Abstract
Social anxiety and eating disorders are highly comorbid. Several explanations for these high levels of comorbidity have been theorized. First, social anxiety might be a vulnerability factor for eating disorders. Second, eating disorders might be a vulnerability factor for social anxiety. Third, the two kinds of disorders may have common, shared psychological vulnerabilities. The current study (N = 300 undergraduate women) investigates a model of social anxiety and eating disorder symptoms that examines each of these possibilities across two time points (Time 1 and six months later). We do not find support for either social anxiety or eating disorder symptoms per se predicting each other across time. Instead, we find that some underlying vulnerabilities prospectively predict symptoms of both disorders, whereas other vulnerabilities are specific to symptoms of one disorder. Specifically we find that maladaptive perfectionism is a shared prospective vulnerability for social anxiety and eating disorder symptoms. Alternatively, we find that social appearance anxiety is specific for eating disorder symptoms, whereas high standards is specific for social anxiety symptoms. These data help clarify our understanding of how and why social anxiety and eating disorder symptoms frequently co-occur.
Keywords: eating disorders, social anxiety, longitudinal data, social appearance anxiety, fear of negative evaluation, perfectionism, comorbidity
Eating and anxiety disorders are highly comorbid, with some studies reporting that up to 83 percent of individuals with an eating disorder also meet criteria for an anxiety disorder (e.g., Godart, Flament, Lecrubier, & Jeammet, 2000; Pallister & Waller, 2008). Social anxiety disorder (SAD) has the highest occurrence of all anxiety disorders in individuals with eating disorders and is significantly more common among individuals with eating disorders than in control groups (Godart et al., 2003; Godart et al., 2000). Further, individuals with SAD are more likely to report disordered eating than controls, and, in individuals with SAD, it has been reported that 20% meet criteria for an eating disorder (Becker, DeViva, & Zayfert, 2004; Godart et al., 2003). We clearly need more research identifying how and why these disorders so frequently co-occur.
Some researchers propose that SAD itself (i.e., a categorical diagnosis of SAD) may create risk for eating disorders, based primarily on retrospective reports showing that SAD may develop earlier than eating disorders (Godart et al., 2003; Kaye et al., 2006; Swinbourne & Touyz, 2007). However, we are aware of only one study that has tested the prospective relationships between SAD and eating disorders. These researchers found the opposite of what has typically been hypothesized to occur. Instead of finding that SAD increased risk for eating disorders, these researchers found that a diagnosis of bulimia nervosa increased risk to receive a later diagnosis of SAD (Buckner, Silgado, & Lewinsohn, 2010).
Alternatively, it may be that neither set of symptoms (eating disorder or social anxiety) create vulnerability for each other. Instead, it has been suggested that shared underlying psychological factors create vulnerability for both disorders (Godart et al., 2003; Pallister & Waller, 2008). This idea has been proposed and supported in other models of comorbidity, such as models explaining why internalizing disorders (depression and anxiety) may co-occur frequently (e.g., Mineka, Watson, & Clark, 1998). These three potential explanations of why SAD and ED co-occur (SAD leading to eating disorders, eating disorders leading to SAD, or shared vulnerabilities leading to both disorders) bring up several important research questions. Namely, (a) do eating disorder symptoms create vulnerability for social anxiety symptoms? (b) do social anxiety symptoms create vulnerability for eating disorder symptoms, or (c) are there shared underlying psychological vulnerabilities that contribute to symptoms of both disorders? Indeed, researchers are beginning to test both (a) if social anxiety and disordered eating symptoms confer vulnerability for each other and (b) if shared vulnerability factors contribute to both disorders (Buckner, Silgado, & Lewinsohn, 2010; Levinson & Rodebaugh, 2012; Levinson et al., 2013).
Several underlying vulnerabilities have been proposed to contribute to both social anxiety and eating disorders, and those that have received the most attention to date are perfectionism (e.g., Shafran, Cooper, & Fairburn, 2002), fear of negative evaluation (e.g., Deboer et al., 2013), and social appearance anxiety (e.g., Levinson et al., 2013). We will briefly outline each of the proposed vulnerability factors below and the existing research that has tested these factors in a combined model of shared vulnerability (Levinson & Rodebaugh, 2012; Levinson et al., 2013; Levinson & Rodebaugh, 2015).
Perfectionism
Perfectionism is elevated in both socially anxious individuals and those with eating disorders as compared to controls (Antony, Purdon, Huta, & Swinson, 1998; Bardone-Cone et al. 2007; Bastiani, Rao, Weltzin, & Kaye, 1995) and has been posited to be a risk factor for the development of these disorders (e.g., Bardone-Cone et al., 2007; Heimberg, Juster, Hope, & Mattia, 1995; Hope, Heimberg, & Klein, 1990; Jacobi, Hayward, de Zwaan, Kraemer, & Agras, 2004; Stice, 2002). Research suggests that there are two dimensional aspects of perfectionism (Hewitt, Flett, Turnbull-Donovan, & Mikail, 1991): An adaptive type (e.g., high standards), related to healthy functioning (DiBartolo, Frost, Chang, LaSota, & Grills, 2004) and a maladaptive type (e.g., evaluative perfectionism in which the individual is highly concerned with making mistakes), related to negative outcomes such as anxiety and depression (DiBartolo, Li, & Frost, 2008). Research has found that maladaptive perfectionism has a strong positive relationship with social anxiety, whereas high standards have a weaker, inverse relationship with social anxiety (Shumaker & Rodebaugh, 2009). In contrast, elevated levels of high standards are often seen within individuals with eating disorders (Bastiani et al., 1995; Boone, Soenens, Braet, & Goossens, 2010; Bardone-Cone et al., 2007).
Fear of Negative Evaluation
Fear of negative evaluation is the fear that one’s self will be judged negatively. Clinical samples of women with eating disorders report higher levels of fear of negative evaluation than controls (Hinrichsen, Wright, Waller, & Meyer, 2003). Additionally, in a non-clinical sample, Gilbert & Meyer (2003) found that, in a cross-sectional dataset, fear of negative evaluation was associated with drive for thinness over and above depression. Further, it was found that inclusion of fear of negative evaluation (or fear of social rejection) improves the predictive validity of the dual pathway model (e.g., Duemm, Adams, & Keating, 2003; Utschig, Presnell, Madeley, & Smits, 2010). In the SAD literature, fear of negative evaluation is considered a cognitive risk factor for SAD (Haikal & Hong, 2010) and is included, in some fashion, in each of the cognitive models of SAD (Clark & Wells, 1995; Heimberg, Brozovich, & Rapee, 2010; Hofmann, 2007).
Social appearance anxiety
Social appearance anxiety is the fear that one will be negatively evaluated because of one’s appearance (Hart et al., 2008). Social appearance anxiety is positively correlated with measures of social anxiety and negative body image (Claes et al., 2012), but does not represent mere overlap among these other constructs. Instead, social appearance anxiety taps into a unique proportion of variability in social anxiety beyond negative body image, depression, personality, and affect (Hart et al., 2008; Levinson & Rodebaugh, 2011). In a clinical sample, Koskina, Van den Eynde, Meisel, Campbell, and Schmidt (2011) found that individuals with a diagnosis of bulimia nervosa had significantly higher levels of social appearance anxiety than healthy controls, and Claes and colleagues (2011) found that social appearance anxiety was positively related to body mass index (BMI), drive for thinness, and body dissatisfaction in women diagnosed with an eating disorder.
