Summary
Increasingly, research is directed at advancing methods to address obesity management in primary care. In this paper we describe the role of interdisciplinary collaboration, or lack thereof, in patient weight management within 12 teams in a large primary care network in Alberta, Canada. Qualitative data for the present analysis were derived from the 5As Team (5AsT) trial, a mixed‐method randomized control trial of a 6‐month participatory, team‐based educational intervention aimed at improving the quality and quantity of obesity management encounters in primary care practice. Participants (n = 29) included in this analysis are healthcare providers supporting chronic disease management in 12 family practice clinics randomized to the intervention arm of the 5AsT trial including mental healthcare workers (n = 7), registered dietitians (n = 7), registered nurses or nurse practitioners (n = 15). Participants were part of a 6‐month intervention consisting of 12 biweekly learning sessions aimed at increasing provider knowledge and confidence in addressing patient weight management. Qualitative methods included interviews, structured field notes and logs. Four common themes of importance in the ability of healthcare providers to address weight with patients within an interdisciplinary care team emerged, (i) Availability; (ii) Referrals; (iii) Role perception and (iv) Messaging. However, we find that what was key to our participants was not that these issues be uniformly agreed upon by all team members, but rather that communication and clinic relationships support their continued negotiation. Our study shows that firm clinic relationships and deliberate communication strategies are the foundation of interdisciplinary care in weight management. Furthermore, there is a clear need for shared messaging concerning obesity and its treatment between members of interdisciplinary teams.
Keywords: Interdisciplinarity, obesity, primary care, weight management
What is already known about this subject
Obesity is a chronic medical condition which is inconsistently addressed in primary care
Interdisciplinary approaches are increasingly suggested in primary care obesity management, though the actual functioning of teams can be challenging
What this study adds
Deliberate clinic communication and solid interdisciplinary relationships support the ongoing negotiation of key challenges that are part of interdisciplinary care: scheduling, messaging, role perception and availability
Failing to account for the role of clinic environment and interdisciplinary relations can undermine the reach and impact of obesity management interventions and Knowledge Translation efforts
Introduction
Increasingly, it is becoming apparent that obesity is a complex chronic illness with numerous underlying comorbidities and risk factors 1 that is best addressed through interdisciplinary care teams 2, 3. It is well‐established that obesity is a pressing public health concern 4, 5 and is not effectively managed in primary care 6. However, interdisciplinary collaboration can be a difficult process 7. For instance, organizational rules and regulations can hamper co‐operation in primary care 8, as can participant commitment 9 or internal communication 10. Saying an illness requires an interdisciplinary healthcare approach does not ensure that cooperation will take place. This was a challenge encountered by healthcare providers within the Implementation and Evaluation of the 5As of Obesity Management in Primary Care 5As Team (5AsT) study 11.
In this paper, we map the role of interdisciplinary collaboration, or lack thereof, in patient weight management in the context of a weight management training intervention with primary care providers. Our objective was to identify contextual factors that could influence the ability of providers to discuss weight with their patients. Data for this analysis are from the 5AsT study; a mixed‐method randomized control trial of a 6‐month participatory, team‐based educational intervention aimed at improving the quality and quantity of obesity management encounters in primary care practice 12. This intervention was co‐created with front‐line practitioners including nurses, nurse practitioners, family physicians, dieticians, mental health workers and tertiary obesity specialists in our community partner primary care network (PCN). This intervention was based upon the 5As of Obesity Management™ (5As) 13. The 5As approach was developed by the Canadian Obesity Network and combines the structure of the Canadian Obesity Clinical Practice Guidelines 14 with the 5As methodological framework (Ask, Assess, Advise, Agree, Assist) 15. This paper describes our finding that high‐functioning interdisciplinary teams are a pre‐condition to being able to improve obesity management in primary care. This will directly influence the structure of future 5AsT programming to improve organization of care for persons with overweight and obesity.
Methods
The 5AsT study is a convergent mixed‐method randomized control trial 11; ethics approval was given by the University of Alberta ethics board (Pro00036740). This trial was registered via Clinical Trials. Gov (NCT01967797).
