Abstract
Research to eliminate health disparities in the United States is best approached from the perspective of population health. The objectives of this paper are to: a) describe how ongoing research at the eight national Centers for Population Health and Health Disparities (CPHHD) is using a population health perspective and a community-based approach to advance the field of health disparities research; and b) to discuss potential implications of such research for health policies that target some of the determinants of population health.
Keywords: Centers for Population Health and Health Disparities, Health Policy, Population Health, Community-based Participatory Research, Underserved Populations
Introduction
Health disparities represent inequalities in health that are deeply rooted in society and in factors such as race, socioeconomic status, gender, and place. Eliminating disparities in the United States is a major challenge. Because they are observed by comparison of groups, they are best approached from a population health perspective.1,2 Determinants of population health include the social, genetic, and physical environments that may affect health outcomes by directly shaping individual health behaviors as well as by influencing access to living conditions, lifestyles, goods, and services such as health care and social resources.3
Population health strategies require multidisciplinarity and an integration of research from disciplines including biology, genetics, behavioral, social, and health sciences in order to understand disease pathways from the molecular to the societal level.4,5 They also require different, and often more complex, research methods than those used for individual-level research. Potentially, a population health approach may not only improve health outcomes, but also social, economic, and environmental outcomes through changes in health policy.3
In this paper we describe how eight national Centers for Population Health and Health Disparities (CPHHDs) (Table 1) are using a population health perspective and community-based participatory research to advance the field of health disparities research. We also discuss potential implications of such research for health policies that target some of the determinants of population health.
Table 1.
Locations of the Eight Centers for Population Health and Health Disparities
| 1. | University of Illinois at Chicago |
| 2. | The University of Chicago and the University of Ibadan (Nigeria) |
| 3. | Tufts University and Northeastern University, Boston, Mass. |
| 4. | RAND Corporation, Santa Monica, Calif., Pittsburgh, Penn.; Washington, DC |
| 5. | University of Pennsylvania, Philadelphia, Penn. |
| 6. | University of Texas Medical Branch, Galveston, Texas |
| 7. | Ohio State University, Columbus, Ohio and the University of Michigan, Ann Arbor, Mich. |
| 8. | Wayne State University, Detroit, Mich. |
Unraveling the Complexity of Health Disparities
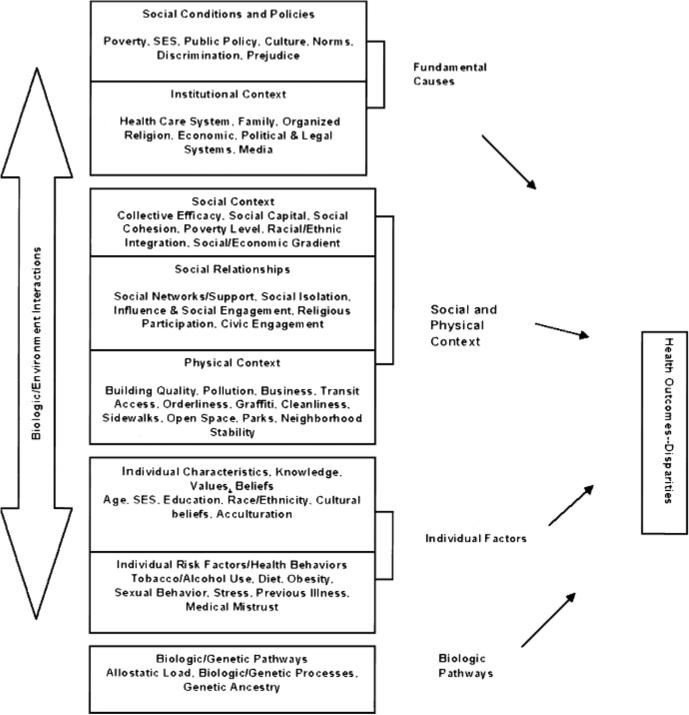
The Centers for Population Health and Health Disparities (CPHHDs) share a common conceptual model shown in Figure 1.6 The model posits that disparities result from interactions (depicted by the double-headed arrow) between and across different levels of factors, which are described by the boxes in the center of the figure. By understanding how health outcomes are linked to more distal causes such as socioeconomic status or racial/ethnic status, we may be able to intervene in the pathways or mechanisms, even if we cannot alter these more distal causes.7
Fig 1.
