Abstract
This review examines current research ascertaining the impact of the Deepwater Horizon oil spill on human health and ecosystems. Driven by the need to strategically focus research funding, the authors also assess the implications of those findings, and promote a transdisciplinary research agenda addressing critical gaps.
Epidemiologic studies conducted in workers and vulnerable communities in the spill’s aftermath showed that non-chemical stressors affect resilience. Ecosystem-wise salt marsh species showed variability in structural and functional changes, attributed to species-specific tolerance, oil exposure, and belowground plant organs damage.
Lacking baseline exposure assessment data hampers assessing the impact of chemical stressors. Research priorities include leveraging existing women/child dyads and worker cohorts to advance exposure characterization and counter early adverse effects in most vulnerable populations. Key policy gaps include mandated just-in-time emergency resources to ascertain immediate post-event exposures, and contemporary legislation addressing human- and ecosystem health in an integrated rather than silo fashion.
Keywords: human health, ecosystem, exposure, non-chemical stressors
Introduction
The health of the ecosystem and that of communities living in disaster-prone areas are inextricably linked. Six years since the Deepwater Horizon (DWH) oil spill, many unanswered questions in science and policy remain. The magnitude of the spill, exacerbated by the uncertainty of dealing with the unprecedented volume of oil compounds and dispersants used, naturally focused attention and funding towards ecosystem assessment and restoration. A robust portfolio of ecosystem research is ongoing, supported by public and private funding. Examples include the Gulf of Mexico Research Initiative (GOMRI) [1], the National Science Foundation (NSF) [2], and the National Academies of Sciences (NAS) Gulf Research Program (GRP) [3]. From a human health perspective, the death of oil rig workers identified occupational exposures as a critical focus of research [4]. Human health research is primarily being supported by the National Institutes of Environmental Health Sciences (NIEHS) targeting workers and communities as vulnerable populations [5, 6]. The GRP has also recently supported demonstration grants addressing human health research [3]. In addition to research, as part of the Deepwater Horizon Medical Benefits Class Action Settlement approved by the U.S. District Court in New Orleans on January 11, 2013 and made effective on February 12, 2014, $105 million was utilized for the Gulf Region Health Outreach Program (GRHOP). The program supports capacity building projects, including in environmental health, to benefit the 17 parishes and counties in Louisiana (LA), Mississippi (MS), Alabama (AL), and Florida (FL) most affected by the spill [7]. This manuscript focuses on three key aspects of research in the aftermath of the DWH oil spill: key findings resulting from ecosystem- and human health research to date, the implications of those findings, and a research agenda for the future to address critical remaining gaps.
Ecosystem effects
The Mississippi River Delta ecosystem suffered chronic wetland degradation prior to the 2010 oil spill [8]. The 2010 oil spill was unprecedented in its extensiveness, impacting shorelines from Texas to Florida [9]. The Gulf of Mexico not only supports a rich biodiversity of both national and global importance [10], but also delivers invaluable ecosystem services such as productive fisheries, storm protection, flood-risk reduction, water quality enhancement, faunal support, and carbon sequestration. Injury and death rates were documented for species of dolphins, sperm whales, manatees, sea turtles, mangroves, sea birds (pelicans), oysters, marine vertebrates, fish,- including shark, tuna, and shellfish-, and seaweed [9–13]). Species that surface for air such as dolphins, whales, and sea turtles showed elevated rates of stranding [10]. Disease rates among these species increased, among those lethal lung disease and primary bacterial pneumonia in bottlenose dolphins [10, 13]. Bottlenose dolphins from Barataria Bay had mortality rates 8% higher than, and reproductive success rates 63% lower than, reference (not oiled) areas [12, 13]. Sperm whale population density around the oil spill area also decreased [13]. Overall, wildlife species experienced acute mortality, as well as non-lethal structural and functional disruption at varying degrees [11]. Death and injury rates are considered an underestimate and thought to be 50x greater [10, 12].
The Mississippi River Delta houses 40% of US coastal wetland, provides crucial habitat to coastal species, and plays a critical role in maintaining coastal stability and preventing erosion [14]. Within this area, Barataria Bay in Louisiana was the most impacted by the 2010 Deepwater Horizon oil spill [9].
Coastal vegetation was damaged, and erosion rates accelerated following the impacts of the oil spill [14, 15]. Along some heavily oiled shorelines, accelerated erosion raises concern of potential acceleration of shoreline retreat [14]. Within 2.5 years post-spill, an estimated 4.1km2 of Louisiana’s wetland was lost, translating to an erosion rate 1.54 m/yr faster than reference (unoiled) islands. Continued ecological stress is likely to exert pressure on emergent plants for decades to come as the marshes recover [15].
The spill’s culminating effect for the seafood industry was loss of important species production. Notably, as oyster recruitment rates decreased, the 2011 harvest season was unproductive [10]. Some juvenile fish species suffered impairments to heart function and swimming ability [12, 13]. Die-off of seaweed species further drove ecological pressures leading to decreased diversity of crabs, shrimp, and lobster [12, 13].
Human health effects
Environmental contaminants of potential concern
Approximately 210 million gallons of crude oil were released as a result of the DWH oil spill and an estimated 1.8 million gallons of chemical dispersants were used in response efforts [16, 17]. Key air pollutants associated with the DWH oil spill include hydrocarbons, particulate matter (PM), or aerosol particles, ozone, carbon monoxide, sulfur oxides and nitrogen oxides sourced from crude oil, in situ burning, and flaring of natural gas [18]. Hydrocarbons of human health concern, which include polycyclic aromatic hydrocarbons (PAHs), were reported to be temporarily increased from pre-shoreline oiling levels directly following the DWH oil spill in certain affected areas, but returned to pre-oiling levels by March 2011 [19]. Emissions of hydrocarbons from the oil slick were identified as the largest source of primary air emissions while reaction byproducts in the atmosphere including ozone and secondary organic aerosols were also detected [18].
