Abstract
Since the 1999 Institute of Medicine (IOM) report To Err is Human, progress has been made in patient safety, but few efforts have focused on safety in patients with limited English proficiency (LEP). This article describes the development, content, and testing of two new evidence-based Agency for Healthcare Research and Quality (AHRQ) tools for LEP patient safety. In the content development phase, a comprehensive mixed-methods approach was used to identify common causes of errors for LEP patients, high-risk scenarios, and evidence-based strategies to address them. Based on our findings, Improving Patient Safety Systems for Limited English Proficient Patients: A Guide for Hospitals contains recommendations to improve detection and prevention of medical errors across diverse populations, and TeamSTEPPS Enhancing Safety for Patients with Limited English Proficiency Module trains staff to improve safety through team communication and incorporating interpreters in the care process. The Hospital Guide was validated with leaders in quality and safety at diverse hospitals, and the TeamSTEPPS LEP module was field-tested in varied settings within three hospitals. Both tools were found to be implementable, acceptable to their audiences, and conducive to learning. Further research on the impact of the combined use of the guide and module would shed light on their value as a multifaceted intervention.
Keywords: patient safety, performance improvement, quality improvement, research–qualitative
The Institute of Medicine (IOM) report To Err is Human: Building a Safer Health System (IOM, 1999) shocked the country by estimating that at least 44,000 and as many as 98,000 people die per year from medical errors that occur in hospitals. Although the principles of patient safety and the science of preventing medical errors have evolved, we may be falling well short of our goals for the nearly 25 million people in the United States (8.6%) with limited English proficiency (LEP; U.S. Census Bureau, 2009).
Communication problems are among the root causes of 59% of serious adverse events reported to the Joint Commission’s Sentinel Event Database (The Joint Commission, 2012), and research suggests that LEP patients are more likely than English-speaking (ES) patients to experience safety events caused by communication errors. LEP patients who experienced an adverse event were more likely to be harmed, the adverse event was more frequently caused by a communication error, and the harm was more likely to be serious, compared to ES patients (Divi, Koss, Schmaltz, & Loeb, 2007).
To address this problem, the Agency for Healthcare Research and Quality (AHRQ) commissioned a new guide for hospitals and training program to improve safety for LEP patients. This article describes the development, content, and testing of these new tools, titled Improving Patient Safety Systems for Limited English Proficient Patients: A Guide for Hospitals (hereinafter referred to as the Guide for Hospitals or the Guide), and TeamSTEPPS Enhancing Safety for Patients with Limited English Proficiency Module (hereinafter referred to as TeamSTEPPS LEP module or the Module; AHRQ, 2012a, 2012b). The Module is part of the TeamSTEPPS system, and can also be used as a stand-alone training program. TeamSTEPPS is a patient safety system developed by AHRQ and the Department of Defense, based on more than 20 years of research showing that communication failures account for the overwhelming majority of adverse events, that effective teamwork can prevent mistakes, and that training can enhance teamwork and safety (Clancy & Tornberg, 2007).
The new tools meet an important need for patients and hospitals. LEP patients have been harmed by poor comprehension of their medicalcondition, treatment plan, discharge instructions, complications, and followup; inaccurate and incomplete medical history; ineffective or improper use of medications or serious medication errors; improper preparation for tests and procedures; and poor or inadequate informed consent. In addition, hospitals have been held liable for the harms endured by LEP patients as a result of communication problems (Carbone, Gorrie, & Oliver, 2003; Price-Wise, 2008; Quan, 2010).
Although many hospitals identify a direct relationship between patient safety issues and patients’ linguistic needs, few monitor their patient safety data by language, and very limited data are available on how healthcare organizations nationwide address issues of LEP patient safety (Wilson-Stronks & Galvez, 2009). New standards have been recently developed to promote effective, culturally and linguistically appropriate hospital communication with patients (Office of Minority Health, 2013; The Joint Commission, 2010). AHRQ’s new Guide for Hospitals and TeamSTEPPS LEP module can help hospitals meet those standards for LEP patients within a patient safety framework.
Study Design and Methods
We used a comprehensive mixed-methods research approach to develop content and test the new tools. An executive advisory board of four hospital patient safety and quality leaders gave input to the study design and execution. Methods are summarized below.1
Content Development
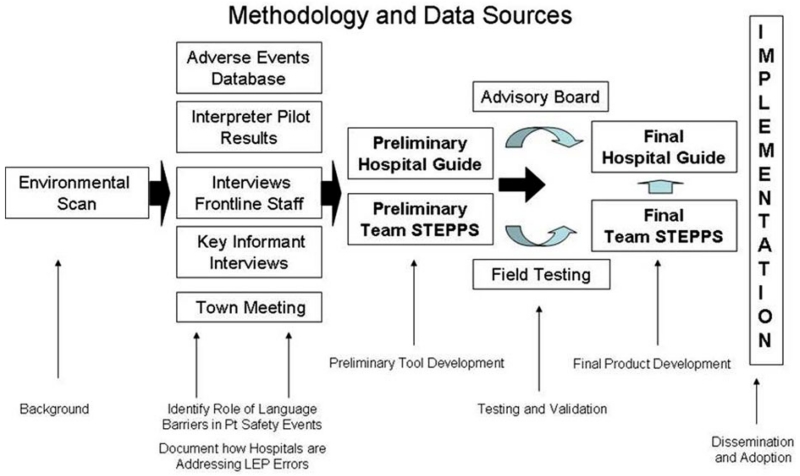
As shown in Figure 1, data to develop content for the new tools were drawn from the following five sources.
