Abstract
Purpose of Review
Since the discovery of BRAFV600E mutations in histiocytic neoplasms, diverse kinase alterations have been uncovered in BRAFV600E-wildtype histiocytoses. The purpose of this review is to outline recent molecular advances in histiocytic neoplasms and discuss their impact on the pathogenesis and treatment of these disorders.
Recent Findings
Activating kinase alterations discovered in BRAFV600E-wildtype Langerhans (LCH) and non-Langerhans cell histiocytoses (non-LCH) result in constitutive activation of the mitogen-activated protein kinase (MAPK) and/or PI3K/AKT pathways. These kinase alterations include activating mutations in ARAF, MAP2K1, NRAS, KRAS, and PIK3CA kinases in LCH and non-LCH; BRAF, ALK, and NTRK1 fusions, as well as the ETV3-NCOA2 fusion in non-LCH; and mutations in the MAP3K1 and HRAS kinases in LCH and histiocytic sarcoma, respectively. These discoveries have refined the understanding of the histiocytoses as clonal, myeloid neoplasms driven by constitutive MAPK signaling and identified molecular therapeutic targets with promising clinical responses to RAF and MEK inhibition.
Summary
Genomic analyses over the last 6 years have identified targetable kinase alterations in BRAFV600E-wildtype histiocytic neoplasms. However, despite this progress, the molecular pathogenesis and therapeutic responsiveness of non-BRAFV600E kinase alterations are still poorly defined in these disorders.
Keywords: Langerhans Cell Histiocytosis, Erdheim-Chester Disease, ARAF, MAP2K1, Kinase Fusions
Introduction
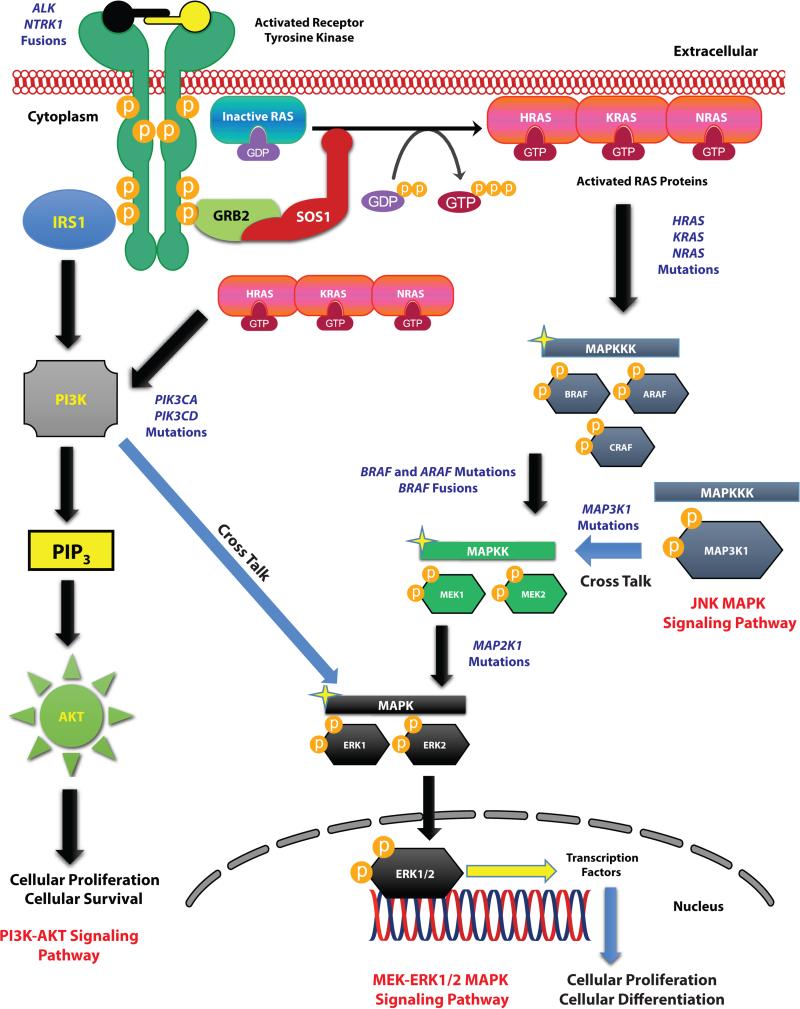
Histiocytic disorders represent a class of diseases with heterogeneous clinical courses and prognoses. They encompass disorders including Langerhans cell histiocytosis (LCH), Erdheim-Chester disease (ECD), Rosai-Dorfman disease (RDD), juvenile xanthogranuloma (JXG), histiocytic sarcoma (HS), and indeterminate cell histiocytosis (ICH). All of these conditions are believed to share a common pathologic characteristic: the accumulation and infiltration of macrophages, monocytes, dendritic cells, interdigitating reticulum cells, or Langerhans cells in the affected tissues. The pathophysiology of these diseases has long been obscure, and it was previously unclear as to whether or not they represented autoimmune or clonal, neoplastic disorders [(1), (2)]. However, starting 6 years ago, a series of recurrent activating mutations involving the MAPK and PI3K-AKT pathways (Figure 1) have been discovered in a large proportion of patients affected by this disorder. Here we review the molecular features of these disorders and the implications of these findings for therapy.
Figure 1. Overview of the MEK-ERK signaling cascade of the MAPK pathway and the PI3K-AKT pathway.
Diagram of activation of the RAS proteins (HRAS, KRAS, NRAS), the MEK-ERK signaling cascade, and the PI3K-AKT signaling pathways with annotation of the signaling proteins affected by mutations in histiocytic neoplasms is shown. Key highlights of cross talk involving members of the JNK MAP Kinase signaling cascade and the PI3K-AKT signaling pathway with the MEK-ERK signaling cascade are also shown.