In addition to the oil-specific compounds, the dispersants used elicited community concerns because of the initial lack of information on the composition and the sheer volume used. Chemical oil dispersants used in DWH oil spill response efforts were COREXIT 9500A and COREXIT 9527A representing mixtures of surfactants and solvents containing propylene glycol, dioctyl sodium sulfosuccinate (DSS), hydro-treated light petroleum distillates, and ethoxylated alcohols [20]. Animal studies have examined effects of dispersant exposure on pulmonary and immunologic endpoints [20–22]. Acute inhalation of COREXIT EC9500A was found to induce a transient decrease in dynamic compliance 1 day after exposure, but was reversed after 7 days, and no differences in lung neutrophils and phagocyte oxidant production, or lung function were found [20]. Another study found transient chronotropic effects on cardiac function in rats 1 day post-acute exposure to COREXIT EC9500A exposure [21]. Immunologic effects were examined in the murine model following exposure to EC9500A; markers of immunosuppression were not found [22]. Although some community concerns remain, currently no epidemiologic studies have included in-depth exposure assessments of dispersants.
Human health studies
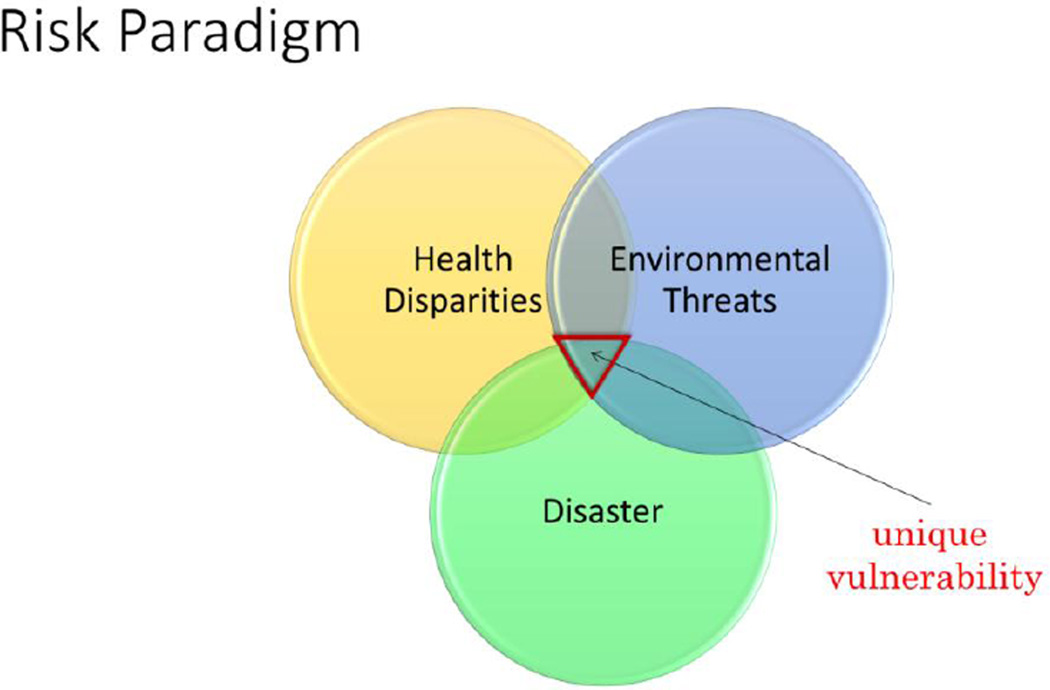
The DWH oil spill affected a uniquely vulnerable population: unlike some other large oi-spills, the unique vulnerability of communities living on the US Gulf coast is rooted in a risk paradigm of three intersecting domains with synergistic impact- a historic burden of health disparities, persistent environmental health threats, and residence in a geographic area prone to both natural and technologic disasters (Figure 1). For example, against national trends, Louisiana adults and children face a set of interdependent chemical and non-chemical (psychosocial stressors): counter to national trends, LA’s children still experience substantial, disproportionate exposures to heavy metals; e.g., blood lead levels (BLLs) remain well above national averages in Louisiana: 1.5% of children ≤ 6 years old have a BLL ≥10 µg/dL and 8% ≤ 6 years old have a BLL ≥5 µg/dL. From a psychosocial perspective, Harville et al., 2011 showed that the combined effect of Hurricanes Gustav and Katrina resulted in a higher symptom rate of depression and PTSD in 102 pregnant and reproductive age women [23]. In 2010, focusing on the increasing human health concerns, the NAS convened two expert panels to urgently identify human health research priorities and review the design and protocol of the Gulf Long-Term Follow-up Worker study [24, 25]. Indicative of the intersecting risk domains depicted in Figure 1, NAS identified five research priority areas: “psychosocial and behavioral effects with special attention to factors associated with vulnerability or resilience; exposure to oil, dispersants, and by-products of controlled burns; short and long-term seafood safety; communication and engagement methods in disaster preparedness research; and the development of a rapid response research framework” [24]. Selected progress in those areas is included below.
Figure 1.
This figure shows the three intersecting domains that impacted the population that the Deepwater Horizon (DWH) oil spill affected: a historic burden of health disparities, persistent environmental health threats, and residence in a geographic area prone to both natural and technologic disasters.