Conceptual model for CPHHD
Fully understanding the determinants of health not only requires innovative multi-level research, but engagement of community members most affected by patterns of disadvantage.8,9 Thus, a philosophical underpinning for all the CPHHDs is the belief that community-based participatory research (ie, involving community stakeholders in the planning and implementation of research) is essential to advancing the science of health disparities research. Involving community members in research planning and implementation prevents separation of individuals under investigation from their culture and context; ensures activities are undertaken in ways that are culturally appropriate, responsive, and sensitive to community needs; and helps overcome the understandable mistrust for research that exists within many communities.10 Community partners and members have intimate knowledge of: community circumstances; cultural values; and community fears and attitudes that can better inform investigations and keep health care focused on real community needs.8 Community partners also have important contacts and knowledge that can be used in all phases of health disparities research including determination of the problem to be studied, recruitment and retention of research participants, design and or selection of appropriate data collection strategies, interpretation of research findings and, translation of findings for health policy.10
In the following sections we describe ongoing investigations at the eight national CPHHDs. Each center focuses on problems not previously addressed, raises novel research questions, uses innovative population health measures, and examines multilevel determinants of health. The sections are organized according to major themes that define the areas of investigation.
Social Status as Defined by Race and Poverty
Poverty is a social condition that influences access to resources and healthcare services, which influence disparities in health. However, the mediators and moderators of this relationship are not well understood. Researchers at the University of Illinois-Chicago (UIC) CPHHD are attempting to enhance our understanding by disentangling race and poverty and to use the information provided by each concept. At the contextual level, the investigators are examining how community-level estimates of poverty can take advantage of diverse units of analysis such as census tract, to separate the effects of race and poverty. They are also applying the information obtained at the contextual level to individual-level data obtained from cancer patients to determine the extent to which community poverty level affects breast cancer stage at presentation, independent of the individual's socioeconomic status (SES). Thus, they are examining the impact of the neighborhood, its racial and ethnic composition, and the level of poverty on access to healthcare services and behavioral responses to diagnosis.
Additionally, the UIC CPHHD investigators are using qualitative methods to identify individual-level barriers to early detection of breast cancer, including a woman's fears, anxieties and cultural beliefs about breast cancer, life stress, satisfaction with life, trust in the healthcare provider and system, access to health care/health insurance, and family income and employment status. Using an ecological analysis, investigators are examining the interaction of a woman's “embeddedness” in a social network with individual-level factors to influence mammography screening. They are also examining how age and neighborhood context mediate network effects and the relationships between SES, individual beliefs, and race/ethnicity. Findings from these studies will be useful for promoting earlier detection of breast cancer both clinically (focusing on barriers for individual women) and through healthcare policy (focusing on barriers identified in the healthcare system). Preliminary findings have already informed the Illinois Comprehensive Control Plan for the Illinois Department of Public Health, sponsored by the Centers of Disease Control and Prevention.
Environment and Public Policy
The RAND CPHHD takes a different approach to examining causes of health disparities by examining how neighborhood characteristics, especially those modifiable by public policy, affect health. Their projects rely on large national health-related data sets that are geocoded to the level of the census tract. Researchers then merge in characteristics of census tracts, which serve as administrative proxies for neighborhoods. Census tract characteristics span a range of factors from neighborhood SES and levels of racial segregation, to air pollution and street connectivity. The goal is to identify modifiable mechanisms through which neighborhood factors affect health. To accomplish this goal, researchers are using a geographic information system (GIS) to relate information in a spatial context, in addition to multilevel and structural equation modeling techniques.
