6 | 191 | 32.2 | 388 | 31.3 |
| Water on site | 333 | 51.7 | 327 | 55.1 | 660 | 53.3 |
| Flush toilet | 340 | 52.8 | 343 | 57.7 | 683 | 55.2 |
| Electricity | 569 | 88.4 | 543 | 91.4 | 1112 | 89.8 |
| Mother hungry past week | 312 | 48.4 | 301 | 50.7 | 613 | 49.5 |
| Children hungry past week | 175 | 27.2 | 185 | 31.1 | 360 | 29.1 |
| Alcohol | ||||||
| Use during pregnancy | 56 | 8.7 | 49 | 9.8 | 105 | 9.2 |
| AUDIT-C > 2 at pregnancy | 113 | 17.6 | 101 | 20.2 | 214 | 18.7 |
| AUDIT-C > 2, after pregnancy discovery | 41 | 6.4 | 24 | 4.8 | 65 | 5.7 |
| Maternal Health and Mental Health | ||||||
| Mean weeks pregnant at assessment (SD) | 26 | 7.9 | 25.8 | 8.4 | 25.9 | 8.1 |
| Non-primipara | 422 | 65.5 | 394 | 66.3 | 816 | 65.9 |
| Previous LBW infants | 61 | 14.5 | 69 | 17.5 | 130 | 15.9 |
| EPDS, mean score (SD) | 11.2 | 6.9 | 10.4 | 7.1 | 10.8 | 7.0 |
| EPDS > 13 | 238 | 37.0 | 195 | 32.8 | 433 | 35.0 |
| HIV and Reproductive Health Behavior | ||||||
| Recent Sexual partnera | 580 | 90.1 | 522 | 87.9 | 1102 | 89.0 |
| Ever tested for HIV | 590 | 91.6 | 550 | 92.6 | 1140 | 92.1 |
| Received HIV test results | 584 | 99.0 | 547 | 99.5 | 1131 | 99.2 |
| Knowledge of partner HIV status | ||||||
| Partner HIV+ | 46 | 7.9 | 50 | 9.6 | 96 | 8.7 |
| Partner HIV- | 325 | 56.0 | 296 | 56.7 | 621 | 56.4 |
| Partner serostatus unknown | 209 | 36.0 | 176 | 33.7 | 385 | 34.9 |
| Request partner HIV test | 391 | 82.5 | 355 | 83.1 | 746 | 82.8 |
| Mothers living with HIV (MLH) | 149 | 25.5 | 146 | 26.7 | 295 | 26.1 |
| Mean number of people disclosed to (SD) | 3.8 | 4.5 | 5 | 7.2 | 4.4 | 6.0 |
| Recent Sexual partnera | 127 | 85.2 | 125 | 85.6 | 252 | 85.4 |
| Disclosed HIV status to partner | 99 | 73.9 | 105 | 82.7 | 204 | 78.2 |
| Knowledge of partner HIV status | ||||||
| Partner HIV+ | 42 | 33.1 | 50 | 40.0 | 92 | 36.5 |
| Partner HIV- | 13 | 10.2 | 17 | 13.6 | 30 | 11.9 |
| Partner serostatus unknown | 72 | 56.7 | 58 | 46.4 | 130 | 51.6 |
“Recent” always refers to the last three months.
Figure 1 summarizes participant flow through the study. 1238 women were assessed at baseline. Follow-up assessments were conducted at two weeks post-birth (92%; mean=1.9 weeks; SD=2.1 weeks); six months (87%; mean=6.2 months, SD=0.7); 18 months (91%; mean=19.1 months; SD=3.0); and 36 months (85%; mean = 37.3 months; SD = 2.2 months). All assessments were completed by 80% of mothers; 1.6% (n=20) completed no follow-up reassessments.
Figure 1.
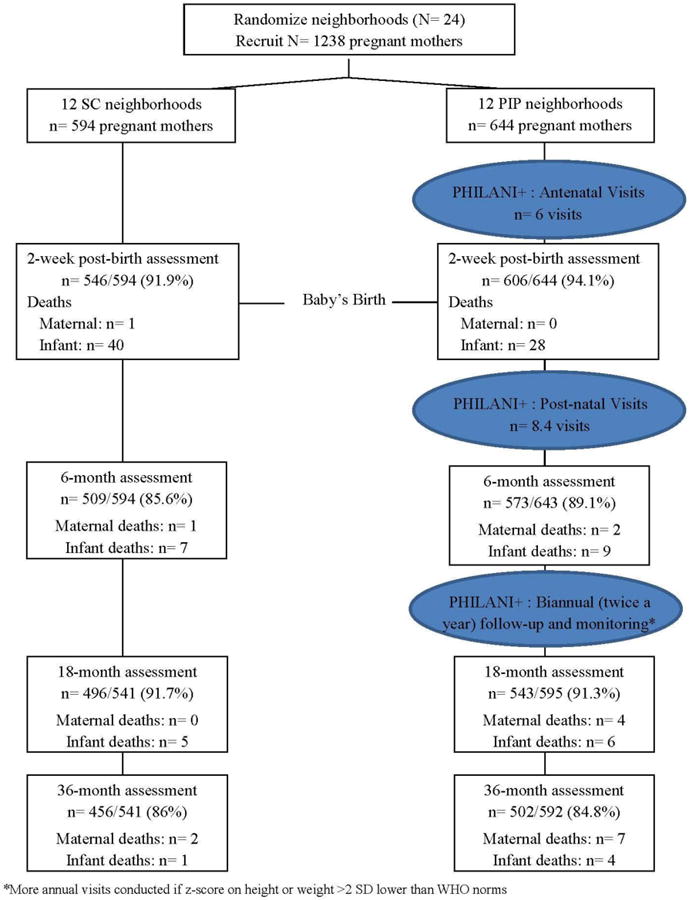
Movement of participants through the RCT at assessment points comparing mothers in a control condition and a home visiting intervention.