Details of the design of the 5AsT randomized control trial have been presented in detail elsewhere 11. In brief, 5AsT was an allocation concealed, randomized trial of 24 family, practice‐based chronic disease management teams. The primary quantitative outcome measure was the number of weight management visits conducted by the registered nurses or nurse practitioners on the teams. Providers were blinded as to the study outcome measure; the research team was not involved in data collection of routine encounter data forms, and data analysts were blind to group allocation. The 5AsT evaluation used a convergent mixed‐method design. The quantitative results will be presented elsewhere. The qualitative focus, presented here, was to determine what contextual factors could influence the primary outcome measure. This paper focuses on one of the principle findings: effective interdisciplinary team care is a key factor in obesity management.
Setting and participants
PCNs are partnerships of community family practices throughout Alberta and provide access to interdisciplinary team‐based care. At the time of study design, our partner PCN employed 52 interdisciplinary healthcare providers who are embedded in practice with 178 family doctors serving over 195 000 Albertans. As the family practices are dispersed, their patients range in age, culture, ethnicity and economic background.
Twenty‐four clinic‐based interdisciplinary PCN teams serving 157 470 patients were randomized to the 5AsT intervention or control. To be eligible, clinics had to have joined the PCN by April 2013 and must have a multidisciplinary team including a nurse or nurse practitioner, mental health worker and a dietitian affiliated with the family practice clinic. Participants, consisting of healthcare providers supporting chronic disease management in clinics, randomized to the intervention (n = 29) included: mental healthcare workers (n = 7), registered dietitians (n = 7), registered nurses or nurse practitioners (n = 15). Nurses tended to be assigned a single clinic while dietitians and mental health workers often had two or more clinics. All PCN practitioners participated in occasional meetings and training sessions at the PCN office, however, many participants seldom saw or interacted with PCN colleagues. Participants aged in range from 29 to 68 and all participants except one were female.
5As Team design
The 5AsT study aimed to increase the number and quality of obesity prevention and management encounters in the PCN through changing provider behaviour. The key theoretical underpinnings for the intervention were (i) Complex Innovations Implementation (CII) 16, a framework developed to elucidate factors that may influence interventions and (ii) Theoretical Domains Framework (TDF) 17, which outlines 14 key domains influencing behaviour change. The influence of both the CII and TDF theoretical frameworks on the structure of interviews and field notes is shown in Table 1. Both of these theories supported the need for rich description of the intervention as well as the importance of understanding the context within which it was taking place.
Table 1.
Field note and interview guide as related to theory
| Field note guide | Interview question guide (adjusted following semi structure format) | Theory and/or intent |
|---|---|---|
|
Context: Setting, Intent of Encounter, Climate, Resources General: Thoughts, Flow of Encounter, Communication, Behaviour, Subject Topics. Individual Clinic/practice Organizational (SSPCN/management/) External Environment (community characteristics, level of community involvement, payment models i.e. fee for service, transportation) |
Background: Role in the primary care network length of time at primary care network How many clinics visited What brought you to work in this field? Describe a typical work week (tasks, interactions with staff) What is most challenging? |
Interview: General Context Theoretical Domains Framework 17, 18 Field notes: General context Levels of influence 19: |
|
Implementation Management: primary care network management, communication, rational for decisions. Values Fit: fit between 5As and individual or primary care network values Resources: including time, money or material resources 5As: any mention of the 5As tool kit of the implementation itself Group Performance: what is the effort being put forward? How is everyone working? History: are people talking about previous experiences with other training or implementation? |
Innovation/Management: Thoughts on 5As framework and tool kit? (Useful? Used in past? Appropriate?) What would influence use of 5As? Is there anything you would change in the 5As approach How have you found the sessions so far? Anything you would change in the intervention? How would you describe work climate? Clinics approach to new programs or tools? How is communication in clinic? |
Field notes, interview: Complex Innovations Theory 16
Is there value fit with approach? What is management climate Resource availability Organizations implementation policies and practices Climate |
|
Behaviour Change Knowledge and Skill: showing, learning, or talking about specific knowledge and skill sets. Expression of intentions and goals of providers, follow through Self‐Views: expressions of optimism or pessimism, belief about self‐confidence, competence, and empowerment. How they see their own role. Social Influence: how is the group influencing each other's behaviour, concrete examples of change based on others, or program. |
Beliefs and Attitudes What is your approach when you see patients for weight? Routinely ask patients? (why/why not) Confidence in discussing root causes? Barriers to in‐clinic weight management that you are aware of? Efforts to address barriers? Influence of intervention on practice if at all? |
Field notes, interview: Theoretical Domains Framework Assess knowledge, skill, intentions Beliefs about capabilities Optimism Environment Context and Resources |
The intervention has been described in detail elsewhere 12. In brief, it was co‐created with the PCN and occurred bi‐weekly for 6 months (12 sessions) with an additional kick‐off session, evaluation session at completion and a 6‐month post‐intervention follow‐up to member‐check qualitative results. Participants were asked to identify areas of knowledge need concerning patient weight management and these suggestions were grouped thematically to form 12 session topics (Table 2). Participants met for 2 h where they participated in an interactive presentation with a topic expert on the session, followed by a facilitated learning collaborative session in team‐based groups, and set goals to integrate new knowledge into their practices. Sessions were supported by a clinic champion 16 who acted as a liaison between the PCN and the research team external practice facilitators, supported participants when needed and helped identify any emergent issues. The intervention was designed to encourage sharing of experiences and expertise between practitioners and to provide space for discussing weight‐management‐related challenges and barriers in clinics. Further details on other activities carried out during these sessions are outlined elsewhere 20 and are available in module format on the Canadian Obesity Network 5AsT page. [http://www.obesitynetwork.ca/5As_Team]
Table 2.