Gulf Long-Term Follow-up Study
Following the 2010 DWH oil spill, the National Institute of Environmental Health Sciences launched the Gulf Long-term Follow-up Study (GuLF STUDY). The GuLF STUDY is a prospective cohort of adults who participated in oil spill response and clean-up work, or who were trained but not hired (n=32,608). The objective of the GuLF STUDY is to determine both short- and long-term health effects of oil spill response and clean-up work following the 2010 DWH oil spill [5]. Baseline enrollment occurred between March 2011 and March 2013, and follow-up is on-going. Participant data collected included information on response and clean-up work, as well as demographic, socioeconomic, lifestyle, and health information. Anthropometric and clinical health measurements were also collected at a home visit in a subgroup of participants who lived in the 5 Gulf states. Early findings have focused on acute effects and mental health service utilization among participants [26].
DWH research consortia
Four research consortia were funded by NIEHS as academic- community partnerships to “identify potential health effects from the DWH oil spill, examine factors that contribute to individual and community resilience/ vulnerability, develop evidence promoting the health and wellbeing among Gulf coast residents, and develop capacity for improved preparedness and response activities” [6]. Table 1 summarizes the ecosystem and human health research studies and/or programs described in this article. In addition to basic research and environmental epidemiology studies, most of those research consortia feature two unique aspects: a dedicated project targeting resilience and a Community Outreach and Dissemination Core (CODC) [27]. Among the research consortia, the Gulf Resilience on Women’s Health (GROWH) (www.gulfcoastenvironmentalhealth.com) centered its research on addressing three key community questions: is the seafood safe to eat?, is the air safe to breathe?, will our babies be safe? The GROWH team used a comprehensive set of exposures and outcomes and a Community- Based Participatory Research (CBPR) approach to answer these three questions. Exposure measures in over 1,600 pregnant and reproductive age women included assessment of the spill’s impact and previous natural disasters, fish consumption including dietary Fatty Acids, PAH DNA adducts as a general biomarker or exposure. Among the interesting findings is that based on locally–derived risk assessment data, the seafood from the Gulf of Mexico is safe to eat while one species of imported seafood is contaminated at levels of potential public health concern [28]. Furthermore, as an example of a non-chemical stressor, the largest cohort of GROWH pregnant and reproductive age women reported financial loss as the most significant negative effect of the DWH oil spill [29]. Consortia studies completed soon after the spill found individuals with spill-related income loss were more likely to experience poor psychosocial symptoms [30]. Oil-spill distress was associated with negative behavioral outcomes, e.g. domestic conflict [31]. Additionally, exposure was associated with psychosocial effects and domestic conflict among partners of oil spill clean-up workers [32].
Table 1.
DWH oil spill Ecosystem and Human Health Research Studies and/or Programs
| Research Studies/Programs |
Focus | Funding Source |
Study Population |
Cohort Characteristics |
|---|---|---|---|---|
| NIEHS DWH Research Consortia | Long-term impact from the oil spill on health of Gulf residents | NIH | Trans-disciplinary Research Consortium for Gulf Resilience on Women's Health (GROWH): GROWH 1-Women living in the Gulf of Mexico region during 2010 (N=1,657); GROWH 3-Low-income pregnant women living in the Gulf of Mexico region during 2010 (N=237) | GROWH 1: Age 18–25 years (33.1%), pregnant (25.5%), Black (57.9%), residing in Jefferson parish (40.5%) GROWH 3: Age <25 years (61.6%), residing in Jefferson parish (47%), African-American (63.6%), High school education (60.1%), income less than $10,000/year (54.5%) |
| The Women And Their Children's Gulf Health Consortium (WATCH): Women and children living in Southeastern Louisiana (N=2,126) [58] | Mean age in years (45.1), White (58.3%), annual income less than $40,000/year (45.8%), worked on oil spill cleanup activities (2.2%) | |||
| Health Impact of Deepwater Horizon Spill in Eastern Gulf Coast Communities Adults in affected residents in Florida and Alabama counties (N=94) [59] | Participants with indirect exposure: Male (49%); mean age in years (48.9), Caucasian (90%) Participants with direct exposure: Male (90%), mean age in years (41.9), Caucasian (100%) |
|||
| Gulf Coast Health Alliance: Health Risks Related to the Macondo Spill (GC-HARMS):Residents from Gulfport, Biloxi, Southeast Louisiana, and Galveston, Texas (comparison community) (N=400) [60] | On-going | |||
| National Institute of Environmental Health Sciences (NIEHS) Gulf Long-term Follow-up Study (GuLF) | Short- and long-term health effects of oil spill response and cleanup work | NIH | Adults who worked on oil spill cleanup and others who were safety trained but not hired (N=32,608) [5] | Age <30 years (19.2%), Male (80.8%), White (63.4%), residing in Alabama (18.2%), Florida (21.4%) Louisiana (24.1%), Mississippi (13.0%), Texas (5.6%), Other (17.7%), annual income <$20,000/year (25.8%) |
| Gulf of Mexico Research | Impacts of petroleum | BP | Ecological and ecosystem | N/A |
| Initiative (GoMRI) | pollution and related stressors on marine and coastal ecosystems | research program. N/A | ||
| Gulf Region Health Outreach Program (GRHOP) | Improved access to physical, behavioral and mental healthcare for Gulf residents | BP as part of the DWH Medical Benefits Class Action Settlement | Healthcare benefits program. N/A | N/A |
| National Academy of Sciences (NAS) Gulf Research Program | Human health and environmental protection in the Gulf of Mexico and the U.S. outer continental shelf | BP and Transocean | No human health research has been funded to date. N/A | N/A |
(Adapted from The Gulf Research Program: A Strategic Vision. Reprinted with permission from the National Academies Press, Copyright 2014, National Academy of Sciences) [57].