Assessments
Township women were recruited, trained, and certified as interviewers, entering responses on mobile phones (Nokia E61i and 2630) programmed by Mobenzi (http://www.mobenzi.com/researcher/). Supervisors monitored and gave feedback on the data quality weekly. Data collection ended in May 2014.
Measures
Maternal outcomes
Demographic characteristics were reported at baseline. At each assessment, current housing and household status was checked.
Alcohol use
The frequency of drinking alcohol was assessed at each assessment (0-9 scale ranging from 0=never to 9=every day), including the amount of alcohol on days using (0-5 scale ranging from 0=none to 5=10 or more drinks). The Derived Alcohol Use Disorder Identification Test (Derived AUDIT-C) (Dawson, Grant, & Stinson, 2005) is a three-item scale, with each rated 0-4 on intensity, which documents the severity of alcohol dependence when the score is greater than three (Saunders, Aasland, Babor, de la Fuente, & Grant, 1993) and has been used extensively among Cape Town residents.
Depressive symptoms
were reported at each assessment using the Edinburgh Postnatal Depression Scale (EPDS) (Cox, Holden, & Sagovsky, 1987), with a cut-off of >13 to indicate depressed mood (Lawrie, Hofmeyr, de Jager, & Berk, 1998). The Hopkins Depression Measure (Derogatis, Lipman, Rickels, Uhlenhuth, & Covi, 1974) was administered at the 36 month assessment, which is a 21-item measure with good internal reliability and construct validity (Deane, Leathem, & Spicer, 1992).
Health
Assessed by self-reports of diabetes, high blood pressure, and tuberculosis on a single question. HIV status and new pregnancies/childbirths were reported at each assessment.
HIV prevention
All mothers reported their number of recent sexual partners (i.e., last three months) and the numbers of episodes of using condoms on each of the last 10 sexual encounters. Partner serostatus and disclosures of serostatus by MLH were reported, as well as re-engagement in HIV care following childbirth and receipt of ARV.
Family support was monitored by receipt of the government child grant, a child receiving day care at a crèche, employment, and moving residences.
Child measures
The Peabody Picture Vocabulary Test (PPVT)
(Dunn, 1965) was administered at 36 months, using a form adapted for South Africa (Pakendorf & Alant, 1996).
Each child had a Road to Health card issued by the government on which each clinic visit and hospitalization was recorded. Growth was measured at each assessment; interviewers measured children's weight, height, and head circumference, after being trained and certified. Infant anthropometric data were then converted to z-scores based on the World Health Organization's (WHO) age-adjusted norms (http://www.who.int/childgrowth/standards/en/). A z-score below -2 was considered a serious health deficit (de Onis & Blossner, 2003), as being stunted (>-2 for HAZ) or malnourished (>-2 for WAZ). About 1% (n= 9) of children had height-for-age z-scores (HAZ) >3 or <-3; 6.1% (n= 54) of children had weight-for-age z-scores (WAZ) >3 or <-3; similarly, 7.0% (n=62) had weight-for-length z-scores (WFLZ) >3 or <-3; and 5.8% (n=51) had head-circumference z-scores (HCZ) >3 or <-3. Growth scores >3 or <-3 values may represent measurement errors and, therefore, these scores were omitted from the final analyses.
SC and interventionconditions
SC condition
Standard clinic care in Cape Town is accessible within 5 km of each study neighborhood. Each antenatal clinic provides comprehensive PMTCT services, including HIV testing. Stand-alone HIV clinics provide access to ARVs for persons with CD4 < 350.
Intervention condition
In addition to access to clinic services similar to the SC condition, home visits were conducted. The Philani Nutrition Programme has operated for 29 years in Cape Town, conducting home visits. Township women, who typically have never worked outside the home and who have less than a high school education, were trained as CHW for one month in cognitive-behavioral change strategies. CHWs were women selected for having good social and problem solving skills and raising healthy children using their own coping skills, and were trained to provide and apply health information about general maternal and child health, HIV, alcohol use, and nutrition. Videotaped models of common situations that CHWs might face were provided. CHWs were certified and supervised biweekly with random observations of home visits. Eight health messages were delivered on HIV/TB prevention, strategies for PMTCT, the consequences of alcohol use/abuse, the importance of breastfeeding, and how to avoid malnutrition. CHW were to deliver these messages in at least four antenatal visits and four post-natal visits within the first two months of life. On average, CHWs made six antenatal visits (SD=3.8), five postnatal visits between birth and two months post-birth (SD=1.9), and until six months post-birth about 1.4 visits/month (range:0.1-6.4 visits/month). Sessions lasted on average 31 minutes each. Visits were biannual after six months, primarily to check for growth and/or abuse.