Current Clinical and Histological Categorization of Histiocytoses with Insights into the Cell-of-Origin
Currently, histiocytic neoplasms are divided into LCH and non-LCH. LCH is the most common histiocytic neoplasm and most commonly occurs in children. LCH is found in 5 out of 1 million children, which is a similar frequency to acute myeloid leukemia and Hodgkin lymphoma in children [(3)]. In 2008, the World Health Organization (WHO) defined LCH as a “clonal neoplastic proliferation of Langerhans-type cells that express CD1a, langerin, and S100 protein, and shows Birbeck granules by ultrastructural examination” [(1)]. LCH originally derived its name due to the fact the Birbeck granule was identified in mononuclear phagocytic cells of LCH lesions. Since the Birbeck granule had only been seen in epidermal Langerhans cells previously, LCH was historically thought to arise from epidermal Langerhans cells [(3), (4)]. However, recent evidence suggests that LCH is actually derived from myeloid precursor cells bearing somatic mutations in MAPK pathway members. Expression profiling studies of the purified CD207+ dendritic cells from human LCH neoplasms demonstrate a significant transcriptional overlap with immature myeloid dendritic cell precursors while there is only minimal overlap with the expression profiles of human Langerhans cells [(5)]. Additionally, BRAF V600E mutations were identified in CD11c+ myeloid dendritic cell precursors and CD14+ monocytes in systemic LCH while BRAF V600E mutations were not present in the peripheral blood of patients with multifocal-tissue-restricted or single-lesion LCH. Furthermore, BRAF V600E mutations were identified in CD34+ hematopoietic progenitor cells in several systemic LCH patients. Moreover, enforced BRAF V600E expression in mouse Cd11c+ cells results in a phenotype resembling systemic LCH while enforced BRAF V600E expression in more differentiated, langerin+ dendritic cells in mice resembled multifocal-tissue-restricted or single-lesion LCH. These data led to the proposal of the “misguided myeloid dendritic cell model of LCH pathogenesis” where the clinical severity and distribution of the LCH lesion(s) are defined by the cellular stage of myeloid differentiation during which the somatic BRAF V600E or other activating kinase mutation arises and results in pathological ERK activation [(3)]. Further work will be needed to verify these results by attempting to understand the self-renewal potential of CD34+ cells bearing the BRAF V600E mutation in LCH patients and to clarify in which exact cell type within the CD34+ compartment the BRAF V600E mutations occur within LCH.
The non-Langerhans cell histiocytoses (non-LCH) are a heterogeneous group of disorders defined by the accumulation of histiocytes believed to be of monocytic/macrophage origin that do not meet the diagnostic criteria for LCH or hemophagocytic lymphohistiocytosis [(1), (6) ,(7)]. Non-LCH histiocytes are immunoreactive for CD68, CD163, Factor XIIIa, and CD14 but negative for CD1a and CD207 (langerin). Some non-LCH express S100 while others do not. The non-LCH consist of ECD, JXG, RDD, HS, ICH, and others [(1),(8)*,(6),(7)]. Currently, whether or not non-LCH neoplasms share a similar or different cell-of-origin than LCH is unknown and will need to be an active area of research.
Somatic Mutations of Genes in the MAP Kinase and PI3K-AKT Signaling Pathways in Histiocytoses
Despite the distinct clinical and histological characteristics of many of the histiocytoses as defined by the WHO, molecular characterization of these disorders has identified molecular alterations, which are recurrent across histological subtypes. The plethora of recurrent genetic alterations recently discovered across histiocytoses encompass somatic kinase alterations affecting members of the canonical MAPK and/or PI3K-AKT signaling pathways (Figure 1). These genetic alterations are detailed below.
BRAF
BRAF (B-Raf Proto-Oncogene) encodes the BRAF serine/threonine protein kinase that belongs to the Raf family of serine/threonine kinases. The RAF family includes the ARAF, BRAF, and CRAF kinases, which transduce mitogenic signals from the cell membrane to the nucleus and regulate the MEK-ERK signaling cascade of the MAPK pathway. BRAF mutations were first described in histiocytic neoplasms in 2010 when recurrent BRAFV600E mutations were discovered in 57% of LCH [(9), (10)] (Figure 2A). This was followed by the discovery of BRAFV600E mutations in 54% of ECD patients [(11)], 62.5% of HS [(12)], and in a proportion of patients deemed to have ICH [(13)]. These findings provided strong evidence that these disorders are clonal neoplastic conditions driven by constitutive MAPK signaling [(11)].
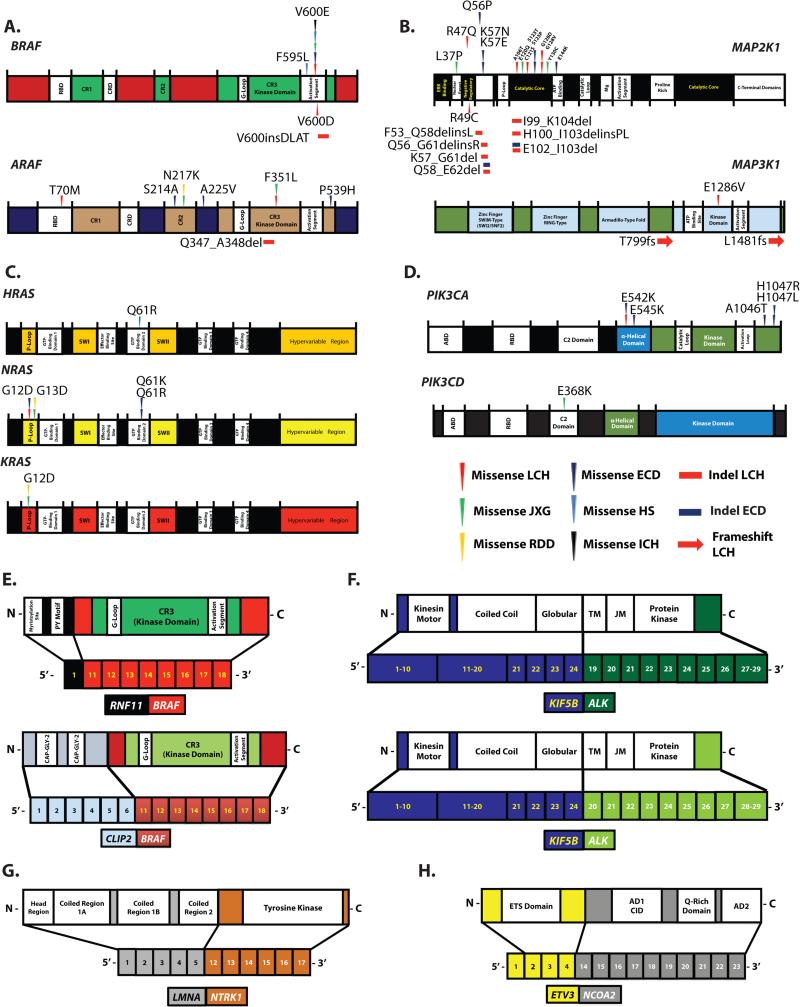
Figure 2. Summary of kinase alterations documented in histiocytic neoplasms.
