Abstract
Background
This study compared the efficacy of combined lateral and medial approach, lateral approach, and anterior medial approach in treatment of terrible triad of the elbow (TTE).
Material/Methods
Thirty-eight TTE patients hospitalized in our center were retrospectively analyzed, among which 14 patients were arranged for combined lateral and medial approach, 12 for lateral approach, and 12 for anterior medial approach. All included patients underwent open reduction, collateral ligament repair, and postoperative function exercise. Follow-up was conducted for 13~22 months. The elbow motion, excellent and good rate, healing time, and complication rate were recorded and compared.
Results
These 3 approaches significantly improved the postoperative elbow motion, MEPS, VAS, excellent and good rate, and open reduction (all P<0.05). The VAS score for lateral approach was evidently higher than that for combined lateral and medial approach (P<0.05). Combined lateral and medial approach and anterior medial approach had better performance on elbow motion, MEPS, and excellent and good rate than lateral approach (both P<0.05). Lateral approach and anterior medial approach had a significantly reduced healing time compared with combined lateral and medial approach (both P<0.05), while anterior medial approach had a higher complication rate compared with anterior medial approach and lateral approach (both P<0.05).
Conclusions
Lateral combined medial surgery approach contributes to wide surgical exposure, facture stability, and decreased complication rate, and thus has superior efficacy than the other 2 surgical approaches.
MeSH Keywords: Amyotrophic Lateral Sclerosis, Anterior Chamber, Elbow
Background
Terrible triad of the elbow (TTE) is known as the dislocation of the elbow in conjunction with fractures of both radial head and the ulnar coronoid [1]. The main mechanism of this injury is the posterior dislocation of the elbow, which may result from a falling on the outstretched hand, with forearm externally rotated [2]. It was reported that TTE accounted for 4% of adult radial head fractures and 31% of elbow dislocations [3]. TTE is characterized by great potential for joint instability and has a relative poor prognosis [4]. Currently, TTE is a challenging injury to manage, with a history of unfavorable complications such as stiffness, instability, pain, and heterotopic ossification [5]. The treatment options for TTE range from closed reduction and non-operative management to surgical treatments using open reduction, external fixation, and internal fixation [6]. It was reported that conservative treatment fails to provide satisfactory overall outcomes, which is often complicated with joint stiffness, elbow instability, and joint osteoarthritis because of immobilization [7], while surgical treatment remains the optimal choice due to its performance on joint stability, anatomical reduction, and early mobility during the postoperative period, thus reducing the risk of postoperative complications [8].
Radial head fixation and arthroplasty, coronoid process fixation, and lateral collateral ligament repair continue to be the mainstays for the treatment of TTE [9]. During the operation, the coronoid fragment should first be fixed and then the radial head needs to be replaced or fixed, followed by repair of the lateral collateral ligament [10]. Currently, both medial and lateral approaches to the coronoid have been popularized in recent literature [11]. A medial surgical approach is advocated when lateral collateral ligament reconstruction or fixation of a large coronoid process fragment is needed, to prevent persistent posterolateral instability [4]. However, in treatment of coronoid fractures, the anterior medial approach is the most commonly used method, which allows for anatomic reduction and stable internal fixation supplemented with screw fixation and buttress plating [12]. Numerous reports have described surgical management of TTE, with no universally accepted surgical approach [8,13]. By grouping TTE patients into those treated with anterior medial approach, lateral approach, or combined lateral and medial approach, we were able to compare the outcomes of these 3 surgical approaches. The present study was conducted to compare the function evaluation, complications, and healing time of anterior medial approach, lateral approach, and combined lateral and medial approach in the treatment of TTE.