Figure 1. Methodology and Data Sources.
Environmental scan. We performed a systematic review of the peer-reviewed and gray literature on LEP (including sign language) and patient safety. PubMed searches were conducted for English-language articles published between 1966 and 2009, using the search terms detailed in Table 1. Google Scholar searches were conducted to complement the PubMed search. Articles were excluded if they (1) did not directly address patient safety or medical errors, and (2) did not directly address language or cultural barriers and patient safety. The gray literature search focused on the websites of foundations, Federal agencies, and other organizations actively engaged in quality and safety for culturally diverse populations. We extracted potential content from each data source by identifying recommended evidence-based trainable team behaviors and hospital system changes for LEP patient safety.
Adverse events analysis. We used early results from a quantitative study on LEP and patient safety that was in progress at two large academic hospitals at the time our project began. The hospitals were selected for the study because both collected electronic data on patient language and interpreter use, and both used the same high-quality adverse event reporting system and patient registration system, allowing data aggregation across facilities. The combined secondary adverse events reporting database included 39,133 patient safety events over a 2-year period (2006–2008). Frequencies of event types were compared for ES versus LEP patients, and chi-square tests were used to test the statistical significance of differences between the two groups. Sample incident reports involving LEP patients were also identified from this database for illustrative purposes.
Interpreter pilot. To gain an understanding of interpreter perspectives on patient safety, we also used results from a quality-improvement study in progress at the time our project began. The study took place at one of the hospitals that was part of the quantitative study described above. This hospital also participated in key informant interviews described below. For the interpreter pilot study, interpreters at one hospital were asked to document situations they thought negatively affected the safety of LEP patients. To the best of our knowledge, no prior study had asked interpreters about their perspectives on patient safety. Interpreters were asked to anonymously report any situations that they, in their role as interpreters, thought negatively affected the health, health care, safety, and wellbeing of a limited English-proficient patient. Specifically, interpreters were asked to document situations in which a patient’s safety was at risk or the patient suffered unnecessary trouble due to an issue surrounding language, literacy, or their cultural perspective. Using the AHRQ patient safety classification Common Formats, Beta version 0.1, August 2008, we identified which patient safety events were (1) incidents–patient safety events that reached the patient, whether or not there was harm, (2) near misses (or close calls)–patient safety events that did not reach the patient, or (3) unsafe conditions–any circumstance that increases the probability of a patient safety event. All incident reports involving harm or potential harm were reported immediately to hospital Quality and Safety leadership. We also identified key themes and applied additional classifications based on those themes.
Key informant interviews. To generate rich content and examples for the new tools, we conducted in-depth semistructured interviews with frontline staff and clinical, interpreter services, and quality and safety leaders, both in person and by phone, at three hospitals in the Boston area. Our goal in selecting hospitals for this research phase was to represent a variety of different perspectives while working within the constraints of limited resources. We drew on professional connections in our geographic area to identify and enroll a teaching hospital that had adopted TeamSTEPPS, a teaching hospital that had not adopted TeamSTEPPS, and an urban safety net hospital with a large LEP population (also a non-TeamSTEPPS site). Standard interview guides were used for key informant interviews (one for frontline staff, one for leaders). Frontline staff were asked about their knowledge of patient safety and medical error terminology, the role of language and cultural factors in patient safety events, their experience and perspectives on patient safety event reporting, and their perspectives on LEP patient safety. Leaders were asked to describe their perspectives on LEP patient safety, to comment on findings from frontline staff interviews, and to respond to a case example from the interpreter pilot.
Town Hall meeting. Further content ideas were generated through an interactive phone discussion (Town Hall meeting) that took place as part of the ongoing activities of the Disparities Leadership Program (DLP), an year-long executive leadership program designed for leaders from hospitals, health plans, and other healthcare organizations who want to (1) develop a strategic plan or (2) advance a project to eliminate racial and ethnic disparities in healthcare, particularly through quality improvement. All past and present DLP participants were invited to participate (a total of 118 persons at the time, representing 58 organizations including 26 hospitals). The final participant list included 19 leaders in quality and safety who were active members in the DLP. Participants represented six hospitals, one health plan, and three hospital associations, and were based in Minnesota, Delaware, California, North Carolina, and New Mexico. A discussion guide was used to touch upon three themes: methods for collecting and reporting medical errors for LEP and culturally diverse patients, mechanisms for monitoring medical errors for LEP and culturally diverse patients, and strategies for preventing and addressing medical errors for LEP and culturally diverse patients. The discussion lasted 1 hr 15 min.