Somatic mutations described in (A) BRAF and ARAF, (B) MAP2K1 and MAP3K1, (C) H/N/KRAS, and (D) PIK3CA and PIK3CD, as well as fusions in (E) BRAF, (F) ALK, (G) NTRK1 and (H) ETV3-NCOA2.
In contrast to recurrent BRAFV600E mutations, other mutations in BRAF have been found only rarely in histiocytoses. These include BRAFV600D in LCH [(10),(14)], BRAF F595L in HS [(15)], and BRAF V600insDLAT in LCH [(16)] (Figure 2A; Supplementary Table 1).
ARAF
The knowledge that BRAFV600E-wildtype histiocytoses consistently showed overexpression of phospho-MEK and phospho-ERK in pathological histiocytes [(9), (18)*, (19)], resulted in a search for other mutations, which might result in MAPK activation in BRAFV600-wildtype histiocytoses. Surprisingly, this led to the discovery of rare, activating ARAF mutations in LCH in 2014 (Figure 2A; Supplementary Table 1) [(10),(17)*, (19)]. ARAF (A-Raf Proto-Oncogene) is a serine/threonine kinase like BRAF but differs from BRAF in its potential to become activated by RAS and stimulate MEK due to biochemical differences in the N-terminus of the protein [(26)]. ARAF mutations were also found to be recurrent in non-LCH and are present in 21% of ECD [(8)*] and 12.5% of RDD patients [(8)*]. Although BRAFV600E mutations have not been identified in JXG, 18% of JXG cases have been found to have an ARAF mutation. However, these activating ARAF mutations were found to co-occur with activating NRAS mutations in those cases [(8)*]. Further work will be needed to understand the functional contribution of ARAF mutations to MAPK signaling given their frequent co-occurrence with other activating mutations such as BRAF and RAS mutations (Supplementary Figure 1).
MAP2K1
Shortly after the discovery of rare ARAF mutations in histiocytoses, several groups discovered MAP2K1 mutations in BRAFV600E-wildtype LCH [(18)*,(19),(10),(20),(8)*]. MAP2K1 (Mitogen-Activated Protein Kinase Kinase 1) encodes the MEK1 kinase, which activate Extracellular Signal-Regulated Kinases 1 and 2 (ERK1/2) through phosphorylation of threonine and tyrosine residues in ERK1/2. Across 4 studies, MAP2K1 mutations appear to be recurrent in LCH and are present in 10-40% of LCH patients [(18)*,(19), (20) (8)*]. MAP2K1 mutations are also present in non-LCH and occur in 14% of ECD and 27% of BRAFV600E-wildtype JXG cases [(8)*]. Based on the above studies, it appears that MAP2K1 mutations in histiocytoses cluster in the N-terminal negative regulatory domain encoded by exon 2 and the N-terminal catalytic core of the kinase domain encoded by exon 3 (Figure 2B; Supplementary Table 1) [(18)*,(19),(10),(20),(8)*]. Some of these MAP2K1 mutations have been biochemically characterized as activating; however, several need to be evaluated functionally. Furthermore, these MAP2K1 mutations need to be systematically evaluated for their response to diverse MEK inhibitors.
MAP3K1
While performing whole exome sequencing (WES) on LCH neoplasms, Nelson et al. also discovered 2 somatic mutations in MAP3K1 (Mitogen-Activated Protein Kinase Kinase Kinase 1), which encodes an enzyme with both E3 ubiquitin ligase activity, as well as serine/threonine kinase activity. MAP3K1 can phosphorylate MEK1 of the ERK MAPK cascade or MAP2K4 in the JNK (c-Jun N-terminal kinase) MAPK cascade. However, the mutations identified in MAP3K1 in LCH were frameshift mutations (MAP3K1 T799fs and MAP3K1 L1481fs), with MAP3K1 L1481fs occurring in the kinase domain. These mutations are therefore presumed to result in loss-of-function (Figure 2B; Supplementary Table 1) [(10),(20)], and the role of these MAP3K1 mutations in LCH and how they might promote neoplastic growth is currently unknown [(10)].
RAS Isoforms
The RAS isoforms include NRAS (Neuroblastoma RAS Viral Oncogene Homolog), KRAS (Kirsten Rat Sarcoma Viral Oncogene Homolog), and HRAS (Harvey Rat Sarcoma Viral Oncogene Homolog), which encode small GTPases that regulate the MAPK and PI3K-AKT signaling pathways. As with other hematological malignancies, recurrent mutations in N/KRAS but not in HRAS have been found in systemic histiocytoses. This includes NRAS mutations in 3-7% of ECD [(23), (24), (8)*] and NRAS and KRAS mutations in 18% of JXG patients, respectively (Figure 2C). However, RAS mutations frequently co-exist with activating ARAF mutations in JXG (Supplementary Figure 1), as discussed above [(8)*]. Similarly, NRAS and KRAS mutations are present in 12.5% and 25% of RDD patients, respectively [(8)*]. In contrast to non-LCH, rare RAS mutations have been reported in LCH patients in the setting of concomitant juvenile myelomonocytic leukemia [(21)] and have not been reported in patients with LCH alone. The sole exception to the lack of HRAS mutations in histiocytosis has been the report of an HRAS mutation in HS (Figure 2C; Supplementary Table 1) with a concomitant BRAF F595L mutation [(15)] (Supplementary Figure 1).
PI3K Isoforms
The PI3K isoforms include PIK3CA (Phosphatidylinositol-4,5-Bisphosphate 3 Kinase, Catalytic Subunit Alpha) and PIK3CD (Phosphatidylinositol-4,5-Bisphosphate 3 Kinase, Catalytic Subunit Delta). These genes encode subunits of the PI 3-Kinases (phosphoinositide 3-kinases), which belong to a family of lipid kinases that play a role in a diverse range of cellular functions that include proliferation and survival and are part of the PI3K-AKT signaling pathway. Consistent with the potential activation of the PI3K-AKT signaling pathway downstream of RAS mutations in non-LCH, PIK3CA mutations have been described in 17% of BRAFV600E-wildtype ECD [(8)*]. These mutations cluster in the α-helical and kinase domains of PIK3CA [(8)*, (23)]. Consistent with the rarity of RAS mutations in LCH, activating mutations in PIK3CA have only been identified in 1.2% of LCH patients [(10),(22)]. In addition to PIK3CA mutations, rare PIK3CD mutations have been identified in JXG (Figure 2D) [(19)]. The expression of PI3K isoforms and the role of constitutive PI3K-AKT signaling needs to be further evaluated in the pathogenesis of the histiocytoses.