Material and Methods
Subjects
We retrospectively analyzed data from 38 TTE patients admitted in Yiwu Central Hospital, Affiliated Hospital of Wenzhou Medical University between January 2010 and January 2015. Among the 38 included subjects, 14 were treated with combined lateral and medial approach, 12 with lateral approach, and 12 with anterior medial approach. According to the Regan-Morrey classification standard, ulna coronary fractures were classified into the following types: type I, avulsion of the tip of the fracture (a fracture of <10% of the coronoid height); type II, a single or comminuted fragment that involves more than just the tip but ≤50% of the coronoid height; and type III, a fragment involving more than 50% of the process [14]. The classifications of radial head fracture were based on Mason-Johnston classification: type I, flap fracture in radial head (<25%); type II, re-constructible fracture; type III, un-reconstructible fracture; and type IV, fracture of radial head complicated with dislocation of the elbow joint [15]. The inclusion criteria for subjects were: (1) patients hospitalized in our hospital who could tolerate surgery; (2) patients older than 18 years who could cooperate with treatment and observation; (3) patients with no past history of elbow fracture and had previously had normal elbow function; (4) patients had a fresh fracture and had received timely treatment; and (5) patients were diagnosed with TTE by frontal and lateral X-ray and CT examination, and confirmed by indications for surgical treatment. The exclusion criteria were: (1) patients with old fractures; (2) the fracture was not caused by high energy trauma, such as car accident, falling from high places, or fall injuries; (3) patients complicated with primary diseases, such as psychosis, cardio-cerebrovascular disease, or diabetes mellitus; (4) patients had distal humerus fracture, olecranon fracture, or fracture of shaft of radius and ulna. This study was carried out with the permission of Ethics Committee of Yiwu Central Hospital, Affiliated Hospital of Wenzhou Medical University, and all patients signed written informed consent prior to the study.
Surgical approaches
The selection criteria on surgical approach were determined by fracture type, the degree of soft tissue injuries, and treatment level. Lateral approach was applied in radial head replacement. For those patients who did not receive radial head replacement, posterior approach was used to separate medial and lateral fascia flap. When severe ulnar coracoid process fracture or valgus deformity of the elbow after fixation by lateral approach or ulnar nerve injury occurred, the medial approach was used.
The patients were placed in a decubitus position under regional anesthesia of the brachial plexus with the fractured arms over the chest. The surgery approach was selected based on their injuries. (1) Combined lateral and medial approach group: lateral approach was performed along with the lateral epicondyle of humerus between triceps and brachioradialis. Then the lateral elbow and collateral ligament were exposed after the anconeus was separated from the extensor carpi ulnaris (ECU). An incision on deep fascia in the lateral epicondyle of humerus was performed to protect the ulnar nerve and then the beginning part of the flexor was cut and dragged for the exposure of deep medial collateral ligament (MCL). (2) Lateral approach: an incision was made along the lateral epicondyle of the humerus between triceps and brachioradialis, which was extended to the anconeus and ECU for the exposure of lateral collateral ligament and joint capsule. (3) Anterior medial approach: 2 cm distal to cubital cross striation, a 6-cm arc incision was made. The lateral antebrachial cutaneous nerve was well protected while the anterior elbow capsule was exposed and cut for the exposure of humeral head and radial head. Then the brachialis was cleaved along with the muscle fiber to expose coronoid process fractures and humeral trochlea.
Restorative procedure
After the surgery approaches were performed, the damaged lesions were exposed. The restorative procedure was conducted initially with internal fixation (ulna coracoid process fractures first, then radial head fractures), followed by reconstruction of the lateral collateral ligament (lateral collateral ligament of the elbow joint first, then MCL of elbow joint). (1) Fixation of coronal fracture: reduction and fixation was performed using 1.0 mm Kirschner wire (Arthrex, San Francisco, USA) for type I fractures, 1~2 titanium screws with diameter of 3 mm (Arthrex, San Francisco, USA) for type II~III fractures. (2) Fixation of head of radius fracture: 1~2 absorbable screws with diameter of 2 mm (Arthrex, San Francisco, USA) was used to secure a safety zone with nail tail parallel with facies ossea for type I~II fractures. Type III fracture was fixed by 1.5 mm Kirschner wire after general fixation. Type IV fracture underwent plate fixation and the plate was placed in the 1/3 of head of radius to ensure forearm rotation. After the fixation was performed, a C-arm X-ray machine was used for examination and confirmation. (3) Lateral collateral ligament repair: the torn part of the lateral collateral ligament of the elbow was stitched with non-absorbable sutures. If the lesions of lateral collateral ligament were exposed again, the same procedure of ligament repair was performed again.