Table 1. PubMed Search Terms, September 14,2009.
| Search No. | Search Terms | Number of Citations Obtainet |
|---|---|---|
| 1 | Interpreter | 797 |
| 2 | “Translation” [all fields] and services [all fields] | 800 |
| 3 | Cultural competence | 3,282 |
| 4 | Cultural competency | 1,226 |
| 5 | Limited English proficiency | 406 |
| 6 | Cultural competen* | 1,609 |
| 7 | Limited English proficien* | 193 |
| 8 | Sign language | 1,938 |
| 9 | Title VI [all fields] | 49 |
| 10 | English as a second language [all fields] | 157 |
| 11 | Linguistically competen* | 83 |
| 12 | Linguistic competency* | 117 |
| 13 | “Speak English” | 261 |
| 14 | “Primary language” | 294 |
| 15 | #1 or #2 or #3 or #4 or #5 or #6 or #7 or #8 or #9 or #10 or #11 or #12 or #13 or #14 |
7,821 |
| 16 | Adverse event [all fields] or adverse events [all fields] | 42,941 |
| 17 | “Medical errors” [MeSH terms] or medical error [all fields] or medical errors [all fields] |
82,548 |
| 18 | Patient safety | 103,778 |
| 19 | Team training [all fields] | 273 |
| 20 | Teamwork [all fields] or teamwork [all fields] | 4,191 |
| 21 | #16 or #17 or #18 or #19 or #20 | 214,477 |
| 22 | #15 and #21 | 217 |
We used data gathered from these sources to develop the Guide and Module.
Field Test
Both tools were validated through a field testing process.
Guide for hospitals field test
We asked nine quality and safety leaders from nine hospitals to (1) participate in an in-depth 30-min telephone interview about the Guide, and (2) share the Guide with members of their implementation teams. Participating hospitals were selected to represent a range of public, private, academic, nonacademic, TeamSTEPPS, non-TeamSTEPPS, and rural and urban perspectives. Eight hospitals were recruited from the DLP; an additional participant was recruited through professional connections to represent a rural hospital perspective. Eight interviewees were executives and key leaders in their hospitals’ patient safety and quality programs. For the rural hospital, the interviewee was a manager of interpreter services and customer relations.
All interviews were audio-recorded, transcribed, and coded for key themes using standard qualitative quality assurance measures. Key themes (structure, design, effectiveness) were predetermined by the interview guide, and subthemes included positive feedback, negative feedback, and specific suggested edits. General feedback was synthesized for each Hospital Guide chapter and illustrated with quotes, and a disposition table was created to process specific suggested edits for each chapter. The research team and AHRQ project officer reviewed each suggested edit and finalized the disposition of each one by consensus.
TeamSTEPPS LEP module field test
The Module was tested in three hospitals that varied in size, geographic location, mission, and level of experience with TeamSTEPPS. Hospitals implemented the Module in inpatient or primary care settings. To replicate real-world conditions, no financial incentive was provided to test sites, and each site was asked to conduct process and outcome evaluations using an evaluation guide provided as part of the TeamSTEPPS module. The evaluation guide provided instructions on evaluating trainee satisfaction, knowledge, staff behaviors, and patient outcomes.
The research team provided technical assistance on module implementation and evaluation, conducted key informant interviews and site visits, reviewed local evaluation results, wrote case study reports for each site, and completed a cross-case report to distill lessons learned across all three sites.
The research team then edited the Module in response to lessons learned from the field test.
Content Development Findings
Environmental scan
Key findings from the literature were that LEP patients are safer with a professional medical interpreter (Carbone, Gorrie, & Oliver, 2003; Flores et al., 2003; Flores 2005; Price-Wise, 2008; Quan, 2010); yet despite the evidence, healthcare professionals often try to “get by” without an interpreter (Diamond, Schenker, Curry, Bradley, & Fernandez, 2009). The literature further showed that integrating interpreters into the care team is a complex endeavor requiring both staff training (to identify and respond to language needs) and organizational change (policies to meet language needs, reorganization of language assistance, and integration of language services into hospital patient safety infrastructure).
Adverse events analysis
Linking adverse event reporting databases to the hospitals’ data on patients’ language and use of interpreter services proved difficult. Although intake records included a language field, we learned that the data in this field were correct only approximately 30% of the time, due to data entry errors and misclassification. We therefore were unable to identify the universe of patients not proficient in English.
Data on interpreter services, however, were reliable. We therefore compared adverse events of patients who had a hospital-provided interpreter at least once during their hospital stay (a proxy for LEP patients) with adverse events of other patients, who primarily were ES, but may have included LEP patients who did not receive a hospital-provided interpreter. Using this nomenclature, 37,415 incidents (95.6%) were reported among ES patients and 1,718 (4.4%) were reported among LEP patients.