Data Analysis
We examined the distribution of all variables by the intervention and SC condition. For continuous or discrete variables assessed at multiple time points, we analyzed the data using a longitudinal model with random intercepts for mother or child. We included fixed effects for the neighborhoods and estimated intervention effects as the average of the intervention neighborhood effects minus the SC neighborhood effects. For continuous child variables collected only a single time, we omit the child random effect, but otherwise use the same analysis with random neighborhood effects. Missing data are assumed missing at random; we used all observations that were possible to use, up to the point where mothers or children died or were lost to follow-up. Mothers and children could return to the study even if they missed an assessment. HIV-positive children were omitted from child analyses (n=23 total). All analyses were adjusted for mothers' HIV status. Given their lack of comparability to singleton births, twin and triplet births were excluded from the analyses of child growth scores (n=25). All longitudinal and regression analyses were conducted in SAS Proc Mixed and Proc Glimmix (version 9.4; SAS Institute Inc., Cary, North Carolina). We used Fisher exact tests to compare mortality across conditions. All analyses were based on intent-to-treat models.
Results
Initial sample
Table 1 summarizes the characteristics of the mothers in the intervention and the SC conditions during pregnancy, which have been presented previously (le Roux et al., 2013; M.J. Rotheram-Borus et al., 2014). There are very few differences across conditions. Mothers were typically in their mid-20s, without a high school education or job, living in a shack, and about half had experienced food insecurity. Only 9.2% drank alcohol after recognizing they were pregnant and 25% prior to pregnancy. Most women had recent sexual partners. Almost every woman had been tested for HIV during pregnancy and 26.1% (n=295) were MLH. Table 2 is a correlation matrix of the outcome variables at the baseline assessment.
Table 2.
Correlation matrix among the outcome variables at the baseline assessment. Overall Baseline Pearson Correlation
| EPDS | AUDIT | Alcohol | Disease | Partner | Violence | #Partners | Condom | |
|---|---|---|---|---|---|---|---|---|
| AUDIT Score | 0.08** | 1 | ||||||
| Recent Alcohol Use | 0.08** | 0.34*** | 1 | |||||
| TB, High BP, or Diabetes | 0.06* | 0.03 | -0.01 | 1 | ||||
| Current Partner | -0.13*** | -0.10** | -0.10** | -0.02 | 1 | |||
| Any Violence with Partner | 0.15*** | 0.17*** | 0.22*** | 0.00 | 0.00 | 1 | ||
| Number of Partners | -0.04 | -0.05 | -0.09** | -0.04 | 0.53*** | 0.04 | 1 | |
| Consistent Condom Use | -0.04 | -0.04 | 0.02 | 0.02 | 0.06 | -0.03 | 0.03 | 1 |
| Full/part-time/or self-employed | -0.06* | 0.02 | -0.06* | -0.02 | 0.05 | -0.12*** | 0.00 | 0.02 |
p < .05,
p <.01,
p <.001
Maternal Outcomes
By 36 months after birth, 1.4% of mothers (n=17) had died; more often, MLH died compared to mothers without HIV (p <0.0001, OR = 7.9, 95%CI = (2.4, 33). Significantly more intervention MLH died than SC MLH (n=11 intervention MLH; n=2 SC MLH, p = 0.02, OR = 0.19, 95%CI = [0.02, 0.88]). From six to 36 months post-birth, 47 additional mothers (5.4%) reported an HIV diagnosis, with similar numbers across conditions. Almost all MLH (94.1%; 318/338) had received antenatal care and PMTCT, as previously reported (M.J. Rotheram-Borus et al., 2014). Migration from Cape Town to the Eastern Cape occurred among 2.6% of participating mothers (27/1052) by the time of the child's birth. At the six month assessment, 8.6% of children were living in the Eastern Cape (87/1006), 29.9% of these without their mother (26/87). At 18 months, 13.3% (128/960) of children were in the Eastern Cape, 39.1% (50/128) without their mother. At 36 months, 24.0% were in the Eastern Cape (211/878), 62.1% (131/211) without their mother.
Table 3 compares mothers in the intervention and SC conditions on multiple measures at 36 months (see Web Appendix for summaries of outcomes at each time point and reliability between time points. Mothers in the intervention condition reported significantly less depression on both the EPDS (mean difference, 0.8; p = 0.009) and the Hopkins Depression Measure (mean difference, 3.3; p = 0.011). There were no significant differences in alcohol use at 36 months or in the frequency of having problematic alcohol use on the AUDIT. Mothers' health was similar across conditions; 18.7% had given birth again. There were no significant differences in partner-related behaviors, including the likelihood of having a current partner, living with a partner, partner violence, or the number of sexual partners. Similar to earlier reports, most women have a sexual partner, but only about half of the partners live in the household. Mothers were equally likely to receive the child grant (80.5%), to leave their child in a crèche (59.7%; day care), and to be employed (44.1%) across conditions. MLH were equally like to re-engage with HIV care and to receive ARV over time across conditions.
Table 3.
Maternal outcomes at 36 months grouped by the Intervention (N=502) and Control (N=456) conditions.