Other Mutations in Genes Influencing the MAP Kinase and PI3K-AKT Signaling Pathways
Other potentially relevant mutations identified in LCH [(19)] based on WES include non-recurrent mutations in PICK1, an adaptor protein that organizes the subcellular localization of a variety of membrane proteins, and PIK3R2, a regulatory component of PI3K. Although these proteins are not directly in the MAPK cascade, they could affect ERK activation. A non-recurrent mutation in ERBB3, a member of the epidermal growth factor receptor family of receptor tyrosine kinases, has also been reported in LCH [(19),(10)]; however, it is not clear if ERBB3 is even expressed in histiocytes.
Gene Fusions Influencing the MAP Kinase Signaling Pathway in Histiocytoses
In addition to somatic mutations, structural alterations and gene fusions represent important somatic alterations driving the pathogenesis of common cancers. However, no gene fusions had been uncovered in the histiocytic neoplasms until 2015 when 2 studies described gene fusions in BRAFV600E-wild type, non-LCH neoplasms [(8)*, (25)**]. The activating or recurrent gene fusions found in the histiocytoses to date are described below.
BRAF Fusions
In addition to BRAF mutations, fusions involving BRAF have been identified in non-LCH. These include an RNF11-BRAF fusion in JXG and a CLIP2-BRAF fusion in a patient with a non-LCH resembling HS. Both fusions were found using RNA-seq and confirmed by RT-PCR followed by Sanger sequencing and interphase FISH [(8)*]. In both cases, exons 11-18 of BRAF were involved in the fusion, leading to loss of the N-terminal regulatory, RAS-binding domain of BRAF with placement of the intact BRAF kinase domain under the aberrant regulation of another promoter (Figure 2E). It is not clear what role, if any, the N-terminal fusion partner to BRAF may play in these cases.
ALK Fusions
In addition to BRAF fusions, 2 fusions involving ALK have been described in ECD (both KIF5B-ALK). In both cases, the N-terminal coiled-coil domain of KIF5B was fused to the intact kinase domain of ALK resulting in inappropriate expression and constitutive activation of ALK (Figure 2F) [(8)*]. KIF5B (Kinesin Family Member 5B) serves as a microtubule-dependent motor involved in the normal distribution of mitochondria and lysosomes while ALK (Anaplastic Lymphoma Receptor Tyrosine Kinase) encodes a neuronal orphan receptor tyrosine kinase whose expression is normally limited to the nervous system. KIF5B-ALK fusions therefore result in inappropriate ALK expression and constitutive activation of the MAPK and PI3K/AKT pathways within histiocytes. The KIF5B-ALK fusions have similar configurations to previously described KIF5B-ALK fusions in non-small cell lung cancer (NSCLC) [(27)] and are functionally activating kinase fusions that show sensitivity to ALK inhibition in vitro [(8)*].
NTRK Fusions
Thus far, fusion of a single NTRK member (NTRK1) has been described in a case of ECD. This alteration was confirmed to lead to fusion of the N-terminal coiled-coil domain of LMNA to the intact kinase domain of NTRK1 resulting in inappropriate expression and constitutive activation of NTRK1 (Figure 2G) [(8)*]. LMNA (Lamin A/C) encodes lamins, which are components of the nuclear lamina, a fibrous layer on the inner nuclear membrane that provides a framework for the nuclear envelope. NTRK1 (Neurotrophic Tyrosine Kinase, Receptor Type 1) encodes the TrkA receptor tyrosine kinase, which is a membrane-bound receptor that phosphorylates itself and members of the MAPK pathway leading to cellular proliferation and differentiation. Similar to ALK, expression of NTRK1 is normally restricted to the nervous system, but LMNA-NTRK1 fusions result in inappropriate expression and constitutive activation of MAPK and P3K/AKT pathways within histiocytes. The LMNA-NTRK1 fusion has a similar configuration to previously described LMNA-NTRK1 fusions in spitzoid neoplasms [(28)].
ETV3-NCOA2
In addition to activating kinase fusions, recurrent ETV3-NCOA2 fusions have now been described in ICH [(25)**]. This fusion juxtaposes the N-terminal ETS domain of ETV3, a winged helix-turn-helix DNA-binding domain [(25)**, (29), (30)], to the C-terminal transcriptional activation domains AD1 (Transcriptional Activation Domain 1), CID (CBP/p300 Interaction Domain), and AD2 (Transcriptional Activation Domain 2) of NCOA2 (Figure 2H). This configuration is consistent with previously described NCOA2 fusions in cancer [(25)**, (29), (31), (32), (33), (34)]. Previous studies of NCOA2 fusions have demonstrated that the AD1 and CID domains are required for transformation of NCOA2 fusion proteins [(29), (32), (34)]. The involvement of the same NCOA2 C-terminal domains and the evidence that the AD1 and CID domains are necessary for NCOA2 fusion protein transformation supports a model where the NCOA2 C-terminal transcriptional activation domains are aberrantly targeted by the DNA-binding domain provided by an N-terminal fusion partner [(25)**, (29), (31), (32), (33), (34)]. It is not yet clear how the ETV3-NCOA2 fusion relates to the persistent MAPK activation known to be present in these ICH cases. Further functional characterization of the ETV3-NCOA2 fusion in the pathogenesis of histiocytic neoplasms is therefore needed.