Postoperative care
Antibiotics (Harbin Pharmaceutical Group holding Co., Ltd., Harbin, China) were regular used to avoid infection and indomethacin (25 mg) was given taken 3 times a day to avoid heterotopic ossification. After surgery, the elbow was bent at 90° and the forearm was fixed using a plaster slab in neutral position. Seven to ten days after surgery, negative exercises, such as flexion and extension of elbow joint and forearm rotation, were conducted. Then the plaster slab was removed to allow positive activities, including flexion and extension of the elbow joint and forearm rotation 3–4 weeks after surgery. The extend elbow range was limited to no more than 150° within 6 weeks after the surgery.
Follow-up and therapeutic evaluation
Follow-up lasted 15 months and no case was lost during follow-up. The follow-up was conducted at postoperative weeks 1 and 2 and t postoperative months 1 and 3, and once every 3 months thereafter. The data, including bone fracture healing recorded by X-ray and the healing time (started counting from 1 day after surgery to no fracture line visible), were collected for each patient. At the end of the follow-up, the motion range of elbow joint flexion and extension and forearm rotation for each patient were recorded using a gravity-activated goniometer (Changzhou Rehabilitation medical factory, Changzhou, China). The evaluation of elbow joint function was assessed based on the Mayo Elbow Performance Score (MEPS), including pain (45 points), range of motion of the elbow joint (20 points), elbow stability (10 points), and ability to perform activities of daily living (25 points) [16]. A final score of more than 90 points was regarded as excellent, 75~89 as good, 60~74 as acceptable, and less than 60 as poor. A visual analogue scale (VAS) was used for evaluation, ranging from 0~10 points, with a higher score indicating more severe pain [17]. X-ray film was also observed to record internal fixation loosening, heterotopic ossification, fracture reduction, complications, and complication rate.
Statistical analysis
SPSS 20.0 software was used for data analysis. Continuous data are expressed as mean ± standard deviation (SD) and compared by t test between 2 groups or variance analysis among multiple groups. Categorical data are presented with percentage or rate, which were compared using chi-square test. P value less than 0.05 was considered as statistical significance.
Results
Baseline characteristics
As shown in Table 1, no significant differences were found in sex, mean age, BMI, fracture causes, unilateral factures, average facture time, ulna coronary fractures I~III, radial head fractures I~IV, average surgery time, immobilization time of the facture arm, hospitalization time, or elbow motion among the 3 different approaches (all P>0.05). The average volume of blood loss in lateral approach patients was not significantly different from that in anterior medical approach patients (P>0.05), both of which were significantly lower compared with combined lateral and medial approach (both P<0.05).
Table 1.
Baseline characteristics for patients included in lateral approach group, anterior medial approach group, and combined lateral and medial approach group.
| Items | Combined lateral and medial approach group (n=14) | Lateral approach group (n=12) | Anterior medial approach group (n=12) | F/χ2 | P |
|---|---|---|---|---|---|
| Sex (male/female) | 9/5 | 8/4 | 7/5 | 0.19 | 0.909 |
| Age (years) | 36.62±2.5 | 37.12±3.1 | 37.28±2.9 | 0.196 | 0.823 |
| BMI (kg/m2) | 20.8±1.9 | 22.0±1.9 | 20.7±1.8 | 1.829 | 0.176 |
| Fracture causes | |||||
| Car accident | 5 | 3 | 3 | ||
| Falling injury | 6 | 4 | 3 | 2.599 | 0.627 |
| Fall from high places | 3 | 5 | 6 | ||
| Lateral fracture | |||||
| Left side | 8 | 7 | 6 | 0.2 | 0.905 |
| Right side | 6 | 5 | 6 | ||
| Mean injury time (d) | 4.6±1.7 | 4.8±1.6 | 5.0±2.1 | 0.148 | 0.863 |
| Regan-Morrey types | |||||
| I | 3 | 5 | 3 | ||
| II | 8 | 4 | 5 | 2.16 | 0.706 |
| III | 3 | 3 | 4 | ||
| Mason types | |||||
| I | 2 | 2 | 3 | ||
| II | 8 | 6 | 6 | 0.644 | 0.958 |
| III | 4 | 4 | 3 | ||
| IV | 0 | 0 | 0 | ||
| Mean surgery time (min) | 81.41±26.54 | 79.25±23.16 | 83.36±26.41 | 0.078 | 0.925 |
| Intraoperative blood loss (ml) | 209.60±49.08 | 154.47±20.25# | 158.18±19.39# | 11.02 | <0.001 |
| Immobilization time (week) | 3.6±1.3 | 3.4±1.6 | 3.5±1.5 | 0.056 | 0.945 |
| Postoperative hospitalization time (months) | 3.5±1.5 | 3.4±0.8 | 3.7±1.1 | 0.19 | 0.828 |
| Elbow motion | |||||
| Flexion and extension (°) | 62.4±8.6 | 63.3±7.9 | 65.1±7.6 | 0.368 | 0.695 |
| Forearm rotation (°) | 72.5±5.5 | 73.6±5.9 | 75.0±5.2 | 0.661 | 0.523 |
BMI – body mass index.