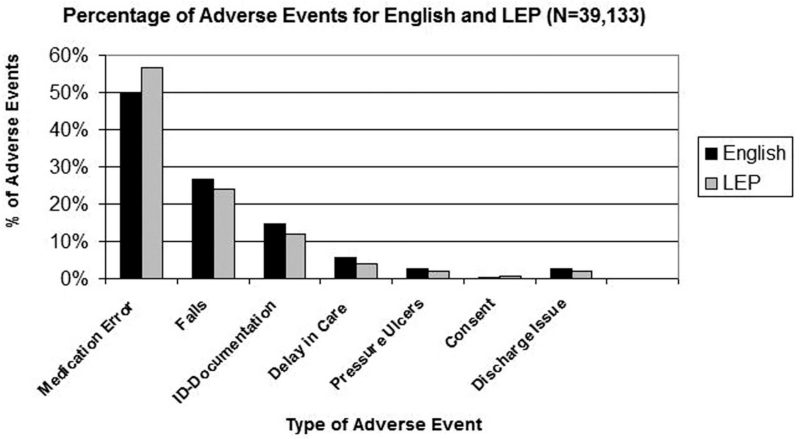
LEP patients who had been provided an interpreter at least once during their hospital stay were more likely to experience an adverse event that was not due to systems procedural and technical issues (49%) than ES patients (42%, p = .003). Medication errors represented a larger share of adverse events for LEP patients than ES patients (57% and 50% respectively, p = .0028) and were the major cause of adverse events for both groups (see Figure 2). LEP patients had a slightly lower rate of adverse events that were classified as near misses with potential harm or temporary/minor harm (34%) compared to ES patients who had a slightly increased rate of events with permanent harm/damage or death (49.5%; overall, p < .001). Unfortunately, the databases we used did not consistently include root-cause analyses for every adverse event, therefore we cannot determine what proportion of adverse events affecting LEP and non-LEP patients were due to communication problems. However, since LEP patients were identified because of their use of an interpreter during their hospitalization, we know that communication barriers existed at baseline for these patients, and may have contributed to reported adverse events. Illustrative examples of incidents affecting LEP patients are shown in Table 2.
Figure 2. Percentage of Adverse Events for English and Limited English Proficiency (N = 39,133).
Table 2. Real-Life Case Examples of Patient Safety Reports.
| The following are real patient safety reports from one hospital in our study that illustrate key issues related to language assistance. | ||
|---|---|---|
| Delays | 1 | Patient arrived in hemodialysis unit to do stat chest X-ray; patient had no identification wristband and could not verify because he did not speak English. |
| 2 | Patient did not have a stress test because a Spanish interpreter was not available. This delayed discharge for at least 24 hours. |
|
| 3 | New patient arrived in infusion unit for first IP taxol appointment without orders, consent, or a recent physician’s note. Patient did not speak English. Interpreter and MD called. Delay in treatment resulted. |
|
| Medical Errors | 4 | Patient is Ethiopian speaking. On multiple occasions, there had been a failure to provide an interpreter. She has been using family members to translate, and they are not always available. This is unacceptable, as we have had issues with medications (i.e., which to take, when) and I believe her worsening diabetes is a direct result of my inability to have effective clinical meetings with her. |
| 5 | Patient came down with his mother for a KUB film. Most exams that are automatically scheduled are chest exams and so I performed one in error. Usually I verify the exam with the patient but he was 11 years old and his mother could not speak English. Immediately after I realized I had done the wrong exam, I called the doctor and had him reorder the exam and I performed the correct one. |
|
| 6 | Informed consent obtained with no Spanish interpreter in emergency room; patient did not understand the procedure when asked by interpreter. |
|
| 7 | Patient was just admitted to the step-down unit from the Medical Intensive Care Unit and was reported to be AOx3 (awake and alert) but Greek speaking primarily. Patient was found on the floor, cardiac monitor attached, and foley still attached to bed. Patient gestured she was going to the bathroom unassisted. |
|
| 8 | LEP patient arrived in the step-down unit s/p thoracic surgery. Hypertension in OR and upon arrival to recovery room, 205/97. Patient with history of CVA in past month, no past medical history or medication list available. Anesthesia unable to give proper report or orders for hypertension management due to lack of information. |
|
Interpreter pilot
Of the 28 eligible incidents identified by interpreters as part of the interpreter pilot, the majority (60%) were related to the theme of misuse of interpreter services, including situations with no interpreter present, use of family members as interpreters, and providers who used their own limited non-English-language skills. Other themes included miscommunication between patients and providers, cultural issues, and one incident respectively of unprofessional behavior by a physician and informed consent completed without an interpreter present.
Key informant interviews
Interviews with frontline staff and quality and safety leaders revealed several common causes andhigh-risk scenarios that significantly affect the care of LEP and culturally diverse patients. We identified the following three common causes of errors (or potential errors) for LEP patients based on the data collected.
Use of family members, friends, or non-qualified staff as interpreters. As reported in the literature, the most commonly reported cause of errors for LEP patients in our in-depth interviews was not using a qualified interpreter, which led to miscommunication between patients and care team members. Qualified interpreters are those who receive training on medical interpretation and meet the professional standards of practice.
Provider use of basic language skills to “get by,” also as reported in the literature. In our in-depth interviews, the second most commonly reported behavior that increased the risk of errors for LEP patients was when staff, particularly clinicians, with basic or intermediate foreign-language skills attempted to “make do” or “get by” without the use of a qualified interpreter. Interpreters reported that even when they were present, some providers declined their services and insisted on using their own limited language skills, and interpreters and nurses did not feel empowered to call a “time out” to address the situation. In some cases, providers mistakenly used seemingly similar languages, such as Spanish for Portuguese or French for Haitian Creole. Staff who were not proficient in the patient’s language also relied on patients’ limited grasp of English. Staff assumed that patients understood based on nonverbal cues, such as nodding or smiling, when often patients were missing vital information.