Combined Vulnerability Model
Researchers have sought to delineate if each of these vulnerability factors are shared between SAD and eating disorders. Given strong but incomplete comorbidity between these disorders (i.e., not every individual with an eating disorder has SAD), it seems plausible that there are both specific vulnerability factors (i.e., factors that contribute to only one disorder) and shared vulnerability factors between the disorders. Each of these factors (perfectionism, fear of negative evaluation, and social appearance anxiety) had previously been tested independently as risk factors for social anxiety and eating disorders, but not in one combined model. To To this end, perfectionism, fear of negative evaluation, and social appearance anxiety were tested in a cross-sectional shared vulnerability model in three independent samples to test the unique relationships between these constructs and eating disorder and social anxiety symptoms (Levinson & Rodebaugh, 2012; Levinson et al., 2013). In these models, fear of negative evaluation and high standards (inversely) were associated with social anxiety, whereas maladaptive perfectionism was associated with eating disorder symptoms. Social appearance anxiety was associated with symptoms of both disorders. These relationships held over and above BMI, negative affect, and depression. These relationships were tested further in an experimental paradigm and it was found that social appearance anxiety created risk for body dissatisfaction and social anxiety, whereas fear of negative evaluation increased food intake (Levinson & Rodebaugh, 2015). From this research, it is unclear if these factors are merely correlates of social anxiety and eating disorder symptoms, or if these vulnerability factors are predictive across time. Prospective research is needed to clarify this question and is a specific aim of this study. We expect that these factors may serve as either shared or specific prospective vulnerability factors for eating disorder and social anxiety symptoms. In other words, it seems likely that social appearance anxiety and perfectionism may be shared vulnerability factors, whereas fear of negative evaluation may be a specific vulnerability factor for social anxiety only, based on prior cross-sectional work testing this model (Levinson et al., 2013).
Prospective Findings
One major limitation of the existing literature on vulnerability for social anxiety and eating disorders, including work on a shared vulnerability model, is that most research has been cross-sectional. Cole and Maxwell (2003) discuss the many benefits of using longitudinal analyses. Further, to appropriately test causal models in observational data it is necessary to include previous iterations of the construct under study combined with the passage of time (Cole & Maxwell, 2003; Maxwell & Cole, 2007; Selig & Preacher, 2009). Failing to do so raises the possibility that the apparent prospective relationship only establishes that the predicted variable correlates with itself across time. Clearly, data from true experiments would be preferable, but when only observational data are feasible (e.g., it would be unethical to attempt to manipulate sustained social anxiety), repeated measurement is crucial to forming reasonable inferences for further testing.
There have been few studies testing potential causal links between social anxiety and eating disorder symptoms prospectively, and even fewer testing these specific vulnerability factors (e.g., perfectionism, fear of negative evaluation) prospectively. As mentioned above, the one study that tested the longitudinal relationship between SAD and eating disorders found that SAD did not predict Anorexia Nervosa (AN) or Bulimia Nervosa (BN) (Buckner, Silgado, & Lewinsohn, 2010). The only significant prospective relationship these researchers found was that BN increased the risk of development of SAD (i.e., the effect proceeded in the opposite of the typically proposed direction).
There have also been few prospective studies testing the proposed shared vulnerability factors for SAD and eating disorders. Two studies found that fear of negative evaluation predicted increased bulimic symptoms over time (Gilbert & Meyers, 2005; Hamann, Wonderlich-Tierney, & Vander Wal, 2009). Another study found that fear of negative evaluation increased body dissatisfaction and eating disorder symptoms (Deboer et al., 2013). Regarding perfectionism, one study found that general perfectionism predicted young adult onset of AN, but not BN (Tyrka, Waldron, Graber, & Brooks-Gunn 2002). In two tests, perfectionism was not found to predict adolescent onset of eating disorders (Tyrka, Waldron, Graber, & Brooks-Gunn 2002; Wojtowicz & Ranson, 2012). Bardone-Cone et al. (2007) specifically recommended that prospective relationships between eating disorders and perfectionism need further investigation. We could locate no studies specifically assessing prospective relationships between perfectionism and social anxiety, though there have been studies showing that perfectionism decreases during cognitive behavioral therapy for SAD (e.g., Lundh & Ost, 2001; but see Rosser, Issakidis, & Peters, 2003 for a conflicting finding). We also could not locate any studies that have tested the prospective relationship between social appearance anxiety, eating disorder symptoms, and social anxiety. For the studies outlined above involving prospective relationships, the researchers tested each vulnerability factor independently and not in a single, combined model.
The Current Study
In the current study we tested the relationships between social anxiety, eating disorder symptoms, and these four proposed vulnerability factors (fear of negative evaluation, social appearance anxiety, high standards, and maladaptive perfectionism) in one model. We sought to replicate and extend the cross-sectional model from Levinson et al., 2013 to prospective data. We tested this model cross-sectionally and then across six months. We also test a model that includes only social anxiety and eating disorder symptoms across 6-months to clarify if these symptoms predict each other across time when not accounting for the vulnerability factors. These models test two primary research questions. First, do social anxiety and eating disorder symptoms predict each other over time? Second, which vulnerability factors prospectively predict social anxiety and eating disorder symptoms? These questions are important because if we are able to pinpoint a underlying mechanism we can build interventions focused on this vulnerability. In other words, if social appearance anxiety is a prospective predictor of social anxiety and eating disorder symptoms, we should arguably focus our interventions on social appearance anxiety specifically, rather than focusing on general social anxiety (as we should do if we expected that social symptoms in general lead to eating disorder symptoms).
We hypothesized that social anxiety and eating disorder symptoms per se would not predict each other, but the potential shared vulnerability factors would predict symptoms of both disorders. Regarding the specific vulnerabilities, based on Levinson et al., 2013, we had the following hypotheses. First we hypothesized that maladaptive perfectionism, high standards, and social appearance anxiety would prospectively predict eating disorder symptoms. Second, we hypothesized that maladaptive perfectionism, fear of negative evaluation, high standards, and social appearance anxiety would predict social anxiety symptoms.
We tested these hypotheses in an all-female young adult sample because women are at higher risk than men for the development of disordered eating and this age group represents a crucial time period when eating disorders emerge (Taylor et al., 2006). Focusing on this group allowed us greater power to delineate what factors might increase the vulnerability toward eating disorder symptoms and social anxiety because it is a high risk, but non-clinical sample (i.e., the majority of participants did not already have a disorder but were vulnerable to developing an eating disorder or SAD). We chose to test these symptoms dimensionally (and therefore in a non-clinical sample), in line with other comorbidity models in the field, as well as to have the full range of symptomatology present (e.g., Krueger & Piasecki, 2002).
Methods
Participants
Participants were 300 undergraduate women who participated for course credit. College women are an ideal population for this study because they are a high risk sample for the development of an eating disorder (Taylor et al., 2006). Indeed, participants’ disordered eating scores at Time 1 (as measured by the Eating Disorder Inventory-2; Garner, 1991) ranged from very low to very high. Scores ranged from 0 to 21 on Drive for Thinness (M = 4.09, SD = 4.63; 3% scoring at or above the mean of a clinical sample of women with eating disorders from Garner et al., 1983), from 0 to 17 on Bulimia (M = 1.12; SD = 2.25; 8.7% scoring in the clinical range), and from 0 to 27 on Body Dissatisfaction (M = 6.95, SD = 5.76; 10.7% scoring in the clinical range). A sizable number of women crossed from either clinical to nonclinical, or nonclinical to clinical levels of these scales across the study: from Time 1 to Time 2 (6 months later), 57 participants crossed. More specifically, at Time 2 the following number of participants crossed from a non-clinical to clinical threshold on Drive for Thinness (n = 3; 3% in clinical range), Bulimia (n = 18; 9.6% in clinical range), and on Body Dissatisfaction (n = 16; 13.3% in clinical range). Additionally, participants’ social anxiety scores (as measured by the Straightforward Social Interaction Anxiety Scale; Mattick & Clarke, 1998; Rodebaugh et al., 2011) ranged from very low (0) to very high (61), with a mean score of 22.06 (SD = 12.31). A total of 26.6% of participants scored a 28 or higher, which has been suggested as a cut-off score for probable social anxiety disorder (Rodebaugh et al., 2011). At Time 2, 25.0% participants scored a 28 or higher, with 21 participants crossing the threshold from non-clinical to clinical status from Time 1 to Time 2 (46 participants crossing in either direction).