Compared with combined lateral and medial approach, P<0.05.
Comparisons of the range of elbow joint motion
Elbow joint motion records before surgery and after follow-up for patients undergoing anterior medical approach, lateral approach, and combined lateral and medial approach are presented in Table 2. TTE patients who received surgical treatments using anterior medical approach, lateral approach, or combined lateral and medial approach all showed significant improvement in flexion and extension elbow motion and forearm rotation (all P<0.05). The flexion and extension range of elbow joint motion and forearm rotation between anterior medial approach and combined lateral and medial approach were not significantly different (all P>0.05), and both of which were remarkably improved compared with lateral approach (both P<0.05).
Table 2.
Comparisons of elbow joint motion among lateral approach, anterior medial approach, and combined lateral and medial approach.
| Items | Combined lateral and medial approach group (n=14) | Lateral approach group (n=12) | Anterior medial approach group (n=12) | F | P |
|---|---|---|---|---|---|
| Flexion and extension | |||||
| Before surgery | 62.4±8.6 | 63.3±7.9 | 65.1±7.6 | 0.371 | 0.693 |
| After surgery | 116.0±10.2* | 98.3±5.9*# | 113.4±10.9*& | 16.04 | <0.001 |
| Forearm rotation | |||||
| Before surgery | 72.5±5.5 | 71.6±5.9 | 75.0±5.2 | 1.23 | 0.306 |
| After surgery | 119.6±12.5* | 101.4±8.3*# | 126.0±18.4*& | 10.55 | <0.001 |
Compared with before surgery, P<0.05.
Compared with combined lateral and medial approach, P < 0.05.
Compared with lateral approach, P<0.05.
Comparisons of MEPS, VAS, and excellent and good rate
The comparisons of MEPS, VAS, and excellent and good rate among the 3 approaches are shown in Table 3. Compared with preoperative MEPS, the postoperative MEPS in patients undergoing anterior medical approach, lateral approach, or combined lateral and medial approach were notably improved (all P<0.05). The MEPS for lateral approach was significantly lower than anterior medical approach and lateral combined with medical approach (both P<0.05), while the comparison between anterior medical approach and lateral combined medical approach was not statistically significant (P>0.05). The postoperative VAS for these 3 approaches were significantly lower compared with preoperative VAS (P<0.05). The VAS score for lateral approach was evidently higher than that for combined lateral and medial approach (P<0.05).
Table 3.
Comparisons on MEPS, VAS, and excellent and good rate among lateral approach, anterior medial approach, and combined lateral and medial approach.
| Items | Combined lateral and medial approach group (n=14) | Lateral approach group (n=12) | Anterior medial approach group (n=12) | F | P |
|---|---|---|---|---|---|
| MEPS | |||||
| Before surgery | 51.2±5.3 | 53.4±6.1 | 49.8±5.6 | 1.19 | 0.317 |
| After surgery | 98.3±7.2* | 87.4±6.5*# | 98.3±5.1*& | 11.98 | <0.001 |
| VAS | |||||
| Before surgery | 4.7±1.8 | 5.1±1.9 | 4.8±1.7 | 0.25 | 0.78 |
| After surgery | 0.8±0.6* | 1.7±0.8*# | 1.2±1.0* | 4.03 | 0.026 |
| Excellent and good rate | |||||
| After surgery (%) | 92.90% | 50.0%# | 90.9%& | 9.75 | 0.04 |
| Excellent | 10 | 2 | 5 | ||
| Good | 3 | 4 | 5 | ||
| Acceptable | 1 | 6 | 2 | ||
Compared with before surgery, P<0.05.