Role of Molecularly Targeted Therapy in the Histiocytic Neoplasms
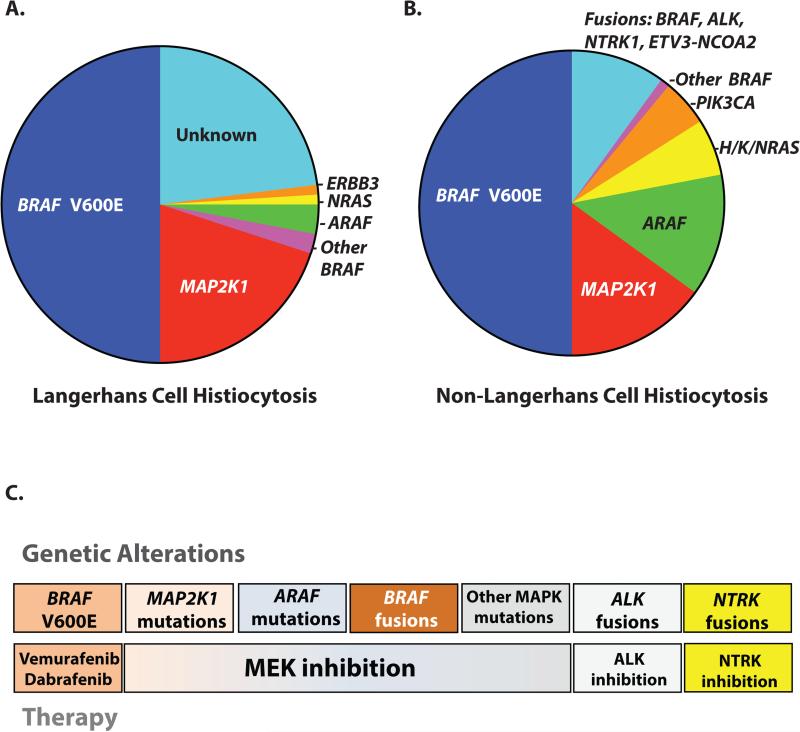
The initial discovery of the BRAFV600E mutation in ~50% of patients with LCH [(9), (8)] and ECD [(11)] and the other molecular advances summarized in this review (Figure 3; Supplementary Table 1) have led to the advent of clinical trials of targeted molecular therapeutics in these orphan hematopoietic neoplasms [(8)*] (Figure 3; Supplementary Table 2) [(35)]. The outcome of reported trials and case series of histiocytosis patients treated with molecularly targeted therapies are described below.
Figure 3. Summary of actionable genetic alterations in histiocytic neoplasms matched with a potential targeted therapy.
Pie chart illustrating the known activating kinase alterations in (A) Langerhans cell histiocytosis and (B) non-Langerhans cell histiocytoses. (C) Diagram summarizing the potential targeted therapies that have or may demonstrate clinical efficacy in histiocytic neoplasms. The RAF inhibitors vemurafenib or dabrafenib have already demonstrated efficacy in BRAF V600E mutant histiocytoses. MEK inhibition may have an important role in histiocytoses, regardless of BRAF V600E mutational status. ALK and NTRK inhibitors need to be studied for the potential role in the therapy of ALK or NTRK-fusion histiocytoses specifically.
RAF Inhibitors
Thus far, there have been 2 major studies of the RAF inhibitor vemurafenib in BRAFV600E-mutant histiocytoses. These include a case series of 8 adult patients with severe, treatment refractory, BRAFV600E-mutated ECD or ECD/LCH hybrid disease [(36)*] and a phase II clinical trial with 18 adults with BRAFV600-mutant ECD or LCH [(37)**]. In the study by Haroche et al., all patients had a significant and sustained clinical response to vemurafenib as measured by PET scanning during a 6-16 month follow up period with a mean follow up period of 10.5 months [(36)*]. In the study by Hyman et al., 14/18 patients were evaluated, and there was a 43% response rate with 86% of patients (12 of 14) showing disease regression. All patients had improvement in disease-related symptoms. There was a median treatment duration of 5.9 months (0.6-18.6 months) with no ECD or LCH patients experiencing progression while on treatment. The 12-month progression-free survival rate was 91% with a 100% overall survival for this study cohort. These data suggest that BRAF inhibition may have a clinically significant effect on the natural history of ECD and LCH [(37)**].
In contrast to the case series and clinical trial in adults, there is only a single report of a child with histiocytosis treated with vemurafenib. In this case, an 8-month-old with BRAFV600E-mutated, high-risk LCH, whose disease failed to respond to multiple rounds of prior therapy, experienced dramatic clinical efficacy to vemurafenib with a sustained response during the 10-month follow up period [(38)*]. With the success of vemurafenib treatment in clinical studies of adult ECD and LCH [(39), (40), (36)*, (37)**], the efficacy of RAF inhibitors should be investigated in clinical trials of infants and children with severe, high-risk, treatment-refractory, BRAFV600E-mutated LCH and other histiocytic neoplasms.
Given the frequency of ARAF mutations in histiocytoses, several studies have investigated therapies to target these alterations. Given a prior report of a patient with ARAF S214C-mutant non-small lung cancer who had a dramatic response to single-agent sorafenib, we treated one ARAF S214A-mutated refractory ECD patient with sorafenib with remarkable results [(8)*]. This patient experienced regression of lesions in the retina and cavernous sinuses with a >50% decrease in ARAF S214A-mutant DNA in the plasma cell-free DNA after 12 weeks of sorafenib. Sorafenib is a multi-kinase inhibitor that inhibits all 3 Raf isoforms (BRAF, CRAF, ARAF), in addition to inhibiting a host of additional kinases (including vascular endothelial growth factor receptor (VEGFR) 1, 2, and 3, c-Kit, Flt-3, RET, and platelet derived growth factor receptor beta (PDGFRβ)). The clinical activity of sorafenib is thought to be due to its capacity to inhibit multiple kinases that are part of ubiquitous signaling pathways dysregulated in neoplastic disease [(41)]. However, pre-clinical studies are needed to evaluate the responsiveness of sorafenib and other RAF inhibitors to different ARAF mutations in the histiocytic neoplasms, and clinical studies on larger series of ARAF-mutated, histiocytosis patients is warranted.
MEK Inhibitors
At present, there has been a single report of the clinical use of MEK inhibitors in MAP2K1-mutated, histiocytosis patients [(8)*]. We treated 2 non-LCH patients with MAP2K1 K57N and MAP2K1 Q56P mutations with trametinib and cobimetinib, respectively. Both patients experienced dramatic radiologic improvements, as well as clinical improvements, and both have been sustained for nearly 6 months. These encouraging results will need to be followed with pre-clinical studies to evaluate MEK inhibitor responsiveness of different MAP2K1 mutations in the histiocytic neoplasms, as well as clinical studies on cohorts of MAP2K1-mutated, histiocytosis patients.
Conclusion
Since BRAFV600E mutations were first described in LCH, there have been tremendous molecular advances in our understanding of histiocytic neoplasms. These discoveries have directly resulted in wider use of RAF inhibitors for the treatment of BRAFV600E mutant histiocytoses and indicate the importance of comprehensive molecular analysis in routine clinical practice. It will now be important to determine how relevant the mutations in these kinases are to histiocytic disorders such as RDD and HS, which have been less systematically studied to date. Moreover, it will be important to determine the clonal composition of histiocytoses using studies of purified lesional histiocytes and surrounding cells from histiocyte tissue biopsies. In addition, currently, the therapeutic relevance of activating ARAF, RAS, and MAP2K1 mutations, as well as activating fusions in BRAF, ALK, and NTRK1 in the histiocytoses remains to be systematically studied in clinical trial settings. Given the relative rarity of these conditions, the wider use of histology-independent clinical trials of molecularly targeted therapeutics (“basket trials”) will hopeful allow inclusion of histiocytosis patients.