One RAND project takes advantage of a large natural experiment in which neighborhood groups and the local government have been working together to design and upgrade park facilities in low-income Los Angeles neighborhoods. The project examines whether park renovation affects disparities in park use and the physical activity of neighborhood residents. The project community partners, including the Multicultural Area Health Education Center, representatives of the Department of Recreation and Parks, and trained local health “promotoras,” help to collect data and respond to preliminary results. Another RAND project uses longitudinal data from the Health Care for Communities survey, a national study of mental health in 60 communities across the United States, to explore the environment's effects on mental health. These findings can be used to identify features of the environment that affect mental health, are modifiable by public policy, and therefore represent legitimate targets for policy changes that could lead to healthier neighborhoods.11
Culture and Community
Both the University of Texas Medical Branch (UTMB) and the Tufts University Boston Puerto Rican CPHHDs are looking at how culture is mediated by patterns of social organization, individual behavior, and biologic pathways to produce disparate health outcomes. The UTMB CPHHD investigates the influence of community characteristics on the health of Hispanic populations in the Southwest. The background is the “Hispanic Paradox” of lower mortality for some Hispanics—especially Mexicans Americans—compared to non-Hispanic Whites, despite lower average SES, impaired healthcare access, and the higher prevalence of chronic disease risks.12 The paradox is partly explained by selective immigration of healthier persons from Mexico to the United States. However, migration selectivity does not fully explain mortality patterns because it does not identify the characteristics of migrants and their communities that contribute to better health.
UTMB investigators are examining influences contributing to these outcomes including hypotheses that point to: better nutrition, fewer risk behaviors such as smoking and drug use, stronger social support, and social and cultural buffering of stressors.13,14 The sociocultural characteristics of ethnic communities may also buffer the adverse effects of economic disadvantage.15 One study compares pathways linking community settings, physiologic stress responses, and health outcomes for Hispanics and non-Hispanics in a blue-collar community near a petrochemical complex. This study is methodologically innovative in several ways. First, it investigates custom definitions of neighborhoods based on physical features of the environment and clustering of responses rather than census boundaries. Second, it combines multiple measures of neighborhood environments including perceived neighborhood satisfaction, objective assessments of the built environment, and census-based measures. Third, it incorporates an extensive collection of serum biomarkers of allostasis. A second project examines variation in Hispanic populations in the prevalence of risk biomarkers and mortality in relation to neighborhood sociodemographic characteristics. These findings will illuminate the protective effects of culture and community on health, and can inform policies that support positive sociocultural institutions and practices.
The Boston Puerto Rican CPHHD at Tufts University has developed a cohort of older adults of Puerto Rican origin living in Massachusetts, to determine the effect of particular stressors on biologic response and disease specific outcomes. Researchers hypothesize that within this group, greater levels of stress, associated with poverty, migration, acculturation and perceived discrimination, lead to greater allostatic load, and subsequently to adverse health outcomes, including depression and physical and cognitive impairment. Allostatic load, a measure of lifetime accumulation of physiological stress on the body, has not been widely investigated in minority groups, but may be crucial to understanding disparate outcomes.
Additionally, the Boston Puerto Rican CPHHD at Tufts University is exploring: how limited social support and low vitamin intake accelerate progression from stress to disability; how these associations are modified by genetic variability; how markers of inflammation can contribute to understanding these mechanisms; and how interventions may alleviate this progression. One of the Center's projects, based at Northeastern University, will conduct intensive interviews to better understand the sources of stress, as well as the validity of the questionnaires used to assess it. Another project explores if allostatic load markers and multiple adverse outcomes are partly due to increased frequency of genetic variants that hamper Puerto Ricans’ adaptation to a “Westernized” lifestyle. In sum, the Boston Puerto Rican CPPHD is examining data at multiple levels including the biological/genetic, individual, social relationships and social context, to understand gene-behavior and gene-diet interactions that may be driving health disparities in Puerto Ricans.