Cultural beliefs and traditions that affect care delivery. The majority of informants referenced the role of culture, and the importance of cultural competence training, as it pertains to care for LEP and culturally diverse patients. Several interviewees, both frontline and leaders, described specifically how cultural beliefs and traditions (e.g., expression of pain, respecting authority, gender roles, class biases) influence the medical encounter and subsequent health outcomes in subtle and often invisible ways. Informants felt that providing cultural competence training for staff to learn about common cultural beliefs and traditions of populations most commonly served would be helpful.
Informants also identified several high-risk clinical situations where adverse events and medical errors are most likely to occur among LEP patients or where the consequences are likely to be severe. These include medication reconciliation, patient discharge, the informed consent process, emergency department visits, and surgical care.
Town Hall Meeting. Town Hall meeting participants noted that the inconsistent collection of patient data on race, ethnicity, and language greatly affects their ability to understand the role of language and culture in patient safety events. Many of the safety reporting systems used by the hospitals that participated in the Town Hall did not include fields for preferred language, English proficiency, or the need or use of an interpreter. The lack of this information precludes stratification of errors and impedes any root-cause analysis of a medical error or adverse event that might be related to LEP factors. If anything, errors related to LEP are bundled as being caused by “communication errors,” which does not allow for analysis based on LEP status.
Content of the New Tools
Based on the research findings, we developed a first draft of the new tools. A brief summary of tool content is provided below. Full content of the tools is available for free online (AHRQ, 2012a, 2012b).
The Guide for Hospitals presents evidence on the issue of patient safety for LEP patients, including common causes and high-risk scenarios. It also presents key reasons for addressing this issue, including the impact of an increasingly diverse nation on healthcare delivery, quality and cost drivers, and role of risk management and accreditation standards in patient safety efforts. It is intended for hospital leaders and executives in quality and safety, as well as other hospital leaders who work in related fields, such as directors of patient registration, nursing, and interpreter services. It can also be used by individuals within hospitals who are in a position to advise their leadership to take action on patient safety for LEP and culturally diverse patients or who are responsible for encouraging hospital leaders to address this issue.
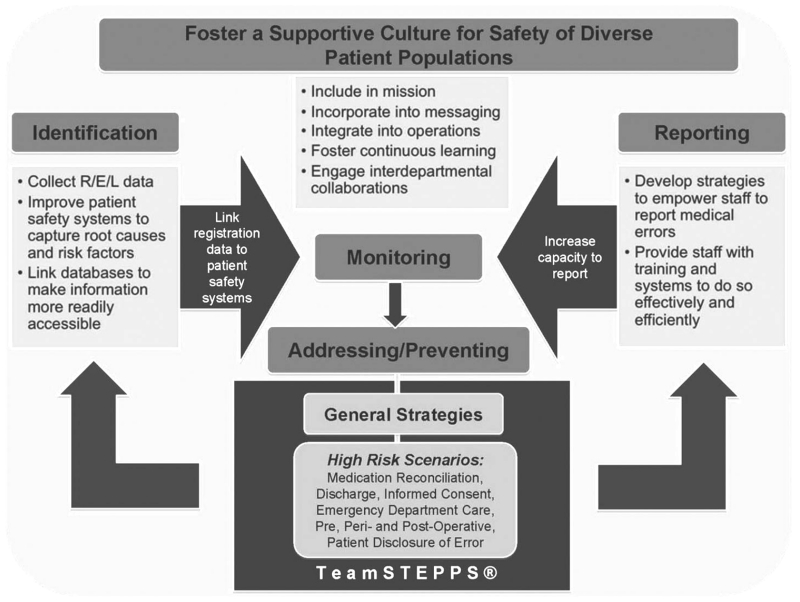
The Guide for Hospitals outlines five key recommendations that aim both to improve detection of medical errors across diverse populations and prevent high-risk scenarios from becoming safety events (Figure 3). These recommendations are as follows:
Foster a supportive culture for safety of diverse patient populations.
Adapt current systems to better identify medical errors in LEP patients.
Develop institutional strategies to empower frontline staff and interpreters to report medical errors.
Develop systems to monitor patient safety among LEP patients routinely, as well as processes to analyze medical errors and near misses that occur among these populations.
Develop strategies and systems to prevent medical errors among LEP patients. These include strengthening interpreter services, improving coordination of clinical services, providing translated materials, and developing training for healthcare providers and staff on team communication, interpreter use, cultural competency, and advocacy.
Figure 3. Key Recommendations to Improve Patient Safety for Limited English Proficiency Patients.
The TeamSTEPPS LEP module
The module trains interprofessional care teams working together in hospital units on the knowledge, attitudes, and team behaviors needed to reduce the number and severity of patient safety events affecting LEP patients.
The TeamSTEPPS LEP module focuses on the following:
the heightened safety risks for LEP patients,
the benefits of including a qualified interpreter on the care team,
structured communication tools to help interpreters and other team members identify and raise communication and safety issues.
The TeamSTEPPS LEP module includes all the materials a trainer needs to implement the module. Train-the-trainer materials and an evaluation guide are also provided.