Supplementary Material
Key Points.
- Recurrent somatic mutations in Langerhans cell histiocytosis (LCH) and non-LCH have refined our understanding of these enigmatic disorders as clonal, myeloid neoplasms driven by constitutive MAPK signaling.
- Activating kinase mutations in BRAF, ARAF, MAP2K1, N/K/HRAS, and PIK3CA have now been described in LCH and non-LCH histiocytic neoplasms due to the implementation of next-generation sequencing technologies.
- Kinase fusions involving BRAF, ALK, NTRK1, and ETV3-NCOA2 have been discovered in non-LCH histiocytic neoplasms.
- Significant clinical responses to RAF inhibitors have been documented in adult and pediatric patients with BRAFV600E-mutated LCH and non-LCH marked by a prolonged durability when compared to BRAF inhibition in more common BRAFV600E-mutated malignancies.
- MAP2K1- and ARAF-mutant histiocytosis patients have been reported to have clinical responses to MEK inhibition and sorafenib, respectively.
Acknowledgements
None
Financial Support and Sponsorship: B.H.D. is supported by the American Society of Hematology Senior Research Training Award for Fellows. E.L.D and O.A.-W. are supported by grants from Erdheim-Chester Disease Global Alliance, the Histiocytosis Association, the Society of MSKCC, the Geoffrey Beene Research Center of MSKCC, and the Translational and Integrative Medicine Research Fund of MSKCC. OAW is also supported by an NIH K08 Clinical Investigator Award (1K08CA160647-01), the Josie Robertson Investigator Program, the V Foundation, a Damon Runyon Clinical Investigator Award with support from the Evans Foundation, and a Leukemia and Lymphoma Society Clinical Scholar Award.
Footnotes
Conflict of Interest Disclosure Statement:
The authors declare no competing financial interests.
References
- 1.Swerdlow SH, Campo E, Harris NL, Jaffe ES, Pileri SA, Stein H, Thiele J, Vardiman JW. WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues. Fourth Edition WHO Press; 2008. [Google Scholar]
- 2.Diamond EL, Dagna L, Hyman DM, Cavalli G, Janku F, Estrada-Veras J, et al. Consensus guidelines for the diagnosis and clinical management of Erdheim-Chester disease. Blood. 2014 Jul 24;124(4):483–92. doi: 10.1182/blood-2014-03-561381. PubMed PMID: 24850756. Pubmed Central PMCID: PMC4110656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Berres ML, Merad M, Allen CE. Progress in understanding the pathogenesis of Langerhans cell histiocytosis: back to Histiocytosis X? British journal of haematology. 2015 Apr;169(1):3–13. doi: 10.1111/bjh.13247. PubMed PMID: 25430560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nezelof C, Basset F, Rousseau MF. Histiocytosis X histogenetic arguments for a Langerhans cell origin. Biomedicine / [publiee pour l'AAICIG] 1973 Sep;18(5):365–71. PubMed PMID: 4356601. [PubMed] [Google Scholar]
- 5.Allen CE, Li L, Peters TL, Leung HC, Yu A, Man TK, et al. Cell-specific gene expression in Langerhans cell histiocytosis lesions reveals a distinct profile compared with epidermal Langerhans cells. Journal of immunology. 2010 Apr 15;184(8):4557–67. doi: 10.4049/jimmunol.0902336. PubMed PMID: 20220088. Pubmed Central PMCID: PMC3142675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Haroche J, Abla O. Uncommon histiocytic disorders: Rosai-Dorfman, juvenile xanthogranuloma, and Erdheim-Chester disease. Hematology / the Education Program of the American Society of Hematology American Society of Hematology Education Program. 2015 Dec 5;2015(1):571–8. doi: 10.1182/asheducation-2015.1.571. PubMed PMID: 26637774. [DOI] [PubMed] [Google Scholar]
- 7.Weitzman S, Jaffe R. Uncommon histiocytic disorders: the non-Langerhans cell histiocytoses. Pediatric blood & cancer. 2005 Sep;45(3):256–64. doi: 10.1002/pbc.20246. PubMed PMID: 15547923. [DOI] [PubMed] [Google Scholar]
- 8*.Diamond EL, Durham BH, Haroche J, Yao Z, Ma J, Parikh SA, et al. Diverse and Targetable Kinase Alterations Drive Histiocytic Neoplasms. Cancer discovery. 2016 Feb;6(2):154–65. doi: 10.1158/2159-8290.CD-15-0913. PubMed PMID: 26566875. Pubmed Central PMCID: PMC4744547. [This study was the first unbiased whole exome and transcriptome sequencing study across histiocytoses and identified recurrent MAP2K1 and ARAF mutations and kinase fusions in non-LCH and the therapeutic potential of MEK inhibition in histiocytoses.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Badalian-Very G, Vergilio JA, Degar BA, MacConaill LE, Brandner B, Calicchio ML, et al. Recurrent BRAF mutations in Langerhans cell histiocytosis. Blood. 2010 Sep 16;116(11):1919–23. doi: 10.1182/blood-2010-04-279083. PubMed PMID: 20519626. Pubmed Central PMCID: PMC3173987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rollins BJ. Genomic Alterations in Langerhans Cell Histiocytosis. Hematology/oncology clinics of North America. 2015 Oct;29(5):839–51. doi: 10.1016/j.hoc.2015.06.004. PubMed PMID: 26461146. [DOI] [PubMed] [Google Scholar]
- 11.Haroche J, Charlotte F, Arnaud L, von Deimling A, Helias-Rodzewicz Z, Hervier B, et al. High prevalence of BRAF V600E mutations in Erdheim-Chester disease but not in other non-Langerhans cell histiocytoses. Blood. 2012 Sep 27;120(13):2700–3. doi: 10.1182/blood-2012-05-430140. PubMed PMID: 22879539. [DOI] [PubMed] [Google Scholar]