Residential Segregation
A project at the University of Pennsylvania CPHHD focuses on the interaction between residence and health care in explaining disparities in prostate cancer, by linking community- and individual-level data. Investigators are assessing the effects of residential segregation on healthcare quality by using a segregation index to compare the spatial distributions of different groups among units in a metropolitan area.16 While segregation has been associated with a number of health outcomes, the project, “Prostate Cancer, Health care and Segregation (PhaSe),” is one of the first to explore how this association may be mediated by healthcare utilization. The investigators hypothesize that Black segregation is associated with household economic deprivation, lack of neighborhood resources, and distrust of White social institutions and that the combination of these factors yield differential access to high quality facilities and providers. They are linking individual-level data about prostate cancer treatment and outcomes from national Medicare files to hospital and provider-level data about case volume and teaching status and to community-level data about residential segregation. This study will increase our understanding of the pathways by which residence might affect prostate cancer outcomes, and as such, holds promise for the development of effective interventions. Although residential segregation in the United States is longstanding and pervasive, where patients seek care and the quality of that care may be more amenable to change.
Race and Society
Researchers at Wayne State University's Center for Urban and African American Health are examining how effects of race are mediated or moderated by social support, neighborhood characteristics, and biological pathways to influence cardiovascular health outcomes in African Americans. In one project, investigators are conducting a randomized clinical trial to determine whether patients and support partners going through cardiac rehabilitation together demonstrate better health behaviors and health outcomes than patients receiving conventional rehabilitation. One widely recognized resource in recovery and management of heart disease is social support,17–19 therefore, meaningfully involving support partners in cardiac rehabilitation programs may amplify the health and survival benefits for African American patients and serve as a catalyst for more long-term heart healthy behaviors. Investigators are using structural equation modeling and multilevel modeling techniques to understand the interaction among low socioeconomic status, self-rated and biological stress levels, social support, and neighborhood characteristics. Community partners at the local cardiac rehabilitation programs have helped develop intervention materials, recruit and retain participants, and will help translate knowledge gathered from biological, individual and neighborhood levels to expand clinical policies and guidelines for cardiac rehabilitation. Findings may suggest the need to expand current individual-focused cardiac rehabilitation policies to policies that incorporate a family system or social network-based perspective.
In another project, Wayne State researchers are examining multiple levels of the CPHHD model to better understand the role of oxidative stress as a major mediator of salt sensitivity among African Americans. Research is underway to determine the main and interactive effects of many environmental stressors (eg, racism, residing in segregated neighborhoods containing concentrated disadvantage and high crime rates), the individual risk of obesity, and the genetic variation of the angiotensin I-converting enzyme (ACE), a key enzyme in the blood pressure regulating renin-angiotensin-aldosterone signaling system that has been linked to salt sensitivity. Uncovering the role of environmental stressors that affect hypertension will help us understand the reasons for elevated rates of hypertension in African Americans, and may suggest effective strategies to reduce the impact of such stressors. Findings may lead investigators and community partners in the City of Detroit Mayor's office to devise ways to build social support networks that can buffer the impact of environmental stressors and improve the coping skills of residents exposed to negative neighborhood conditions.
All projects at Wayne State are examining genetic heterogeneity in ancestral origins with a population of self-identified African Americans. Historically, race has been viewed as primarily reflecting biological homogeneity.31 However, current scientific evidence suggests that our current racial categories are more alike than different in terms of biological characteristics and genetics, with 95% of human genetic variation existing within racial groups not between racial groups.31 To better understand the interactive relationships among race, ancestry and disparate health outcomes, investigators are estimating individual ancestry using information from genetic markers across the genome. These estimates can help us understand ancestral origins of an individual's gene pool or how much of the genetic makeup comes from which ancestral group (ie, European vs African vs Native American). Enhancing our understanding of variation between individuals using genetic ancestry estimates could shed light on differences in responses to treatments or interventions, responses that cannot be understood by looking at racial categories alone.