The GROWH team also conducted research aimed at strengthening public health promotion and practice. Community Health Workers (CHWs), assigned to low-income women during pregnancy, were able to develop a therapeutic relationship with their participant during the study period [33]. Subsequently, this therapeutic relationship was found to be predictive of long term study adherence [33]. The developed relationship between CHW and low-income mothers allowed for the use of qualitative ethnographic methods to determine cultural beliefs and behaviors regarding post oil-spill environmental threats [34].
To date, the adverse human health effects primarily reported in the aftermath of large oil spills, such as the DWH one, are mental health impacts [35]. Cross-sectional studies on psychological impact of DWH in coastal communities have described worse anxiety and depression scores in those with spill-related income loss compared to residents with stable incomes, and adverse mental health parameters in coastal communities compared to national estimates [36, 37]. Mental health impacts have also been studied in sub-populations of interest such as fishing communities and county-specific residents [38, 39]. Studies highlight the importance of population-specific health effects following DWH exposure: Low income and low social support were found to predict depression symptoms in disaster-affected communities [39].
This collection of data aligns with the body of research on other health outcomes following oil spills, three of which produced epidemiological studies on psychosocial health outcomes. Research associated with the Exxon Valdez oil spill in Alaska clearly demonstrated reduced social support, increased social conflict, and uncertainty, leading to a range of psychiatric disorders, substance abuse, and domestic violence [36]. The Sea Empress spill in Wales produced several studies finding higher anxiety and depression scores, and perceived risk among the affected population [40, 41]. The Prestige spill in Spain showed coastal residents expressing suboptimal mental health scores [42].
Challenges in conducting environmental epidemiologic studies
Exposure assessment
Exposure assessment is a key to establishing causality between environmental exposures and health relationships. Establishing the presence of a completed exposure pathway for each chemical and group of compounds associated with the oil spill represented the greatest challenge given the chemical characteristics of the combustion products and dispersants combined with the time lag between exposure and biospecimen collection to assess early adverse pathophysiologic effects. Even if a completed exposure pathway can be confirmed, as is the case in some workers employed in the immediate aftermath of the spill, assessing exposure is further complicated by the lack of validated models to accurately reconstruct key exposure assessment components including dose and duration.
Left-censored data, where measurements are below the limit of detection (LOD), are a common challenge in environmental health research and specialized analytical approaches are needed to address this exposure assessment challenge. Personal monitoring samples collected following the DWH oil spill have been reported as having a substantial percentage of samples falling below the LOD [43]. Multiple analytical techniques have been proposed to address left censored data. The most commonly used technique is simple substitution [44]. Studies have proposed methods specifically to address high proportions of left censored data including distribution-based multiple imputation and Tobit regression, and a robust Bayesian maximum likelihood estimation [44–46]. Analogous to the mechanistic research-based exposomic studies, researchers are exploring the public health exposome, a resource-conscious research strategy to address environmental health disparities [47]. Targeting disparate secondary data sources, the team deploys complex combinatorial analytics aimed at refining exposure estimates and ultimately to enable tailored and cost-effective analytic environmental epidemiologic research. Such analytic studies would be better positioned to specifically examine how persistent health disparities influence the impact of newly introduced exposures on health outcomes of concern [48].
Analytical challenges
Environmental epidemiologic studies use transdisciplinary, complex approaches to answer seemingly simple questions: is the seafood safe to eat? Beyond the traditional aspects that distinguish human research from animal studies (e.g. voluntary participation), environmental epidemiologic studies present unique design and analytical challenges: From a design perspective, earning community trust is a prerequisite for successful recruitment and retention and consequently affects the statistical power to draw meaningful conclusions. The protracted design phase can also significantly impact the window of exposure assessment resulting in insufficient exposure characterization. Community dissatisfaction and often distrust in the results is compounded by the lag time between design and dissemination. A long standing track record of partnership, using a CBPR approach and being flexible while assuring scientific rigor are key to successfully designing and implementing environmental epidemiology studies in the context of natural and technological disasters [49, 27].
One of the greatest challenges facing environmental scientists pertain to decisions about where and when to sample for both monitoring and research. A comprehensive sampling plan is the core of unbiased research. There are four broad sampling designs used in environmental research to estimate pollutants in air, soil and water. The most frequently used sampling design is judgment sampling, a subjective selection process used mostly because the researcher has prior knowledge about the contamination. Another frequently used sampling design is haphazard sampling, which does not follow any systematic way of selecting samples and selected based on convenience of sample collections. Search sampling is a non-research sampling design used to locate sources of pollution or find areas of elevated contamination. Such sampling designs lead to biased estimates of the population parameters since this design is selected for the unique value of the environmental sample rather than making inferences about a wider population. Lastly, probability or scientific sampling designs refer to methods where selection of samples is random. The most basic probability sampling design used in environmental research is simple random sampling, where each member of the population has an equal probability of selection. If the population is heterogeneous but has non-overlapping homogenous regions, then a stratified sampling design would be appropriate. Multistage sampling design involves dividing the population into homogenous regions and then randomly selecting regions for sampling in two or more stages. Probability sampling aids in elimination of subjective bias, allows for the full representation of a group, fulfills the randomization assumption of most statistical methods, and finally allows generalizability of results [50, 51].
Discussion
Implications for ecosystems- and human health research
Overall, the focused investments in ecosystem research have resulted in a significantly enriched knowledge base informing impact, remediation, prevention and the development of predictive models. Many research projects also included fellowships, providing a pathway to create a sustainable cadre of ecosystem scientists. However, examining the role of documented short-term effects on the longer-term ecological impact of the DWH oil spill must remain an important commitment.