| Intervention (N=502) | Standard Care (N=456) | Total (N=958) | ||||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| Maternal depression | ||||||
| Mean EPDS score (SD) | 6.1 | 7.34 | 6.9 | 7.9 | 6.5 | 7.6** |
| Mean Hopkins score (SD) | 34.2 | 14.9 | 36.2 | 17.4 | 35.1 | 16.1** |
| Alcohol use | ||||||
| Recent usea | 84 | 16.8 | 85 | 18.7 | 169 | 17.7 |
| AUDIT > 2 | 61 | 12.2 | 69 | 15.2 | 130 | 13.6 |
| Maternal health | ||||||
| TB, High BP, or Diabetes | 49 | 9.8 | 49 | 10.7 | 98 | 10.2 |
| New pregnancies | 95 | 19.0 | 84 | 18.5 | 179 | 18.7 |
| Develop new HIV case by 36 months | 25 | 5.5 | 22 | 5.3 | 47 | 5.4 |
| Acquired during pregnancy | 12 | 1.9 | 10 | 1.7 | 22 | 1.8 |
| Acquired by 6 months | 2 | 0.3 | 5 | 0.8 | 7 | 0.6 |
| Acquired by 18 months | 1 | 0.2 | 3 | 0.5 | 4 | 0.3 |
| Acquired by 36 months | 10 | 1.6 | 4 | 0.7 | 14 | 1.1 |
| HIV prevention | ||||||
| Maternal partner | ||||||
| Current partner | 442 | 88.2 | 394 | 86.4 | 836 | 87.4 |
| Lives with mother | 266 | 53.1 | 229 | 50.3 | 495 | 51.8 |
| Any violence with intimate partner | 72 | 14.4 | 70 | 15.4 | 142 | 14.9 |
| Number of recentsexual partnersa | ||||||
| 0 | 70 | 14.0 | 73 | 16.0 | 143 | 15.0 |
| 1 | 419 | 83.6 | 371 | 81.5 | 790 | 82.6 |
| > 1 | 12 | 2.4 | 11 | 2.4 | 23 | 2.4 |
| Consistent condom use (10/10) | 200 | 46.4 | 159 | 41.7 | 359 | 44.2 |
| Linked to care | 81 | 59.1 | 84 | 66.1 | 165 | 62.5 |
| ARV use by MLH | 73 | 53.3 | 67 | 52.8 | 140 | 53.0 |
| Family Support | ||||||
| Child Grant | 401 | 80.0 | 369 | 80.9 | 770 | 80.5 |
| Child in Crècheb | 299 | 61.1 | 257 | 58.1 | 556 | 59.7 |
| Full/part-time/or self- employed | 220 | 43.9 | 202 | 44.3 | 422 | 44.1 |
| Household moves | 146 | 29.1 | 128 | 28.1 | 274 | 28.6 |
“Recent” always refers to the last three months.
Measured at 3 year assessment only
p< .05,
p< .01,
p< .001
Child Outcomes
By 36 months, 8.2% (n=101) of the children had died; however, children of MLH were no more likely to die than children of mothers without HIV (p = 0.3, OR = 0.76, 95%CI = [0.45, 1.23]). Only 6.2% (n=23; 10 intervention, 13 SC) of children were seropositive, similar across conditions. Table 4 summarizes the child outcomes. Intervention children had significantly higher scores on the Peabody Picture Vocabulary Test (p = 0.039) and were also significantly less likely to have been hospitalized compared to children in the SC condition (p = 0.026).
Table 4.
Child outcomes at 36 months grouped by the Intervention (N=492) and Standard Care (N=447) conditions.
| Intervention (N=492) | Standard Care (N=447) | Total (N=939) | ||||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| Age in months | 35.6 | 2.2 | 36.5 | 2.2 | 36.6 | 2.2 |
| Child Language (SD) | ||||||
| PPVT score | 20.0 | 7.9 | 19.2 | 8.2 | 19.6 | 8.1* |
| Health | ||||||
| Child Admitted to Hospital (N/%) | 122 | 24.8 | 141 | 31.6 | 263 | 28.1* |
| Zero | 369 | 75.2 | 305 | 68.4 | 674 | 71.9 |
| One | 92 | 18.7 | 95 | 21.3 | 187 | 20.0 |
| Two | 13 | 2.6 | 26 | 5.8 | 39 | 4.2 |
| Three | 8 | 1.6 | 9 | 2.0 | 17 | 1.8 |
| Four | 5 | 1.0 | 6 | 1.3 | 11 | 1.2 |
| Five + | 4 | 0.8 | 5 | 1.1 | 9 | 0.9 |
| Growth Measures | ||||||
| Height for Age Z Score | -1.2 | 1.0 | -1.0 | 1.0 | -1.1 | 1.0 |
| Weight for Age Z Score | 0.1 | 1.0 | 0.1 | 1.0 | 0.1 | 1.0 |
| Weight for Height by Age Z Score | 1.0 | 1.0 | 1.1 | 1.0 | 1.0 | 1.0 |
| Head Circ. for Age Z Score | 0.9 | 1.0 | 0.9 | 0.9 | 0.9 | 1.0 |
| Height/age < -2SD Score | 75 | 18.1 | 95 | 24.3 | 170 | 21.1* |
| Weight/age < -2SD Score | 8 | 1.8 | 6 | 1.5 | 14 | 1.6 |
p< .05,
p< .01,
p< .001
Children were similar across conditions at 36 months on weight, height, and head circumference for age z-scores. Intervention children were significantly less likely to be stunted compared to children in the SC condition (24.3% vs 18.1%.p <0.013, as shown on Figure 2 and Table 4), but rates of malnutrition were similar across conditions (1.6%). Overall, 27.3% have a height, weight, or head circumference for age z-score <-2. Figure 2 shows the proportion of stunted children over time from birth to 36 months for the intervention and SC conditions. Post-birth, children across conditions had significantly lower height-for-age z-scores at each assessment point, compared to height-for-age z-scores at birth: six months (est. 0.16, SE=0.05, df= 2270, t=3.32 p <.0001); 18 months, (est.-0.25, SE=0.05, df=2270, t=-5.2, p< 0.0001); and 36 months (est.-0.87, SE=0.05, df=2270, t=-17.97, p <0.0001).
Figure 2.
