Abstract
Objective
To determine whether eating self-efficacy and physical activity self-efficacy are predictive of dietary intake, physical activity, and weight change within a behavioral weight loss intervention, and whether dietary intake and physical activity mediate relationships between self-efficacy and weight change.
Methods
The study sample included 246 participants from a randomized trial with complete data on study variables at 12 months. Eating self-efficacy (ESE), physical activity self-efficacy (PASE), calories consumed, minutes of moderate-to-vigorous physical activity (MVPA), and weight were measured at baseline, 6, and 12 months.
Results
ESE at baseline was associated with 12-month weight change, and was mediated by average calories consumed at 6 and 12 months. Change in ESE from baseline to 6 months was associated with calories consumed at 12 months and 12-month percent weight loss (PWL), but the mediated relationship was not significant. Baseline PASE was not associated with average MVPA at 6 and 12 months or 12-month weight change, but change in PASE from baseline to 6 months was associated with 12-month weight change through its effect on MVPA at 12 months.
Conclusions
Increases in eating self-efficacy and physical activity self-efficacy during the active phase of the intervention are predictive of dietary intake, physical activity and weight loss at later points, but further research should explore the reciprocal relationship between behavior and self-efficacy in order to better inform intervention strategies that target self-efficacy and promote behavior change.
Keywords: self-efficacy, weight loss, dietary intake, physical activity
Introduction
Self-efficacy is defined as an individuals' confidence in their ability to make the behavior changes necessary to achieve their goals across a wide variety of situations (Bandura, 2004). Health behavior theories suggest that increasing self-efficacy over time will lead to behavior change. Self-efficacy has been associated with the adoption of and engagement in many health behaviors, including smoking cessation and cancer screening (Emmons et al., 2005; Gwaltney, Metrik, Kahler, & Shiffman, 2009; Sohler, Jerant, & Franks, 2015; Strecher, DeVellis, Becker, & Rosenstock, 1986). In addition, self-efficacy has been widely studied as a psychosocial correlate and predictor of changes in weight and weight-related behaviors. In fact, it has often been viewed as an essential target for change in behavioral weight loss interventions (Jeffery, 2004), which are designed specifically to incorporate strategies to enhance self-efficacy in order to promote improvements in dietary intake, physical activity, and weight loss.
Despite the assumption that targeting an increase in self-efficacy will promote behavior change and weight loss, the existing research has not fully supported that conclusion. Not only is it difficult to compare results across studies due to a wide variety of self-efficacy measures, study designs, and study populations, but the existing studies have had inconsistent and even opposing results on the role of self-efficacy in weight loss (Fontaine & Cheskin, 1997; Jeffery et al., 1984; Linde et al., 2004; Martin, Dutton, & Brantley, 2004; Teixeira et al., 2002; Wamsteker et al., 2005). Given that individuals enter behavioral interventions at various levels of self-efficacy, several studies have evaluated the effect of baseline self-efficacy on short-term weight loss. Some have found no association between baseline self-efficacy and weight change (Fontaine & Cheskin, 1997), others have found that higher baseline self-efficacy was associated with greater weight loss (Jeffery et al., 1984; Linde et al., 2004; Teixeira et al., 2002; Wamsteker et al., 2005), and one found that higher self-efficacy at baseline was associated with lower weight loss (Martin et al., 2004).
While it is interesting to study the relationship between baseline levels of self-efficacy and success in weight loss treatment, it does not explain anything about the effect of treatment-induced changes in self-efficacy. Many studies have found that increases in self-efficacy over the course of an intervention are correlated with greater reductions in weight (Annesi, 2011; Gallagher et al., 2012; Jeffery et al., 2009; Palmeira et al., 2007; Warziski, Sereika, Styn, Music, & Burke, 2008), but they have evaluated concurrent changes in self-efficacy and weight. Because most behavioral weight loss interventions target self-efficacy as an agent of change in order to lead to weight loss, it is more informative to test the hypothesis that changes in self-efficacy during an intervention affect weight loss at later time points.
Social Cognitive Theory posits that an outcome is the result of behavior change, and behavior change is a function of efficacy expectations (Bandura, 1977; Strecher et al., 1986). Thus, in the case of self-efficacy and weight loss, self-efficacy does not directly affect weight, but should influence weight through its effects on weight control behaviors. Thus, it might be more informative to use and evaluate behavior-specific measures of self-efficacy (e.g. for dietary intake and physical activity), in addition to weight change. In doing so, instead of measuring self-efficacy for weight loss, it is important to use self-efficacy measures that are specific to making changes in dietary intake or making changes in physical activity. Several studies have included such measures, but the results have been inconsistent (Becofsky, Baruth, & Wilcox, 2014; Napolitano et al., 2008; Wingo et al., 2013). Two studies evaluated physical activity self-efficacy and changes in physical activity. One study found that change in self-efficacy for physical activity was not associated with an increase in physical activity over 6 months of a physical activity intervention (Napolitano et al., 2008) while another found that change in physical activity self-efficacy was positively associated with physical activity behavior change (Becofsky et al., 2014). In a more comprehensive study that evaluated changes in eating behavior and physical activity self-efficacy, weight control behaviors, and weight, Wingo (2013) found that change in eating self-efficacy at 6 months was associated with 6-month weight change but not with change in daily caloric intake. This same study found that change in physical activity self-efficacy at 6 months was associated with weight change but not with change in weekly minutes of physical activity.
While the results of Wingo et al. (2013) suggest that the effect of self-efficacy change on weight loss did not operate through its effects on dietary intake and physical activity, the study evaluated changes in all variables over the same 6-month time period, meaning that conclusions cannot be made about the predictive effect of change in self-efficacy on weight. This is similar to much of the self-efficacy research to date, and is likely due in part to the limited time points that are available within short-term interventions. However, to evaluate the effect of changes in self-efficacy on behavior or weight change, the measurement of self-efficacy change needs to occur prior to the measurement of behavior and weight. To date, only two studies have evaluated prospective, mediating relationships between behavior-specific self-efficacy, behavior, and weight. The first study evaluated self-monitoring behaviors as mediators and found that physical activity self-efficacy at 4 weeks was related to 8-week weight change through the effect of exercise self-monitoring from weeks 5-8. Though eating self-efficacy at 4 weeks was associated with dietary self-monitoring from weeks 5 to 8, it was not predictive of 8-week weight change (Linde, Rothman, Baldwin, & Jeffery, 2006). A long-term 16-month study used structural equation modeling to evaluate similar relationships, but instead evaluated changes in dietary behaviors and physical activity as mediators. Results indicated that an increase in eating self-efficacy by 6 months was associated with greater weight loss at 16 months, and this was mediated by change in fruit and vegetable intake from baseline to 16 months. A significant mediating relationship was also found for changes in physical activity self-efficacy, physical activity, and weight (Anderson-Bill, Winett, Wojcik, & Winett, 2011).