From a chemical stressors perspective, previous cross-sectional studies have assessed short-term impact of oil spills on human health, but there is a paucity of data on longitudinal effects following large-scale oil spills [35]. Longitudinal follow-up is required to assess any potential long-term health effects of the DWH disaster. Research conducted as a result of the DWH oil spill contributed to solidify the public health knowledge base regarding the non-chemical impacts of technological disasters such as oil spills. This comports with previous research following the Exxon Valdez spill, where the non-chemical effects were (a) powerful, (b) wide-reaching, and (c) long-lasting [36]. Conceptually, advancements were made across the NIEHS-consortia through a resilience activation framework was published to facilitate a systematic examination of factors influencing both community resilience, which will help for future projects [52]. Taken together, this line of post-disaster research demonstrates the need for a more robust local public health presence, particularly related to behavioral health outreach. Specifically, research demonstrates the need for improved public health surveillance, targeted outreach following an event, and long-term follow-up to prevent the cumulative exposures presented by multiple disasters [29].
Post-oil spill research also demonstrated the practical benefits of engaging community health workers as research partners. CHWs can be effective in building trust, accelerating recruitment [49], strengthen retention as well as study outcomes [53]. The lack of shovel-ready study protocols to assess baseline and collect critical acute exposure data in the aftermath of the oil spill was an important impetus to the creation of the Disaster Response Research Program (DR2). Sponsored by the National Institutes of Health, the program focuses on the availability of just-in-time and just-in-case data collection tools, research protocols, and expedited processes to obtain Institutional Review Board approval (https://dr2.nlm.nih.gov/)
The DWH oil spill also has wide-ranging implications regarding environmental health policy. The spill uncovered a credibility gap in the ability of the current U.S. policy network (e.g., Clean Water Act, Oil Pollution Act) to prevent ecological disasters, and protect human and ecological health, and help populations get compensation for their losses [54]. Minority communities - such as Vietnamese American communities - along the Gulf may have been disproportionately impacted by the spill [56]. Other research has demonstrated the toll levied on communities navigating the claims process [56], and due to language and cultural barriers, these insular communities may have faced greater barriers in seeking remediation [55]. Health policies are created to inherently provide protection and either incentives or fines to promote adherence. However, many policies overlook vulnerable and underserved communities, creating not only policy gaps but health risks to those already facing multiple, often cumulative heath threats. Improving healthcare capacity is important for building community resilience to future technological or natural disasters in the health disparate Gulf Coast states affected by the oil spill. GRHOP has built capacity in primary care community health clinics along the Gulf Coast and embedded mental health and environmental health expertise in these same clinics. Also included is training and deployment of CHWs in health clinics and community-based organizations to improve residents’ to access primary and specialty care and preventive services. GRHOP’s capacity building efforts complement the work of the community and outreach dissemination projects, supported by the NIEHS funded research consortia. For details about the BP Medical Benefits Class Action settlement see https://deepwaterhorizonmedicalsettlement.com/Portals/23/DWHDocuments/MedicalBenefitsSettlementAgreementwithoutexhibitsFiled20120503.pdf
A research agenda for the future
To date, while some progress has been made to address the research priorities identified by the National Academies of Science in 2010, many gaps remain [24]. For both ecosystem- and human health research continued “inter-disaster” monitoring is critical to more accurately determine baseline exposure conditions. Compared to fish and other fauna and flora, with some exception to occupational settings, obtaining immediate post disaster population-based exposure measurements is difficult and can be perceived as unethical. Although few in numbers, ongoing cohort studies support biospecimen collection which, with additional funding, will allow for establishing inter-disaster baselines and more accurate characterization of exposures and potential adverse health effects. As part of the 2016 GOMRI conference, a session dedicated to national and global research examining the interconnectedness between ecosystem- and human health concluded with a set of more refined priority research gaps. The resulting research agenda is not only informed by the findings of both ecosystem and human health research to date, but also by the persistent and lingering community concerns:1) analyze health consequences in susceptible populations; 2) embed cumulative risk assessments in longitudinal cohort studies; 3) improve air quality (indoor and outdoor) monitoring to characterize inhalation exposure; 4) conduct culturally-tailored dietary assessments targeting risks and benefits of seafood consumption; 5) leverage existing women/child dyads and worker cohorts to advance transdisciplinary research at the human /environment interface; 6) “mine” biospecimen repositories to expand biomarker portfolio; 7) invest in finger printing for exposure effects and especially susceptibility; 8) Advance CBPR by strengthening community environmental health literacy; and 9) Improve data synthesis across fields of science to facilitate research translation to community action. Together with the urgent need for robust baseline exposure characterization, the proposed agenda can serve as a “top 10” research roadmap in the aftermath of the DWH oil spill and in anticipation of future events.
Acknowledgments
This research was supported in part by the National Institutes of Health grant number 5U19ES020677. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
This research was supported in part by the Gulf Region Health Outreach Program, which is funded from the Deepwater Horizon Medical Benefits Class Action Settlement approved by the U.S. District Court in New Orleans on January 11, 2013 and made effective on February 12, 2014.
This research was supported in part by the Intramural Research Program of the NIH, National Institute of Environmental Health Sciences.
Footnotes
Compliance with Ethics Guidelines
Conflict of Interest
Maureen Lichtveld reports grants from NIH/NIEHS and GRHOP. Christopher Mundorf reports grants from National Institutes of Health. Samendra Sherchan, Kaitlyn B. Gam, Richard K. Kwok, Arti Shankar, and Lissa Soares declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Contributor Information
Maureen Lichtveld, mlichtve@tulane.edu, 1440 Canal Street, suite 2100 New Orleans, Louisiana 70112, Department of Global Environmental Health Sciences, Tulane School of Public Health and Tropical Medicine, New Orleans, LA.