Participants were mostly Caucasian (n = 182, 60.7%). Other ethnicities reported were Asian (n = 82, 19.3%), Black (n = 12, 4.0%), Hispanic (n = 8, 2.7%), multi-racial (n = 15, 5.0%), and 1 participant reported ethnicity as not listed. Participants had a median age of 18.00 (SD = 1.05) and most participants were in their 1st year of undergraduate school (N = 164; 57.1%).
Measures
The Eating Disorder Inventory-2 (EDI-2) (Garner, 1991) is a 91-item self-report questionnaire designed to measure core psychological features commonly associated with anorexia nervosa (AN) and bulimia nervosa (BN) (e.g., I eat when I am upset; I think about dieting). The EDI-2 has good internal consistency and good convergent and discriminant validity (Garner, 1991) and clinicians frequently use the EDI-2 to assess for eating disorder symptoms (Brookings & Wilson, 1994). We used three of the eleven EDI-2 subscales for this study: the Drive for Thinness, Body Dissatisfaction, and Bulimia subscales. These subscales (the “symptom indices”) were used because they assess core features of AN and BN and are most frequently used to identify possible eating disorder case status. The Drive for Thinness subscale includes 7-items that assess excessive concern with dieting, preoccupation with weight, and fear of gaining weight. The Body Dissatisfaction subscale includes 9-items that assess dissatisfaction with overall body shape as well as the size of specific regions of the body, such as hips, stomach, and thighs. The Bulimia subscale includes 7-items that assess bulimic behaviors such as bingeing and purging. These three subscales were standardized and combined to create a measure of eating disorder symptoms. In the current study, internal consistencies were adequate (αs = .73−.79).
The Social Interaction Anxiety Scale (SIAS) (Mattick & Clarke, 1998) is a 20-item measure designed to assess social interaction anxiety. The items describe anxiety-related reactions to a variety of social situations (e.g., I have difficulty talking with other people; I am tense mixing in a group). Overall, research on the scale suggests good to excellent reliability and good construct validity (Heimberg & Turk, 2002). The three reverse-scored items were omitted for all statistical analyses, as available evidence suggests that these items fail to load on the same factor as the other items (S-SIAS; Rodebaugh, Woods, Heimberg, Liebowitz, & Schneier, 2006) and appear less related to social anxiety and more related to extraversion than is desirable (Rodebaugh, Woods, & Heimberg, 2007). Removal of the reverse-scored items has no negative effects on the validity of the scale, and generally improves convergent validity (Rodebaugh et al., 2011). In the current study, internal consistencies were excellent (αs = .92 −.96).
The Frost Multidimensional Perfectionism Scale (FMPS) (Frost, Marten, Lahart, & Rosenblate, 1990) measures several dimensional aspects of perfectionism: Concern over Mistakes, Doubts about Actions, Parental Criticism, Parental Expectations, Personal Standards, and Order and Organization. We used a combination of these subscales to create a measure of maladaptive perfectionism and high standards as used in previous research (Frost et al., 1993; DiBartolo et al., 2004). The Maladaptive Perfectionism (MP) subscale sums items from the Concern over Mistakes, Doubts about Actions, Parental Criticism, and Parental Expectations subscales. The MP assesses critical self-evaluation and perceptions of parentally influenced perfectionism. An example item is People will probably think less of me if I make a mistake. The MP is related to indicators of poor psychological functioning, such as self-concealment and depression (DiBartolo et al., 2008). To measure high standards we used the Pure Personal Standards subscale that includes the Personal Standards subscale items that are least related to fear of negative evaluation (DiBartolo et al., 2004). An example item is I set higher goals for myself than most people. We utilized this scoring because confirmatory factor analyses suggest that these two facets exhibit the best fit versus a single factor structure for the FMPS (Cox, Enns, & Clara, 2002). Internal consistencies for maladaptive perfectionism were adequate (αs = .73−.76) and for high standards were good (αs = .81−.86).
The Brief Fear of Negative Evaluation (BFNE) scale (Leary, 1983) is a 12-item version of the original Fear of Negative Evaluation scale (Watson & Friend, 1969). The items (e.g., I am afraid others will not approve of me) assess fear of negative evaluation. The BFNE has been shown to correlate positively with other measures of social anxiety and has excellent psychometric properties both in college and clinical samples when the four reverse scored items are excluded, as they are here (for a discussion of the improved validity of the BFNE with removal of reverse-scored items, please see Rodebaugh et al., 2011). Internal consistencies for fear of negative evaluation were excellent (αs = .91−.94).
The Social Appearance Anxiety Scale (SAAS) (Hart et al., 2008) is a 16-item measure developed to assess anxiety about being negatively evaluated by others because of one’s overall appearance, including body shape. Research on the psychometric properties of the SAAS demonstrated high test-retest reliability, good internal consistency, and good factor validity, incremental validity (e.g., it was uniquely associated with social anxiety above and beyond negative body image indicators), and divergent validity in college age samples (Hart et al., 2008 Levinson & Rodebaugh, 2011). Example items from the SAAS are I am concerned people would not like me because of the way I look and I am afraid that people find me unattractive. Internal consistencies for the SAAS were excellent (αs = .94−.95).
Procedure
All procedures were approved by the Washington University Institutional Review Board. Participants were invited to participate in a longitudinal study on personality and behavior. Participants completed all measures listed above at two time points: Time 1 and six months after Time 1 (Time 2). Participants were awarded course credit or entry into a gift card raffle. Nearly two-thirds of participants returned for the session (n = 190; 63.3%). Many participants did not return because they no longer needed course credit. There were no significant differences on any measures between completers and non-completers. Missing data was imputed (see data analytic plan below) and therefore we were able to use data from all 300 participants. There were no substantial changes to any of the results when analyzed with imputed versus non-imputed data.
Data Analytic Plan
Mplus program Version 7.1 (Muthén & Muthén, 1998-2014) was used for all structural equation modeling analyses utilizing the MLM estimator to report standardized path estimates. This estimator was used because it corrects for any potential violations to multivariate normality. Model fit was evaluated using the: (a) comparative fit index (CFI) (Bentler, 1990), (b) Tucker-Lewis incremental fit index (TLI) (Tucker & Lewis, 1973), (c) root mean square error of approximation (RMSEA) (Steiger & Lind, 1980), and (d) standardized root mean square residual (SRMR) (Jöreskog, 1979). The magnitudes of these indices were evaluated with the aid of recommendations by Hu and Bentler (1999). For the CFI and TLI, values of .90 and above were considered adequate, whereas values of .95 or above were considered very good; for the RMSEA and SRMR, values of .08 and below were considered adequate and .05 or less very good. We first tested fully saturated models (df = 0) and then tested models with non-significant paths removed to provide a meaningful test of model fit.
Missing data were estimated using multiple imputation (MI) performed in Amelia II (Honaker, King, & Blackwell, 2006-2008). The data used for MI included items for all measures used in analyses below with a ridge prior set at 3. We used three diagnostics (comparing densities, overimpution, and overdispersed starting values) that examine ways that imputation might fall short of properly representing the likely values of the missing data; please see Honaker et al. for details. Diagnostics indicated that our imputation had been successful.