The existing studies have provided an important foundation for studying self-efficacy and weight loss within behavioral interventions. However, what remains relatively unstudied is whether or not baseline levels and changes in self-efficacy within an intervention are predictive of changes in dietary intake, physical activity, and weight. It is important to address this research question given that most interventions are developed with strategies meant to increase self-efficacy, despite a conflicting literature on its effectiveness in promoting weight loss. The current study addresses this gap in the literature by using temporally-based mediation analyses to evaluate the prospective relationships between behavior-specific self-efficacy, dietary intake, physical activity and weight change over one year using data from an 18-month behavioral weight loss program.
Methods
Participants
Participants (N = 363) were recruited through television and newspaper advertisements to join Step-Up, an 18-month randomized controlled trial that randomly assigned sedentary overweight and obese adults to a stepped-care weight loss intervention (STEP) or to a standard behavioral weight loss intervention (Jakicic et al., 2012). Individuals were eligible if they had a BMI between 25 and 40 kg/m2, were between the ages of 18 and 55, and participated in less than the equivalent of 20 minutes per day of physical activity three times per week.
Procedures
Both the STEP and SBWI groups were asked to reduce their energy intake to 1200-1800 kcal/day and to progressively increase to 300 minutes a week of moderate-to-vigorous exercise. The SBWI group attended weekly group sessions for months 1 through 6, biweekly sessions for months 7 through 12, and monthly sessions for months 13 through 18. The sessions focused on improving knowledge about initiation of healthy eating and exercise behaviors and strategies to promote maintenance of behavior change. The STEP group attended monthly intervention sessions. They were mailed the intervention content given to the SBWI group on weeks when a group session was not held. Participants who did not meet weight loss goals at each step (5% at 3 months, 7% at 6 months, 10% at 9-18 months) were moved to a higher step that consisted of greater treatment contact, such as telephone counseling sessions, individual face-to-face sessions, and meal replacements. Strategies to increase self-efficacy were used in both treatment groups, including goal setting, review of goals, self-monitoring of dietary intake and exercise, identification of barriers, problem solving for how to overcome barriers, modeling by program staff and other participants, and personalized feedback and encouragement on progress toward dietary intake, exercise and weight loss goals. This study was approved by the Institutional Review Boards at the University of Pittsburgh and the University of North Carolina at Chapel Hill.
Measures
Participants' age, gender, race, education, and income were assessed using a demographics questionnaire at baseline. They completed in-person assessments and additional questionnaires at baseline, 6, and 12 months. Participants received $25 after completing the assessments at 6 and 12 months. Also, small incentive gifts (water bottles, pens, etc.) were given throughout the study to encourage continued participation, and study staff contacted participants frequently to remind them of assessment visits and to reach them following missed or incomplete assessments.
Eating Self-Efficacy
Eating self-efficacy was measured using the Weight Efficacy Lifestyle Questionnaire (Clark, Abrams, Niaura, Eaton, & Rossi, 1991), a 20-item measure that assesses confidence in following dietary recommendations and avoiding overeating in specific circumstances. Examples of items include “I am confident that I can control my eating on the weekends” and “I am confident that I can resist eating even when high calorie foods are available,” and are rated on a Likert scale (0 = not confident at all to 9 = very confident). The ESE score was calculated by summing all 20 items. The WEL had good internal consistency in this sample (α = .93).
Physical Activity Self-Efficacy
Physical activity self-efficacy was measured using a 5-item questionnaire designed to assess confidence in the ability to exercise when faced with specific barriers (Marcus, Selby, Niaura, & Rossi, 1992). Questions ask the participant to rate their confidence in engaging in physical activity across a variety of situations, including when the weather is bad and when they are tired. Responses are measured on a Likert scale ranging from 1 to 5 (1 = not at all confident, 5 = extremely confident). The PASE score was calculated by taking the sum of the 5 items. The scale had acceptable internal consistency in this sample (α = .78).
Dietary Intake
Dietary intake was assessed using a Food Frequency Questionnaire (Block et al., 1986), which estimates energy intake and macronutrient content. It has been validated using food records (Block, Woods, Potosky, & Clifford, 1990) and 24-hour recalls (Subar et al., 2001), and dietary changes have been associated with weight loss in previous studies (Epstein, Carr, Lin, Fletcher, & Roemmich, 2012; Jeffery et al., 1993). The outcome variable of interest in this study was total kilocalories per day (hereafter referred to as calories consumed).
Physical Activity
Physical activity was objectively measured using the SenseWear Pro Armband (BodyMedia, Inc.). The armband was worn for 7 consecutive days at each assessment period. Participants needed to have at least 4 days with 10 hours or more of wear time to have valid data included in the analyses. Weekly minutes of moderate-to-vigorous physical activity were calculated by summing the activity minutes acquired during bouts of activity at 3 or more metabolic equivalents (METs; a ratio that compares the rate of energy expenditure during an activity compared to the energy expenditure during periods of rest) that lasted for a duration of 10 minutes or longer (DHHS, 2008). The SenseWear Pro Armband has been validated against doubly labeled water (St-Onge, Mignault, Allison, & Rabasa-Lhoret, 2007) and indirect calorimetry (Fruin & Rankin, 2004), and increases in physical activity measured by the armband have been associated with weight loss in behavioral weight loss studies (Shuger et al., 2011).
Weight
Body weight was measured in the clinic to the nearest 0.1 kg using a calibrated digital scale with the participant in a hospital gown or lightweight clothing. Percent weight loss at 6 and 12 months was calculated as: ((Weight6,12– WeightBaseline)/WeightBaseline) × 100, such that those who lost weight had a negative value for PWL.