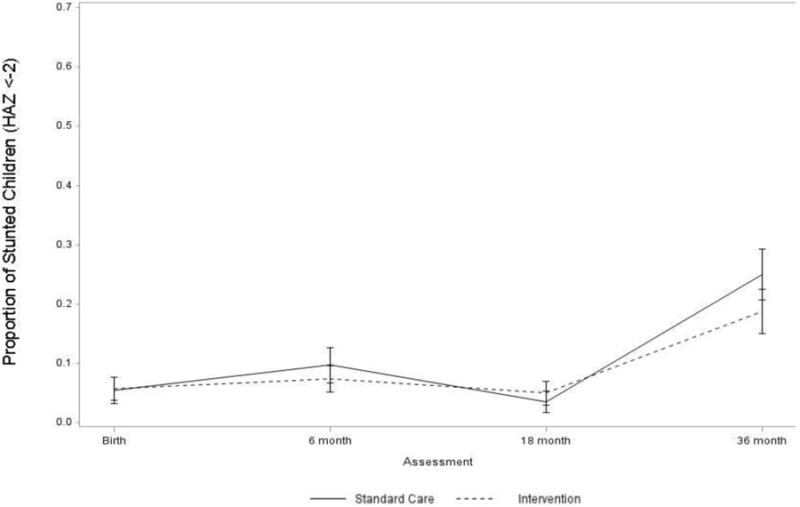
Proportion of children with height-for-age < -2 (stunting) +/-2 SE at assessment for intervention and control groups.
Discussion
At 36 months postpartum, intervention mothers were significantly less depressed and intervention children had better vocabularies and were less likely to be hospitalized and stunted compared to those in the control condition. Importantly, we have shown that these benefits accrue, even though home visiting was only about twice a year after the child was six months old. While mothers continued to experience poverty, had partners who were typically unemployed, abused alcohol, and became violent at times, their children's developmental capacities evolved. Given these stressors, it may be seen as surprising that any intervention benefits remained at 36 months.
Maternal depression, especially among mothers of young children, often sets lifelong negative developmental trajectories for their children (Tomlinson, Cooper, Stein, Swartz, & Molteno, 2006). Earlier evaluations of this intervention did not find that mothers were less depressed (le Roux et al., 2013; M.J. Rotheram-Borus et al., 2014). Yet, it was found at six and 18 months that depressed mothers were better caretakers, in being significantly more likely to breastfeed, to breastfeed longer, and to have children with better early growth and higher scores on the Bayley Scales of Infant Development at 18 months (Tomlinson et al., 2015). Even so, mothers had not benefited earlier by being less depressed themselves at six or 18 months. The CHWs consistently stressed the importance of maternal caretaking and breastfeeding, but had not been trained to treat maternal depression. Even though there were both direct and indirect intervention effects on maternal depression, the next iteration of the Philani intervention should also target maternal depression.
Children in LMIC are often at a substantial disadvantage by the time that school starts (Engle & Black, 2008). Children in the intervention neighborhoods continue to have some advantages over children in the control neighborhoods. Their language development was significantly better than their peers, which should substantially help prepare children for school. There is a substantial literature detailing the impact of combined nutrition and stimulation interventions on improved child language (Aboud & Akhter, 2011; Super, Herrera, & Mora, 1990; Waber et al., 1981). Our vocabulary finding is notable, as cognitive stimulation is not a specific focus of the Philani intervention. What the Philani intervention does focus on is increasing rates of early breastfeeding, illness detection and early engagement of mothers and infants. We would suggest that the focus of the Philani intervention on the mother-child dyad may have facilitated a process where caregivers were able to more sensitively follow infant cues and engage infants in reciprocal exchange (Vally, Murray, Tomlinson, & Cooper, 2015). The precursors to language are extremely complex, but there is evidence of how these early social interaction play a role in language development (Bruner, 1985).
Physical health status also appears better, as there were fewer hospitalizations and fewer stunted children. These benefits are key given stunting influences lifelong health and well-being (Victora et al., 2008). The pattern of results for mothers and children across intervention conditions demonstrates the consequences of HIV. More than 5% of mothers report HIV from six to 36 months post-birth; it may be that women knew they were infected earlier and only later disclosed their serostatus to the research team. We could validate maternal HIV status on the government-issued Road-to-Health card, but we did not independently assess HIV status or access clinic records. One-third of the newly identified MLH were identified when tested for HIV during a subsequent pregnancy. Messages regarding condom use may have influenced about half of the mothers—an insufficient number to stop a generalized epidemic. Only 1.4% of mothers died overall, and these were more likely to be MLH and more likely to be in the intervention condition (11 vs 2 MLH deaths). Even though we had 85% follow-up, if two more mothers in the SC condition had died, there would be no significant difference between the conditions in maternal deaths. Such small numbers lead us to interpret this finding conservatively. A substantial minority of children are missing key supportive services. Even 36 months post-birth, 20% of households are not receiving a child grant (100% are eligible). Two of five children get no preschool or crèche experiences, and about one in five has a younger sibling, competing for maternal caretaking. It is also distressing to see the rise in stunting at 36 months and the consistently lower z-scores in height for age over time.