First, we tested a model with all variables measured at Time 1 (cross-sectional model) to replicate the cross-sectional model from Levinson and Rodebaugh (2012). Next, we tested two prospective models (a) a model including only social anxiety and eating disorders symptoms and (b) a model including both types of symptoms and the four vulnerabilities.
Results
Descriptives and Zero-Order Correlations
All descriptive statistics for study variables are presented in Table 1. As can be seen in Table 1, most study variables were moderately to strongly correlated.
Table 1.
Descriptive statistics and zero-order correlations among all study variables at Time 1 and Time 2 (6 months later)
| T1SAA | T1FNE | T1HS | T1MP | T1SIAS | T1BD | T1DT | T1BN | T2SAA | T2FNE | T2HS | T2MP | T2SIAS | T2BD | T2DT | T2BN | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||||||
| Mean (SD) |
29.80 (12.23) |
23.33 (6.94) |
18.76 (3.66) |
57.61 (15.10) |
22.06 (12.23) |
−5.64 (8.83) |
14.71 (6.66) |
13.63 (5.08) |
28.58 (12.83) |
20.24 (7.13) |
17.75 (4.26) |
53.90 (15.30) |
19.47 (12.21) |
−6.11 (9.96) |
13.21 (5.96) |
13.79 (5.68) |
| T1SAA | _ | .60** | .01 | .37** | .58** | .49** | .36** | .39** | .68** | .59** | .01 | .33** | .51** | .47** | .38** | .29** |
| T1FNE | _ | .18* | .40** | .53** | .35** | .31** | .33** | .41** | .70** | .12 | .34** | .51** | .24** | .26** | .40** | |
| T1HS | _ | .33** | .42** | −.02 | .19** | .27** | .01 | .18* | .61** | .23** | −.01 | −.02 | .19** | .05 | ||
| T1MP | _ | .42** | .35** | .33** | .27** | .37** | .39** | .33** | .70** | .42** | .28** | .32** | .29** | |||
| T1SIAS | _ | .19* | .20** | .29** | .42** | .52** | .02 | .31** | .77** | .19** | .21* | .29** | ||||
| T1BD | _ | .46** | .42** | .54** | .42** | −.11 | .31** | .27** | .82** | .47** | .43** | |||||
| T1DT | _ | .55** | .23** | .19* | .11 | .23** | .01 | .42** | .72** | .69** | ||||||
| T1BN | _ | .32** | .28** | .05 | .27** | .19** | .45** | .47** | .69** | |||||||
| T2SAA | _ | .69** | −.03 | .47** | .54** | .64** | .50** | .56** | ||||||||
| T2FNE | _ | .02 | .52** | .65** | .42** | .37** | .42** | |||||||||
| T2HS | _ | .37** | −.01 | .29** | .32** | .34** | ||||||||||
| T2MP | _ | .45** | .29** | .32** | .34** | |||||||||||
| T2SIAS | _ | .28** | .19* | .32** | ||||||||||||
| T2BD | _ | .56** | .55** | |||||||||||||
| T2DT | _ | .57** | ||||||||||||||
| T2BN | _ | |||||||||||||||
Notes: T1 = Time 1; T2 = Time 2 (6 months later); SAA = social appearance anxiety; FNE = fear of negative evaluation; HS = high standards; MP = maladaptive perfectionism; SIAS = social interaction anxiety; BD = Eating Disorder Inventory-II Body Dissatisfaction; DT = Eating Disorder Inventory-II Drive for Thinness; BN = Eating Disorder Inventory-II Bulimia Symptoms; The Eating Disorder Symptoms shown in Figures 1-3 is a composite of BD, DT, and BN
p < .01,
p < .05
Cross-Sectional Model
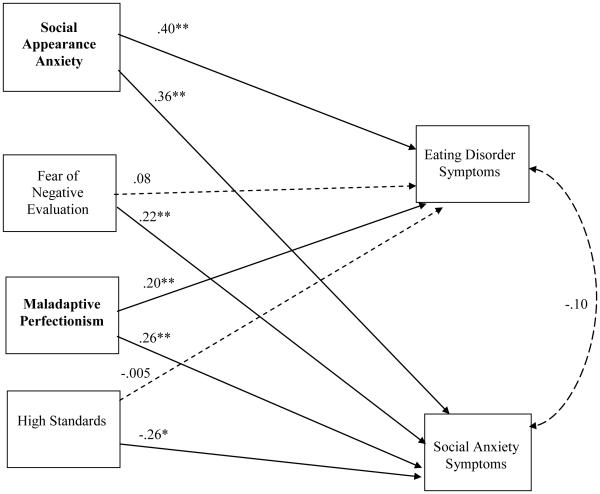
The initial model was saturated, making model fit perfect and therefore uninformative; when non-significant paths were removed so that the model was no longer saturated, fit remained excellent (CFI = .99, TLI = 1.00, RMSEA = .02, SRMR = .01). As can be seen in Figure 1, eating disorder symptoms were significantly predicted by social appearance anxiety and maladaptive perfectionism, but not by fear of negative evaluation and high standards. Social anxiety was predicted by all four risk factors: Fear of negative evaluation, social appearance anxiety, high standards, and maladaptive perfectionism. Social anxiety symptoms and eating disorder symptoms were significantly correlated (r = .19, p = .006) when the vulnerabilities were not accounted for, but were no longer significantly correlated when they were accounted for. Prospective Eating Disorder and Social Anxiety Symptom Model
Figure 1.
A cross-sectional model of social anxiety and eating disorder risk. Solid lines indicate significant relationships; dashed lines indicate non-significant relationships. Bolded risk factors are shared between both disorders. ** p < .01, * p < .05.
We first examined whether there was appreciable variance to be explained in Time 2 scores given Time 1 scores for social anxiety and eating disorder symptoms. Time 1 social anxiety predicted 59.1% of the variance in Time 2 social anxiety, indicating that there was 40.9% of the variance left to explain. Time 1 eating disorder symptoms predicted 64.2% of the variance in Time 2 eating disorder symptoms, indicating that there was 35.8% of the variance left to explain.
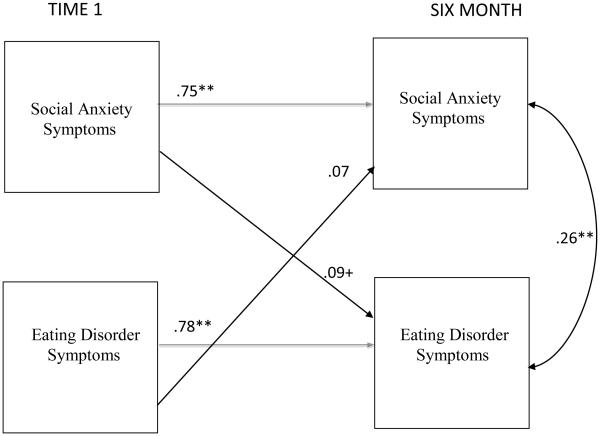
We then tested a model that included Time 1 and Time 2 social anxiety and eating disorder symptoms. Model fit was excellent (CFI = 1.00, TLI = 1.00, RMSEA = 0.00, SRMR = 0.00). As can be seen in Figure 2, social anxiety symptoms and eating disorder symptoms did not significantly predict each other across time.
Figure 2.