Statistical Analysis
All analyses were conducted using SAS 9.3 (SAS Institute, Cary, NC). Descriptive statistics, including means and frequencies, were calculated for demographic variables, ESE, PASE, calories consumed, MVPA, and PWL. Demographic variables were tested for their association with changes in ESE/PASE and PWL, and significant confounders were included as covariates in the regression analyses. Mixed effects models were used to evaluate change over time in ESE, PASE, calories consumed, MVPA, and PWL.
Simple mediation models were used to evaluate weight control behaviors as mediators between self-efficacy and weight change. In simple mediation, an independent variable (IV) exerts an influence on a dependent variable (DV) through its effects on an intervening variable, or mediator (Kraemer, Wilson, Fairburn, & Agras, 2002; MacKinnon, Krull, & Lockwood, 2000). The relationship between the IV and the DV is termed the total effect, which can be partitioned into the indirect effect of the IV on the DV through the mediator and its direct effect on the DV, controlling for the effect of the mediator.
The INDIRECT macro for SAS was used to examine direct relationships between self-efficacy (IV) and weight change (DV), relationships between self-efficacy (IV) and weight control behaviors (mediators; calories consumed and MVPA) and to evaluate weight control behaviors as mediators between self-efficacy and weight change (Preacher & Hayes, 2008). INDIRECT is a regression-based model that estimates total, direct, and indirect effects and uses bias-corrected bootstrapped confidence intervals to evaluate the significance of the indirect effect of the independent variable (X) on the outcome (Y) through one or more mediators (M). In this study, simple mediation models were used because self-efficacy is thought to be specific to certain weight control behaviors, such that ESE would be associated with calories consumed and PASE would be associated with MVPA. Thus, models with ESE as the independent variable included calories consumed as the mediator, and separate models with PASE as the independent variable included MVPA as the mediator. Figure 1 depicts the pathways in each of the four simple mediation models. Results of the INDIRECT macro inform (1) Path c: the total effect of the IV (ESE/PASE) on the DV (PWL), (2) Path a: the effect of the IV on the mediator (calories consumed/MVPA), (3) Path b: the effect of the mediator on the DV, controlling for the IV, and (4) Path c': the direct effect of the IV on the DV. Results also include a confidence interval for the indirect effect of the IV on the DV through the mediator. If the confidence interval excludes 0, it indicates that the mediator significantly mediates the relationship between the IV and the DV.
Figure 1.
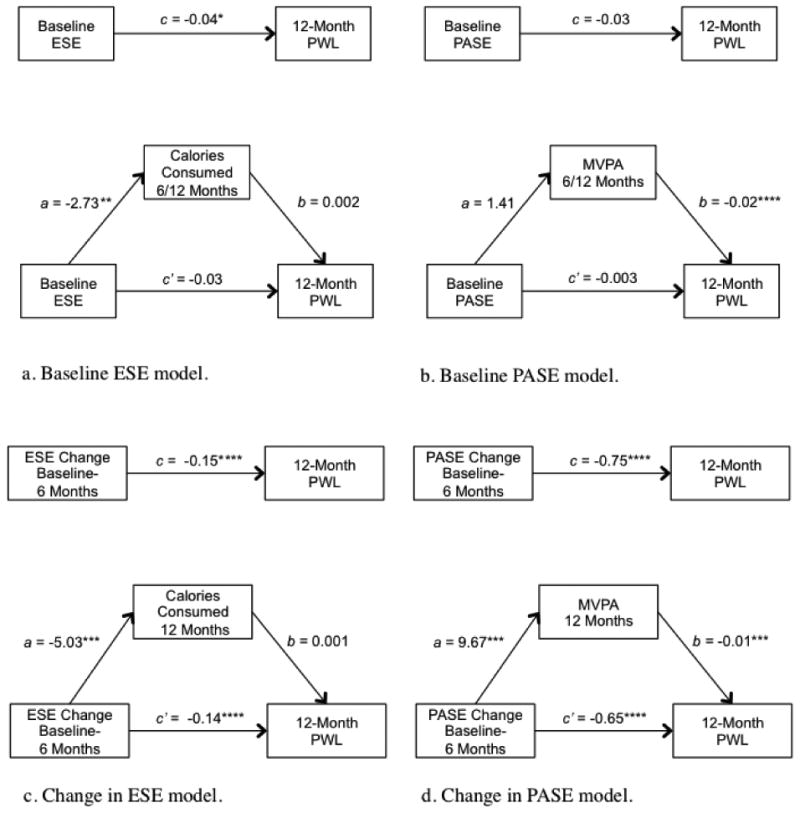
Depiction of mediation models and results. ESE = Eating self-efficacy; PASE = Physical activity self-efficacy; MVPA = moderate-to-vigorous physical activity; PWL = percent weight loss. Significance of unstandardized regression coefficients, *p < .05, **p < .01, ***p < .001, ****p <.0001.
All models were constructed in order to meet the temporal precedence assumption of mediation, such that each measure of self-efficacy occurred prior to the measures of behavior and weight change outcomes. To test the effect of baseline self-efficacy on behavior and weight loss, models included baseline ESE/PASE as the IV, an average value of calories consumed/MVPA at 6 and 12 months as the mediator, and 12-month PWL as the DV. Average values of calories consumed/MVPA at 6 and 12 months were used because any change in weight from baseline to 12 months would be the result of caloric intake and physical activity levels between baseline and 12 months, which would be captured by the 6- and 12-month assessment visits. To test the effect of change in self-efficacy from baseline to 6 months, the models included change scores for ESE/PASE as the IV, calories consumed/MVPA at 12 months as the mediator, and PWL at 12 months as the DV, and controlled for the baseline value of ESE/PASE.
Analyses collapsed across treatment groups. There were differences in changes in self-efficacy and PWL across time by gender, race, and age, so they were included as covariates in all regression analyses, in addition to treatment group and clinic site.