These data suggest it may be useful to maintain frequent CHW visits past the first six months of life. A considerable evidence base has emerged demonstrating the enduring impact of adversity during pregnancy and the first two years, resulting in an increased focus of global health policy and intervention on the “first 1000 days” (Black & Aboud, 2011; Gertler et al., 2014). Coupled with this, Heckman (1995) has demonstrated the cost effectiveness of early investments in children's well-being compared to later interventions at school or job training programmes post-school. We would argue however, that the benefits to child development and adult health that accrue across the life-course may require more than simply efficacious interventions in the first 1000 days, and that if early benefits are to be sustained and built upon, that services such as preschool, primary school, and health care need to be widely available to children and families in the years following interventions in the first 1000 days. This has been demonstrated in a recent follow-up of a trial for perinatal depression by Maselko et al. (2015) that showed how the cognitive, socio-emotional, and physical developmental outcomes of children at age 7 years whose mother had prenatal depression did not differ between those who received the intervention and those who did not. In communities without later supports and services it may be important to sustain visits over the 36-60 months post-birth period, which would cover the phases of children' language development, goal setting, and key processes central to cognitive and socio-emotional development. Children would likely also benefit indirectly by the improved health of their mothers, if visits were extended.
The Philani Programme was implemented with strategies outlined in each of the two most recent literature reviews: CHW selection criteria were based on social competency; CHWs were paid a stipend; and, monitoring and supervision was consistent over time and utilized mobile phones. Mentor Mothers received ongoing training with a random visit from their supervisor once every two weeks and went to a half day of in-service training monthly. Mentor Mothers were trained on a within-session protocol and a between-session approach to implementing a behavior change program. However, we have no real-time measures of the content covered or the skills addressed in each session. We only can ensure that the Mentor Mothers actually delivered a visit (based on the Global Positioning Information collected).
Mentor Mothers were always cautioned to not provide only information. Features of the Philani that make it successful include a focus on establishing strong relationships; setting goals and helping the mothers acquire the skills to problem solve daily events, especially related to HIV, alcohol, and malnutrition; enduring that the Mentor Mother did not take-on solving the mother's daily challenges, but to keep responsibility with the mothers for creating healthy routines for their children; and explicitly addressing the barriers to reducing alcohol use, seeking HIV treatment, and providing adequate nutrition.
We can only speculate, however, one the competitive advantages of the CHWs employed by the Philani Programme that may have led to these sustained benefits at 36 months. Five features distinguish these CHW: 1) they are selected based on being positive peer deviants (Bolles, Speraw, Berggren, & Lafontant, 2002); 2) CHW are trained to address multiple health challenges, not only one; 3) there are clear expectations for performance (e.g., a defined caseload of 40 families) and accountability structures for both interpersonal supervision and monitoring by paper documentation of visits or mobile phones; 4) CHWs are encouraged to leverage their relationship to motivate mothers to care well for their infants; and, 5) the CHW are paid a stipend and only employed half time (as this is the first job for almost all the CHW).
These features appear to the researchers to offer a competitive advantage, but must be empirically evaluated to confirm if they are, in fact, advantageous. The opportunity exists currently as Philani Intervention Model is being diffused to rural South Africa, Ethiopia and Swaziland.
A universal goal for developing interventions in LMIC is sustainability. Africa has particular challenges with broad implementation of effective interventions due to the poorly trained and poorly monitored health personnel. Philani has been operating since the early 1990's. CHW salaries and experience are in line with South African government guidelines and would therefore be sustainable. As the South African government begins to implement a model that targets multiple domains, we have demonstrated a strategy to implement and to evaluate such an intervention. In addition to sustainability, home visits offer a viable strategy to circumvent challenges associated with obtaining healthcare from clinics such as appointment scheduling; long waiting lines; and transport is expensive transport. A CHW approach grounded in cognitive-behavioural skills, with local-tailored content addressing local health risks, strong supervision and accountability be a strategy that is scalable globally. The results of this RCT will be applicable to the existing 1.2 million CHW globally (Singh & Sachs, 2013) to the 50% of Africa that is similarly deeply rural, and responds to the recent Accra Call for Action for global funding at the national level for CHW (One Million Community Health Worker's Campaign).
Supplementary Material
Acknowledgments
Funding: This work was supported by the National Institute on Alcohol Abuse and Alcoholism (R01AA017104, R24AA022919), National Institute of Mental Health (P30MH058107), Ilifa Labantwana, National Institute of Allergy and Infectious Diseases (AI028697), and the National Center for Advancing Translational Science (UL1TR000124). The content is solely the responsibility of the authors and does not necessarily represent the official views of NIH.
Footnotes
Disclosure of Potential Conflicts of Interest: The authors disclose that they have no conflict of interest.
Compliance with Ethical Standards: Ethical Approval: The Institutional Review Boards of University of California Los Angeles (UCLA), Stellenbosch University, and Emory University approved the study. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent: Informed consent was obtained from all individual participants included in the study.
Contributor Information
Mark Tomlinson, Email: markt@sun.ac.za.
Mary Jane Rotheram-Borus, Email: mrotheram@mednet.ucla.edu.
Ingrid M. le Roux, Email: ingridleroux@gmail.com.
Maryann Youssef, Email: mkoussa@mednet.ucla.edu.
Sandahl H. Nelson, Email: sandahln@gmail.com.
Aaron Scheffler, Email: ascheffler@ucla.edu.
Robert E. Weiss, Email: robweiss@ucla.edu.
Carol M. Worthman, Email: worthman@emory.edu.