5As Team session topics and brief description
| Session | Topics | Brief Description |
|---|---|---|
| 1 | Weight Bias | Recognizing and avoiding bias |
| 2 | Emotional Eating | Types of hunger, responses, tips |
| 3 | Clinical Assessment of Obesity Related Risk | Types of assessment and associated risks |
| 4 | Pregnancy, Post‐partum, Obesity | Assessment, associated risks, communication |
| 5 | Exercise and Weight Management | Impact of exercise, exercise recommendations for various conditions |
| 6 | Culture and the Body, Culture and Food – Perspectives on Obesity | The impact of culture on how food and the body is perceived |
| 7 | 5As of Obesity Management | Review of the 5As and its components |
| 8 | Weight Gain Prevention | The role of prevention, recognizing times of need |
| 9 | How to Sustain the Change | Keeping up motivation, follow up visits, communication |
| 10 | Depression Anxiety and Obesity | Impact of depression and anxiety on obesity |
| 11 | Critical Conversations | When and how to address obesity, communicating with other health professionals |
| 12 | PCN Communication and Process | Primary care network (PCN) internal structure and communication |
Data collection
Qualitative data collection had three goals: to describe the intervention, provide continual intervention monitoring and to identify contextual factors that could influence the primary outcome measure. Convergent mixed methods study design 21 seeks elaboration and enhancement of results, triangulation between data types and works to create a comprehensive account of an issue. Such an approach allowed us not only to measure the impact of the intervention in terms of activity but also provided a better understanding of the challenges and barriers inherent in weight management.
Intervention evaluation relied on structured field notes taken during sessions, semi‐structured interviews (n = 29) and clinic champion log. During interviews, participants were asked to describe their background, daily routine and details regarding their work situation (length of time at the clinic and type of patients seen most often). Questions were asked pertaining to aspects of their work that they found most rewarding or challenging, their experience with and views of the 5As of obesity, communication and interactions with their colleagues, general clinic environment, work support, the nature of weight management visits they conduct and their comfort level with various aspect of weight management (asking, identifying need, referrals, assessing root cause).
Analysis
Thematic analysis was used to determine themes from within the qualitative data 22, 23. Using NVIVO 10 software, transcripts were inductively coded line by line according to broad subject. A code manual was created from the first six interviews, and each code was reviewed for recurrent patterns or subthemes. Patterns were compared between codes to identify themes. Following Sandelowski and Leeman, we defined theme as an integration of the disparate pieces of data that constitute the findings 19; a theme had to be consistently present, link numerous codes and could be latent or manifest. Field notes were likewise coded and reviewed for patterns pertaining to context, flow of sessions and content. All analysis was cross‐checked by research team members and an independent third party. Key findings, including the content of this paper, were shared with participants at 12 months where an opportunity for comment was provided.
Results
In transcripts ‘interactions with other healthcare providers’ were coded in a single category, as were ‘descriptions of provider's work environment’; these two codes, although independent, were strongly related. Within these, four common patterns of importance in the ability of healthcare providers to address weight with patients were (i) Availability; (ii) Referrals; (iii) Role perception and (iv) Messaging. Underlying these concepts is the broader theme of (v) Interdisciplinarity, as expressed through communication and clinic relationships, and (vi) Interdisciplinary confidence.