Samendra Sherchan, sshercha@tulane.edu, 1440 Canal Street, suite 2100 New Orleans, Louisiana 70112, Department of Global Environmental Health Sciences, Tulane School of Public Health and Tropical Medicine, New Orleans, LA.
Kaitlyn B. Gam, kaitlyn.gam@nih.gov, P.O. Box 12233, Mail Drop A3-05, Research Triangle Park, NC 27709, Department of Epidemiology, National Institute of Environmental Health Sciences, Research Triangle Park, NC, Tulane University School of Public Health and Tropical Medicine, New Orleans, LA.
Richard K. Kwok, richard.kwok@nih.gov, P.O. Box 12233, Mail Drop A3-05, Research Triangle Park, NC 27709, Department of Epidemiology, National Institute of Environmental Health Sciences, Research Triangle Park, NC.
Christopher Mundorf, camundorf@gmail.com, P.O. Box 67, Hiram, Ohio 44234, Hiram College.
Arti Shankar, sarti@tulane.edu, 1440 Canal Street, suite 2000 New Orleans, Louisiana 70112, Department of Biostatistics and Bioinformatics, Tulane School of Public Health and Tropical Medicine, New Orleans, LA.
Lissa Soares, lsoares@tulane.edu, 1440 Canal Street, suite 2100 New Orleans, Louisiana 70112, Department of Global Environmental Health Sciences, Tulane School of Public Health and Tropical Medicine, New Orleans, LA.
References
Papers of particular interest, published recently, have been highlighted as:
•Of importance
••Of outstanding importance
- 1.Gulf of Mexico Research Initiative. [Accessed 08/21/2016];Investigating the effect of oil spills on the environment and human health. 2013 http://gulfresearchinitiative.org/
- 2.National Science Foundation. [Accessed 08/21/2016];National Science Foundation-Where Discoveries Begin. https://www.nsf.gov/
- 3.National Academies of Sciences, Engineering, and Medicine. [Accessed 08/21/2016];Gulf Research Program. 2016 http://www.nationalacademies.org/gulf/index.html.
- 4. Goldstein BD, Osofsky HJ, Lichtveld MY. The Gulf Oil Spill. New England Journal of Medicine. 2011;364(14):1334–1348. doi: 10.1056/NEJMra1007197. Provides a more comprehensive description of clinical and public health consequences and attention to the vulnerable populations on the US Gulf Coast. The manuscript also examines how the research agenda set by the IOM/NAS can advance addressing Health concerns.
- 5.Kwok RK, Engel LS, Miller AK, et al. The GuLF STUDY: a prospective study of persons involved in the Deepwater Horizon oil spill response and clean-up. Environmental Health Perspectives. doi: 10.1289/EHP715. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.National Institute of Environmental Health Sciences. [Accessed 08/22/2016];Deepwater Horizon Research Consortia. http://www.niehs.nih.gov/research/supported/centers/gulfconsortium/
- 7.Deepwater Horizon Medical Benefits Class Action Settlement Agreement. 2012 [Google Scholar]
- 8.Mendelssohn IA, Andersen GL, Baltz DM, et al. Oil impacts on coastal wetlands: implications for the Mississippi River Delta ecosystem after the Deepwater Horizon oil spill. BioScience. 2012;62(6):562–574. [Google Scholar]
- 9.Elliot D. 5 Years After BP Oil Spill, Effects Linger And Recovery Is Slow. Morning Edition. 2015 [Google Scholar]
- 10.Adams A. Summary of Information concerning the Ecological and Economic Impacts of the BP Deepwater Horizon Oil Spill Disaster. Natural Resource Defense Council. 2015 [Google Scholar]
- 11.Wilson C, editor. Ecology, Ecosystems services and Related Methodologies. Gulf of Mexico Oil Spill & Ecosystem Science Conference; Tampa, Florida. 2016 February 1–4. [Google Scholar]
- 12.Biedron SE. Time for Action: Six Years After Deepwater. Horizon Washington DC, USA: Oceana; 2016. Apr, [Google Scholar]
- 13.Beyer J, Trannum HC, Bakke T, et al. Environmental effects of the Deepwater Horizon oil spill: a review. Marine Pollution Bulletin. 2016 doi: 10.1016/j.marpolbul.2016.06.027. [DOI] [PubMed] [Google Scholar]
- 14.Lin Q, Mendelssohn IA, Graham SA, et al. Response of salt marshes to oiling from the Deepwater Horizon spill: Implications for plant growth, soil surface-erosion, and shoreline stability. Science of The Total Environment. 2016;557:369–377. doi: 10.1016/j.scitotenv.2016.03.049. [DOI] [PubMed] [Google Scholar]
- 15.Turner RE, McClenachan G, Tweel AW. Islands in the oil: Quantifying salt marsh shoreline erosion after the Deepwater Horizon oiling. Marine Pollution Bulletin. 2016;110(1):316–323. doi: 10.1016/j.marpolbul.2016.06.046. [DOI] [PubMed] [Google Scholar]
- 16.McNutt MK, Camilli R, Crone TJ, et al. Review of flow rate estimates of the Deepwater Horizon oil spill. Proceedings of the National Academy of Sciences. 2012;109(50):20260–20267. doi: 10.1073/pnas.1112139108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.US Coast Guard. On Scene Coordinator Report Deepwater Horizon Oil Spill: Submitted to the National Response Team, September 2011. Retrieved October. 2011;10:2014. [Google Scholar]
- 18.Middlebrook AM, Murphy DM, Ahmadov R, et al. Air quality implications of the Deepwater Horizon oil spill. Proceedings of the National Academy of Sciences. 2012;109(50):20280–20285. doi: 10.1073/pnas.1110052108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Allan SE, Smith BW, Anderson KA. Impact of the Deepwater Horizon oil spill on bioavailable polycyclic aromatic hydrocarbons in Gulf of Mexico coastal waters. [Accessed 08/21 2016];Environmental science & technology. 2012 46(4):2033–2039. doi: 10.1021/es202942q. https://ntp.niehs.nih.gov/results/areas/pacs/index.html. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Roberts JR, Reynolds JS, Thompson JA, et al. Pulmonary effects after acute inhalation of oil dispersant (COREXIT EC9500A) in rats. Journal of Toxicology and Environmental Health, Part A. 2011;74(21):1381–1396. doi: 10.1080/15287394.2011.606794. [DOI] [PubMed] [Google Scholar]