Racial and ethnic disparities in the incidence and outcomes of prostate cancer remain large and puzzling. The University of Pennsylvania's CPHHD is advancing the knowledge base for addressing prostate cancer disparities by investigating the interaction among factors often studied separately. In the Study of Clinical Outcomes, Risk and Ethnicity (SCORE) investigators are comparing the following three health issues between African American and Caucasian men: a) the relationship of candidate genes with characteristics of prostate tumors at the time of diagnosis (eg, histopathological characteristics, prostate specific antigen [PSA]); b) whether genotypes and other factors predict biochemical relapse-free survival in men who have undergone prostatectomy; and c) whether biological factors interact with behavioral (screening) factors to influence prostate cancer outcomes. Investigators will interview 1000 men who have undergone prostatectomy for the treatment of their cancer to obtain information on demographics and risk factors. They will also obtain a biosample via cheek swab for DNA analysis, and data on tumor pathology, primary mode of diagnosis, PSA, digital rectal exam (DRE) screening results, and treatment from medical records. This longitudinal study will track clinical outcomes of each man for a maximum of five years. Identifying genes and biochemical pathways that influence tumor type and prognosis may lead to breakthroughs in future immunotherapy, early detection, or chemopreventive interventions. In addition, understanding the complex interplay of screening behaviors and genetic variability may lead to more optimal strategies to target prostate cancer screening and prevention to men at the highest risk for poor outcomes.
Researchers at the University of Chicago CPHHD are examining how race may affect disparities through social exclusion and isolation.20 Social exclusion and isolation may be perceived by individuals as loneliness, silence, stigma and fearfulness or anxiety about what others may or may not do because of their race.21 Racial segregation, particularly in racially stigmatized urban neighborhoods with concentrated poverty, low levels of collective efficacy, few opportunities for social participation, and high levels of violence may demand a constant state of vigilance against a threatening environment.22 These factors, combined with chronic and severe socioeconomic stresses, create an additional pathway by which the longstanding social and economic inequities faced by African Americans “get under the skin” and are expressed as health disparities. Researchers are seeking to understand the biological pathways by which the social environment of neighborhoods reach down through households and social networks and affect individuals down to the level of neurons, and even gene-protein interactions.23
Investigators are addressing the interactive and synergistic effects of immunologic processes and mammary tissue metabolism, as well as the direct effects of chronic cognitive stress on neurohormonal regulatory control of gene expression in experimental animal models of tumor development. Fine-grained analyses of linking psychosocial stress responsive biomarkers and disease outcomes in the animal models are then applied to human studies.24 One project is designed to look at social isolation, stress-related hormones, and the molecular characterization of patient samples in the Chicago metropolitan region to see if alterations in both known and novel BRCA tumor suppressor genes contribute to breast cancer in younger Black women. Researchers are examining the contributions of stress dysregulated patterns of glucocorticoids to epigenetic alterations in gene expression,25 along with biomedical factors, family histories and both neighborhood and individual level social determinants of health.11,26 In a related research effort, collaborating researchers from the University of Ibadan will examine if Nigerian women who have moved to urban areas, lack normal social support and are socially isolated are more likely to develop breast cancer.
These findings may help explain breast cancer disparities in African American women, as well as have important implications for breast cancer screening, diagnosis and treatment. At the macro level, the links between neighborhood environment, psychosocial stress and social isolation and biomarkers of glucocorticoid dysregulation reaffirms the necessity of “reconstructing” neighborhoods whose physical and social fabric have been devastated by poverty, crime and discrimination. Academic-community partnerships, such as the Breast Cancer Summit, are taking the first steps in this process by educating community, business and healthcare leaders about breast cancer and will be critical in disseminating these findings at local and regional levels.
Geographic Location
Appalachia is a region associated with the Appalachian Mountains and includes portions of 13 states along the eastern coast of the United States.27 Although economically and culturally diverse, Appalachia is notable for higher unemployment, greater poverty, lower education levels, greater health professional shortages, and disproportionate disease morbidity and mortality, particularly for cervical cancer, as compared to non-Appalachian US.28 The excess mortality rates for cervical cancer in Appalachia are troubling as the disease is both highly preventable and treatable,29 and may be attributed in part to lower cervical screening rates30 and higher smoking rates.31 Unfortunately, few investigators have examined these issues in the Appalachian population.