Availability (i) refers to the ability of two or more people to meet and communicate as needed within a reasonable amount of time. This included the interdisciplinary team members knowing and meeting each other, being able to consistently communicate during the work‐day, or deliberately asynchronously, and having work schedules that allowed collaboration.
Two concerns regarding availability were brought up most often; the first was scheduling that limited face‐to‐face time between providers and subsequently limited the potential for collaboration or discussion. As the excerpt below shows, it was not uncommon for providers to not personally know or even have met other providers within their same clinic. In this primary care network there is a distributed model where dietitians and mental health workers may be shared between several smaller clinics.
‘The dietitian comes once a, no maybe more. She does come. I'm not sure. She comes on Wednesdays so I'm not here Wednesdays. I'm not sure if it's every Wednesday and then we have an RN that's here four days a week and then we have mental health once a week and our team once a month and then we have another NP that's here Wednesdays. I work with our RN all the time so on a daily basis we talk about things going back and forth but the others I don't really see to be honest …’ (Nurse7)
Another issue was lack of in‐clinic time to speak to providers who were physically present but otherwise unavailable. In this primary care setting, physicians are fee for service, while interdisciplinary team members are salaried. There is currently no billing code to support team‐based discussion.
‘I can talk to them about it. It's the time, when to talk to them about it … I'm trying to catch them as they go between, this room to this room to see the next patient so I have about a minute, maybe 90 s to get the question that I had for this patient that I'm seeing right now so to sit down and discuss it, it would be lunch hours. Well that doesn't really happen. We have a drug rep on Tuesday and, and otherwise they're gone, they go out for lunch and nobody is willing to give up their own time … that part is tough. That discussion time is tough’ (Nurse4)
Referrals (ii) points to the need for weight management referrals to take place, for those referrals to be appropriate to provider ability and for the patient to be knowledgeable about, or in agreement with the reason for referral. Many practitioners felt they were not receiving the weight management referrals they could, or that the referrals often left the patient and provider unclear as to where to begin the conversation.
‘… in some clinics the physicians work more collaboratively with the staff in the clinics and so for example at X Clinic, the physician will come down and say oh I've referred Mrs. A to you for weight management, FYI, she's a binge eater. And so we can work collaboratively on that whereas in other clinics … there's just a referral, see Mrs. A … about 50 pound weight loss so then Mrs. A comes in and she says oh I need to lose 50 pounds and I (ask) can you tell me about where that number came from?’ (Dietitian 3)
‘… cause there's four or five doctors working, just the way they approach it sometimes they'll just go and tell the patient they need to lose (weight) and … doesn't tell them anything and just refers to me.’ (Nurse6)
Role perception (iii) concerns the way a provider's role is understood by other interdisciplinary team members. Issues pertaining to role perception were fairly consistent and strongly linked to concerns with referrals. All three professions felt providers within their clinics were sometimes unclear as to their role in weight management, although mental healthcare workers expressed this issue more markedly. Common examples included concern that they were not receiving the type of referrals they could, that other providers did not understand their role in weight management, or that they as providers did not understand the role of others. As seen in the excerpts below, the ability of providers to contribute to patient weight management is not always recognized by their colleagues.
‘It depends on what clinic you go to. Some … see me more as someone to talk about diabetes but not weight management. They wouldn't, you know they would probably tell their patient to go to Weight Watchers before they would refer to me.’ (Nurse 1)
‘Not, most of the part that we get with that is the eating disorder stuff so not normally aside from the dietitian that works here, I always do her Weight Wise mental health screens for her so that would be the only time it would be more of a weight management on the obesity scale. Now we're supposed to see them more but I still don't think the doctors have clued into everything they can refer to us …’ (Mental Health Worker 6)
Messaging (iv) refers to the overall approach to weight management that providers within the same clinic were using, as well as the key information being shared between providers and patients. Inconsistent messaging among providers within clinics, as well as with specialist seen by the patient, was a common concern raised during interviews. In such cases there was feeling that advice was not patient‐centred, that efforts had not been taken to consider patient history and that as a consequence, the patient might suffer a setback, reduced interest, or reduced personal confidence. In these cases the message a patient had received from another provider was counter to the message or approach the interviewee was giving.
