In this series we draw attention to medicines that have entered the European market with an entirely new mechanism of action. Publication is not to be confused with endorsement of use in clinical practice. Copyright to the images belongs to Leiden University, but use of the images (also available at http://coo.lumc.nl/trc and the app stores) is free.
Introduction
Chronic hepatitis C infection is a major cause of chronic liver disease, cirrhosis and liver cancer as well as an important indication for liver transplantation. Sofosbuvir (Sovaldi®) 1 and daclatasvir (Daklinza®) 2 are new direct acting antivirals (DAAs) with a favourable safety and tolerability profile, which have significantly changed treatment for this condition.
Mechanism
After entering hepatocytes, the viral genome of the hepatitis C virus (HCV) is translated into a single polypeptide. This polypeptide is subsequently cleaved into viral proteins, including non‐structural (NS) proteins NS3, NS4A, NS5B and NS5B RNA dependent RNA polymerase (Figure 1) 3, 4. These viral proteins are essential for viral replication and assembly making them significant targets for therapy. Sofosbuvir is the first available inhibitor of NS5B RNA dependent RNA polymerase. Daclatasvir is an inhibitor of NS5B.
Figure 1.
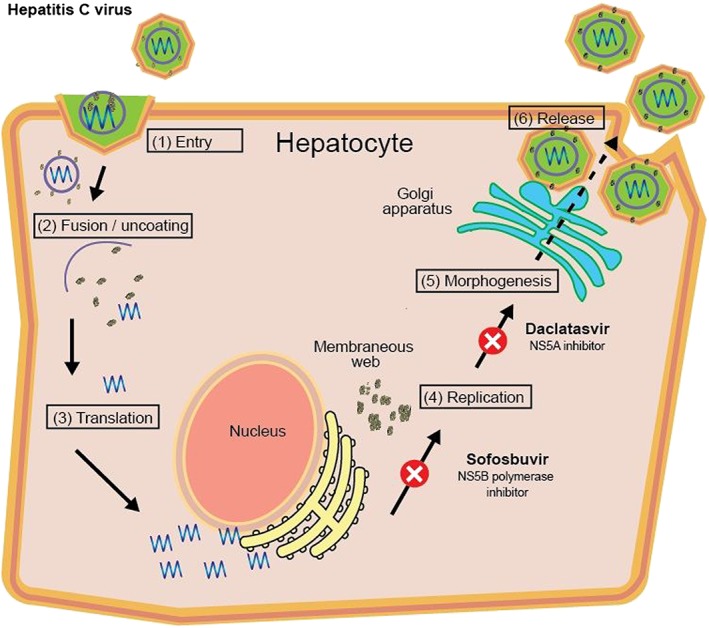
Mechanism of action of sofosbuvir and daclatasvir 3, 4. After entering hepatocytes, the viral genome of HVC is translated into a single polypeptide which is subsequently cleaved into viral proteins that are essential for HVC replication and viral assembly. Sofosbuvir inhibits NS5B RNA dependent RNA polymerase and daclatasvir is an inhibitor of NS5B, both inducing disruption of viral replication
Indication
Sofosbuvir has activity against all six major HCV genotypes and stops HCV from multiplying and infecting new cells 5, 6, 7. Daclatasvir is effective against genotype 1–4 7, 8. Sofosbuvir is used in combination with peginterferon and/or ribavirin but is also approved for use without interferon treatment, in combination with daclatasvir with or without ribavirin 5, 6, 7, 8.