Results
Sample Characteristics
At 12 months, 67.7% (N = 246) of participants had returned for their follow-up weight measurements at both 6 and 12 months and had completed either the dietary intake or physical activity measurements, or both. The analysis sample for the ESE models was created using participants with complete weight and dietary data at 6 and 12 months (N=241). The analysis sample for the PASE models included participants with complete weight and physical activity data at 6 and 12 months (N=220). Descriptive statistics for each sample can be found in Table 1. On average, the participants in the completers' samples were 43.2 years of age (SD = 8.9), 80.5% female, and 76% white, with an average BMI of 32.6 (SD = 3.5). Participants with complete dietary data and those without did not differ on baseline ESE (111.0 ± 32.7 vs. 105.8 ± 31.2, p = .14) and participants with complete physical activity data and those without did not differ on baseline PASE (14.2 ± 3.8 vs. 14.1 ± 3.9, p = .80). However, participants with complete dietary data had a greater increase in ESE from baseline to 6 months (adjusted for baseline) than participants without (20.3 ± 28.5 vs. 15.0 ± 27.3, p = .05) and participants with complete physical activity data had a greater increase in PASE from baseline to 6 months than participants without (1.8 ± 4.7 vs. 0.6 ± 5.1, p = .01).
Table 1. Demographic Characteristics of Dietary Intake, Physical Activity, and Randomized Samples.
| Variable | Dietary Intake Sample Mean (SD)/% (N = 241) |
Physical Activity Sample Mean (SD)/% (N = 220) |
All Randomized Mean (SD)/% (N = 363) |
|---|---|---|---|
| Age | 43.2 (8.9) | 43.4 (9.1) | 42.2 (9.0) |
| BMI | 32.6 (3.5) | 32.5 (3.5) | 33.0 (3.6) |
| Weight (kg) | 91.8 (14.5) | 91.5 (14.4) | 92.8 (14.7) |
| Female (%) | 80.5 | 80.5 | 82.6 |
| Race | |||
| White | 76.4 | 75.9 | 68.3 |
| Black | 21.6 | 21.8 | 28.1 |
| Other | 2.0 | 2.3 | 3.6 |
| Education | |||
| High School | 6.2 | 5.9 | 6.7 |
| Vocational training or some college | 32.8 | 33.7 | 34.0 |
| College degree | 34.9 | 34.0 | 33.8 |
| Graduate or professional education | 26.1 | 26.4 | 25.5 |
Observed means and standard deviations of self-efficacy, calories consumed, MVPA, and PWL across time can be found in Table 2. In separate mixed effects models, ESE and PASE increased significantly from baseline to 12 months (time main effect p's < .0001). In addition, participants reduced their calories consumed and increased MVPA from baseline to 12 months (time main effect p's < .0001). At 6 months, participants had lost 10.9% of their body weight, which remained similar at 11.0% at 12 months.
Table 2. Means Across Time for Self-Efficacy, Weight Control Behaviors, and Percent Weight Loss.
| Baseline | 6 months | 12 months | ||||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | |
| Dietary Intake Sample (N = 241) | ||||||
| ESE | 111.0 | 32.7 | 131.3 | 29.3 | 126.1 | 34.3 |
| Average caloric intake/day | 2062.4 | 850.8 | 1496.6 | 545.5 | 1526.7 | 582.3 |
| PWL | -10.9 | 6.2 | -11.0 | 8.5 | ||
|
| ||||||
| Physical Activity Sample (N = 220) | ||||||
| PASE | 14.2 | 3.8 | 16.0 | 4.1 | 14.8 | 4.5 |
| Average MVPA min/week | 87.1 | 139.8 | 248.3 | 217.3 | 175.2 | 182.6 |
| PWL | -10.9 | 6.2 | -11.0 | 8.5 | ||
Note. All changes over time were statistically significant in mixed effect models, p < .0001.
Baseline Self-Efficacy, Weight Control Behaviors, and Percent Weight Loss
The first goal of the study was to evaluate the effect of baseline self-efficacy on dietary intake, physical activity, and weight loss. There was a significant effect of baseline ESE on PWL at 12 months, such that higher levels of ESE were associated with greater weight losses (Figure 1). Baseline ESE was also associated with average calories consumed at 6 and 12 months, such that a higher ESE score was associated with lower calories. The relationship between average calories consumed at 6 and 12 months with PWL at 12 months approached significance. Nonetheless, results indicated that average calories consumed at 6 and 12 months significantly mediated the relationship between baseline ESE and PWL (Table 3).
Table 3. Indirect Effects of Self-Efficacy on PWL.
| Model and Independent Variable | Est. | 95% CI |
|---|---|---|
| ESE | ||
| Baseline | -0.005 | (-0.013, -0.001)a |
| Change BL-6 | -0.002 | (-0.013, 0.004) |
| PASE | ||
| Baseline | -0.027 | (-0.122, 0.064) |
| Change BL-6 | -0.099 | (-0.199, -0.023)a |
Notes: Analyses controlled for treatment group, clinic, race, age, and gender. The change models also controlled for baseline values of self-efficacy.
Indirect effect is significant when the confidence interval excludes 0.
There was no effect of baseline PASE on PWL at 12 months, and no effect of baseline PASE on average MVPA at 6 and 12 months. Consistent with those results, average MVPA at 6 and 12 months did not mediate the relationship between baseline PASE and PWL at 12 months.
Change in Self-Efficacy, Weight Control Behaviors, and Percent Weight Loss
The change in self-efficacy from baseline to 6 months, controlling for baseline levels, was also evaluated for its association with dietary intake, physical activity, and weight. There was a significant relationship between change in ESE from baseline to 6 months and PWL at 12 months, such that greater increases in ESE were associated with greater PWL. Greater increases in ESE were also associated with lower calories consumed at 12 months. However, calories consumed at 12 months was not a significant mediator of the relationship between change in ESE and PWL.
In the physical activity model, greater increases in PASE from baseline to 6 months were significantly associated with greater PWL at 12 months. Increases in PASE were also associated with greater MVPA at 12 months. The relationship between change in PASE from baseline to 6 months and 12-month PWL was significantly mediated by MVPA at 12 months.
Discussion
This study showed that levels of self-efficacy before and during an intervention can have an effect on dietary intake, physical activity, and weight loss. While higher levels of eating self-efficacy at study entry were associated with lower caloric intake, and in turn increased weight loss by 12 months, baseline levels of physical activity self-efficacy were not associated with MVPA or weight loss. In addition, greater increases in eating self-efficacy were associated with reduced caloric intake and greater weight loss at 12 months, while increased physical activity self-efficacy was associated with greater weight loss through the effect of increased MVPA. This study contributes to the literature by being the first to use a temporal design and behavior-specific self-efficacy measures to test the effect of self-efficacy on weight control behaviors in an intervention, in addition to weight change. Furthermore, it fills a gap in the literature by being the first to examine the mediating effect of measured dietary intake and objectively measured physical activity on the relationship between self-efficacy and weight change.