Compared with combined lateral and medial approach, P < 0.05.
Compared with lateral approach, P<0.05.
MEPS – mayo elbow performance Score; VAS – visual analogue scale.
Comparisons on X-ray film measurements for fracture
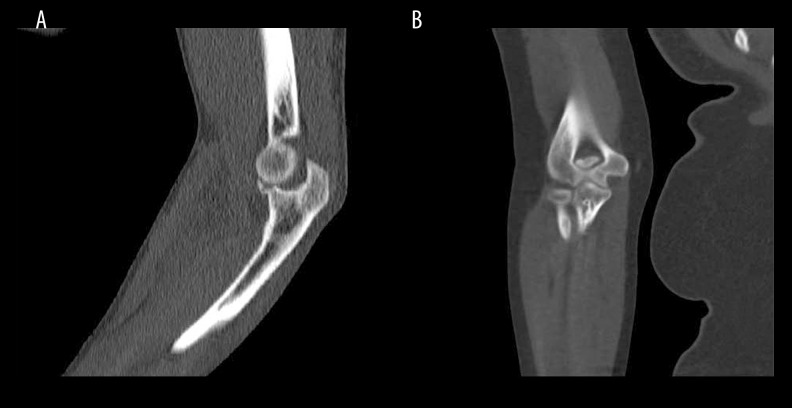
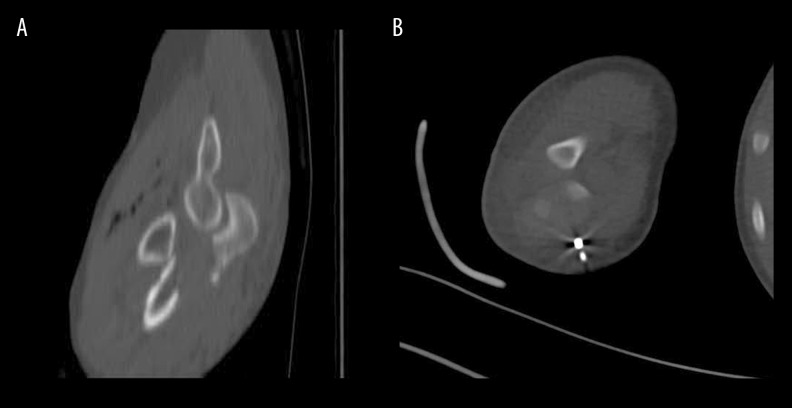
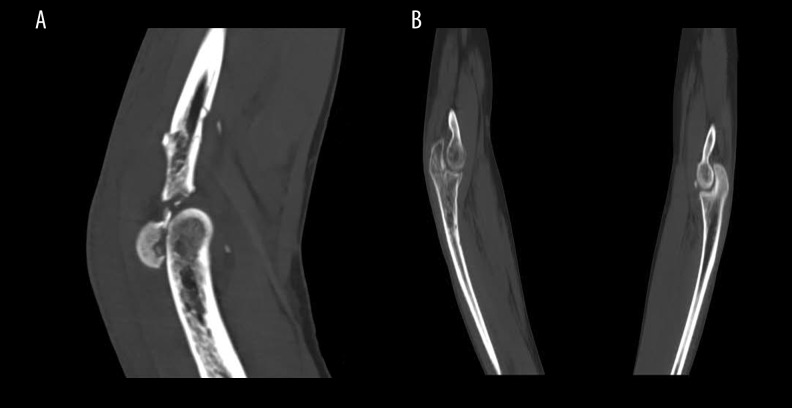
At the end of the follow-up, all patients achieved good facture healing and fracture reduction. No heterotopic ossification or elbow dislocation was observed. Compared with the preoperative CT image, the postoperative CT image showed remarkable improvement for all 3 approaches (Figures 1–3).
Figure 1.
The preoperative and postoperative CT image for a representative patient who underwent combined lateral and medial surgical approach (A, anteroposterior radiograph before surgery; B, anteroposterior radiograph after surgery).