‘I've even had patients bring me stories about seeing other providers like for an orthopedic surgeon for like a hip replacement or a knee replacement, saying you need to lose 50 pounds and they've already lost 50 pounds and they come to see me and they're like in tears and so I've seen that from a lot of other providers too.’(Nurse 6)
‘… from mental health perspective or behavioral health, the nursing perspective and the physician's perspective, we all need to be on the same wave length. We all need to be giving them the same message ‘cause if we're not and so the doctor might say one thing, I say one thing and or maybe X and I say one thing and he says another thing, then how does that help because then you've got two messages that you're sending out to that patient.’ (Dietitian 4)
Interdisciplinarity (v): clinic processes and personal differences between providers can often hinder issues needing interdisciplinary support. Looking deeper into our observations, however, we find that what was key to our participants was not that availability, referrals, role perception and messaging be uniformly agreed upon by all clinic staff, but instead that communication and clinic relationships support their continued negotiation. Take for instance the following two extracts:
‘I actually, even when I think it was Dr. Sharma's blog I was on and it had the thing about the knees and the weight, I actually did send it out to one lead doctor here, said ‘interesting blog, I think you should read it about the, the weight loss and knee replacements’ …’ (Nurse 5)
‘So I had a, a 90 year old man, a referral sent to me from the doctor saying extreme weight loss needed. He's 90 and when I called the patient I said you're more than welcome to decline if this isn't what you want and he did … those kinds of referrals and I guess the comfort level … for me to go approach them about that, I'm not there yet with the relationship with that physician … They're not there as often as when I'm there, or the interaction is not there, so just to go and talk to him about it, I'm not comfortable.’ (Dietitian 6)
Strong communication and clinic relationships underlie the ability of interdisciplinary teams to work effectively. Clinics are dynamic settings where schedules change, time tables do not always overlap and new research shifts messaging and treatment consistently. In such settings, divergent perspectives are perhaps unavoidable, however, ongoing negotiation between clinic staff is vital and this cannot happen without feelings of support and openness to communicate. In the first example, the nurse felt comfortable enough to forward information to a provider within her clinic, while in the second the dietitian was not comfortable addressing a referral with the physician. Below is an example of a dietitian working in more than one clinic with divergent experience in terms of approachability.
‘… so out of the two clinics one of them … I think we're freely open to talk and communicate and things like that and I think there's, the doctors are very receptive and, and we're certainly receptive so that's one. The other one is more very old school kind of medical model … I sometimes feel like I'm intruding when I want to try and have a conversation and I'm taking up their time … I might be passing information on but I don't think there's necessarily a conversation.’ (Dietitian 4)
Challenges with comfort were not unique; certain providers felt uncomfortable eating in the shared lunch room or suggesting any kind of change to clinic procedure. Other providers expressed strong communication, feelings of support and subsequently reported more discussions with their interdisciplinary team around problematic elements of weight management. The relationship between these elements is visualized in Fig. 1. The ability for the four central elements to be negotiated facilitates interdisciplinary cooperation that is necessary to address obesity in the most productive way possible.
Figure 1.
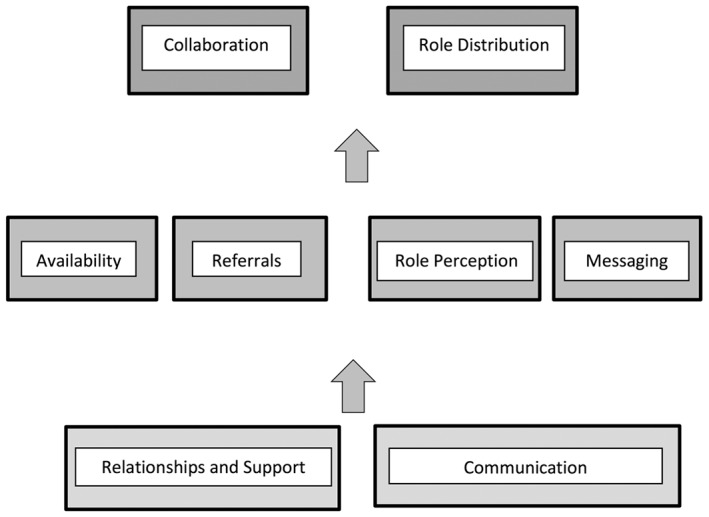
Interaction between key patterns regarding interdisciplinarity in patient weight management.
Interdisciplinary confidence (vi) refers to individual providers feeling comfortable asking about or addressing areas of health outside of their expertise. For example, a nurse assessing for mental health concerns or a dietitian asking about medication adverse‐effects. This area was both a challenge and strength of 5AsT. Initially, providers did not necessarily have the confidence necessary to assess root causes of weight gain outside of their own expertise.