A six-month prospective model of social anxiety and eating disorder symptoms. Autoregressive parameters are shown in gray to ease interpretation. Time 1 = original assessment point. Six months = measures collected six months after the original assessment point. ** p < .01, * p < .05, + p < .10
Prospective Social Anxiety, Eating Disorder, and Vulnerabilities Model
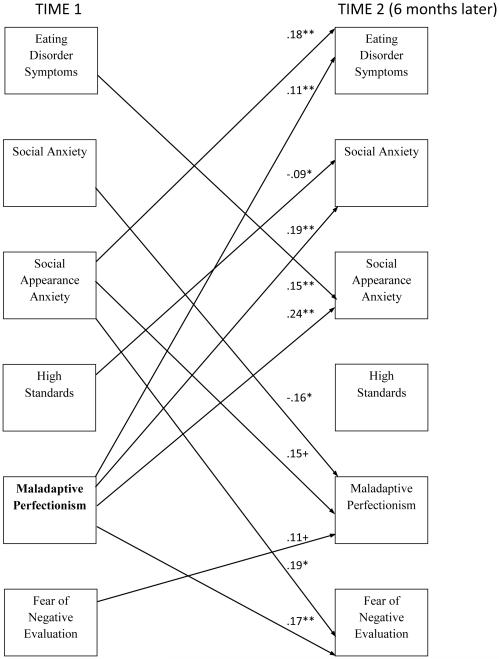
A saturated model was first fit, and when non-significant paths were removed so that the model was no longer saturated to provide meaningful model fit, fit remained adequate to excellent (CFI = .98, TLI = .95, RMSEA = .07, SRMR = .03). Echoing the cross-sectional model, and as can be seen in Figure 3, Time 1 social appearance anxiety and Time 1 maladaptive perfectionism significantly predicted Time 2 eating disorder symptoms. However, high standards did not significantly predict eating disorder symptoms prospectively. Turning to social anxiety, Time 1 maladaptive perfectionism predicted Time 2 social anxiety symptoms. Time 1 high standards was also a significant (negative) predictor of Time 2 social anxiety symptoms. Social anxiety symptoms did not predict eating disorder symptoms, nor did eating disorder symptoms predict social anxiety symptoms. Time 1 fear of negative evaluation did not predict either eating disorder or social anxiety symptoms.
Figure 3.
A prospective model of social anxiety and eating disorder risk. All relationships were modeled. Only tionships for which p <.10 are shown. Time 1 = original assessment point. Six month = measures collected months after the original assessment point. Autoregressive parameters are not shown to ease interpretation ge .46−.69). The bolded risk factor is shared between both disorders.** p< .01, * p< .05, + p<.10
To test if fear of negative evaluation was related to eating disorder symptoms without the inclusion of the other vulnerabilities, we also tested a model that did not include maladaptive perfectionism, high standards, or social appearance anxiety. This model only included Time 1 and Time 2 fear of negative evaluation, social anxiety, and disordered eating. Fear of negative evaluation did not significantly predict eating disorder symptoms when social appearance anxiety and perfectionism were removed (p = .190).
Discussion
We did not find that social anxiety prospectively predicted eating disorder symptoms, nor did we find that eating disorder symptoms prospectively predicted social anxiety. Instead, we found that (a) several of the vulnerability factors prospectively predicted either social anxiety and eating disorder symptoms and (b) that maladaptive perfectionism predicted symptoms of both social anxiety and eating disorders. These findings are important for our understanding of how social anxiety and eating disorder symptoms develop and co-occur with each other. Our findings go against the theory based on retrospective findings that social anxiety per se causes eating disorders (e.g., Godart et al., 2003; Kaye et al., 2006; Swinbourne & Touyz, 2007). Instead, we found that underlying vulnerabilities may be crucial for understanding why these disorders co-occur together.
Social appearance anxiety consistently predicted eating disorder symptoms cross-sectionally, and across six months, consistent with previous correlational and experimental research finding that social appearance anxiety is a vulnerability for disordered eating and possibly a component of social anxiety (Levinson & Rodebaugh, 2012; Levinson et al., 2013; Levinson & Rodebaugh, 2015). We did not find that social appearance anxiety prospectively predicted social anxiety symptoms. This finding is consistent with an alternative hypothesis that we find plausible: social appearance anxiety may not be a shared vulnerability factor, but rather a component of social anxiety (cross-sectionally correlated with other social anxiety symptoms) that is specifically relevant for the vulnerability toward an eating disorder. If supported by future research, this finding suggests that social appearance anxiety could be the specific type of social anxiety (rather than, for example, social interaction anxiety) that should be focused on for prevention of eating disorders (Godart et al., 2003; Kaye et al., 2006; Swinbourne & Touyz, 2007). Notably, we also did not find that fear of negative evaluation prospectively predicted either social anxiety or eating disorder symptoms. This finding may be because social appearance anxiety is a specific form of fear of negative evaluation (e.g., focused on one’s appearance) and therefore may account for the relationship between fear of negative evaluation and eating disorder symptoms. We hope future research will test this idea in multiple waves of data.
We also found that maladaptive perfectionism consistently predicted social anxiety across all models. However, the only shared vulnerability factors between social anxiety and eating disorder symptoms were (a) social appearance anxiety cross-sectionally and (b) maladaptive perfectionism in the prospective model. These findings suggest that there are both shared and specific vulnerability factors for social anxiety and eating disorder symptoms. Social appearance anxiety may be a specific vulnerability factor for eating disorder symptoms, whereas fear of negative evaluation is a specific vulnerability factor for social anxiety symptoms. On the other hand, maladaptive perfectionism may be a shared vulnerability. These findings are important for several reasons. First, they suggest that when an individual presents for treatment with comorbid social anxiety and eating disorder symptoms, clinicians should consider intervening on social appearance anxiety. Addressing this shared vulnerability might address both types of symptoms. Second, our findings suggest that prevention efforts may want to include treatment of maladaptive perfectionism. Perhaps targeting perfectionism might prevent the development of both social anxiety and eating disorder symptoms. There is research showing that perfectionism interventions can decrease symptoms of both social anxiety and disordered eating (Handley, Egan, Kane, & Rees, 2015). Our findings suggest that researchers might want to test these types of interventions before such symptoms develop.
Our data also have several crucial implications both for delineation of comorbidity in general and specifically for comorbidity between SAD and eating disorders. There has recently been a greater focus on discovering shared vulnerabilities between multiple disorders because it is thought that mental disorders represent clusters of illness with overlapping genetic and non-genetic risk factors (e.g., Fyer & Brown, 2009) . In our data we found support for the idea that there are both specific and shared underlying vulnerabilities and that these vulnerabilities may be more important for understanding comorbidity rather than categorical symptom sets. Additionally, several of the vulnerability factors predicted each other over time (e.g., maladaptive perfectionism predicted social appearance anxiety and fear of negative evaluation). Researchers attempting to evaluate potential causal relationships should attempt to measure shared vulnerabilities at as many time points as possible to clearly delineate how these factors lead to each other, as well as to symptoms of disorders.
Specifically regarding social anxiety and eating disorder comorbidity, our data represent a step forward in our understanding of how these disorders impact each other across time. We did not find that social anxiety and eating disorder symptoms per se prospectively predicted each other. Instead, it seems clear that social appearance anxiety, fear of negative evaluation, and maladaptive perfectionism (which can be understood as potential vulnerabilities for both disorders) each play an important role in the prediction of symptoms or other vulnerabilities of these disorders. These relationships may be part of a complex network of psychopathology, in which each factor contributes to higher vulnerability for each other and social anxiety and eating disorders over time (Krueger & Markon, 2006). Thus, to better understand causal models and improve treatment of comorbidity, researchers could intervene regarding specific vulnerability factors and test if the intervention is effective and decreases symptoms of both disorders, as well as the other risk factors. This type of experiment would also provide a more stringent test of causality than observational data alone (e.g., Pearl, 2000).