Figure 2.
The preoperative and postoperative CT image for a representative patient who underwent lateral surgical approach (A, anteroposterior radiograph before surgery; B, anteroposterior radiograph after surgery).
Figure 3.
The preoperative and postoperative CT image for a representative patient who underwent anterior medial surgical approach (A, anteroposterior radiograph before surgery; B, anteroposterior radiograph after surgery).
Comparisons of healing time and complications
The healing time and complications for these 3 approaches are presented in Table 4. Both lateral approach and anterior medical approach had shorter healing times compared with combined lateral and medical approach (both P<0.05), while no significant difference was detected between lateral approach and anterior medical approach (P>0.05). The complication rates in lateral approach and combined lateral and medial approach were not significantly different (P>0.05). Both lateral approach and lateral combined medical approach had lower complication rate than that in anterior medical approach (both P<0.05).
Table 4.
Comparisons on healing time and complications among lateral approach, anterior medial approach, and combined lateral and medial approach.
| Items | Combined lateral and medial approach group (n=14) | Lateral approach group (n=12) | Anterior medial approach group (n=12) | F | P |
|---|---|---|---|---|---|
| Healing time (week) | 13.33±2.58 | 9.48±1.73# | 11.03±2.15# | 10.09 | <0.001 |
| Complication rate (%) | 7.10% | 8.30% | 50.0%#& | 8.195 | 0.033 |
| Delayed ulnar neuritis | 0 | 1 | 3 | ||
| Late ulnar nerve palsy | 1 | 0 | 3 |
Compared with combined lateral and medial approach, P<0.05.
Compared with lateral approach, P<0.05.
Discussion
We investigated the influence of different surgery approaches on TTE and our results showed that these three approaches – lateral approach, anterior medial approach, and combined lateral and medial approach – were all effective in treating TTE based on our results observed in elbow motion, MEPS, VAS, excellent and good rate, and CT images. After pair-wise comparisons among the 3 approaches, our results demonstrated that combined lateral and medial approach was associated with adequate surgical exposure, efficient management of elbow stability, and significantly reduced complications, compared with lateral approach and anterior medial approach. Our results show that those 3 different approaches contributed to TTE improvement after the operation was performed, indicating that operations for TTE were associated with better performance and significant elbow repair function compared with conservative treatment. The conservative treatment for TTE was reported to have a rather high dislocation rate due to the persistent instability [18]. TTE can lead to severe elbow instability and often carries a poor prognosis, thus surgery should be advocated to restore the anatomic structures, to repair the collateral ligament, to avoid immobilization, and to restore articular function [19]. Consistent with our results, previous evidence shows that excellent results of treatment have been reported with the improved surgical strategies for TTE [8].
Regarding elbow motion range, MEPS, and excellent and good rate, our results demonstrated that anterior medial approach and combined lateral and medial approach had better overall management compared with lateral approach, suggesting that lateral approach may lead to poor stability of the elbow, resulting in poor functional outcome. It has been reported that repair of the MCL is of great importance in treatment of elbow fracture-dislocation and MCL may play an import role in valgus stability of the elbow [5]. A previous study showed that restoration of the damaged structures, including medial soft tissue structures, indicates excellent results based on MEPS in patients with TTE [20]. In TTE, the lateral collateral ligament, MCL, and anterior capsule are usually torn and soft tissues were injured, all of which are important determinants of elbow stability [21]. Our results show that lateral approach alone may not as beneficial as the other 2 approaches in terms of joint stability of the elbow, while the operation using anteromedial combined lateral approach has advantages of providing both bone and soft-tissue stability simultaneously, allowing early exercise and improving early functional recovery in TTE treatment [22].
Our results also demonstrated that combined lateral and medial approach had a longer healing time compared with lateral approach and anterior medial approach, suggesting that lateral combined surgical approach may not be the best choice for TTE recovery in terms of healing time. This result is consistent with findings of a previous study showing that the lateral approach or medial window provide with a much wider surgical space for the coronoid fractures, even without damaged MCLs, and common flexor masses can be easily repaired [20]. This is reasonable since combined lateral and medial approach involves a much more complicated surgical process. In addition, the VAS score for lateral approach was clearly higher than that for combined lateral and medial approach. During the TTE operation, lateral approaches are useful in addressing pathology at the radial head, coronoid process, and anterior and posterior capsules, while medial approach is effective in addressing ulnar nerve, the anterior and posterior capsules, and the coronoid process [23]. Although the combined lateral and medial approach may be associated with longer recovery time, this approach was able to restore anterior and lateral lesions, as well as medial lesion in TTE tissue, and use of the lateral approach may not be able to remove all the small bone fragments [20].