‘… obviously on the food side of things you know if, if it's a lifestyle and they've been eating more processed foods … I'm comfortable with talking about. When it comes to the mental health aspect or they've had depression and they're on medications and they gained weight or the sleep part of it where it's not necessarily something, I can suggest for them to look into the sleep apnea but I don't have necessarily the background or authority I guess to say you need to go for a sleep study.’ (Dietitian 6)
Broad training in the various contributors to obesity enables providers to not only see their own role in treatment, but to better understand the role of others and therefore begin addressing problems in referrals, messaging and role perception. 5AsT supported growth in interdisciplinary confidence although it had not been an explicit goal. For example, an internal tool suggested by and created in part with 5AsT providers was a pamphlet that summarized key messaging important in the 4Ms (Mental, Metabolic, Monetary and Mechanical) 24. This provided a summary of key issues necessary to assess root causes of weight gain and support the referral process. These interdisciplinary aspects of 5AsT, topic choice, diverse providers in training and the space for those providers to discuss weight management was consistently positively reviewed by providers and is a key learning for future 5AsT projects.
‘I think it gives us new ways to look at things and I think we need each other's ideas because lots of times there's just one little thing that somebody else does that you never thought of and if we work in isolation, you know if we never have meetings then we always do the same thing with patients, we don't get any new ideas and I think that's important in learning, you know trying different things.’ (Nurse 5)
‘I actually like the interaction between all team members’ cause I found we all have slightly different perspective right which is super, it's great.’ (Nurse 5)
‘Some things I find are really new. Other things are refreshers but refreshers are always good. Just collaborating at the end, having an open discussion, getting perspectives from different health care professionals is always good too and like even for today, we identified gaps in terms of the classes that we were offering for nutrition so it brought to light … change that can happen so it's good.’ (Dietitian 4)
Discussion and limitations
Our findings show that clinic environments are a key factor in the implementation of interdisciplinary obesity management. Thus, while participants in the 5AsT intervention reported stronger interdisciplinary collaboration during sessions, and provided examples of positive change in terms of weight management visits, clinic environment sometimes limited the ability of providers to transform the information they had learned into practice. These findings are contextual in nature, and the term ‘factor’ as opposed to ‘barrier’ is deliberate. Barriers are too easily thought of as distinct and independent variables, while what we report on here are interrelated and occasionally subtle factors which, while likely found in other settings, need to be understood within their specific contextual surroundings. In terms of our study outcome, this could limit the efficacy of the 5AsT intervention. For instance, if a provider learns that a particular change could help increase patient comfort, the impact of that knowledge is reduced if they feel uncomfortable making the suggestion. Statements like this were not uncommon:
‘I don't feel comfortable yet bringing things up or talking about certain things, like for example when we had the session on weight bias, one of my goals actually was to bring up putting the scale somewhere else and I don't feel comfortable just because things at that clinic are done in a different way.’ (Nurse)
Although interdisciplinary collaboration is suggested as a solution to the complex nature of many chronic illnesses, this is far more difficult to implement than by simply placing diverse providers within the same clinic. If providers are unclear as to the full scope of their roles, are sharing contradictory messaging and are not receiving or sending appropriate referrals, the benefit of team care is lost. There is a paucity of research working with primary care team‐based care on obesity 25 and the potential for team issues to influence knowledge translation is large. Some research exists, specifically related to chronic disease management, within which interdisciplinary teams were a key focus. For example, Chan et al. found that developing communication strategies between physicians and other healthcare providers increased collaborative confidence, trust and teamwork 26. Similarly, Vachon et al., working with a provider‐focused interdisciplinary educational intervention for chronic disease, noted the negative impact that lack of communication and poor understanding of each other's professional roles played in hampering interdisciplinary relationships 27.