Field Test Findings
Overall, reviewers found the Guide for Hospitals to be applicable to a variety of hospitals (e.g., rural, urban, public, private, veterans affairs) and reported that the Guide was clear, concise, practical, easy to read, and appropriate for a variety of audiences. Many reviewers particularly appreciated the executive summary, frequently asked questions, case study, and appendices, as key features of the Guide that were effective and useful. Reviewers felt they could use the Guide incrementally, identifying various sections as possible starting points. Reviewers also had many specific suggestions for the Guide content, structure, and format. For example, reviewers asked for more case examples early in the guide and more details about TeamSTEPPS. The research team agreed with and implemented most suggested changes.
The TeamSTEPPS LEP module was successfully implemented in three hospitals despite hospital leadership concerns about the time and cost involved, competing quality initiatives, insufficient interpreter resources, and staff turnover. Master trainers from each hospital were trained in a 4-hr train-the-trainer session, and they in turn trained 268 staff members in varied settings at their respective hospitals, including two labor and delivery/obstetrics units, an emergency department, and a pediatric primary care clinic. The module served as a catalyst for institutional change, as sites reallocated interpreter resources to better cover the areas of greatest need, clarified interpreter use policies, and expanded their certification programs to allow healthcare providers to deliver care in a non-English language that they are fluent in. As a result of the training, clinical staff reported feeling more aware of the need to call an interpreter, and interpreters felt more empowered to address communication issues with the clinical team, for example by requesting a briefing or calling a “time out” to ask for clarity. However, formal evaluation was challenging for all sites, even with the evaluation guide provided by the research team.
For the two sites that completed trainee satisfaction surveys, trainee satisfaction scores were high: mean 2.94 for one site and 3 for the other site on a scale of 1 to 3 (with 3 being the highest rating). Trainee knowledge scores increased at the two sites that administered both pre- and posttraining tests, from 50% to 83% in one of the TeamSTEPPS sites (t(26) = 8.12, p < .001) and from 60% to 76% in the non-TeamSTEPPSsite (t-statistic not calculated for the second site because the local evaluation team tabulated scores question by question, instead of by respondent). Two sites tried to use their own interpreter service use data to quantitatively evaluate changes in provider behaviors before and after training, but could not obtain valid pre- and postintervention denominators for LEP patient volume due to data quality issues. No sites implemented the provider behavior survey and patient outcome surveys that were offered as part of the TeamSTEPPS evaluation guide.
Several edits were made to the Module in response to field sites’ experience implementing it. For example, the time estimate to complete the module was changed from 1 hr to 1.5 hr; we added material in response to requests for guidance on managing a patient’s or family member’s resistance to the use of an interpreter; and we added to the evaluation guide a recommendation that change teams assign a team member dedicated to the evaluation task.
Limitations
In the content development phase, each evidence source taken individually had its own limitations. The systematic literature review identified key findings and evidence-based recommendations, but it lacked the richness needed to develop realistic content. The interpreter pilot, in-depth interviews, and Town Hall provided more richness of experience but lacked generalizability. Finally, the adverse events database analysis provided information about where LEP patients might be most likely to experience adverse events, but data quality issues prevented us from identifying the universe of patients not proficient in English. Using the data sources in combination provided a more comprehensive source of evidence than any one source alone, but the evidence gathered may not be generalizable to all hospitals that might use AHRQ’s new tools.
In the field testing phase, resource limitations only allowed us to work with small samples. Field testing allowed us to ascertain that the tools are acceptable to key audiences, implementable, and conducive to learning. This is important to establish the evaluability of the tools. Field testing did not, however, provide an indication of the impact of the tools on LEP patient safety. Ultimately, the data recommendations from the Hospital Guide will need to be implemented more widely before data quality is sufficiently improved to allow for a valid evaluation of LEP patient safety outcomes.
Conclusion
As hospitals continue to improve quality and meet the Joint Commission’s patient-centered communication standards for hospitals and other new accreditation standards, they will look for resources in these critical areas of patient safety. We recommend that hospitals consider implementing Improving Patient Safety Systems for Patients With Limited English Proficiency: A Guide for Hospitals and the TeamSTEPPS Enhancing Safety for Patients with Limited English Proficiency Module as part of their strategy to meet the new standards. These tools provide the case for why this field is important, and the basic strategies necessary to build safety systems that truly protect all patients. The small sample of hospitals and hospital leaders used to validate these tools, and data quality issues preventing us from conducting an impact assessment, are limitations of this study. Further research on the impact of the combined use of the Guide and Module would shed light on their value as a multifaceted intervention.
Journal for Healthcare Quality is pleased to offer the opportunity to earn continuing education (CE) credit to those who read this article and take the online posttest at http://www.nahq.org/education/content/jhq-ce.html. This continuing education offering, JHQ 248, will provide 1 contact hour to those who complete it appropriately.
Core CPHQ Examination Content Area
IV. Patient Safety
Learning Objectives.
Describe the heightened safety risk for patients with limited English proficiency (LEP)
Describe the content and validation of the Guide for Hospitals and TeamSTEPPS LEP module
Evaluate whether the Guide for Hospitals and TeamSTEPPS LEP module may be beneficial for your organization
Posttest questions.
- Evidence shows that patients with limited English proficiency have a heightened safety risk because:
- LEP patients experience discrimination in medical settings
- LEP patients experience more medical communication errors than non-LEP patients
- LEP patients have riskier conditions than non-LEP patients
- LEP patients delay care-seeking longer than non-LEP patients
- Which of the following is usually NOT a high-risk scenario for a Spanish-speaking LEP patient?