Our study had several limitations that should be considered. First, our time course was somewhat short (six-months) and we concentrated on young adult women. It would be ideal to have a longer time course, with multiple assessment points, and to start assessment of these risk factors at an earlier age. However, this study represents a crucial step forward because it moves beyond cross-sectional vulnerability models and tests multiple vulnerability factors across time in one combined model. Additionally, we chose this age group because it is a time at which both eating and social anxiety disorders often emerge, and previous researchers found that perfectionism led to eating disorder risk during young adulthood but not in adolescence (Tyrka, Waldron, Graber, & Brooks-Gunn 2002; Wojtowicz & Ranson, 2012). However, it would be ideal to start assessment at a younger age, because we might find that some of these risk factors have a different effect earlier in development. For example, we find it plausible that social appearance anxiety might not lead to social anxiety symptoms at the time point we focused on, but may do so at earlier age, given that social anxiety often develops earlier than eating disorders (Kessler et al., 2005; Woodside & Garfinkel, 1992). That is, at the time point we examined, social appearance anxiety may have already caused as much increase in social anxiety as it was going to cause; it might be necessary to assess younger participants to catch social appearance anxiety in its effect on social anxiety. Additionally, we chose to examine eating disorder symptoms unidimensionally, and it is recognized that there may be specific domains of eating disorders that there may be differences between types of eating disorder symptoms. We hope that future research will continue to explore this idea. There were also several methodological limitations, including presenting all questionnaires in the same order and having a large amount of drop out at follow up, which was handled with multiple imputation. Finally, it is recognized that there are several other potential shared vulnerability factors that we did not test (e.g., guilt; Berg et al., 2013). Every model inevitably omits variables that may explain more of the residual covariation (Cole & Maxwell, 2003). We hope that future researchers will continue to add vulnerability factors to this model to provide a more complete understanding of comorbidity between SAD and eating disorders.
In summary, we found that there are complex prospective relationships between several vulnerability factors for social anxiety and eating disorder symptoms. We did not find that social anxiety and eating disorder symptoms predict each other across time. These findings represent a step forward in our understanding of the prospective relationships between social anxiety and eating disorder comorbidity. We hope that researchers can use this information to design interventions that target these vulnerability factors, decreasing symptomatology of both disorders and reducing the associated suffering that inevitably occurs alongside these disorders.
Acknowledgments
This research was funded in part by F31-MH096433 to Cheri A. Levinson and 5T32DA007261-24 to Washington University. We would like to thank Julia Belsky, Leigh Brosof, Meg Buker, Bailey Davidson, Lucas Delort, Charlotte Gordon, Alice Kassinger, Simona Kaplan, Rachel Ludwig, Bethany McCord, Latrionna Moore, Rina Matsumoto, Emily Ness, Sarah Perry, Samuel Polivick, Elizabeth Riley, Stephanie Rowitz, Deborah Wohl, and Trish Yeh for their research assistance, and Leigh Brosof, Natasha Tonge, and Jaclyn S. Weisman for their feedback on a previous draft.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Authorship Statement. C.A.L. developed the study concept, conducted data collection, data analysis, and prepared the manuscript. T.L.R. provided input on the study, analysis, and manuscript preparation. All authors approved the final version of the manuscript.
References
- Antony MM, Purdon CL, Huta V, Swinson RP. Dimensions of perfectionism across the anxiety disorders. Behaviour Research and Therapy. 1998;36:1143–1154. doi: 10.1016/s0005-7967(98)00083-7. [DOI] [PubMed] [Google Scholar]
- Bardone-Cone AM, Wonderlich SA, Frost RO, Bulik CM, Mitchell JE, Uppala S, Simonich H. Perfectionism and eating disorders: Current status and future directions. Clinical Psychology Review. 2007;27:384–405. doi: 10.1016/j.cpr.2006.12.005. [DOI] [PubMed] [Google Scholar]
- Bastiani AM, Rao R, Weltzin T, Kaye WH. Perfectionism in anorexia nervosa. International Journal of Eating Disorders. 1995;17:147–152. doi: 10.1002/1098-108x(199503)17:2<147::aid-eat2260170207>3.0.co;2-x. [DOI] [PubMed] [Google Scholar]
- Becker CB, Deviva JC, Zayfert C. Eating disorder symptoms among female anxiety disorder patients in clinical practice: The importance of anxiety comorbidity assessment. Journal of Anxiety Disorders. 2004;18:255–274. doi: 10.1016/S0887-6185(03)00002-1. [DOI] [PubMed] [Google Scholar]
- Bentler PM. Comparative Fit Indexes in Structural Models. Psychological Bulletin. 1990;107:238–246. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- Berg KC, Crosby RD, Cao L, Peterson CB, Engel SG, Mitchell JE, Wonderlich SA. Facets of negative affect prior to and following binge-only, purge-only, and binge/purge events in women with bulimia nervosa. Journal of Abnormal Psychology. 2013;122:111–118. doi: 10.1037/a0029703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boone L, Soenens B, Braet C, Goossens L. An empirical typology of perfectionism in early-to-mid adolescents and its relation with eating disorder symptoms. Behaviour Research and Therapy. 2010;48:686–691. doi: 10.1016/j.brat.2010.03.022. [DOI] [PubMed] [Google Scholar]
- Buckner JD, Silgado J, Lewinsohn PM. Delineation of differential temporal relations between specific eating and anxiety disorders. Journal of Psychiatric Research. 2010;44:781–787. doi: 10.1016/j.jpsychires.2010.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Claes L, Hart TA, Smits D, Van Den Eynde F, Mueller A, Mitchell JE. Validation of the social appearance anxiety scale in female eating disorder patients. European Eating Disorder Review. 2012;20:406–409. doi: 10.1002/erv.1147. [DOI] [PubMed] [Google Scholar]
- Clark DM, Wells A. A cognitive model of social phobia. Social phobia: Diagnosis, assessment, and treatment. 1995;41:69–93. [Google Scholar]
- Cole DA, Maxwell SE. Testing mediational models with longitudinal data: questions and tips in the use of structural equation modeling. Journal of Abnormal Psychology. 2003;112:558–577. doi: 10.1037/0021-843X.112.4.558. [DOI] [PubMed] [Google Scholar]
- Cox BJ, Enns MW, Clara IP. The multidimensional structure of perfectionism in clinically distressed and college student samples. Psychological Assessment. 2002;14:365–373. [PubMed] [Google Scholar]
- DeBoer LB, Medina JL, Davis ML, Presnell KE, Powers MB, Smits JA. Associations between fear of negative evaluation and eating pathology during intervention and 12-month follow-up. Cognitive Therapy and Research. 2013;37:941–952. doi: 10.1007/s10608-013-9547-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dibartolo P, Li C, Frost R. How Do the Dimensions of Perfectionism Relate to Mental Health? Cognitive Therapy and Research. 2008;32:401–417. [Google Scholar]