Researchers have called into question the utility of the self-efficacy construct in weight loss research (Jeffery, 2004), but the results of this study suggest that intervention-related changes in self-efficacy can be a useful predictor of success. Increases in self-efficacy for both eating behavior and physical activity during the most active phase of the intervention (0-6 months) were associated with behaviors measured at 12 months and weight loss. These results suggest that interventionists should continue to consider ways to enhance behavior-specific self-efficacy within an intervention. It is standard to employ strategies such as goal setting, problem solving, and giving personalized feedback in order to help participants increase their self-efficacy for changes in their eating behavior or exercise. Because we know that increases in self-efficacy can lead to improved behavior change, the next step in intervention research would be to determine if the strategies currently employed by interventions are actually associated with increases in self-efficacy. For example, a recent meta-analysis showed that interventions that provided feedback on participants' progress and those that included learning through vicarious experience resulted in the greatest increases in physical activity self-efficacy (Ashford, Edmunds, & French, 2009).
While the results of this study support the utility of targeting self-efficacy in intervention studies, these results are only a small part of the self-efficacy literature as whole that has produced inconsistent conclusions due to varied study designs, measures, and study populations. The current study consisted of sedentary, primarily white and female participants. It will be important for future studies to examine whether the relationships between increases in self-efficacy and behavior and weight change are consistent or different between different study populations. In addition, it would also be of interest to evaluate changes in self-efficacy among subgroups of participants with differing levels of self-efficacy at baseline, as this study demonstrated that baseline self-efficacy can have an effect on success.
In this study, higher baseline ESE was predictive of lower calories consumed at 6 and 12 months, and was also associated with greater weight loss at 12 months. Perhaps participants' levels of ESE at study entry are related to previous attempts at making dietary changes to lose weight, and those that have been unsuccessful in the past have a more difficult time making changes during the intervention. This speaks to the need for further research to explore why participants enter studies with either low or high levels of ESE, for example, assessing their weight loss history, reasons for joining the study, and other psychosocial variables such as motivation, stress, or depression. Subsequently, research should evaluate if these factors negatively affect eating self-efficacy, and what can be done in an intervention to overcome these barriers so that they can effectively increase their self-efficacy and make dietary changes to lose weight. Baseline PASE was not associated with either MVPA at 6 and 12 months or 12-month weight loss. This finding is in contrast to results of other studies that have found that higher baseline PASE is associated with greater weight loss (Linde et al., 2006; Teixeira et al., 2002; Teixeira et al., 2004), although none of those studies examined its effect on change in physical activity. The current study was among sedentary adults who had low levels of activity at baseline, whereas the three studies cited here did not exclude participants based on activity level. Perhaps some participants in the Teixeira and Linde studies were already engaged in some level of exercise and could more accurately judge their confidence in making changes to their physical activity. A judgment of PASE based on previous experiences could be a more accurate predictor of actual changes in exercise and weight loss. While the Teixeira study did not report PASE scores at baseline, the Linde study and other studies that have used the same measure have reported baseline PASE scores similar to the baseline score in this study sample (Annesi, 2011; Lewis, Williams, Martinson, Dunsiger, & Marcus, 2013; Linde et al., 2006). Only one of those studies specifically recruited sedentary individuals, so it is unlikely that the relationships between PASE and weight loss differed due to exercise experience at baseline. In fact, results of the current study suggest that entry levels of PASE in sedentary adults do not affect participants' ability to make changes in their physical activity and lose weight over the course of 12 months.
The importance of ESE at baseline, but not PASE, suggests that entering an intervention with lower confidence in the ability to make changes to one's diet somehow limits success during the intervention, whereas lower confidence in the ability to make exercise changes does not hinder success, provided they receive comprehensive behavioral intervention support and that PASE increases over time. It is not possible to make a conclusion about the joint effects of baseline ESE and ESE change over time, but additional analyses suggest that an increase in ESE from baseline to 6 months was predictive of weight loss regardless of whether baseline ESE was low, moderate, or high. However, while an increase in ESE was predictive of reduced 12-month caloric intake for participants who started out with moderate or high levels of ESE, it was not significant among those that started at a low level of ESE (data not shown). This could suggest that there are other factors associated with low eating self-efficacy that are difficult to overcome in order to make dietary changes, such as previous failed attempts at dieting, or low motivation to make changes. Future studies should explore these relationships further to better understand the mechanisms by which baseline levels of eating self-efficacy affect behavior change. With a greater understanding of why the relationship exists, researchers may be able to incorporate additional strategies into interventions that are specifically intended to target participants with low ESE at baseline.
In addition to the direct effects found between self-efficacy, behavior, and weight loss, the results also indicated that the relationship between change in PASE and weight loss was at least partially mediated through the effect of moderate-to-vigorous physical activity levels. Thus, those who increased their PASE in the first 6 months of the intervention were successful at increasing their MVPA by 12 months, which in turn led to greater weight losses. This suggests that targeting an increase in physical activity self-efficacy during an intervention can be an effective manner by which to increase exercise and promote long-term weight loss. Interestingly, caloric intake did not mediate the relationship between change in ESE and PWL. This finding is likely due to the fact that there was no relationship between caloric intake at 12 months and 12-month weight loss. It is unclear why there was no relationship between caloric intake and weight loss, given that weight loss is due to an energy imbalance that results from changes in both dietary intake and physical activity. But it is not uncommon for caloric intake as measured by the FFQ to show no association with weight change, as it is a self-report measure that is known to underreport energy intake (Johnson, 2002). Alternatively, there could be other mechanisms by which an increase in ESE leads to weight loss, including the possibility that it also promotes changes in physical activity. This hypothesis was not tested in the current study.