References
- Aboud FE, Akhter S. A cluster-randomized evaluation of a responsive stimulation and feeding intervention in bangladesh. Pediatrics. 2011;127(5):e1191–1197. doi: 10.1542/peds.2010-2160. [DOI] [PubMed] [Google Scholar]
- Aracena M, Krause M, Pérez C, Méndez MJ, Salvatierra L, Soto M, Altimir C. A cost-effectiveness evaluation of a home visit program for adolescent mothers. Journal of Health Psychology. 2009;14(7):878. doi: 10.1177/1359105309340988.. [DOI] [PubMed] [Google Scholar]
- Black MM, Aboud FE. Response feeding is embedded in a theoretical framework of responsive parenting. Journal of Nutrition. 2011;141(3):490–494. doi: 10.3945/jn.110.129973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bolles K, Speraw C, Berggren G, Lafontant JG. Ti Foyer (hearth) community-based nutrition activities informed by the positive deviance approach in Leogane, Haiti: A programmatic description. Food & Nutrition Bulletin. 2002;23(Supplement 2):9. [PubMed] [Google Scholar]
- Bruner J. Child's talk: Learning to use language. Child Language Teaching and Therapy. 1985;1(1):111–114. [Google Scholar]
- Campbell C, Scott K. Retreat from Alma Ata? The WHO's report on Task Shifting to community health workers for AIDS care in poor countries. Global Public Health. 2011;6(2):125. doi: 10.1080/17441690903334232. [DOI] [PubMed] [Google Scholar]
- Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression - Development of the 10-item Edinburgh Postnatal Depression Scale. British Journal of Psychiatry. 1987;150(Journal Article):782–786. doi: 10.1192/bjp.150.6.782. [DOI] [PubMed] [Google Scholar]
- Dawson DA, Grant BF, Stinson FS. The AUDIT-C: screening for alcohol use disorders and risk drinking in the presence of other psychiatric disorders. Comprehensive Psychiatry. 2005;46(6):405–416. doi: 10.1016/j.comppsych.2005.01.006. [DOI] [PubMed] [Google Scholar]
- de Onis M, Blossner M. The World Health Organization Global Database on Child Growth and Malnutrition: methodology and applications. International Journal of Epidemiology. 2003;32(Journal Article):518–526. doi: 10.1093/ije/dyg099. [DOI] [PubMed] [Google Scholar]
- Deane FP, Leathem J, Spicer J. Clinical Norms, Reliability and Validity for the Hopkins Symptom Checklist-21. Australian Journal of Psychology. 1992;44(1):21–25. doi: 10.1080/00049539208260158. [DOI] [Google Scholar]
- Derogatis LR, Lipman RS, Rickels K, Uhlenhuth EH, Covi L. The Hopkins Symptom Checklist (HSCL): A self-report symptom inventory. Behavioral Science. 1974;19(1):1–15. doi: 10.1002/bs.3830190102. [DOI] [PubMed] [Google Scholar]
- Dunn LM. Peabody picture vocabulary test. Circle Pines, MN: American Guidance Service; 1965. [Google Scholar]
- Engle PL, Black MM. The effect of poverty on child development and educational outcomes. Annals of the New York Academy of Sciences. 2008;1136:243–256. doi: 10.1196/annals.1425.023. [DOI] [PubMed] [Google Scholar]
- Flay BR, Biglan A, Boruch RF, Castro FG, Gottfredson D, Kellam S, et al. Ji P. Standards of evidence: criteria for efficacy, effectiveness and dissemination. Prevention Science. 2005;6(3):151–175. doi: 10.1007/s11121-005-5553-y. Retrieved from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=16365954. [DOI] [PubMed] [Google Scholar]
- Gertler P, Heckman J, Pinto R, Zanolini A, Vermeersch C, Walker S, et al. Grantham-McGregor S. Labor market returns to an early childhood stimulation intervention in Jamaica. Science. 2014;344(6187):998–1001. doi: 10.1126/science.1251178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grantham-McGregor SM, Powell CA, Walker SP, Himes JH. Nutritional supplementation, psychosocial stimulation, and mental development of stunted children: The Jamaican Study. The Lancet. 1991;338(338):1. doi: 10.1016/0140-6736(91)90001-6. [DOI] [PubMed] [Google Scholar]
- Heckman JJ. Lessons from the Bell Curve. Journal of Political Economy. 1995;103(5):1091–1120. doi: 10.1086/262014. [DOI] [Google Scholar]
- Heckman JJ. Skill formation and the economics of investing in disadvantaged children. Science. 2006;312(5782):1900–1902. doi: 10.1126/science.1128898. [DOI] [PubMed] [Google Scholar]
- Kalembo FW, Zgambo M. Loss to followup: a major challenge to successful implementation of prevention of mother-to-child transmission of HIV-1 programs in Sub-Saharan Africa. ISRN AIDS. 2012;2012(Journal Article):598817. doi: 10.5402/2012/589817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawrie TA, Hofmeyr GJ, de Jager M, Berk M. Validation of the Edinburgh Postnatal Depression Scale on a cohort of South African women. The South African Medical Journal. 1998;88(10):1340–1344. [PubMed] [Google Scholar]
- le Roux IM, Tomlinson M, Harwood JM, O'Connor M, Worthman CM, Mbewu N, Rotheram-Borus MJ. Outcomes of Home Visits for Pregnant Mothers and their Infants: a Cluster Randomised Controlled Trial. Aids. 2013;27(9):1461. doi: 10.1097/QAD.0b013e3283601b53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marmot M, Friel S, Bell R, Houweling TA, Taylor S, Health CoSDo. Closing the gap in a generation: health equity through action on the social determinants of health. Lancet. 2008;372(9650):1661–1669. doi: 10.1016/S0140-6736(08)61690-6. [DOI] [PubMed] [Google Scholar]
- Maselko J, Sikander S, Bhalotra S, Bangash O, Ganga N, Mukherjee S, et al. Rahman A. Effect of an early perinatal depression intervention on long-term child development outcomes: follow-up of the Thinking Healthy Programme randomised controlled trial. Lancet Psychiatry. 2015;2(7):609–617. doi: 10.1016/S2215-0366(15)00109-1. [DOI] [PubMed] [Google Scholar]
- Michalopoulos C, Lee H, Duggan A, Lundquist E, Tso A, Crowne SS, et al. Knox V. The Mother and Infant Home Visiting Program Evaluation: Early Findings on the Maternal, Infant, and Early Childhood Home Visiting Program. ACF Web Report. 2015 Retrieved from http://www.acf.hhs.gov/sites/default/files/opre/mihope_report_to_congress_final_1.pdf.