The Ohio State University CPHHD is examining cultural, behavioral, and psychosocial factors and testing interventions to decrease the excess morbidity and mortality due to cervical cancer in Appalachian Ohio. Specifically, human papillomavirus, smoking, and screening behavior are being explored in terms of their contribution to the development and progression of cervical cancer. In a multiphase project, the first phase is using interviews to examine social, environmental, behavioral, and biological correlates of “risk-appropriate” Pap smear utilization. After a determination of those who are not up-to-date on cervical cancer screening and those who are smokers, the second phase of the project will test the effects of a smoking cessation intervention and/or a lay health advisor program to increase Pap screening utilization. An additional study will examine behavioral risk factors and different strains of the human papillomavirus for their association with cervical abnormalities. These findings have direct implications for cervical cancer screening and treatment. For example, one intervention may be to develop an infrastructure of lay health advisors from the community to help the underserved overcome access barriers to cancer screening and to cease behaviors that are damaging to health such as smoking.
Summary and Conclusions
The eight CPHHDs are developing new information and knowledge about the complex interactions among fundamental causes, patterns within social and physical contexts, individual factors and biologic pathways and their contributions to population health disparities. These efforts hold great promise for the development of policies and interventions that can target key factors to achieve better health outcomes and greater access to quality health care. Other countries such as Australia, United Kingdom and Sweden already concentrate on social, physical and economic environments as potential targets for interventions to eliminate health disparities3; international experiences and data, coupled with research findings from the eight CPHHDs, may guide future policy development in this country.
In addition to the specific policies and programs that might emerge from the results of CPHHD projects, this kind of research can influence how policymakers and the public think about disparities. It can replace a one-dimensional focus on individual behavior, genetics, or a particular social factor (eg, “poverty”) as the cause of disparities, and lead to a greater willingness to adopt interventions that address the multilevel nature of the problem. Eliminating health disparities will require policies that target the intersections among fundamental causes, social and physical contexts, individual factors and metabolic pathways that lead to disparate health outcomes in population groups across the life course.
Potentially, a population health approach may not only improve health outcomes, but also social, economic, and environmental outcomes through changes in health policy.
In addition to the specific policies and programs that might emerge from the results of CPHHD projects, this kind of research can influence how policymakers and the public think about disparities.
Acknowledgments
This work was supported by the Centers for Population Health and Health Disparities and grant numbers 1P59 CA105632, 5P50 ES12383, 5P01 AG023394-3, 1P50 CA 106743-01, 1P50 CA195641, P50 ES012395, 5P50 ES012382, 5P50 CA105631.