Based on the results of the 5AsT study, our ability to fully engage family physicians as part of interdisciplinary training will determine in part the success of future 5AsT programmes. The 5AsT team is currently creating an implementation module to help move the 5AsT programme into other PCNs who have expressed interest. This programme will include lessons learned regarding the importance of interdisciplinarity in weight management and will work towards physician engagement. The broad focus of 5AsT and its inclusion of diverse providers is one way to address this issue. It is a key recommendation of ours in moving forward that such interventions include diverse providers and occur over a sufficient length of time as to support relationship building. Beyond 5AsT, the degree to which interdisciplinary relations can impede knowledge translation or educational efforts in other health domains needs to be further explored. Tension, lack of communication, or misunderstandings between interdisciplinary team members has the potential to derail efforts in any health domain and is not often enough addressed within study methods. Despite the clear and consistent findings with regard to the factors that influence interdisciplinary obesity management, several limitations must be considered. The 5AsT study worked with specific healthcare providers in the limited context of an established PCN in an urban centre. Nevertheless, given the broad nature of these findings, we feel that the underlying issues of interdisciplinarity may likely extend beyond this context.
An important limitation of this study was the exclusion of primary care physicians due to our inability to compensate them for the substantial time that would have been required to participate in the trial. The physicians in this context are paid fee‐for‐service, while the team members in the trial are all salaried. However, physicians were a key part of the research team, were involved in study development and oversight and on occasion were speakers during 5AsT session. Furthermore, a sub‐study was developed to assess physician interest in 5AsT, and (in an unrelated project) to focus more attention on physician obesity education within medical school. Moreover, previous work on physicians using the 5As has shown that brief training programmes aimed at physicians can improve patient–provider interactions and the comprehensiveness of weight management plans 28. A planned direction of future studies is to use a modified short course intervention on the 5As to facilitate more physician involvement.
Conclusion
Our study shows that firm clinic relationships and deliberate communication strategies are the foundation of interdisciplinary care in obesity management. Our findings also confirm that there is a clear need for shared messaging concerning obesity and its treatment between members of interdisciplinary teams. Ongoing negotiation of clinic elements (availability, referrals, role perception, messaging) is key in dynamic systems and often precedes collaborative practice. The complexity of obesity necessitates a broad approach and many existing primary healthcare structures are already in place to help support it. However, actualizing these efforts can be challenging and knowledge translation, behaviour change, education and research efforts need to consider the contextual barriers that may hinder looked for outcomes.
Disclosures
Dr. Sharma is a member of an Advisory Board with a commercial organization (Vivus: Consultancy for anti‐obesity drug; Novo Nordisk: National [Canada] Advisory Board for anti‐diabetes drug; Boeinger‐Ingelheim: National and International Advisory Boards for Anti‐hypertension and anti‐diabetes drug). Dr. Sharma is a member of a Speakers Bureau (Vivus: Payment for development of educational presentations including service on speaker’ bureau). Drs. Campbell‐Scherer, J. Asselin, A.M. Osunlana and A.A. Ogunleye have nothing to disclose.
Authors Contributions
DCS, AS, JA, AAO, AMO are responsible for study design, JA, AAO, AMO and DCS for data collection, JA conducted analysis with review support from DCS, AAO, and AMO. JA and DCS wrote the initial manuscript with input from AS, AAO and AMO.
Acknowledgements
We would like to acknowledge our funders, Alberta Innovates Health Solutions and our community partner, the Edmonton South Side Primary Care Network.
The copyright line for this article was changed on 2 November 2016 after original online publication
References
- 1. Shea J, Diamandis EP, Sharma AM et al The obesity epidemic. Clin Chem 2012; 58: 968–973. [DOI] [PubMed] [Google Scholar]