Overall, the findings that eating self-efficacy and physical activity self-efficacy are predictive of behavior and weight loss have important implications for intervention research. First, the specificity of self-efficacy measures to the behaviors associated with weight loss underscore the need for interventions to measure eating self-efficacy and physical activity self-efficacy separately. Secondly, most behavioral weight loss interventions have integrated strategies that are specifically designed to target an increase in self-efficacy, such as personalized feedback intended to increase participants' confidence in making behavior changes, despite very little empirical evidence that changes in self-efficacy actually lead to changes in weight. The results of this study support the theoretical relationships between self-efficacy, weight control behaviors, and weight, and suggest that it could be beneficial for studies to specifically target eating self-efficacy and physical activity self-efficacy separately in order to promote weight loss. Interventions do not currently use measured ESE or PASE levels to determine what content an individual will receive; therefore, it might be helpful to target specific intervention content (e.g. tailored feedback on dietary or exercise changes, lesson content, etc.) to participants based on their ESE and PASE at baseline and throughout the intervention.
A strength of this study is that it is the first to use temporally-based mediation models to evaluate the effect of behavior-specific self-efficacy on the behaviors most associated with weight loss (dietary intake and physical activity) in addition to weight loss success within an intervention. However, despite the finding that increases in self-efficacy are predictive of changes in behavior and weight, a limitation of this study is that it was not able to determine the cause of the increase in ESE and PASE from baseline to 6 months. Because interventions specifically incorporate strategies intended to increase self-efficacy, it is tempting to conclude that any observed increases in self-efficacy during the intervention were due to the intervention itself. However, it is possible that successful initiation of behaviors within an intervention, and subsequently successful weight loss, leads to an increase in self-efficacy. For example, eating self-efficacy in this study increased from baseline to 6 months, but caloric intake also decreased from baseline to 6 months. Perhaps the success that participants experienced in changing their dietary intake and losing weight during the first few months of the intervention led to an increase in their confidence to make those changes. Without interim data at 3 months, it is not possible to test the reverse hypothesis in which successful behavior change leads to improvements in self-efficacy at 6 months. However, exploratory analyses revealed that behavior changes from baseline to 6 months (a decrease in calories consumed and increase in MVPA, adjusted for baseline levels) were associated with increased ESE and PASE, respectively, at 12 months. Similarly, greater percent weight loss at 6 months was associated with increased ESE and PASE at 12 months (data not shown).
The research question of whether successful behavior change or change in self-efficacy comes first has been the center of many debates surrounding the use of self-efficacy in intervention research. One hypothesis is that there could be reciprocity between self-efficacy and behavior change, such that self-efficacy can be both an effect of successful behavior change as well as a predictor. Cross-lagged panel designs could be a promising statistical method to explore this reciprocal relationship, but in the current study there were not enough time points available for self-efficacy data to use a cross-lagged panel model to answer this research question. However, even when using cross-lagged panel models, it is difficult to accurately test this hypothesis using data from intervention research that is usually only available at distant time points (e.g. baseline, 3 months, 6 months, etc.). With the advent of continuous monitoring, such as ecological momentary assessment, and the increasing use within interventions of smartphone applications, activity trackers, and smart scales that record data on a daily basis, it may soon be possible to further explore this relationship.
Because interventions are designed to increase self-efficacy, another strength of this study is that self-efficacy values increased over time, and thus it was reasonable to test the research question of whether or not the increases in self-efficacy were predictive of changes in behavior and weight. This is in contrast to the decreases in ESE and PASE observed in the study by Linde and colleagues (2006), and the decrease in PASE in the study by Anderson-Bill and colleagues (2011). In addition, of the handful of studies that have evaluated the effect of physical activity self-efficacy on behavior, none have used armbands to objectively measure physical activity, whereas the current study used an objective measure of physical activity. Conversely, the measurement of dietary intake using an FFQ is a limitation of the study, given its bias to underreporting caloric intake. But at the current time, self-report is the most feasible method of assessing dietary intake within intervention studies. The gold standard methods, such as doubly labeled water, are rarely used due to their time and cost. Also, a limitation of this study is the amount of missing data at 12 months, particularly in measures of dietary intake and physical activity. Many participants completed the in-person weight assessments at 12 months, but it was a large time commitment to complete the FFQ and a full week of armband monitoring at each assessment period, which led to greater attrition on these measures. Average weight losses were higher in this sample compared to the original RCT (Jakicic et al., 2012), meaning it was a sample that was more likely to be successful at making behavior changes and losing weight. This is a strength of the study, in that the relationships found between self-efficacy, behavior, and weight change were significant even among a more successful group of participants. However, the largely reduced sample at 18 months was one of the reasons this paper did not extend analyses to 18 months. Thus, the conclusions from this paper apply only to the initial effects of self-efficacy on behavior and weight loss, not its long-term effects on behavior and weight maintenance.
In conclusion, this study uniquely contributes to the conflicting self-efficacy and weight loss literature by using temporally-based models to more clearly define that behavior-specific measures of self-efficacy, particularly eating self-efficacy and physical activity self-efficacy, are predictive of dietary intake and physical activity, in addition to weight loss. Given the benefit of behavioral weight loss programs to overweight and obese adults, it is important to determine which psychosocial variables are reliable predictors of successful behavior and weight change. The results of this study suggest that self-efficacy remains a useful predictor of behavior change within weight loss interventions. Unfortunately, it is not possible to conclude from this study if efforts made to directly target increases in self-efficacy are critical components of interventions, or if the initiation of behavior change is enough to improve levels of self-efficacy. Nonetheless, the current study informs the field of intervention research by indicating that increases in self-efficacy, regardless of how they were induced, can be predictive of behavior and weight change.
Acknowledgments
Funding: This study was supported by grant HL084400 from the National Institutes of Health and the National Heart, Lung, and Blood Institute.
Contributor Information
Brooke T. Nezami, University of North Carolina at Chapel Hill
Wei Lang, Wake Forest University School of Medicine.
John M. Jakicic, University of Pittsburgh
Kelliann K. Davis, University of Pittsburgh
Kristen Polzien, University of North Carolina at Chapel Hill.