Footnotes
Author Contributions
Design concept of study: Artinian, Warnecke, Kelly, Weiner, Flack, Long, Furumoto-Dawson, Hankin, DeGraffinreid
Acquisition of data: Artinian, Weiner, Lurie, Mattei, Furumoto-Dawson, DeGraffinreid
Data analysis and interpretation: Artinian, Warnecke, Lurie, Flack, Mattei, Eschbach, Furumoto-Dawson
Manuscript draft: Artinian, Warnecke, Kelly, Weiner, Lurie, Flack, Mattei, Eschbach, Long, Furumoto-Dawson, Hankin
Statistical expertise: Flack, Furumoto-Dawson
Acquisition of funding: Furumoto-Dawson
Administrative, technical, or material assistance: Kelly, Lurie, Furumoto-Dawson, DeGraffinreid
Supervision: Artinian, Kelly, Furumoto-Dawson, Hankin
References
- 1.Link B, Phelan J. Part II: Promoting population health and reducing disparities. Chapter 5 Fundamental sources of health inequalities. In: Mechanic D, Rogut L, Colby D, Knickman J, editors. Policy Challenges in Modern Health Care. Rutgers University Press; Piscataway, NJ: 2005. pp. 71–84. [Google Scholar]
- 2.Rose G. Sick individuals and sick populations. Int J Epidemiol. 1985;14(1):32–38. doi: 10.1093/ije/14.1.32. [DOI] [PubMed] [Google Scholar]
- 3.Cardarelli KM, de Moor JS, Low MD, Low BJ. Fundamental determinants of population health. In: Aday LA, editor. Reinventing Public Health: Policies and Practices for a Healthy Nation. Jossey-Bass; San Francisco: 2005. pp. 35–64. [Google Scholar]
- 4.Singer B, Ryff C, editors. New Horizons in Health: An Integrative Approach. New Academies Press; Washington, DC: 2001. [PubMed] [Google Scholar]
- 5.Ryff CD, Singer B. Social environments and the genetics of aging: advancing knowledge of protective health mechanisms. J Gerontol B Psychol Sci Soc Sci. 2005;60(Spec No. 1):12–23. doi: 10.1093/geronb/60.special_issue_1.12. [DOI] [PubMed] [Google Scholar]
- 6.Warnecke R, et al. Approaching health disparities from a population perspective. Am J Public Health. doi: 10.2105/AJPH.2006.102525. under review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.House JS, Williams DR. Understanding and reducing socioeconomic and racial/ethnic disparities in health. In: Smedley BD, Syme S, editors. Promoting Health: Intervention Strategies from Social and Behavioral Research. National Academy Press; Washington, DC: 2000. pp. 81–124. [PubMed] [Google Scholar]
- 8.Israel BA, Schulz AJ, Parker EA, Becker AB, Allen AJ, Gizman JR. Critical issues in developing and following community based participatory research principles. In: Minkler M, Wallerstein N, editors. Community-Based Participatory Research for Health. Jossey-Bass; San Francisco: 2003. pp. 53–79. [Google Scholar]
- 9.Minkler M, Wallerstein N. Introduction to community-based participatory research. In: Minkler M, Wallestein N, editors. Community-Based Participatory Research for Health. Jossey-Bass; San Francisco: 2003. pp. 3–26. [Google Scholar]
- 10.Israel B, Parker E, Rowe Z, et al. Community-based participatory research: lessons learned from the Centers for Children's Environmental Health and Disease Prevention Research. Environ Health Perspect. 2005;113(10):1463–1471. doi: 10.1289/ehp.7675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Northridge M, Stover G, Rosenthal J, Sherard D. Environmental equity and health: understanding complexity and moving forward. Am J Public Health. 2003;93(2):209–214. doi: 10.2105/ajph.93.2.209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Markides K, Coreil J. The health of Hispanics in the southwestern United States: an epidemiologic paradox. Public Health Rep. 1986;101(3):253–265. [PMC free article] [PubMed] [Google Scholar]
- 13.Franzini L, Ribble J, Keddie A. Understanding the Hispanic paradox. Ethn Dis. 2001;11(3):496–518. [PubMed] [Google Scholar]
- 14.Markides K, Eschbach K. Aging, migration, and mortality: current status of research on the Hispanic paradox. J Gerontol B Psychol Sci Soc Sci. 2005;60B(Spec No 2):68–75. doi: 10.1093/geronb/60.special_issue_2.s68. [DOI] [PubMed] [Google Scholar]