- Dibartolo PM, Frost RO, Chang P, Lasota M, Grills AE. Shedding Light on the Relationship Between Personal Standards and Psychopathology: The Case for Contingent Self-Worth. Journal of Rational-Emotive & Cognitive-Behavior Therapy. 2004;22:237–250. [Google Scholar]
- Duemm I, Adams GR, Keating L. The addition of sociotropy to the dual pathway model of bulimia. Canadian Journal of Behavioural Science/Revue canadienne des sciences du comportement. 2003;35:281. [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of general psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Frost RO, Heimberg RG, Holt CS, Mattia JI, Neubauer AL. A comparison of two measures of perfectionism. Personality and Individual Differences. 1993;14:119–126. [Google Scholar]
- Frost RO, Marten P, Lahart C, Rosenblate R. The Dimensions of Perfectionism. Cognitive Therapy and Research. 1990;14:449–468. [Google Scholar]
- Garner DM, Olmstead MP, Polivy J. Development and Validation of a Multidimensional Eating Disorder Inventory for Anorexia-Nervosa and Bulimia. International Journal of Eating Disorders. 1983;2:15–34. [Google Scholar]
- Garner DM. EDI-2. Eating disorder inventory-2. Professional manual. 1991 [Google Scholar]
- Gilbert N, Meyer C. Social anxiety and social comparison: differential links with restrictive and bulimic attitudes among nonclinical women. Eating Behaviors. 2003;4:257–264. doi: 10.1016/S1471-0153(03)00026-6. [DOI] [PubMed] [Google Scholar]
- Gilbert N, Meyer C. Fear of negative evaluation and the development of eating psychopathology: A longitudinal study among nonclinical women. International Journal of Eating Disorders. 2005;37:307–312. doi: 10.1002/eat.20105. [DOI] [PubMed] [Google Scholar]
- Godart NT, Flament MF, Curt F, Perdereau F, Lang F, Venisse JL, Fermanian J. Anxiety disorders in subjects seeking treatment for eating disorders: a DSM-IV controlled study. Psychiatry Research. 2003;117:245–258. doi: 10.1016/s0165-1781(03)00038-6. [DOI] [PubMed] [Google Scholar]
- Godart NT, Flament MF, Lecrubier Y, Jeammet P. Anxiety disorders in anorexia nervosa and bulimia nervosa: co-morbidity and chronology of appearance. European Psychiatry. 2000;15:38–45. doi: 10.1016/s0924-9338(00)00212-1. [DOI] [PubMed] [Google Scholar]
- Gollob HF, Reichardt CS. Building time lags into causal models of cross-sectional data. Proceedings of the Social Statistics Section of the American Statistical Association. 1985;28:165–170. [Google Scholar]
- Gollob HF, Reichardt CS. Taking account of time lags in causal models. Child Development. 1987;58:80–92. [PubMed] [Google Scholar]
- Gollob HF, Reichardt CS. Interpreting and estimating indirect effects assuming time lags really matter. In: Collins LM, Horn JL, editors. Best methods for the analysis of change: Recent advances, unanswered questions, future directions. American Psychological Association; Washington, DC: 1991. pp. 243–259. [Google Scholar]
- Haikal M, Hong RY. The effects of social evaluation and looming threat on self-attentional biases and social anxiety. Journal of Anxiety Disorders. 2010;24:345–352. doi: 10.1016/j.janxdis.2010.01.007. [DOI] [PubMed] [Google Scholar]
- Hamann DM, Wonderlich-Tierney AL, Vander Wal JS. Interpersonal sensitivity predicts bulimic symptomatology cross-sectionally and longitudinally. Eating behaviors. 2009;10:125–127. doi: 10.1016/j.eatbeh.2009.01.001. [DOI] [PubMed] [Google Scholar]
- Handley AK, Egan SJ, Kane RT, Rees CS. A randomised controlled trial of group cognitive behavioural therapy for perfectionism. Behaviour Research and Therapy. 2015;68:37–47. doi: 10.1016/j.brat.2015.02.006. [DOI] [PubMed] [Google Scholar]
- Hart TA, Mora DB, Palyo SA, Fresco DM, Holle C, Heimberg RG. Development and examination of the social appearance anxiety scale. Assessment. 2008;15:48–59. doi: 10.1177/1073191107306673. [DOI] [PubMed] [Google Scholar]
- Heimberg RG, Brozovich FA, Rapee RM. A cognitive-behavioral model of social anxiety: Update and extension. In: Hofman SG, Di Bartolo PM, editors. Social Anxiety: Clinical, Developmental, and Social Perspectives. 2 Academic Pres; Waltham, MA: 2010. pp. 395–422. [Google Scholar]
- Heimberg R, Juster H, Hope D, Mattia J. Cognitive-behavioral group treatment: Description, case presentation, and empirical support. In: Stein MB, editor. Social phobia: Clinical and research perspectives. American Psychiatric Association; Washington, DC: 1995. pp. 293–321. [Google Scholar]
- Heimberg RG, Turk CL. Assessment of social phobia. In: Heimberg RG, Becker E, editors. Cognitive-behavioral group therapy for social phobia: Basic mechanisms and clinical strategies. Guilford Press; New York, NY: 2002. pp. 107–126. [Google Scholar]
- Hewitt PL, Flett GL, Turnbull-Donovan W, Mikail SF. The Multidimensional Perfectionism Scale: Reliability, validity, and psychometric properties in psychiatric samples. Psychological Assessment: A Journal of Consulting and Clinical Psychology. 1991;3:464–468. [Google Scholar]
- Hinrichsen H, Wright F, Waller G, Meyer C. Social anxiety and coping strategies in the eating disorders. Eating Behaviors. 2003;4:117–126. doi: 10.1016/S1471-0153(03)00016-3. [DOI] [PubMed] [Google Scholar]
- Holland PW. Statistics and causal inference. Journal of the American Statistical Association. 1986;81:945–960. [Google Scholar]
- Hofmann SG. Cognitive factors that maintain social anxiety disorder: A comprehensive model and its treatment implications. Cognitive behaviour therapy. 2007;36:193–209. doi: 10.1080/16506070701421313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Honaker J, King G, Blackwell M. Amelia II: A program for missing data (Version 1.2-17) 2006-2008 [Google Scholar]
- Hope DA, Heimberg RG, Klein JF. Social Anxiety and the Recall of Interpersonal Information. Journal of Cognitive Psychotherapy. 1990;4:185–195. [Google Scholar]
- Hu LT, Bentler PM. Cutoff Criteria for Fit Indexes in Covariance Structure Analysis: Conventional Criteria Versus New Alternatives. Structural Equation Modeling-a Multidisciplinary Journal. 1999;6:1–55. [Google Scholar]
- Hume D. A Treatise of Human Nature. Oxford University Press; Cambridge, England: 1978. [Google Scholar]
- Hussong AM, Cai L, Curran PJ, Flora DB, Chassin LA, Zucker RA. Disaggregating the distal, proximal, and time-varying effects of parent alcoholism on children’s internalizing symptoms. Journal of Abnormal Child Psychology. 2008;36:335–346. doi: 10.1007/s10802-007-9181-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobi C, Hayward C, De Zwaan M, Kraemer HC, Agras WS. Coming to terms with risk factors for eating disorders: Application of risk terminology and suggestions for a general taxonomy. Psychological Bulletin. 2004;130:19–65. doi: 10.1037/0033-2909.130.1.19. [DOI] [PubMed] [Google Scholar]
- Jöreskog KG. Statistical estimation of structural models in longitudinal-developmental investigations. In: Nesselroade JR, Baltes PB, editors. Longitudinal research in the study of behavior and development. Academic Press; New York: 1979. pp. 303–374. [Google Scholar]
- Kaye WH, Bulik CM, Thornton L, Barbarich N, Masters K, Price Foundation Collaborative Group Comorbidity of anxiety disorders with anorexia and bulimia nervosa. American Journal of Psychiatry. 2004;161:2215–2221. doi: 10.1176/appi.ajp.161.12.2215. [DOI] [PubMed] [Google Scholar]