- 12.Go H, Jeon YK, Huh J, Choi SJ, Choi YD, Cha HJ, et al. Frequent detection of BRAF(V600E) mutations in histiocytic and dendritic cell neoplasms. Histopathology. 2014 Aug;65(2):261–72. doi: 10.1111/his.12416. PubMed PMID: 24720374. [DOI] [PubMed] [Google Scholar]
- 13.O'Malley DP, Agrawal R, Grimm KE, Hummel J, Glazyrin A, Dim DC, et al. Evidence of BRAF V600E in indeterminate cell tumor and interdigitating dendritic cell sarcoma. Annals of diagnostic pathology. 2015 Jun;19(3):113–6. doi: 10.1016/j.anndiagpath.2015.02.008. PubMed PMID: 25787243. [DOI] [PubMed] [Google Scholar]
- 14.Kansal R, Quintanilla-Martinez L, Datta V, Lopategui J, Garshfield G, Nathwani BN. Identification of the V600D mutation in Exon 15 of the BRAF oncogene in congenital, benign langerhans cell histiocytosis. Genes, chromosomes & cancer. 2013 Jan;52(1):99–106. doi: 10.1002/gcc.22010. PubMed PMID: 22996177. [DOI] [PubMed] [Google Scholar]
- 15.Kordes M, Roring M, Heining C, Braun S, Hutter B, Richter D, et al. Cooperation of BRAF and mutant HRAS in histiocytic sarcoma provides new insights into oncogenic BRAF signaling. Leukemia. 2015 Nov 19; doi: 10.1038/leu.2015.319. PubMed PMID: 26582644. [DOI] [PubMed] [Google Scholar]
- 16.Satoh T, Smith A, Sarde A, Lu HC, Mian S, Trouillet C, et al. B-RAF mutant alleles associated with Langerhans cell histiocytosis, a granulomatous pediatric disease. PloS one. 2012;7(4):e33891. doi: 10.1371/journal.pone.0033891. PubMed PMID: 22506009. Pubmed Central PMCID: PMC3323620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17*.Nelson DS, Quispel W, Badalian-Very G, van Halteren AG, van den Bos C, Bovee JV, et al. Somatic activating ARAF mutations in Langerhans cell histiocytosis. Blood. 2014 May 15;123(20):3152–5. doi: 10.1182/blood-2013-06-511139. PubMed PMID: 24652991. [This was the first paper to identify ARAF mutations in the histiocytoses.] [DOI] [PubMed] [Google Scholar]
- 18*.Brown NA, Furtado LV, Betz BL, Kiel MJ, Weigelin HC, Lim MS, et al. High prevalence of somatic MAP2K1 mutations in BRAF V600E-negative Langerhans cell histiocytosis. Blood. 2014 Sep 4;124(10):1655–8. doi: 10.1182/blood-2014-05-577361. PubMed PMID: 24982505. [This was the first paper to identify activating MAP2K1 mutations in the histiocytoses.] [DOI] [PubMed] [Google Scholar]
- 19.Chakraborty R, Hampton OA, Shen X, Simko SJ, Shih A, Abhyankar H, et al. Mutually exclusive recurrent somatic mutations in MAP2K1 and BRAF support a central role for ERK activation in LCH pathogenesis. Blood. 2014 Nov 6;124(19):3007–15. doi: 10.1182/blood-2014-05-577825. PubMed PMID: 25202140. Pubmed Central PMCID: PMC4224195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nelson DS, van Halteren A, Quispel WT, van den Bos C, Bovee JV, Patel B, et al. MAP2K1 and MAP3K1 mutations in Langerhans cell histiocytosis. Genes, chromosomes & cancer. 2015 Jun;54(6):361–8. doi: 10.1002/gcc.22247. PubMed PMID: 25899310. [DOI] [PubMed] [Google Scholar]
- 21.Ozono S, Inada H, Nakagawa S, Ueda K, Matsumura H, Kojima S, et al. Juvenile myelomonocytic leukemia characterized by cutaneous lesion containing Langerhans cell histiocytosis-like cells. International journal of hematology. 2011 Mar;93(3):389–93. doi: 10.1007/s12185-011-0787-x. PubMed PMID: 21350822. [DOI] [PubMed] [Google Scholar]
- 22.Heritier S, Saffroy R, Radosevic-Robin N, Pothin Y, Pacquement H, Peuchmaur M, et al. Common cancer-associated PIK3CA activating mutations rarely occur in Langerhans cell histiocytosis. Blood. 2015 Apr 9;125(15):2448–9. doi: 10.1182/blood-2015-01-625491. PubMed PMID: 25858893. [DOI] [PubMed] [Google Scholar]
- 23.Emile JF, Diamond EL, Helias-Rodzewicz Z, Cohen-Aubart F, Charlotte F, Hyman DM, et al. Recurrent RAS and PIK3CA mutations in Erdheim-Chester disease. Blood. 2014 Nov 6;124(19):3016–9. doi: 10.1182/blood-2014-04-570937. PubMed PMID: 25150293. Pubmed Central PMCID: PMC4224196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Diamond EL, Abdel-Wahab O, Pentsova E, Borsu L, Chiu A, Teruya-Feldstein J, et al. Detection of an NRAS mutation in Erdheim-Chester disease. Blood. 2013 Aug 8;122(6):1089–91. doi: 10.1182/blood-2013-02-482984. PubMed PMID: 23929840. [DOI] [PubMed] [Google Scholar]
- 25**.Brown RA, Kwong BY, McCalmont TH, Ragsdale B, Ma L, Cheung C, et al. ETV3-NCOA2 in indeterminate cell histiocytosis: clonal translocation supports sui generis. Blood. 2015 Nov 12;126(20):2344–5. doi: 10.1182/blood-2015-07-655530. PubMed PMID: 26438513. [This study was a case series that discovered recurrent ETV3-NCOA2 gene fusions in the non-LCH neoplasm indeterminate cell histiocytosis and was one of the 2 studies to first describe gene fusions in the histiocytoses.] [DOI] [PubMed] [Google Scholar]
- 26.Emuss V, Garnett M, Mason C, Marais R. Mutations of C-RAF are rare in human cancer because C-RAF has a low basal kinase activity compared with B-RAF. Cancer research. 2005 Nov 1;65(21):9719–26. doi: 10.1158/0008-5472.CAN-05-1683. PubMed PMID: 16266992. [DOI] [PubMed] [Google Scholar]
- 27.Takeuchi K, Choi YL, Togashi Y, Soda M, Hatano S, Inamura K, et al. KIF5B-ALK, a novel fusion oncokinase identified by an immunohistochemistry-based diagnostic system for ALK-positive lung cancer. Clinical cancer research : an official journal of the American Association for Cancer Research. 2009 May 1;15(9):3143–9. doi: 10.1158/1078-0432.CCR-08-3248. PubMed PMID: 19383809. [DOI] [PubMed] [Google Scholar]