Amy D. Rickman, University of Pittsburgh
Karen E. Hatley, University of North Carolina at Chapel Hill
Deborah F. Tate, University of North Carolina at Chapel Hill
References
- Anderson-Bill ES, Winett RA, Wojcik JR, Winett SG. Web-based guide to health: relationship of theoretical variables to change in physical activity, nutrition and weight at 16-months. Journal of medical Internet research. 2011;13(1):e27. doi: 10.2196/jmir.1614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Annesi JJ. Behaviorally supported exercise predicts weight loss in obese adults through improvements in mood, self-efficacy, and self-regulation, rather than by caloric expenditure. The Permanente journal. 2011;15(1):23–27. doi: 10.7812/tpp/10-153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ashford S, Edmunds J, French DP. What is the best way to change self-efficacy to promote lifestyle and recreational physical activity? A systematic review with meta-analysis. Br J Health Psychol. 2009;15:265–288. doi: 10.1348/135910709x461752. 10.1348/135910709X461752. Epub 2009 Jul 7. [DOI] [PubMed] [Google Scholar]
- Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977;84(2):191–215. doi: 10.1037//0033-295x.84.2.191. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/847061. [DOI] [PubMed] [Google Scholar]
- Bandura A. Health promotion by social cognitive means. Health education & behavior : the official publication of the Society for Public Health Education. 2004;31(2):143–164. doi: 10.1177/1090198104263660. [DOI] [PubMed] [Google Scholar]
- Becofsky K, Baruth M, Wilcox S. Psychosocial mediators of two community-based physical activity programs. Annals of Behavioral Medicine : A Publication of the Society of Behavioral Medicine. 2014;48(1):125–129. doi: 10.1007/s12160-013-9578-3. [doi] [DOI] [PubMed] [Google Scholar]
- Block G, Hartman AM, Dresser CM, Carroll MD, Gannon J, Gardner L. A data-based approach to diet questionnaire design and testing. American Journal of Epidemiology. 1986;124(3):453–469. doi: 10.1093/oxfordjournals.aje.a114416. [DOI] [PubMed] [Google Scholar]
- Block G, Woods M, Potosky A, Clifford C. Validation of a self-administered diet history questionnaire using multiple diet records. Journal of Clinical Epidemiology. 1990;43:1327–1335. doi: 10.1016/0895-4356(90)90099-b. 0895-4356 (Print) [DOI] [PubMed] [Google Scholar]
- Clark MM, Abrams DB, Niaura RS, Eaton CA, Rossi JS. Self-efficacy in weight management. Journal of consulting and clinical psychology. 1991;59(5):739–744. doi: 10.1037//0022-006x.59.5.739. [DOI] [PubMed] [Google Scholar]
- DHHS U. 2008 Physical Activity Guidelines for Americans: Appendix 1. 2008 Retrieved from http://health.gov/paguidelines/guidelines/appendix1.aspx.
- Emmons KM, Puleo E, Park E, Gritz ER, Butterfield RM, Weeks JC, Li FP. Peer-delivered smoking counseling for childhood cancer survivors increases rate of cessation: the partnership for health study. J Clin Oncol. 2005;23(27):6516–6523. doi: 10.1200/JCO.2005.07.048. [DOI] [PubMed] [Google Scholar]
- Epstein LH, Carr KA, Lin H, Fletcher KD, Roemmich JN. Usual energy intake mediates the relationship between food reinforcement and BMI. Obesity (Silver Spring) 2012;20(9):1815–1819. doi: 10.1038/oby.2012.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fontaine KR, Cheskin LJ. Self-efficacy, attendance, and weight loss in obesity treatment. Addictive Behaviors. 1997;22(4):567–570. doi: 10.1016/s0306-4603(96)00068-8. [DOI] [PubMed] [Google Scholar]
- Fruin ML, Rankin JW. Validity of a multi-sensor armband in estimating rest and exercise energy expenditure. Med Sci Sports Exerc. 2004;36(6):1063–1069. doi: 10.1249/01.mss.0000128144.91337.38. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/15179178. [DOI] [PubMed] [Google Scholar]
- Gallagher R, Kirkness A, Zelestis E, Hollams D, Kneale C, Armari E, Tofler G. A randomised trial of a weight loss intervention for overweight and obese people diagnosed with coronary heart disease and/or type 2 diabetes. Annals of Behavioral Medicine : A Publication of the Society of Behavioral Medicine. 2012;44(1):119–128. doi: 10.1007/s12160-012-9369-2. [doi] [DOI] [PubMed] [Google Scholar]
- Gwaltney CJ, Metrik J, Kahler CW, Shiffman S. Self-efficacy and smoking cessation: a meta-analysis. Psychol Addict Behav. 2009;23(1):56–66. doi: 10.1037/a0013529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jakicic JM, Tate DF, Lang W, Davis KK, Polzien K, Rickman AD, Finkelstein EA. Effect of a stepped-care intervention approach on weight loss in adults: a randomized clinical trial. JAMA : the journal of the American Medical Association. 2012;307(24):2617–2626. doi: 10.1001/jama.2012.6866. 10.1001/jama.2012.6866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeffery RW. How can Health Behavior Theory be made more useful for intervention research? Int J Behav Nutr Phys Act, 1. 2004;10 doi: 10.1186/1479-5868-1-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeffery RW, Bjornson-Benson WM, Rosenthal BS, Lindquist RA, Kurth CL, Johnson SL. Correlates of weight loss and its maintenance over two years of follow-up among middle-aged men. Preventive medicine. 1984;13(2):155–168. doi: 10.1016/0091-7435(84)90048-3. [DOI] [PubMed] [Google Scholar]
- Jeffery RW, Levy RL, Langer SL, Welsh EM, Flood AP, Jaeb MA, Finch EA. A comparison of maintenance-tailored therapy (MTT) and standard behavior therapy (SBT) for the treatment of obesity. Preventive medicine. 2009;49(5):384–389. doi: 10.1016/j.ypmed.2009.08.004. [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeffery RW, Wing RR, Thorson C, Burton LR, Raether C, Harvey J, Mullen M. Strengthening behavioral interventions for weight loss: a randomized trial of food provision and monetary incentives. J Consult Clin Psychol. 1993;61(6):1038–1045. doi: 10.1037//0022-006x.61.6.1038. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/8113481. [DOI] [PubMed] [Google Scholar]
- Johnson RK. Dietary intake--how do we measure what people are really eating? Obes Res. 2002;10(Suppl 1):63s–68s. doi: 10.1038/oby.2002.192. [DOI] [PubMed] [Google Scholar]