- 15.Eschbach K, Ostir G, Patel K, Markides K, Goodwin J. Neighborhood context and mortality among older Mexican Americans: is there a barrio advantage? Am J Public Health. 2004;94(10):1807–1812. doi: 10.2105/ajph.94.10.1807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Massey DS, Denton NA. The dimensions of racial segregation. Social Forces. 1988;67:281–315. [Google Scholar]
- 17.Salminen M, Isoaho R, Vahlberg T, Ojanlatva A, Kivela S. Effects of a health advocacy, counselling, and activation programme on depressive symptoms in older coronary heart disease patients. Int J Geriatr Psychiatry. 2005;20(6):552–558. doi: 10.1002/gps.1323. [DOI] [PubMed] [Google Scholar]
- 18.Toobert D, Strycker L, Glasgow R, Barrera JM, Angell K. Effects of the Mediterranean lifestyle program on multiple risk behaviors and psychosocial outcomes among women at risk for heart disease. Ann Behav Med. 2005;29(2):128–137. doi: 10.1207/s15324796abm2902_7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Seeman T, Chen X. Risk and protective factors for physical functioning in older adults with and without chronic conditions: MacArthur Studies of Successful Aging. J Gerontol B Psychol Sci Soc Sci. 2002;57(3):S135–144. doi: 10.1093/geronb/57.3.s135. [DOI] [PubMed] [Google Scholar]
- 20.Cacioppo J, Hawkley L. Social isolation and health, with an emphasis on underlying mechanisms. Perspect Biol Med. 2003;46(3 Suppl):S39–S52. [PubMed] [Google Scholar]
- 21.Geronimus A, Hicken M, Keene D, Bound J. “Weathering” and age patterns of allostatic load scores among blacks and whites in the United States. Am J Public Health. 2006;96(5):826–833. doi: 10.2105/AJPH.2004.060749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sampson R, Raudenbush S, Earls F. Neighborhoods and violent crime: a multilevel study of collective efficacy. Science. 1997;277(5328):918–924. doi: 10.1126/science.277.5328.918. [DOI] [PubMed] [Google Scholar]
- 23.McClintock M, Conzen S, Gehlert S, Masi C, Olopade F. Mammary cancer and social interactions: identifying multiple environments that regulate gene expression throughout the life span. J Gerontol B Psychol Sci Soc Sci. 2005;60(Spec No 1):32–41. doi: 10.1093/geronb/60.special_issue_1.32. [DOI] [PubMed] [Google Scholar]
- 24.Hermes G, Rosenthal L, Montag A, Mc-Clintock M. Social isolation and the inflammatory response: sex differences in the enduring effects of a prior stressor. Am J Physiol Regul Integr Comp Physiol. 2006;290(2):R273–282. doi: 10.1152/ajpregu.00368.2005. [DOI] [PubMed] [Google Scholar]
- 25.Wei M, Grushko T, Dignam J, et al. BRCA1 promoter methylation in sporadic breast cancer is associated with reduced BRCA1 copy number and chromosome 17 aneusomy. Cancer Res. 2005;65(23):10692–10699. doi: 10.1158/0008-5472.CAN-05-1277. [DOI] [PubMed] [Google Scholar]
- 26.Acevedo-Garcia D, Lochner K, Osypuk T, Subramanian S. Future directions in residential segregation and health research: a multilevel approach. Am J Public Health. 2003;93(2):215–221. doi: 10.2105/ajph.93.2.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Appalachian Regional Commission [1/3/2005];Appalachian Regional Commission home page. Available at http://www.arc.gov/index.do?nodeID+27.
- 28.Hopenhayn C, Bush H, Christian A, Shelton B. Comparative analysis of invasive cervical cancer incidence rates in three Appalachian states. J. Preventive Medicine. 2005;41(5–6):859–864. doi: 10.1016/j.ypmed.2005.08.006. [DOI] [PubMed] [Google Scholar]
- 29.Schiffman MHB, Devesa SS, Fraumeni J, Joseph F. Cervical cancer. In: Schottenfeld DF, Joseph F, editors. Cancer Epidemiology and Prevention. Oxford University Press; New York City: 1996. [Google Scholar]
- 30.Hall H, Uhler R, Coughlin S, Miller D. Breast and cervical cancer screening among Appalachian women. Cancer Epidemiol Biomarkers Prev. 2002;11(1):137–142. [PubMed] [Google Scholar]
- 31.Hopenhayn C, Jenkins T, Petrik J. The burden of lung cancer in Kentucky. J Kentucky Med Assoc. 2003;101(1):15–20. [PubMed] [Google Scholar]