- 21.Roberts JR, Anderson SE, Kan H, et al. Evaluation of Pulmonary and Systemic Toxicity of Oil Dispersant (COREXIT EC9500A((R))) Following Acute Repeated Inhalation Exposure. Environmental health insights. 2014;8(Suppl 1):63–74. doi: 10.4137/EHI.S15262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Anderson SE, Franko J, Lukomska E, et al. Potential immunotoxicological health effects following exposure to COREXIT 9500A during cleanup of the Deepwater Horizon oil spill. Journal of Toxicology and Environmental Health, Part A. 2011;74(21):1419–1430. doi: 10.1080/15287394.2011.606797. [DOI] [PubMed] [Google Scholar]
- 23.Harville EW, Xiong X, Smith BW, et al. Combined effects of Hurricane Katrina and Hurricane Gustav on the mental health of mothers of small children. Journal of psychiatric and mental health nursing. 2011;18(4):288–296. doi: 10.1111/j.1365-2850.2010.01658.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. McCoy MA, Salerno JA. Assessing the effects of the Gulf of Mexico oil spill on human health. Washington, DC: The National Academy of Sciences; 2010. Assessing the effects of the home oil spill on human health: this article sets the first National human health research agenda shortly after the oil spill. Noteworthy is the prominent placement of the psychosocial and behavioral effects and the emphasis on resilience as a key area of study alongside more traditional chemical stressors.
- 25.Goldman L, Mitchell A, Patlak M. Review of the Proposal for the Gulf Long-term Follow-up Study: Highlights from the September 2010 Workshop: Workshop Report. National Academies Press; 2010. [PubMed] [Google Scholar]
- 26.Lowe SR, Kwok RK, Payne J, et al. Mental health service use by cleanup workers in the aftermath of the Deepwater Horizon oil spill. Social Science & Medicine. 2015;130:125–134. doi: 10.1016/j.socscimed.2015.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Canfield C, Angove R, Boselovic J, et al. Developing a Community-Based participatory Research Curriculum to Support Environmental Health Research Partnerships: An Initiative of the GROWH Community Outreach and Dissemination Core. International Journal Nursing and Clinical Practice. 2016;3(187) doi: 10.15344/2394-4978/2016/187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wilson MJ, Frickel S, Nguyen D, et al. A targeted health risk assessment following the Deepwater Horizon oil spill: polycyclic aromatic hydrocarbon exposure in Vietnamese-American shrimp consumers. Environmental Health Perspectives (Online) 2015;123(2):152. doi: 10.1289/ehp.1408684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jacobs MB, Harville EW. Long-term mental health among low-income, minority women following exposure to multiple natural disasters in early and late adolescence compared to adulthood. Child & youth care forum. Springer; 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Grattan LM, Roberts S, Mahan WT, Jr, et al. The early psychological impacts of the Deepwater Horizon oil spill on Florida and Alabama communities. Environmental Health Perspectives. 2011;119(6):838. doi: 10.1289/ehp.1002915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rung AL, Gaston S, Oral E, et al. Depression, mental distress and domestic conflict among Louisiana women exposed to the Deepwater Horizon Oil Spill in the WaTCH Study. Environmental health perspectives. 2016 doi: 10.1289/EHP167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rung AL, Oral E, Fontham E, et al. Mental health impact of the Deepwater Horizon Oil Spill among wives of clean-up workers. Epidemiology (Cambridge, Mass) 2015;26(4):e44. doi: 10.1097/EDE.0000000000000303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Lichtveld MY, Shankar A, Mundorf C, et al. Measuring the Developing Therapeutic Relationship Between Pregnant Women and Community Health Workers Over the Course of the Pregnancy in a Study Intervention. Journal of community health. 2016:1–10. doi: 10.1007/s10900-016-0198-2. This manuscript describes for the first time a quantitative strategy to measure the impact of the relationship between a community health worker and a pregnant woman participant in a non-clinical setting using a modified Scale to Assess the Therapeutic Relationship (STAR) assessment tool. To date, the STAR has been exclusively used in clinical settings.
- 34.Mundorf CA, Lichtveld MY. Using community-based, ethnographic methods to examine risk perceptions and actions of low-income, first-time mothers in a post-spill environment. Journal of Risk Research. 2016:1–15. doi: 10.1080/13669877.2016.1200656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Laffon B, Pasaro E, Valdiglesias V. Effects of exposure to oil spills on human health: Updated review. Journal of toxicology and environmental health Part B, Critical reviews. 2016;19(3–4):105–128. doi: 10.1080/10937404.2016.1168730. This article is the most updated comprehensive review of human health effects of oil spill exposure.