- The patient’s wife, who speaks English fluently, is interpreting for her husband and the doctor
- The nurse speaks some Spanish, the patient speaks some English
- The doctor is using a telephone interpreter while waiting for an in-person interpreter to arrive
- The patient is being discharged from the hospital with no interpreter present.
- It is challenging for hospitals to monitor LEP patient safety because …
- Patient safety reports often cannot be linked to patient language data
- LEP patients are less likely to report patient safety events than non-LEP patients
- Clinicians are less likely to report patient safety events that happen to LEP patients
- There is little or no funding for this type of activity
- In the Guide for Hospitals (available here: http://www.ahrq.gov/legacy/populations/lepguide/index.html), which of the following strategies are recommended to better identify medical errors affecting LEP patients?
- Ask patients about the role of language in causing medical errors they experienced
- Use patient surname to identify LEP patients in patient safety records
- Perform manual chart reviews to identify the role of language in patient safety events
- Collect race, ethnicity and patient language data; link the data to patient safety reports
- Which of the following strategies does the Guide for Hospitals recommend to prevent errors affecting LEP patients?
- Spanish classes for health care professionals
- Disciplinary action for medical staff who fail to use an interpreter
- Strengthening interpreter services, team communication training
- Stationing bilingual volunteers at the bedside of LEP patients
- Which of the following is NOT a goal of the Guide for Hospitals?
- Inventory current hospital practices to address culture and language issues
- Foster a supportive culture for safety of diverse patient populations
- Develop strategies and systems to prevent medical errors among LEP patients
- Help hospitals to empower frontline staff and interpreters to report medical errors
- In the TeamSTEPPS module (available here: http://www.ahrq.gov/legacy/teamsteppstools/lep/), the Staff Training Instructor guide describes how health care team leaders can create psychological safety for interpreters, and how interpreters can create psychological safety for patients. Which of the following describes how to create psychological safety?
- Smile and be yourself
- Proactively invite input, be accessible, ask for mutual support
- Speak in a reassuring tone of voice, hold the patient’s hand
- Use plain language to explain treatment options
- Which of the following is NOT a goal of the TeamSTEPPS LEP module?
- Describe the heightened safety risks for LEP patients
- Describe the benefits of including a qualified interpreter on the care team
- Provide structured communication tools to address communication and safety issues
- Teach hospital staff about different patient cultures
- The field-test process for the TeamSTEPPS LEP module provided information about …
- The module’s implementability, trainee satisfaction, and learning outcomes
- The module’s implementability, trainee behavior change, and cost of implementation
- Trainee learning, trainee behavior change, and patient outcomes
- Barriers, costs and facilitators of implementation
- Which of the following challenges was most difficult for hospitals to address during the TeamSTEPPS LEP module field test?
- Insufficient time
- Cost
- Staff turnover
- Evaluating staff behavior change
Biographies
Authors’ Biographies
Melanie Wasserman, PhD, MPA, is a Senior Associate at Abt Associates who uses rigorous qualitative, quantitative, and technical assistance methods to further the practice of evidence-based care and prevention and to reduce health disparities. Over the past 12 years, Dr. Wasserman’s work has focused on improving access to high-quality care for LEP, culturally diverse, and other vulnerable populations. She also has formal training and prior experience as translator and interpreter.
Megan R. Renfrew, MA is Senior Project Manager at the Massachusetts General Hospital Physicians Organization and former Senior Project Coordinator at the Disparities Solutions Center. She coordinates quality improvement initiatives focused on improving quality and decreasing costs and efforts to assess surgical appropriateness. Ms. Renfrew has over 14 years of experience in research and project management with a focus on racial and ethnic disparities in care, cross-cultural care, and quality improvement.
Alexander R. Green, MD, MPH, is the Associate Director of the Disparities Solutions Center and Senior Scientist at the Mongan Institute for Health Policy at Massachusetts General Hospital. He is also Chair of the Cross-Cultural Care Committee at Harvard Medical School. His work focuses on programs designed to eliminate racial and ethnic disparities in care, including the use of culturally competent quality improvement interventions, leadership development, and dissemination strategies.
Lenny Lopez, MD, MDiv, MPH, is Senior Faculty at the Disparities Solutions Center. Dr. Lopez is an internist trained at the Brigham and Women’s Hospital (BWH), an Assistant Professor at Harvard Medical School, and is an Assistant at the Mongan Institute for Health Policy at Massachusetts General Hospital (MGH). His research interests extend across a range of issues relating to racial and ethnic disparities including language barriers and patient safety, quality measurement and improvement in hospital care, and the impact of health information technology on disparity reduction.
Aswita Tan-McGrory, MBA, MSPH, is the Deputy Director of the Disparities Solutions Center. She is a key member of the senior management team and supervises the broad portfolio of projects and administration of the Center. In addition, she works closely with the Director to chart the DSC’s future growth and strategic response to an ever-increasing demand for the Center’s services. Her interests are in providing equitable care to underserved populations and she has over 19 years of professional experience in the areas of disparities, maternal/child health, elder homelessness, and HIV testing and counseling.