- Kraemer HC, Wilson GT, Fairburn CG, Agras WS. Mediators and moderators of treatment effects in randomized clinical trials. Arch Gen Psychiatry. 2002;59(10):877–883. doi: 10.1001/archpsyc.59.10.877. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/12365874. [DOI] [PubMed] [Google Scholar]
- Lewis BA, Williams DM, Martinson BC, Dunsiger S, Marcus BH. Healthy for life: a randomized trial examining physical activity outcomes and psychosocial mediators. Annals of Behavioral Medicine : A Publication of the Society of Behavioral Medicine. 2013;45(2):203–212. doi: 10.1007/s12160-012-9439-5. [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linde JA, Jeffery RW, Levy RL, Sherwood NE, Utter J, Pronk NP, Boyle RG. Binge eating disorder, weight control self-efficacy, and depression in overweight men and women. International journal of obesity and related metabolic disorders : journal of the International Association for the Study of Obesity. 2004;28(3):418–425. doi: 10.1038/sj.ijo.0802570. [DOI] [PubMed] [Google Scholar]
- Linde JA, Rothman AJ, Baldwin AS, Jeffery RW. The impact of self-efficacy on behavior change and weight change among overweight participants in a weight loss trial. Health psychology : official journal of the Division of Health Psychology, American Psychological Association. 2006;25(3):282–291. doi: 10.1037/0278-6133.25.3.282. [DOI] [PubMed] [Google Scholar]
- MacKinnon DP, Krull JL, Lockwood CM. Equivalence of the mediation, confounding and suppression effect. Prev Sci. 2000;1(4):173–181. doi: 10.1023/a:1026595011371. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/11523746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marcus BH, Selby VC, Niaura RS, Rossi JS. Self-efficacy and the stages of exercise behavior change. Research quarterly for exercise and sport. 1992;63(1):60–66. doi: 10.1080/02701367.1992.10607557. [DOI] [PubMed] [Google Scholar]
- Martin PD, Dutton GR, Brantley PJ. Self-efficacy as a predictor of weight change in African-American women. Obesity research. 2004;12(4):646–651. doi: 10.1038/oby.2004.74. [DOI] [PubMed] [Google Scholar]
- Napolitano MA, Papandonatos GD, Lewis BA, Whiteley JA, Williams DM, King AC, Marcus BH. Mediators of physical activity behavior change: a multivariate approach. Health psychology : official journal of the Division of Health Psychology, American Psychological Association. 2008;27(4):409–418. doi: 10.1037/0278-6133.27.4.409. [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palmeira AL, Teixeira PJ, Branco TL, Martins SS, Minderico CS, Barata JT, Sardinha LB. Predicting short-term weight loss using four leading health behavior change theories. The international journal of behavioral nutrition and physical activity, 4. 2007;14 doi: 10.1186/1479-5868-4-14. doi:1479-5868-4-14. [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior research methods. 2008;40(3):879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- Shuger SL, Barry VW, Sui X, McClain A, Hand GA, Wilcox S, Blair SN. Electronic feedback in a diet- and physical activity-based lifestyle intervention for weight loss: a randomized controlled trial. Int J Behav Nutr Phys Act. 2011;8:41. doi: 10.1186/1479-5868-8-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sohler NL, Jerant A, Franks P. Socio-psychological factors in the Expanded Health Belief Model and subsequent colorectal cancer screening. Patient Educ Couns. 2015;98(7):901–907. doi: 10.1016/j.pec.2015.03.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- St-Onge M, Mignault D, Allison DB, Rabasa-Lhoret R. Evaluation of a portable device to measure daily energy expenditure in free-living adults. Am J Clin Nutr. 2007;85(3):742–749. doi: 10.1093/ajcn/85.3.742. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/17344495. [DOI] [PubMed] [Google Scholar]
- Strecher VJ, DeVellis BM, Becker MH, Rosenstock IM. The role of self-efficacy in achieving health behavior change. Health education quarterly. 1986;13(1):73–92. doi: 10.1177/109019818601300108. [DOI] [PubMed] [Google Scholar]
- Subar AF, Thompson FE, Kipnis V, Midthune D, Hurwitz P, McNutt S, Rosenfeld S. Comparative validation of the Block, Willett, and National Cancer Institute food frequency questionnaires : the Eating at America's Table Study. American Journal of Epidemiology. 2001;15:1089–1099. doi: 10.1093/aje/154.12.1089. 0002-9262 (Print) [DOI] [PubMed] [Google Scholar]
- Teixeira PJ, Going SB, Houtkooper LB, Cussler EC, Martin CJ, Metcalfe LL, Lohman TG. Weight loss readiness in middle-aged women: psychosocial predictors of success for behavioral weight reduction. Journal of Behavioral Medicine. 2002;25(6):499–523. doi: 10.1023/a:1020687832448. [DOI] [PubMed] [Google Scholar]
- Teixeira PJ, Going SB, Houtkooper LB, Cussler EC, Metcalfe LL, Blew RM, Lohman TG. Pretreatment predictors of attrition and successful weight management in women. International journal of obesity and related metabolic disorders : journal of the International Association for the Study of Obesity. 2004;28(9):1124–1133. doi: 10.1038/sj.ijo.0802727. [DOI] [PubMed] [Google Scholar]
- Wamsteker EW, Geenen R, Iestra J, Larsen JK, Zelissen PM, van Staveren WA. Obesity-related beliefs predict weight loss after an 8-week low-calorie diet. Journal of the American Dietetic Association. 2005;105(3):441–444. doi: 10.1016/j.jada.2004.12.031. doi:S0002822304019911. [pii] [DOI] [PubMed] [Google Scholar]
- Warziski MT, Sereika SM, Styn MA, Music E, Burke LE. Changes in self-efficacy and dietary adherence: the impact on weight loss in the PREFER study. Journal of Behavioral Medicine. 2008;31(1):81–92. doi: 10.1007/s10865-007-9135-2. [doi] [DOI] [PubMed] [Google Scholar]
- Wingo BC, Desmond RA, Brantley P, Appel L, Svetkey L, Stevens VJ, Ard JD. Self-efficacy as a Predictor of Weight Change and Behavior Change in the PREMIER Trial. Journal of nutrition education and behavior. 2013;45(4):314–321. doi: 10.1016/j.jneb.2012.12.004. 10.1016/j.jneb.2012.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]