Clinical application
The goal of HCV treatment is to obtain a sustained virologic response (SVR), classically defined as undetectable HCV RNA 12 weeks or more following treatment completion. Until 2011, HCV was treated by a combination of peginterferon and ribavirin. This dual therapy achieves SVR rates of 40–80%, but the response is genotype dependent and associated with significant side effects. The approval of sofosbuvir offered the first possibility for complete oral regimes of DAAs. Compared with the first generation protease inhibitors (telaprivir and boceprevir), sofosbuvir has easier dosing regimens, lower toxicity and fewer drug–drug interactions. It is highly effective and safe for the treatment of chronic hepatitis C infected patients, even those who are difficult to treat because of cirrhosis 5, 6, 7. However, DAAs should not be administrated as monotherapy because this may lead to drug‐resistance. Several clinical trials with sofosbuvir in combination with peginterferon and ribavirin have demonstrated overall efficacy rates of 50–93% 5, 6, while patients with genotype 2 and 3 treated with a combination of sofosbuvir and daclatasvir demonstrated a SVR of 94–100% 8, 9. The approval of these compounds has led to significant revisions of the chronic hepatitis C treatment guidelines in the USA and Europe.
Adverse effects
Sofosbuvir and daclatasvir are generally well tolerated with only a few adverse effects reported. The most common side effects reported with sofosbuvir in combination with daclatasvir are fatigue, nausea, headache and insomnia. Sofosbufir is a substrate of the glycoprotein (P‐gp) transporter and daclatasvir is a substrate of CYP3A4 and P‐gp. Co‐administration with enzymes which induce or inhibit these pathways may be best avoided or necessitate dose adjustments.
Competing Interests
All authors have completed the Unified Competing Interest form at http://www.icmje.org/coi_disclosure.pdf (available on request from the corresponding author) and declare no support from any organization for the submitted work, no financial relationships with any organizations that might have an interest in the submitted work in the previous 3 years and no other relationships or activities that could appear to have influenced the submitted work.
Hessel, M. H. M. , Cohen, A. F. , and Rissmann, R. (2016) Sofosbuvir and daclatasvir. Br J Clin Pharmacol, 82: 878–879. doi: 10.1111/bcp.13011.
References
- 1. European Medicines Agency . Sovaldi:EPAR‐ Product Information [online]. February 5 2014. Available at http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_‐_Summary_for_the_public/human/002798/WC500160599.pdf (updated July 20 2015, last accessed 4 August 2015).
- 2. European Medicines Agency . Daklinza:EPAR‐ Product Information [online]. September 15 2014. Available at http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_‐_Summary_for_the_public/human/003768/WC500172850.pdf (updated March 31 2016, last accessed 4 May 2016).
- 3. Kohli A, Shaffer A, Sherman A, Kottilil S. Treatment of hepatitis C. A systemic review. JAMA 2014; 312: 631–40. [DOI] [PubMed] [Google Scholar]
- 4. Manns PM, Cornberg M. Sofosbuvir: the final nail in the coffin for hepatitis C? Lancet 2013; 13: 378–9. [DOI] [PubMed] [Google Scholar]
- 5. Lawitz E, Mangia A, Wyles D, Rodriguez‐Torres M, Hassanein T, Gordon SC, et al. Sofosbuvir for previously untreated chronic hepatitis C infection. N Engl J Med 2013; 369: 678–9. [DOI] [PubMed] [Google Scholar]
- 6. Khullar V, Firpi RJ. Hepatitis C cirrhosis: New perspectives for diagnosis and treatment. World J Hepathol 2015; 7: 1843–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Bertino G, Ardiri A, Proiti M, Rigano G, Frazzetto E, Demma S, et al. Chronic hepatitis C: This and the new era of treatment. World J Hepatol 2016; 8: 92–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Nelson DR, Cooper JN, Lalezari JP, Lawitz E, Pockros PJ, Gitlin N, et al. All‐oral 12‐week treatment with daclatasvir plus sofosbuvir in patients with hepatitis C virus genotype 3 infection: ALLY‐3 phase III study. Hepatology 2015; 61: 1127–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Yang SS, Kao JH. Daclatasvir‐containing all‐oral regimens for the treatment of hepatitis C virus infection. Hepatol Int 2016; 10: 258–66. [DOI] [PubMed] [Google Scholar]