Our study also compared the complication rate among the 3 surgical approaches in TTE patients. We found that the anterior medial approach had a higher complication rate compared with lateral approach and combined lateral and medial approach. Our results indicate that anterior medial approach may be associated with motion deficits in TTE. Moreover, it was reported that most TTE patients achieved satisfactory results without using a medial approach [6]. Instead of anteromedial approach, a previous study revealed that combination of lateral approach and anteromedial approach is an effective method for TTE treatment [5]. Moreover, evidence also suggests that some TTE injuries can be successfully managed with superficial stabilization via the lateral surgical approach, with a low complication rate [24]. It was reported that a medial-incision approach for coronoid fixation may be more extensive since it requires partial detachment or splitting of the flexor-pronator musculature, resulting in more surgical trauma and therefore increasing the risk of additional complications, such as ectopic bone formation [25].
Conclusions
Our study demonstrates that the 3 surgical approaches – lateral approach, anterior medial approach, and combined lateral and medial approach – each have their own merits, but combined lateral and medial surgery may be the best approach. However, the credibility of our study was restrained by the limited numbers of included subjects, and may have lacked sufficient power to detect significant differences. Therefore, further research is needed to determine the best surgical approach in patients with TTE.
Footnotes
Source of support: Departmental sources
Competing interests
None.
References
- 1.Chen HW, Liu GD, Ou S, et al. Operative treatment of terrible triad of the elbow via posterolateral and anteromedial approaches. PLoS One. 2015;10:e0124821. doi: 10.1371/journal.pone.0124821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.de Aquino Santos A, Tonelli TA, Matsunaga FT, et al. Result from surgical treatment on the terrible triad of the elbow. Rev Bras Ortop. 2015;50:403–8. doi: 10.1016/j.rboe.2015.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bohn K, Ipaktchi K, Livermore M, et al. Current treatment concepts for “terrible triad” injuries of the elbow. Orthopedics. 2014;37:831–37. doi: 10.3928/01477447-20141124-06. [DOI] [PubMed] [Google Scholar]
- 4.Chemama B, Bonnevialle N, Peter O, et al. Terrible triad injury of the elbow: How to improve outcomes? Orthop Traumatol Surg Res. 2010;96:147–54. doi: 10.1016/j.rcot.2010.02.008. [DOI] [PubMed] [Google Scholar]
- 5.Zhang C, Zhong B, Luo CF. Treatment strategy of terrible triad of the elbow: experience in Shanghai 6th People’s Hospital. Injury. 2014;45:942–48. doi: 10.1016/j.injury.2013.12.012. [DOI] [PubMed] [Google Scholar]
- 6.Leigh WB, Ball CM. Radial head reconstruction versus replacement in the treatment of terrible triad injuries of the elbow. J Shoulder Elbow Surg. 2012;21:1336–41. doi: 10.1016/j.jse.2012.03.005. [DOI] [PubMed] [Google Scholar]
- 7.Hill L. Hepatitis C virus direct-acting antiviral drug interactions and use in renal and hepatic impairment. Top Antivir Med. 2015;23:92–96. [PMC free article] [PubMed] [Google Scholar]
- 8.Mathew PK, Athwal GS, King GJ. Terrible triad injury of the elbow: Current concepts. J Am Acad Orthop Surg. 2009;17:137–51. doi: 10.5435/00124635-200903000-00003. [DOI] [PubMed] [Google Scholar]
- 9.Chen NC, Ring D. Terrible triad injuries of the elbow. J Hand Surg Am. 2015;40:2297–303. doi: 10.1016/j.jhsa.2015.04.039. [DOI] [PubMed] [Google Scholar]