Cindy Brach, MPP, is a senior health policy researcher at the Agency for Healthcare Research and Quality (AHRQ), where she conducts and oversees research on cultural competence, health literacy, primary care improvement, and Medicaid and CHIP. In addition to overseeing the development of TeamSTEPPS LEP tools, she has overseen the development of the AHRQ Health Literacy Universal Precautions Toolkit, the CAHPS Item Set for Addressing Health Literacy, and the Re-engineered Discharge (RED) Toolkit. She also serves on the Institute of Medicine (IOM) Health Literacy Roundtable and was a member of the National Project Advisory Committee for the enhancement of the National Standards for Culturally and Linguistically Appropriate Services.
Joseph R. Betancourt, MD, MPH, directs the Disparities Solutions Center at Massachusetts General Hospital, which works with healthcare organizations to improve quality of care, address racial and ethnic disparities, and achieve equity. He is Director of Multicultural Education for Massachusetts General Hospital (MGH), and an expert in cross-cultural care and communication. Dr. Betancourt served on several Institute of Medicine committees, including those that produced Unequal Treatment: Confronting Racial/Ethnic Disparities in Health Care and Guidance for a National Health Care Disparities Report.
Footnotes
Due to space limitations, only a summary of the methods and results is provided in this article. Further details are available upon request from the corresponding author.
Disclaimer
The views expressed in this paper are those of the authors. No official endorsement by any agency of the federal government is intended or should be inferred.
References
- AHRQ TeamSTEPPS® enhancing safety for patients with limited English proficiency module. 2012a Retrieved February 3, 2014, from www.ahrq.gov/legacy/teamsteppstools/lep/
- AHRQ Improving patient safety systems for patients with limited English proficiency: A guide for hospitals. 2012b Retrieved February 3, 2014, from www.ahrq.gov/legacy/populations/lepguide/index.html.
- Carbone E, Gorrie J, Oliver R. Without proper language interpretation, sight is lost in Oregon and a $350,000 verdict is reached. Legal Review and Commentary Supplement Healthcare Risk Management. 2003;23(Suppl 13):2. [Google Scholar]
- Clancy CM, Tornberg DN. TeamSTEPPS: Assuring optimal teamwork in clinical settings. American Journal of Medical Quality. 2007;22:214–217. doi: 10.1177/1062860607300616. [DOI] [PubMed] [Google Scholar]
- Diamond LC, Schenker Y, Curry L, Bradley EH, Fernandez A. Getting by: Underuse of interpreters by resident physicians. Journal of General Internal Medicine. 2009;24:256–262. doi: 10.1007/s11606-008-0875-7. 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Divi C, Koss RG, Schmaltz SP, Loeb JM. Language proficiency and adverse events in US hospitals: A pilot study. International Journal for Quality Health Care: Journal of the International Society for Quality in Health Care. 2007;19:60–67. doi: 10.1093/intqhc/mzl069. [DOI] [PubMed] [Google Scholar]
- Flores G. The impact of medical interpreter services on the quality of health care: A systematic review. Medical Care Research and Review. 2005;62:255–299. doi: 10.1177/1077558705275416. [DOI] [PubMed] [Google Scholar]
- Flores G, Laws MB, Mayo SJ, Zuckerman B, Abreu M, Medina L, et al. Errors in medical interpretation and their potential clinical consequences in pediatric encounters. Pediatrics. 2003;111:6–14. doi: 10.1542/peds.111.1.6. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine (IOM) In: To err is human: Building a safer health system. Kohn LT, Corrigan JM, Donaldson MS, editors. National Academy Press; Washington, DC: 1999. [PubMed] [Google Scholar]
- Office of Minority Health The national CLAS standards. 2013 Retrieved October 15, 2013, from http://minorityhealth.hhs.gov/templates/browse.aspx?lvl=2&lvlID=15.
- Price-Wise G. Language, culture, and medical tragedy: The case of Willie Ramirez. Health Affairs Blog. 2008 Retrieved November 19, 2008, from http://health-affairs.org/blog/2008/11/19/language-culture-and-medical-tragedy-the-case-of-willie-ramirez/
- Quan K. The high costs of language barriers in medical malpractice. University of California, School of Public Health, National Health Law Program; Berkeley, CA: 2010. Retrieved from www.healthlaw.org/images/stories/High_Costs_of_Language_Barriers_in_Malpractice.pdf. [Google Scholar]
- The Joint Commission Advancing effective communication, cultural competence, and patient- and family-centered care: A roadmap for hospitals. 2010 Retrieved from www.jointcommission.org/assets/1/6/aroadmapforhospitalsfinalversion727.pdf.
- The Joint Commission Sentinel event data: Root causes by type. 2012 Retrieved May 3, 2012, from www.jointcommission.org/Sentinel_Event_Statistics/
- U.S. Census Bureau American Community Survey (ACS) [electronic version], from data assessed through American Factfinder. 2009 Retrieved June 1, 2010, from http://factfinder.census.gov/home/saff/main.html?_lang=eng.
- Wilson-Stronks A, Galvez E. Hospitals, language and culture: A snapshot of the nation. The Joint Commission/The California Endowment; Chicago, IL: 2009. Retrieved from www.jointcommission.org/assets/1/6/hlc_paper.pdf. [Google Scholar]