- 2. Tsai AG, Wadden TA. Treatment of obesity in primary care practice in the United States: a systematic review. J Gen Intern Med 2009; 24: 1073–1079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Carvajal R, Wadden TA, Tsai AG et al Managing obesity in primary care practice: a narrative review. Ann N Y Acad Sci 2013; 1281: 191–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Wass J, Finer N. Action on obesity: comprehensive care for all. Clin Med 2013; 13: 4–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Wadden TA, Volger S, Tsai AG et al Managing obesity in primary care practice: an overview with perspective from the POWER‐UP study. Int J Obes 2013; 37: S3–S11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Manns BJ, Tonelli M, Zhang J et al Enrolment in primary care networks: impact on outcomes and processes of care for patients with diabetes. CMAJ 2012; 184: E144–E152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Xyrichis A, Lowton K. What fosters or prevents interprofessional teamworking in primary and community care? A literature review. Int J Nurs Stud 2008; 45: 140–153. [DOI] [PubMed] [Google Scholar]
- 8. Elissen AMJ, van Raak AJA, Paulus ATG. Can we make sense of multidisciplinary co‐operation in primary care by considering routines and rules? Health Soc Care Community 2011; 19: 33–42. [DOI] [PubMed] [Google Scholar]
- 9. van Raak A, Mur‐Veeman I, Paulus A. Understanding the feasibility of integrated care: a rival viewpoint on the influence of actions and the institutional context. Int J Health Plann Manage 1999; 14: 235–248. [DOI] [PubMed] [Google Scholar]
- 10. Miller JS, Charles‐Jones HD, Barry A et al Multidisciplinary primary care mental health teams: a challenge to communication. Primary Care Mental Health 2005; 3: 171–180. [Google Scholar]
- 11. Campbell‐Scherer DL, Asselin J, Osunlana AM et al Implementation and evaluation of the 5As framework of obesity management in primary care: design of the 5As Team (5AsT) randomized control trial. Implement Sci 2014; 9: 78. 5908‐9–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Ogunleye AA, Osunlana AM, Asselin J et al The 5As Team intervention: bridging the knowledge gap in obesity management among primary care providers. BMC Res Notes 2015; [Accepted 1 Nov 2015.] In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Vallis M, Piccinini‐Vallis H, Sharma AM et al Clinical Review: modified 5 As Minimal intervention for obesity counseling in primary care. Can Fam Physician 2013; 59: 27–31. [PMC free article] [PubMed] [Google Scholar]
- 14. Lau DC, Douketis JD, Morrison KM et al 2006 Canadian clinical practice guidelines on the management and prevention of obesity in adults and children [summary]. CMAJ 2007; 176: S1–S117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Schlair S, Moore S, McMacken M et al How to deliver high‐quality obesity counseling in primary care using the 5As framework. JCOM 2012; 19: 221–229. [Google Scholar]
- 16. Helfrich CD, Weiner BJ, McKinney MM et al Determinants of implementation effectiveness adapting a framework for complex innovations. Med Care Res Rev 2007; 64: 279–303. [DOI] [PubMed] [Google Scholar]
- 17. Cane J, O'Connor D, Michie S. Validation of the theoretical domains framework for use in behaviour change and implementation research. Implement Sci 2012; 7: 37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Tomoaia‐Cotisel A, Scammon DL, Waitzman NJ et al Context matters: the experience of 14 research teams in systematically reporting contextual factors important for practice change. Ann Fam Med 2013; 11(Suppl. 1): S115–S123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Sandelowski M, Leeman J. Writing usable qualitative health research findings. Qual Health Res 2012; 22: 1404–1413. [DOI] [PubMed] [Google Scholar]
- 20. Osunlana AM, Campbell‐Scherer DL, Asselin J et al 5As Team obesity intervention in primary care: development and evaluation of shared decision‐making weight management tools. Clin Obes 2015; in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Creswell JW, Plano Clark VL. Designing and Conducting Mixed Methods Research, 2nd edn SAGE Publications: Los Angeles, 2011. [Google Scholar]
- 22. Morse JM. Qualitative Research Methods for Health Professionals, 2nd edn Sage Publications: Thousand Oaks, 1995. [Google Scholar]
- 23. Morse JM. Mixing qualitative methods. Qual Health Res 2009; 19: 1523–1524. [DOI] [PubMed] [Google Scholar]
- 24. Sharma AM. M, M, M & M: a mnemonic for assessing obesity. Obes Rev 2010; 11: 808–809. [DOI] [PubMed] [Google Scholar]
- 25. Flodgren G, Deane K, Dickinson HO et al Interventions to change the behaviour of health professionals and the organisation of care to promote weight reduction in overweight and obese adults. Cochrane Database Syst Rev 2010; (3): CD000984. doi: 10.1002/14651858.CD000984.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Chan BC, Perkins D, Wan Q et al Finding common ground? Evaluating an intervention to improve teamwork among primary health‐care professionals. Int J Qual Health Care 2010; 22: 519–524. [DOI] [PubMed] [Google Scholar]
- 27. Vachon B, Desorcy B, Camirand M et al Engaging primary care practitioners in quality improvement: making explicit the program theory of an interprofessional education intervention. BMC Health Serv Res 2013; 13: 106. 6963‐13–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Rueda‐Clausen C, Benterud E, Bond T et al Effect of implementing the 5As of Obesity Management framework on provider–patient interactions in primary care. Clin Obes 2014; 4: 39–44. [DOI] [PubMed] [Google Scholar]