- 10.Rodriguez-Martin J, Pretell-Mazzini J, Andres-Esteban EM, Larrainzar-Garijo R. Outcomes after terrible triads of the elbow treated with the current surgical protocols. A review. Int Orthop. 2011;35:851–60. doi: 10.1007/s00264-010-1024-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Reichel LM, Milam GS, Reitman CA. Anterior approach for operative fixation of coronoid fractures in complex elbow instability. Tech Hand Up Extrem Surg. 2012;16:98–104. doi: 10.1097/BTH.0b013e31824e6a74. [DOI] [PubMed] [Google Scholar]
- 12.Kang LQ, Ding ZQ, Sha M, et al. A minimally invasive anterior approach to reduction and screw fixation of coronoid fractures. J Hand Surg Eur Vol. 2010;35:224–27. doi: 10.1177/1753193409352285. [DOI] [PubMed] [Google Scholar]
- 13.Dodds SD, Fishler T. Terrible triad of the elbow. Orthop Clin North Am. 2013;44:47–58. doi: 10.1016/j.ocl.2012.08.006. [DOI] [PubMed] [Google Scholar]
- 14.Regan W, Morrey B. Fractures of the coronoid process of the ulna. J Bone Joint Surg Am. 1989;71:1348–54. [PubMed] [Google Scholar]
- 15.Mason ML. Some observations on fractures of the head of the radius with a review of one hundred cases. Br J Surg. 1954;42:123–32. doi: 10.1002/bjs.18004217203. [DOI] [PubMed] [Google Scholar]
- 16.Ring D, Jupiter JB, Zilberfarb J. Posterior dislocation of the elbow with fractures of the radial head and coronoid. J Bone Joint Surg Am. 2002;84-A:547–51. doi: 10.2106/00004623-200204000-00006. [DOI] [PubMed] [Google Scholar]
- 17.Solarino G, Vicenti G, Abate A, et al. Mason type II and III radial head fracture in patients older than 65: Is there still a place for radial head resection? Aging Clin Exp Res. 2015;27(Suppl 1):S77–83. doi: 10.1007/s40520-015-0425-1. [DOI] [PubMed] [Google Scholar]
- 18.Sorensen AK, Sojbjerg JO. Treatment of persistent instability after posterior fracture-dislocation of the elbow: Restoring stability and mobility by internal fixation and hinged external fixation. J Shoulder Elbow Surg. 2011;20:1300–9. doi: 10.1016/j.jse.2011.06.002. [DOI] [PubMed] [Google Scholar]
- 19.Chen S, Huang F, Hu X, et al. [Operative treatment of terrible triad of the elbow]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2009;23:45–48. [in Chinese] [PubMed] [Google Scholar]
- 20.Jeong WK, Oh JK, Hwang JH, et al. Results of terrible triads in the elbow: The advantage of primary restoration of medial structure. J Orthop Sci. 2010;15:612–19. doi: 10.1007/s00776-010-1515-8. [DOI] [PubMed] [Google Scholar]
- 21.Micic I, Kim SY, Park IH, et al. Surgical management of unstable elbow dislocation without intra-articular fracture. Int Orthop. 2009;33:1141–47. doi: 10.1007/s00264-008-0624-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Du JF, Zhu YY. [Treatment of terrible triad of elbow with open reduction and internal fixation through anteromedial approach combined with lateral approach]. Zhongguo Gu Shang. 2014;27:896–99. [in Chinese] [PubMed] [Google Scholar]
- 23.Cheung EV, Steinmann SP. Surgical approaches to the elbow. J Am Acad Orthop Surg. 2009;17:325–33. doi: 10.5435/00124635-200905000-00007. [DOI] [PubMed] [Google Scholar]
- 24.Winter M, Chuinard C, Cikes A, et al. Surgical management of elbow dislocation associated with non-reparable fractures of the radial head. Chir Main. 2009;28:158–67. doi: 10.1016/j.main.2009.02.003. [DOI] [PubMed] [Google Scholar]
- 25.Abrams GD, Bellino MJ, Cheung EV. Risk factors for development of heterotopic ossification of the elbow after fracture fixation. J Shoulder Elbow Surg. 2012;21:1550–54. doi: 10.1016/j.jse.2012.05.040. [DOI] [PubMed] [Google Scholar]