- 36.Palinkas LA. A conceptual framework for understanding the mental health impacts of oil spills: Lessons from the Exxon Valdez oil spill. Psychiatry. 2012;75(3):203–222. doi: 10.1521/psyc.2012.75.3.203. [DOI] [PubMed] [Google Scholar]
- 37.Buttke D, Vagi S, Bayleyegn T, et al. Mental health needs assessment after the Gulf Coast oil spill-Alabama and Mississippi, 2010. Prehospital and disaster medicine. 2012;27(5):401–408. doi: 10.1017/S1049023X12001100. [DOI] [PubMed] [Google Scholar]
- 38.Gill DA, Picou JS, Ritchie LA. The Exxon Valdez and BP oil spills: a comparison of initial social and psychological impacts. American Behavioral Scientist. 2011 0002764211408585. [Google Scholar]
- 39.Cherry KE, Sampson L, Nezat PF, et al. Long-term psychological outcomes in older adults after disaster: relationships to religiosity and social support. Aging & Mental Health. 2015;19(5):430–443. doi: 10.1080/13607863.2014.941325. [DOI] [PubMed] [Google Scholar]
- 40.Lyons RA, Temple JM, Evans DF, et al. Acute health effects of the Sea Empress oil spill. Journal of epidemiology and community health. 1999;53(5):306–310. doi: 10.1136/jech.53.5.306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Gallacher J, Bronstering K, Palmer S, et al. Symptomatology attributable to psychological exposure to a chemical incident: a natural experiment. Journal of epidemiology and community health. 2007;61(6):506–512. doi: 10.1136/jech.2006.046987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Carrasco JM, Pérez-Gómez B, García-Mendizábal MJ, et al. Health-related quality of life and mental health in the medium-term aftermath of the Prestige oil spill in Galiza (Spain): a cross-sectional study. BMC public health. 2007;7(1) doi: 10.1186/1471-2458-7-245. 1.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Huynh T, Ramachandran G, Banerjee S, et al. Comparison of methods for analyzing left-censored occupational exposure data. The Annals of occupational hygiene. 2014;58(9):1126–1142. doi: 10.1093/annhyg/meu067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Baccarelli A, Pfeiffer R, Consonni D, et al. Handling of dioxin measurement data in the presence of non-detectable values: overview of available methods and their application in the Seveso chloracne study. Chemosphere. 2005;60(7):898–906. doi: 10.1016/j.chemosphere.2005.01.055. [DOI] [PubMed] [Google Scholar]
- 45.Lubin JH, Colt JS, Camann D, et al. Epidemiologic evaluation of measurement data in the presence of detection limits. Environmental health perspectives. 2004:1691–1696. doi: 10.1289/ehp.7199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hewett P, Ganser GH. A comparison of several methods for analyzing censored data. Annals of Occupational Hygiene. 2007;51(7):611–632. doi: 10.1093/annhyg/mem045. [DOI] [PubMed] [Google Scholar]
- 47.Juarez PD, Matthews-Juarez P, Hood DB, et al. The public health exposome: a population-based, exposure science approach to health disparities research. International journal of environmental research and public health. 2014;11(12):12866–12895. doi: 10.3390/ijerph111212866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Langston MA, Levine RS, Kilbourne BJ, et al. Scalable combinatorial tools for health disparities research. International journal of environmental research and public health. 2014;11(10):10419–10443. doi: 10.3390/ijerph111010419. 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lichtveld M, Kennedy S, Krouse RZ, et al. From Design to Dissemination: Implementing Community-Based Participatory Research in Postdisaster Communities. American journal of public health. 2016;106(7):1235–1242. doi: 10.2105/AJPH.2016.303169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Manly BJ. Statistics for Environmental Science and Management. Florida: Chapman & Hall/CRC; 2001. [Google Scholar]
- 51.Gilbert RO. Statistical Methods for Environmental Pollution Monitoring. New York: Van Nostrand Reinhold Company; 1987. [Google Scholar]
- 52.Abramson DM, Grattan LM, Mayer B, et al. The Resilience Activation Framework: A conceptual model of how access to social resources promotes adaptation and rapid recovery in post-disaster settings. The journal of behavioral health services & research. 2015;42(1):42–57. doi: 10.1007/s11414-014-9410-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Mundorf C, Shankar A, Peng T, et al. Therapeutic Relationship and Study Adherence in a Community Health Worker-Led Intervention. Journal of Community Health. 2016:1–9. doi: 10.1007/s10900-016-0220-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Birkland TA, DeYoung SE. Emergency response, doctrinal confusion, and federalism in the Deepwater Horizon oil spill. Publius: The Journal of Federalism. 2011;41(3):471–493. [Google Scholar]
- 55.Ngo D, Gibbons JL, Scire G, et al. Mental Health Needs in Vietnamese American Communities Affected by the Gulf Oil Spill. Psychology. 2014;5(2):109. [Google Scholar]
- 56.Mayer B, Running K, Bergstrand K, et al. Sociological Forum. Wiley Online Library; 2015. Compensation and Community Corrosion: Perceived Inequalities, Social Comparisons, and Competition Following the Deepwater Horizon Oil Spill. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.The Gulf Research Program: A Strategic Vision. Washington, DC: The National Academies Press; 2014. [Google Scholar]
- 58.Peres LC, Trapido E, Rung AL, et al. The deepwater Horizon Oil spill and physical health among adult women in Southern Louisiana: The women and their children's health (WaTCH) study. Environ Health Perspect. 2016 doi: 10.1289/ehp.1510348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Grattan LM, Roberts S, Mahan WT, Jr, et al. The early psychological impacts of the Deepwater Horizon oil spill on Florida and Alabama communities. Environmental Health Perspectives. 2011;119(6):838. doi: 10.1289/ehp.1002915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Gulf Coast Health Alliance. [Accessed 09/25/2016];Project 1: Community Health Assessment of health Risks associated with the Macondo Spill: Increasing Resilience in Diverse Vulnerable Communities. https://www.utmb.edu/GCHARMS/project_1.asp.