- 28.Wiesner T, He J, Yelensky R, Esteve-Puig R, Botton T, Yeh I, et al. Kinase fusions are frequent in Spitz tumours and spitzoid melanomas. Nature communications. 2014;5:3116. doi: 10.1038/ncomms4116. PubMed PMID: 24445538. Pubmed Central PMCID: PMC4084638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wang L, Motoi T, Khanin R, Olshen A, Mertens F, Bridge J, et al. Identification of a novel, recurrent HEY1-NCOA2 fusion in mesenchymal chondrosarcoma based on a genome-wide screen of exon-level expression data. Genes, chromosomes & cancer. 2012 Feb;51(2):127–39. doi: 10.1002/gcc.20937. PubMed PMID: 22034177. Pubmed Central PMCID: PMC3235801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mesquita B, Lopes P, Rodrigues A, Pereira D, Afonso M, Leal C, et al. Frequent copy number gains at 1q21 and 1q32 are associated with overexpression of the ETS transcription factors ETV3 and ELF3 in breast cancer irrespective of molecular subtypes. Breast cancer research and treatment. 2013 Feb;138(1):37–45. doi: 10.1007/s10549-013-2408-2. PubMed PMID: 23329352. [DOI] [PubMed] [Google Scholar]
- 31.Carapeti M, Aguiar RC, Goldman JM, Cross NC. A novel fusion between MOZ and the nuclear receptor coactivator TIF2 in acute myeloid leukemia. Blood. 1998 May 1;91(9):3127–33. PubMed PMID: 9558366. [PubMed] [Google Scholar]
- 32.Deguchi K, Ayton PM, Carapeti M, Kutok JL, Snyder CS, Williams IR, et al. MOZ-TIF2-induced acute myeloid leukemia requires the MOZ nucleosome binding motif and TIF2-mediated recruitment of CBP. Cancer cell. 2003 Mar;3(3):259–71. doi: 10.1016/s1535-6108(03)00051-5. PubMed PMID: 12676584. [DOI] [PubMed] [Google Scholar]
- 33.Strehl S, Nebral K, Konig M, Harbott J, Strobl H, Ratei R, et al. ETV6-NCOA2: a novel fusion gene in acute leukemia associated with coexpression of T-lymphoid and myeloid markers and frequent NOTCH1 mutations. Clinical cancer research : an official journal of the American Association for Cancer Research. 2008 Feb 15;14(4):977–83. doi: 10.1158/1078-0432.CCR-07-4022. PubMed PMID: 18281529. [DOI] [PubMed] [Google Scholar]
- 34.Sumegi J, Streblow R, Frayer RW, Dal Cin P, Rosenberg A, Meloni-Ehrig A, et al. Recurrent t(2;2) and t(2;8) translocations in rhabdomyosarcoma without the canonical PAX-FOXO1 fuse PAX3 to members of the nuclear receptor transcriptional coactivator family. Genes, chromosomes & cancer. 2010 Mar;49(3):224–36. doi: 10.1002/gcc.20731. PubMed PMID: 19953635. Pubmed Central PMCID: PMC2808450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Samatar AA, Poulikakos PI. Targeting RAS-ERK signalling in cancer: promises and challenges. Nature reviews Drug discovery. 2014 Dec;13(12):928–42. doi: 10.1038/nrd4281. PubMed PMID: 25435214. [DOI] [PubMed] [Google Scholar]
- 36*.Haroche J, Cohen-Aubart F, Emile JF, Maksud P, Drier A, Toledano D, et al. Reproducible and sustained efficacy of targeted therapy with vemurafenib in patients with BRAF(V600E)-mutated Erdheim-Chester disease. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2015 Feb 10;33(5):411–8. doi: 10.1200/JCO.2014.57.1950. PubMed PMID: 25422482. [This study revealed the dramatic and sustained clinical response to vemurafenib in BRAF V600E-mutant histiocytoses.] [DOI] [PubMed] [Google Scholar]
- 37**.Hyman DM, Puzanov I, Subbiah V, Faris JE, Chau I, Blay JY, et al. Vemurafenib in Multiple Nonmelanoma Cancers with BRAF V600 Mutations. The New England journal of medicine. 2015 Aug 20;373(8):726–36. doi: 10.1056/NEJMoa1502309. PubMed PMID: 26287849. [This study revealed excellent responses to vemurafenib in BRAF V600E-mutant LCH and ECD patients in the context of a vemurafenib, histology-independent, phase II clinical trial (“basket trial”).] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38*.Heritier S, Jehanne M, Leverger G, Emile JF, Alvarez JC, Haroche J, et al. Vemurafenib Use in an Infant for High-Risk Langerhans Cell Histiocytosis. JAMA oncology. 2015 Sep;1(6):836–8. doi: 10.1001/jamaoncol.2015.0736. PubMed PMID: 26180941. [This study revealed the therapeutic potential of RAF inhibition in pediatric BRAF V600E-mutant, multi-system LCH patients refractory to conventional therapy.] [DOI] [PubMed] [Google Scholar]
- 39.Haroche J, Cohen-Aubart F, Emile JF, Arnaud L, Maksud P, Charlotte F, et al. Dramatic efficacy of vemurafenib in both multisystemic and refractory Erdheim-Chester disease and Langerhans cell histiocytosis harboring the BRAF V600E mutation. Blood. 2013 Feb 28;121(9):1495–500. doi: 10.1182/blood-2012-07-446286. PubMed PMID: 23258922. [DOI] [PubMed] [Google Scholar]
- 40.Charles J, Beani JC, Fiandrino G, Busser B. Major response to vemurafenib in patient with severe cutaneous Langerhans cell histiocytosis harboring BRAF V600E mutation. Journal of the American Academy of Dermatology. 2014 Sep;71(3):e97–9. doi: 10.1016/j.jaad.2014.03.038. PubMed PMID: 25128147. [DOI] [PubMed] [Google Scholar]
- 41.Wilhelm S, Carter C, Lynch M, Lowinger T, Dumas J, Smith RA, et al. Discovery and development of sorafenib: a multikinase inhibitor for treating cancer. Nature reviews Drug discovery. 2006 Oct;5(10):835–44. doi: 10.1038/nrd2130. PubMed PMID: 17016424. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.