- Nahar B, Hossain MI, Hamadani JD, Ahmed T, Grantham-McGregor S, Persson LA. Effects of psychosocial stimulation on improving home environment and child-rearing practices: results from a community-based trial among severely malnourished children in Bangladesh. BMC Public Health. 2012;12(1):622. doi: 10.1186/1471-2458-12-622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olds DL, Kitzman H, Knudtson MD, Anson E, Smith JA, Cole R. Effect of home visiting by nurses on maternal and child mortality: results of a 2-decade follow-up of a randomized clinical trial. JAMA pediatrics. 2014;168(9):800. doi: 10.1001/jamapediatrics.2014.472.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- One Million Community Health Worker's Campaign. Financing Community Health Worker Systems at Scale in sub-Saharan Africa: Workshop Report. Retrieved from http://1millionhealthworkers.org/files/2015/09/1mCHW_SSC_Workshop_Report_External_2015-09-10_Final.compressed-1.pdf.
- Pakendorf C, Alant E. Culturally valid assessment tools: northern Sotho translation of the Peabody Picture Vocabulary Test-Revised. The South African journal of communication disorders. 1996;44(Journal Article):3–12. [PubMed] [Google Scholar]
- Panter-Brick C, Eggerman M, Tomlinson M. How might global health master deadly sins and strive for greater virtues? Glob Health Action. 2014;7:23411. doi: 10.3402/gha.v7.23411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peacock S, Konrad S, Watson E, Nickel D, Muhajarine N. Effectiveness of home visiting programs on child outcomes: A systematic review. BMC Public Health. 2013;13(1):17. doi: 10.1186/1471-2458-13-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rahman A, Iqbal Z, Roberts C, Husain N. Cluster randomized trial of a parent-based intervention to support early development of children in a low-income country. Child: Care, Health and Development. 2009;35(1):56. doi: 10.1111/j.1365-2214.2008.00897.x. [DOI] [PubMed] [Google Scholar]
- Rotheram-Borus MJ, le Roux IM, Tomlinson M, Mbewu N, Comulada WS, le Roux K, Swendeman D. Philani Plus (+): a Mentor Mother community health worker home visiting program to improve maternal and infants' outcomes. Prevention Science. 2011;12(4):372. doi: 10.1007/s11121-011-0238-1,PMCID:3907085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rotheram-Borus MJ, Richter LM, van Heerden A, van Rooyen H, Tomlinson M, Harwood JM, et al. Stein A. A cluster randomized controlled trial evaluating the efficacy of peer mentors to support South African women living with HIV and their infants. PLoS One. 2014;9(1):e84867. doi: 10.1371/journal.pone.0084867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, de la Fuente JR, Grant M. Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption. Addiction. 1993;88(6):791. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- Singh P, Sachs JD. 1 million community health workers in sub-Saharan Africa by 2015. Lancet. 2013;382(9889):363–365. doi: 10.1016/S0140-6736(12)62002-9. [DOI] [PubMed] [Google Scholar]
- Super CM, Herrera MG, Mora JO. Long-term effects of food supplementation and psychosocial intervention on the physical growth of Colombian infants at risk of malnutrition. Child Dev. 1990;61(1):29–49. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/2307045. [PubMed] [Google Scholar]
- Tomlinson M, Cooper PJ, Stein A, Swartz L, Molteno C. Post-partum depression and infant growth in a South African peri-urban settlement. Child Care Health Dev. 2006;32(1):81–86. doi: 10.1111/j.1365-2214.2006.00598.x. [DOI] [PubMed] [Google Scholar]
- Tomlinson M, Rotheram-Borus MJ, Harwood J, le Roux IM, O'Connor M, Worthman C. Community health workers can improve child growth of antenatally-depressed, South African mothers: a cluster randomized controlled trial. BMC Psychiatry. 2015;15 doi: 10.1186/S12888-015-0606-7. Artn 225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vally Z, Murray L, Tomlinson M, Cooper PJ. The impact of dialogic book-sharing training on infant language and attention: a randomized controlled trial in a deprived South African community. J Child Psychol Psychiatry. 2015;56(8):865–873. doi: 10.1111/jcpp.12352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Victora CG, Adair L, Fall C, Hallal PC, Martorell R, Richter L, et al. Child Undernutrition Study, G. Maternal and child undernutrition: consequences for adult health and human capital. Lancet. 2008;371(9609):340–357. doi: 10.1016/S0140-6736(07)61692-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waber DP, Vuori-Christiansen L, Ortiz N, Clement JR, Christiansen NE, Mora JO, et al. Herrera MG. Nutritional supplementation, maternal education, and cognitive development of infants at risk of malnutrition. Am J Clin Nutr. 1981;34(Suppl 4):807–813. doi: 10.1093/ajcn/34.4.807. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/7223696. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