- Krueger RF, Markon KE. Understanding Psychopathology Melding Behavior Genetics, Personality, and Quantitative Psychology to Develop an Empirically Based Model. Current Directions in Psychological Science. 2006;15:113–117. doi: 10.1111/j.0963-7214.2006.00418.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krueger RF, Piasecki TM. Toward a dimensional and psychometrically-informed approach to conceptualizing psychopathology. Behaviour Research and Therapy. 2002;40:485–499. doi: 10.1016/s0005-7967(02)00016-5. [DOI] [PubMed] [Google Scholar]
- Koskina A, Van Den Eynde F, Meisel S, Campbell IC, Schmidt U. Social appearance anxiety and bulimia nervosa. Eating and Weight Disorders. 2011;16:e142–145. doi: 10.1007/BF03325321. [DOI] [PubMed] [Google Scholar]
- Leary MR. A Brief Version of the Fear of Negative Evaluation Scale. Personality and Social Psychology Bulletin. 1983;9:371–375. [Google Scholar]
- Levinson CA, Rodebaugh TL. Validation of the Social Appearance Anxiety Scale: factor, convergent, and divergent validity. Assessment. 2011;18:350–356. doi: 10.1177/1073191111404808. [DOI] [PubMed] [Google Scholar]
- Levinson CA, Rodebaugh TL. Social anxiety and eating disorders: The role of negative social evaluation fears. Eating Behaviors. 2012;13:27–35. doi: 10.1016/j.eatbeh.2011.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levinson CA, Rodebaugh TL, White EK, Menatti AR, Weeks JW, Iacovino JM, Warren CS. Social appearance anxiety, perfectionism, and fear of negative evaluation. Distinct or shared risk factors for social anxiety and eating disorders? Appetite. 2013;67:125–133. doi: 10.1016/j.appet.2013.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levinson CA, Rodebaugh TL. Negative social evaluative fears produce social anxiety, food intake, and body dissatisfaction: Evidence of similar mechanisms through different pathways. Clinical Psychological Science. 2015:1–14. doi: 10.1177/2167702614548891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lundh LG, Öst LG. Attentional bias, self-consciousness and perfectionism in social phobia before and after cognitive-behaviour therapy. Scandinavian Journal of Behaviour Therapy. 2001;30:4–16. [Google Scholar]
- Mattick RP, Clarke JC. Development and validation of measures of social phobia scrutiny fear and social interaction anxiety. Behaviour Research and Therapy. 1998;36:455–470. doi: 10.1016/s0005-7967(97)10031-6. [DOI] [PubMed] [Google Scholar]
- Maxwell SE, Cole DA. Bias in cross-sectional analyses of longitudinal mediation. Psychological Methods. 2007;12:23–44. doi: 10.1037/1082-989X.12.1.23. [DOI] [PubMed] [Google Scholar]
- Maxwell SE, Cole DA, Mitchell MA. Bias in cross-sectional analyses of longitudinal mediation: Partial and complete mediation under an autoregressive model. Multivariate Behavioral Research. 2011;46:816–841. doi: 10.1080/00273171.2011.606716. [DOI] [PubMed] [Google Scholar]
- Mineka S, Watson D, Clark LA. Comorbidity of anxiety and unipolar mood disorders. Annual Review of Psychology. 1998;4:377–412. doi: 10.1146/annurev.psych.49.1.377. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus user's guide. Seventh Muthén & Muthén; Los Angeles, CA: 1998-2014. [Google Scholar]
- Pallister E, Waller G. Anxiety in the eating disorders: understanding the overlap. Clinical Psychology Review. 2008;28:366–386. doi: 10.1016/j.cpr.2007.07.001. [DOI] [PubMed] [Google Scholar]
- Pearl J. Causality: models, reasoning and inference. Vol. 29. MIT press; Cambridge: 2000. [Google Scholar]
- Rodebaugh TL, Heimberg RG, Brown PJ, Fernandez KC, Blanco C, Schneier FR, Liebowitz MR. More reasons to be straightforward: Findings and norms for two scales relevant to social anxiety. Journal of Anxiety Disorders. 2011;25:623–630. doi: 10.1016/j.janxdis.2011.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodebaugh TL, Woods CM, Heimberg RG, Liebowitz MR, Schneier FR. The factor structure and screening utility of the social interaction anxiety scale. Psychological Assessment. 2006;18:231–237. doi: 10.1037/1040-3590.18.2.231. [DOI] [PubMed] [Google Scholar]
- Rodebaugh TL, Woods CM, Heimberg RG. The Reverse of Social Anxiety Is Not Always the Opposite: The Reverse-Scored Items of the Social Interaction Anxiety Scale Do Not Belong. Behavior Therapy. 2007;38:192–206. doi: 10.1016/j.beth.2006.08.001. [DOI] [PubMed] [Google Scholar]
- Rosser S, Issakidis C, Peters L. Perfectionism and social phobia: Relationship between the constructs and impact on cognitive behavior therapy. Cognitive Therapy and Research. 2003;27:143–151. [Google Scholar]
- Selig JP, Preacher KJ. Mediation models for longitudinal data in developmental research. Research in Human Development. 2009;6:144–164. [Google Scholar]
- Shafran R, Cooper Z, Fairburn CG. Clinical perfectionism: A cognitive–behavioural analysis. Behaviour Research and Therapy. 2002;40:773–791. doi: 10.1016/s0005-7967(01)00059-6. [DOI] [PubMed] [Google Scholar]
- Shumaker EA, Rodebaugh TL. Perfectionism and social anxiety: Rethinking the role of high standards. Journal of Behavior Therapy and Experimental Psychiatry. 2009;40:423–433. doi: 10.1016/j.jbtep.2009.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobel ME. Effect analysis and caustion in linear structural equation models. Psychometrika. 1990;55:495–515. [Google Scholar]
- Steiger JH, Lind JC. Statistically-based tests for the number of factors; Paper presented at the Annual Spring Meeting of the Psychometric Society; Iowa City, Iowa. 1980. [Google Scholar]
- Stice E. Risk and maintenance factors for eating pathology: A meta-analytic review. Psychological Bulletin. 2002;128:825–848. doi: 10.1037/0033-2909.128.5.825. [DOI] [PubMed] [Google Scholar]
- Swinbourne JM, Touyz SW. The co-morbidity of eating disorders and anxiety disorders: a review. European Eating Disorders Review. 2007;15:253–274. doi: 10.1002/erv.784. [DOI] [PubMed] [Google Scholar]
- Taylor CB, Bryson S, Luce KH, Cunning D, Doyle AC, Abascal LB, Wilfley DE. Prevention of eating disorders in at-risk college-age women. Archives of General Psychiatry. 2006;63:881–888. doi: 10.1001/archpsyc.63.8.881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tucker L, Lewis C. A reliability coefficient for maximum likelihood factor analysis. Psychometrika. 1973;38:1–10. [Google Scholar]
- Tyrka AR, Waldron I, Graber JA, Brooks-Gunn J. Prospective predictors of the onset of anorexic and bulimic syndromes. International Journal of Eating Disorders. 2002;32:282–290. doi: 10.1002/eat.10094. [DOI] [PubMed] [Google Scholar]
- Utschig AC, Presnell K, Madeley MC, Smits JA. An investigation of the relationship between fear of negative evaluation and bulimic psychopathology. Eating Behaviors. 2010;11:231–238. doi: 10.1016/j.eatbeh.2010.05.003. [DOI] [PubMed] [Google Scholar]
- Watson D, Friend R. Measurement of social-evaluative anxiety. Journal of Consulting and Clinical Psychology. 1969;33:448–457. doi: 10.1037/h0027806. [DOI] [PubMed] [Google Scholar]
- Wojtowicz AE, Von Ranson KM. Weighing in on risk factors for body dissatisfaction: A one-year prospective study of middle-adolescent girls. Body Image. 2012;9:20–30. doi: 10.1016/j.bodyim.2011.07.004. [DOI] [PubMed] [Google Scholar]
- Woodside DB, Garfinkel PE. Age of onset in eating disorders. International Journal of Eating Disorders. 1992;12:31–36. [Google Scholar]